Abstract
Introduction
Rates of cesarean sections (CS) have increased dramatically over the past two decades in India. This increase has been disproportionately high in private facilities, but little is known about the drivers of the CS rate increase and how they vary over time and geographically.
Methods
Women enrolled in the Nagpur, India site of the Global Network for Women’s and Children’s Health Research Maternal and Neonatal Health Registry, who delivered in a health facility with CS capability were included in this study. The trend in CS rates from 2010 to 2017 in public and private facilities were assessed and displayed by subdistrict. Multivariable generalized estimating equations models were used to assess the association of delivering in private versus public facilities with having a CS, adjusting for known risk factors.
Results
CS rates increased substantially between 2010 and 2017 at both public and private facilities. The odds of having a CS at a private facility were 40% higher than at a public facility after adjusting for other known risk factors. CS rates had unequal spatial distributions at the subdistrict level.
Discussion
Our study findings contribute to the knowledge of increasing CS rates in both public and private facilities in India. Maps of the spatial distribution of subdistrict-based CS rates are helpful in understanding patterns of CS deliveries, but more investigation as to why clusters of high CS rates have formed in warranted.
Introduction
Cesarean section (CS) is a life-saving procedure when certain complications arise during pregnancy and delivery. At a 1985 meeting of the World Health Organization (WHO), a panel of reproductive health experts identified the “ideal” population-based CS rate to be between 10 and 15% [1]. Since then, global CS rates rose from 12.1% in 2000 to 21.1% in 2015 [2]. This increase prompted WHO to revisit the ideal rate suggested in 1985, and resulted in a recommendation that every effort should be taken to ensure that CS are provided to women in need, rather than focusing on achieving a certain CS rate [3]. In order to avoid major obstetric complications that can lead to maternal and infant death, CS are essential treatment for antepartum hemorrhage, prolonged or obstructed labor, pre-eclampsia or eclampsia, and intrapartum fetal distress [4].
The unprecedented rise in the use of CS in the past two decades can be explained by both an increase of institutional births and increased use of CS within facilities [5]. Reasons for increased CS within facilities are due to factors related to the pregnant women, their families, health professionals and health care systems [6]. Privately owned facilities have disproportionately contributed to increasing CS rates, although rates continue to increase in publicly funded facilities as well [5]. Using the most recent Demographic and Health Survey (DHS) data from 50 low- and middle-income countries between 2000 and 2013, Benova et al. found that privately funded facilities had higher CS rates in every region [7].
Reasons for having CS include both demographic characteristics, such as older maternal age, higher parity and higher socioeconomic status, and clinical indicators, including non-reassuring fetal status, labor arrest disorders, malpresentation, multi-gestation births [8–11]. Consequences of CS include higher maternal and perinatal mortality than with vaginal birth and increased short- and long-term health consequences for mothers, such as uterine rupture, infection or hemorrhage, and infants, including altered immune development, an increased likelihood of allergy, atopy, and asthma, and reduced intestinal gut microbiome diversity [11,12]. There is also an increased risk of maternal death for CS when conducted without a medical indication [13].
Financial schemes to incentivize facility-based deliveries can also influence the rate of CS [14]. In India, Janani Suraksha Yojana (JSY) was implemented in 2005 to reduce maternal and neonatal mortality by promoting institutional delivery as opposed to home deliveries among pregnant women below the poverty line [15]. In the 2005–2006 Indian National Family Health Survey (NFHS-3), 39% of deliveries took place in institutions but in NHFS-4 during 2015–2016, 79% of deliveries occurred in institutions [16,17]. CS rates increased from 9% of all live births in 2005–2006 [16] to 17% in 2015–2016 [17]. The Indian district level household survey in 2011 (DLHS-4) found that CS births were disproportionately high and nearly three times more likely in private facilities than in public facilities [8].
While rates of CS in India have increased in the last 10 years, less is known about the drivers of the change in CS rates and whether they vary over time and geographically. The Eunice Kennedy Shriver National Institute of Child Health and Human Development’s (NICHD’s) Global Network (GN), is a multi-site research network representing partnerships of U.S. and international investigators at rural and semi-urban study sites in Guatemala, India (2 sites: Nagpur and Belgaum), Pakistan, Kenya, Zambia and the Democratic Republic of the Congo. The GN Maternal and Newborn Health Registry (MNHR) has been collecting data on a population-based sample of pregnant women and their babies starting in 2008. Using data from the Nagpur, India site, the primary aims of this study are to (1) assess the change in CS rates over time in the public and private facilities where the women deliver their babies and (2) determine the maternal characteristics associated with CS rates in private and public facilities in the catchment area of the study population. A secondary aim of this study was to visualize the geographic distribution of CS rates in the subdistricts over time.
Materials and methods
Study population
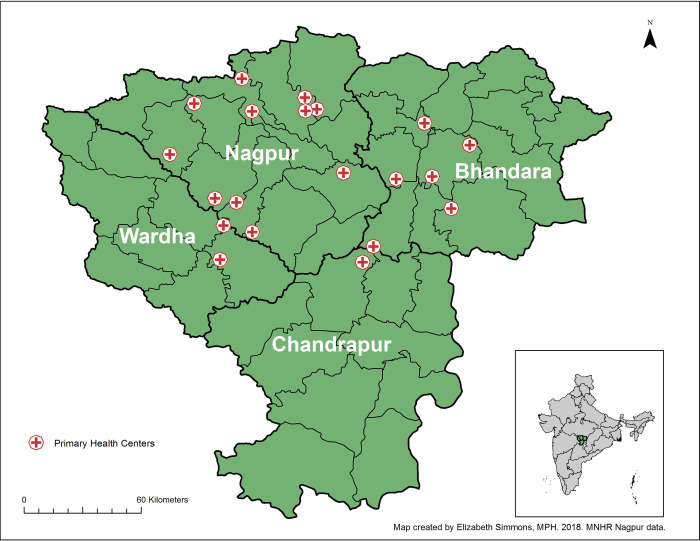
Prospectively-collected data from pregnant women and their babies enrolled in the Nagpur site (Eastern Maharashtra) of the MNHR was used for this study. The details of the MNHR registry have been previously published [18]. In brief, each GN site, including the Nagpur site, studies a population of 8 to 20 predetermined geographic areas or clusters. In Nagpur, each cluster is defined as the catchment area of a primary health center (PHC), with 300–500 expected births each year. Between 2010 and 2018, the Nagpur site included 20 PHCs in the Nagpur, Bhandara, Wardha and Chandrapur districts in eastern Maharashtra that extend 25–100 km radially from the urban center, Nagpur city (Fig 1). Women are enrolled as early as possible in pregnancy (usually early in the 2nd trimester of pregnancy, but increasingly over time during the first trimester) and are followed-up after labor and delivery through day 42 post-partum to collect details of maternal and neonatal outcomes.
Fig 1. Map of 20 primary health centers in Nagpur area.
Ethical approvals
Pregnant women presenting for antenatal care at one of the Nagpur site’s PHC were informed about the study and invited to participate in the MNH registry. Those who agreed and provided written informed consent were enrolled in the Registry. Institutional Review Boards at Lata Medical Research Foundation (LMRF) and Boston University Medical Campus (BUMC) approved the protocol and consent forms. The GN for Women’s and Child’s Health Research MNMR Study is registered on clinicaltrials.gov under NCT01073475.
Demographic and health data collection
Three forms were used to collect data on women enrolled in the MNHR [19]. The enrollment form collected background information, residence status and planned delivery location from the mother at the time of enrollment. The enrollment form collected maternal age (<20, 20–24, 25–20, 30+ years), parity (≥1 vs. 0), maternal education (None, 1–6, 7–12, >12 years) and anemia [yes (hemoglobin < 11 g/dL) vs. no (hemoglobin ≥ 11 g/dL)]. Within 7 days of delivery, the perinatal form was completed with data on health care services the mother received during pregnancy, delivery information, neonatal and maternal outcomes and treatments provided at time of delivery. These data were used to derive the gestational age at birth (full term (≥37 weeks) vs. preterm), birth weight (normal (≥2500 g) vs. low) and year of delivery (2010–2017). The perinatal form also collected information on our primary outcome, mode of delivery (vaginal/vaginal assisted versus cesarean section) for the women enrolled in the MNHR.
Identification and geocoding of public and private facilities with CS capability
Between 2010 to 2017, women participating in the Nagpur site of MNH Registry delivered at 133 facilities (101 private; 32 public) with CS capabilities. For the purposes of this study, having CS capability was defined as being a secondary level facility or higher, as primary health centers manage normal deliveries only [20]. While it would have been ideal to identify facilities with a blood bank on site, this information was not readily available in this study, particularly for the private facilities. In the public health system, we are confident that secondary facilities and higher have the ability to conduct CS. We kept this definition consistent for private facilities in the absence of more information. During field research officer visits to each facility, the GPS coordinates were collected at the front gate of the facility using a smartphone. The number of private facilities used by women in the MNHR in the area more than tripled from 2010 to 2017, from 29 to 101. Growth in public facilities in the area increased from 22 in 2010 to 32 in 2017.
Statistical methods
Descriptive statistics were calculated for all variables to describe the study population. Chi-square analysis was used to compare differences in proportions between public and private facilities. CS rates of each subregion were calculated for each year from 2011 to 2017 and displayed geographically using ArcGIS (Esri, Redlands, California). We obtained Odds ratios (OR) and 95% Confidence Intervals (CI) from multivariable generalized estimating equations models that assessed the association of public/private facilities with having a CS adjusting for known risk factors. We also tested the interaction between maternal age and parity was included in the multivariable model. We tested whether the trend in the odds of having a CS increased significantly with each year by including the delivery year as a continuous variable in the models. We further used a random effects model with random intercept and slope to assess if the trajectory of the CS rates was similar in public and private facilities. This accounts for the within-facility and between-facility variability. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and a two-sided p<0.05 was considered to be significant.
Results
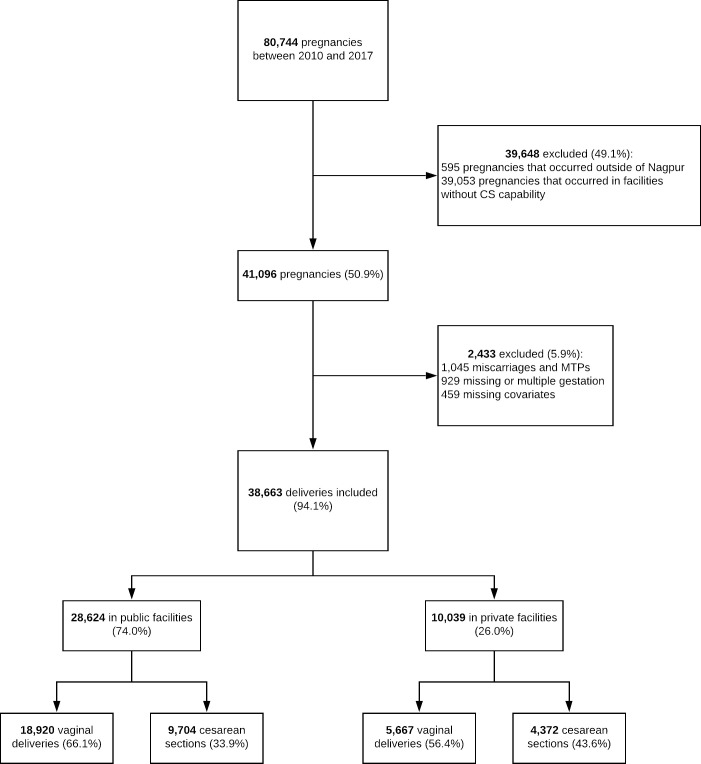
From 2010 to 2017, 80,744 deliveries were recorded in the MNHR. This analysis included the 38,663 deliveries that occurred in facilities where CS were performed and excluded women who had a miscarriage or a medical termination of pregnancy (1,045), women with a multiple or missing gestation (708), and women with missing covariates (136). Thirty-six percent of all MNHR registry deliveries, 34% of all MNHR deliveries in public facilities and 44% of all MNHR deliveries in private facilities were by CS (Fig 2).
Fig 2. Flow diagram.
Table 1 displays characteristics of our study sample by delivery facility type. Over half of women age 30 and over who delivered in private facilities had a CS, compared with only 43.5% of women in the same age group who delivered in public facilities. Almost half of women with more than 12 years of education who delivered in a private facility had a CS whereas 37.9% of women with the same educational attainment had a CS in public facilities.
Table 1. Background characteristics of population by type of facility of delivery.
| Type of facility | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All deliveries n = 38663 | All Public Deliveries n = 28624 | All Private Deliveries n = 10039 | |||||||
| CS | No CS | pa | CS | No CS | pa | CS | No CS | pa | |
| N(Row%) | N(Row%) | N(Row%) | N(Row%) | N(Row%) | N(Row%) | ||||
| Maternal Age | |||||||||
| < 20 years | 257 (28.9) | 633 (71.1) | < .0001 | 197 (27.7) | 514 (72.3) | < .0001 | 60 (33.5) | 119 (66.5) | < .0001 |
| 20–24 years | 8563 (34.2) | 16505 (65.8) | 6049 (32.1) | 12770 (67.9) | 2514 (40.2) | 3735 (59.8) | |||
| 25–29 years | 4336 (40.2) | 6450 (59.8) | 2874 (37.1) | 4878 (62.9) | 1462 (48.2) | 1572 (51.8) | |||
| 30+ years | 920 (47.9) | 999 (52.1) | 584 (43.5) | 758 (56.5) | 336 (58.2) | 241 (41.8) | |||
| Parity | |||||||||
| ≥1 | 6099 (36.4) | 10652 (63.6) | 0.99 | 4234 (33.9) | 8253 (66.1) | 0.99 | 1865 (43.7) | 2399 (56.3) | 0.74 |
| 0 | 7977 (36.4) | 13935 (63.6) | 5470 (33.9) | 10667 (66.1) | 2507 (43.4) | 3268 (56.6) | |||
| Education | |||||||||
| None | 244 (28.3) | 618 (71.7) | < .0001 | 175 (27.3) | 466 (72.7) | < .0001 | 69 (31.2) | 152 (68.8) | < .0001 |
| 1–6 years | 1087 (29.3) | 2629 (70.8) | 847 (27.9) | 2186 (72.1) | 240 (35.1) | 443 (64.9) | |||
| 7–12 years | 9621 (36.0) | 17072 (64.0) | 6912 (34.1) | 13365 (65.9) | 2709 (42.2) | 3707 (57.8) | |||
| >12 years | 3124 (42.3) | 4268 (57.7) | 1770 (37.9) | 2903 (62.1) | 1354 (49.8) | 1365 (50.2) | |||
| Gestational Age | |||||||||
| Full term | 12978 (36.9) | 22236 (63.2) | < .0001 | 9022 (34.5) | 17105 (65.5) | < .0001 | 5131 (56.5) | 3956 (43.5) | 0.92 |
| Preterm | 1098 (31.8) | 2351 (68.2) | 682 (27.3) | 1815 (72.7) | 536 (56.3) | 416 (43.7) | |||
| Birth weight | |||||||||
| Normal | 9045 (37.9) | 14831 (62.1) | < .0001 | 6120 (35.5) | 11133 (64.5) | < .0001 | 2925 (44.2) | 3698 (55.8) | 0.08 |
| Low | 5031 (34.0) | 9756 (66.0) | 3584 (31.5) | 7787 (68.5) | 1447 (42.4) | 1969 (57.6) | |||
| Anemia | |||||||||
| Yes | 12433 (35.8) | 22344 (64.3) | < .0001 | 8740 (33.4) | 17395 (66.6) | < .0001 | 3693 (42.7) | 4949 (57.3) | < .0001 |
| No | 1643 (42.3) | 2243 (57.7) | 964 (38.7) | 1525 (61.3) | 679 (48.6) | 718 (51.4) | |||
| Year of Delivery | |||||||||
| 2010 | 1253 (28.2) | 3196 (71.8) | < .0001 | 906 (26.3) | 2533 (73.7) | < .0001 | 347 (34.4) | 663 (65.6) | < .0001 |
| 2011 | 1388 (30.0) | 3236 (70.0) | 956 (28.1) | 2441 (71.9) | 432 (35.2) | 795 (64.8) | |||
| 2012 | 1454 (32.8) | 2980 (67.2) | 1049 (31.0) | 2331 (69.0) | 405 (38.4) | 649 (61.6) | |||
| 2013 | 1706 (34.1) | 3300 (65.9) | 1192 (31.3) | 2623 (68.8) | 514 (43.2) | 677 (56.8) | |||
| 2014 | 1727 (36.8) | 2963 (63.2) | 1241 (35.0) | 2306 (65.0) | 486 (42.5) | 657 (57.5) | |||
| 2015 | 2198 (41.9) | 3047 (58.1) | 1490 (39.5) | 2287 (60.6) | 708 (48.2) | 760 (51.8) | |||
| 2016 | 2257 (43.2) | 2972 (56.8) | 1481 (40.1) | 2209 (59.9) | 776 (50.4) | 763 (49.6) | |||
| 2017 | 2093 (42.0) | 2893 (58.0) | 1389 (38.8) | 2190 (61.2) | 704 (50.0) | 703 (50.0) | |||
a p-value produced using chi-square test of independence.
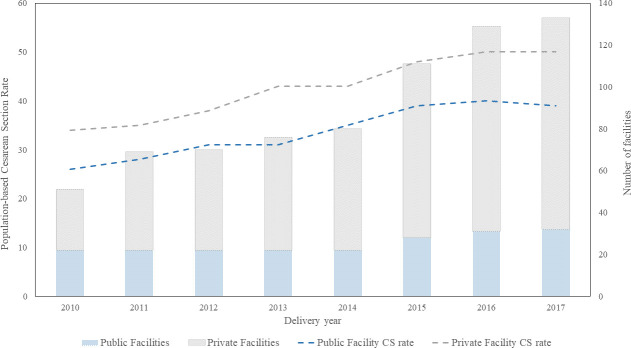
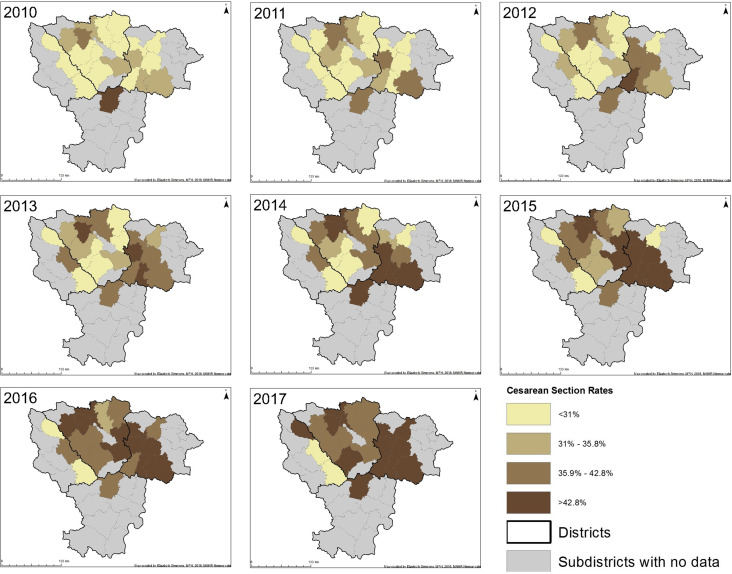
The number of private and public facilities and CS rates by type of facility over time are displayed in Fig 3. While the number of public facilities increased slightly over time, the number of private facilities increased by 250% in the 8-year period. However, there was no evidence to suggest that the increase over time was statistically different between private and public facilities over the same period. Subdistrict-based CS rates also increased over time in almost all subdistricts (Fig 4).
Fig 3. Linear trend in population-based Cesarean section (CS) rate and histogram of number of private and public facilities from 2010 to 2017 by facility type.
Fig 4. Change in subdistrict population-based cesarean section rate from 2010 to 2017.
Table 2 displays the ORs and 95% CIs evaluating the association between having a CS with type of facility adjusted for known risk factors. Private facilities had a 40% increase in the odds of having a CS delivery compared with public facilities, after adjusting for all covariates [OR(95% CI): 1.40(1.14, 1.72); p<0.01]. The adjusted results indicate the odds of having a CS increased with higher maternal education [1–6 years: 1.28(1.07, 1.54); 7–12 years: 1.50(1.30, 1.72); >12 years: 1.89(1.66, 2.15); p<0.0001], increasing year of delivery [2011: 1.07(0.99, 1.16); 2017: 1.71(1.49, 1.97); p<0.0001] and with being not anemic [1.15(1.05, 1.26); p<0.01]. Nulliparous women at every age had higher odds of delivering by CS than primi- and multiparous women with those aged 30+ having the highest odds [3.24(1.25, 8.41); p<0.0001]. The odds of having a CS decreased for preterm babies [0.82(0.73, 0.91); p<0.001] and for low birth weight babies [0.91(0.86, 0.96); p = 0.001]. The trend test indicated that the odds of having a CS increased by 9% for each year between 2010 and 2017 [1.09(1.08–1.11); p<0.0001].
Table 2. Odds ratios (OR) and 95% Confidence Intervals (CI) obtained from multivariable generalized estimating equations models evaluating the association of CS with type of facility adjusting for known risk factors.
| Type of Delivery | Unadjusted Model | p | Adjusted Modela | p | ||
|---|---|---|---|---|---|---|
| Vaginal Delivery | Cesarean Section | |||||
| n(Row %) | OR (95%CI) | OR (95%CI) | ||||
| Type of Facility | ||||||
| Public (REF) | 18920 (66) | 9704 (34) | <0.001 | <0.01 | ||
| Private | 5667 (56) | 4372 (44) | 1.50 (1.20, 1.89) | 1.40 (1.14, 1.72) | ||
| Maternal Age (years)b | ||||||
| <20 (REF) | 633 (71) | 257 (29) | ||||
| 20–24 | 16505 (66) | 8563 (34) | ||||
| 25–29 | 6450 (60) | 4336 (40) | ||||
| 30+ | 999 (52) | 920 (48) | ||||
| Parityb | ||||||
| ≥1 (REF) | 10652 (64) | 6099 (36) | ||||
| 0 | 13935 (64) | 7977 (36) | ||||
| Maternal age (years), Parity | ||||||
| <20, ≥1 (REF) | 14 (74) | 5 (26) | < .0001 | < .0001 | ||
| <20, 0 (REF) | 619 (71) | 252 (29) | ||||
| 20–24, ≥1 (REF) | 4972 (66) | 2512 (34) | ||||
| 20–24, 0 | 11533 (66) | 6051 (34) | 1.47 (0.52, 4.12) | 1.25 (0.46, 3.38) | ||
| 25–29, ≥1 (REF) | 4864 (62) | 2944 (38) | ||||
| 25–29, 0 | 1586 (53) | 1392 (47) | 2.46 (0.92, 6.53) | 1.91 (0.74, 4.90) | ||
| 30+, ≥1 (REF) | 802 (56) | 638 (44) | ||||
| 30+, 0 | 197 (41) | 282 (59) | 4.01 (1.47, 10.93) | 3.24 (1.25, 8.41) | ||
| Education (years) | ||||||
| None (REF) | 618 (72) | 244 (28) | < .0001 | < .0001 | ||
| 1–6 | 2629 (71) | 1087 (29) | 1.05 (0.89, 1.23) | 1.28 (1.07, 1.54) | ||
| 7–12 | 17072 (64) | 9621 (36) | 1.43 (1.23, 1.66) | 1.50 (1.30, 1.72) | ||
| >12 | 4268 (58) | 3124 (42) | 1.85 (1.59, 2.17) | 1.89 (1.66, 2.15) | ||
| Gestational Age | ||||||
| Full term (REF) | 22236 (63) | 12978 (37) | < .0001 | <0.001 | ||
| Preterm | 2351 (68) | 1098 (32) | 0.80 (0.74, 0.86) | 0.82 (0.73, 0.91) | ||
| Birth weight | ||||||
| Normal (REF) | 14831 (62) | 9045 (38) | < .0001 | <0.01 | ||
| Low | 9756 (66) | 5031 (34) | 0.85 (0.81, 0.88) | 0.91 (0.86, 0.96) | ||
| Anemia | ||||||
| Yes (REF) | 22344 (64) | 12433 (36) | < .0001 | <0.01 | ||
| No | 2243 (58) | 1643 (42) | 1.32 (1.23, 1.41) | 1.15 (1.05, 1.26) | ||
| Year of Delivery | ||||||
| 2010 (REF) | 3196 (72) | 1253 (28) | < .0001 | < .0001 | ||
| 2011 | 3236 (70) | 1388 (30) | 1.09 (1.00, 1.20) | 1.07 (0.99, 1.16) | ||
| 2012 | 2980 (67) | 1454 (33) | 1.24 (1.14, 1.36) | 1.22 (1.08, 1.38) | ||
| 2013 | 3300 (66) | 1706 (34) | 1.32 (1.21, 1.44) | 1.28 (1.13, 1.44) | ||
| 2014 | 2963 (63) | 1727 (37) | 1.49 (1.36, 1.62) | 1.46 (1.29, 1.64) | ||
| 2015 | 3047 (58) | 2198 (42) | 1.84 (1.69, 2.00) | 1.76 (1.58, 1.95) | ||
| 2016 | 2972 (57) | 2257 (43) | 1.94 (1.78, 2.11) | 1.81 (1.60, 2.05) | ||
| 2017 | 2893 (58) | 2093 (42) | 1.85 (1.69, 2.01) | 1.71 (1.49, 1.97) | ||
| Year of Delivery Trend Testc | 1.11 (1.09, 1.13) | < .0001 | 1.09 (1.08, 1.11) | < .0001 | ||
a Includes maternal age, parity, interaction of maternal age and parity, maternal education, gestational age, birth weight, anemia and year of delivery.
b ORs and 95% CI not represented as these variables are part of the interaction term.
c Estimated in a separate model with year of delivery included as a continuous variable.
Discussion
In the rural and semi-urban population of pregnant women surrounding Nagpur city in Eastern Maharashtra, we found that the odds of having a CS at a private facility were 40% higher than at a public facility after adjusting for other known risk factors. CS rates increased substantially between 2010 and 2017 at both public and private facilities, with privately funded facilities having a higher CS rate throughout the study period. We also observed an unequal spatial distribution of sub-district-based CS rates. CS rates increased more rapidly in the northern and eastern sub-districts during the 8-year study period, perhaps due to mushrooming of more private facilities in these regions.
The odds of having a CS for women in our study increased with more years of maternal education, increasing age and nulliparity, having no maternal anemia and year of delivery and decreased for preterm babies and babies of low birth weight. The same association between having a CS and maternal education has been consistently reported in India [21,22]. Women with more education are likely of higher socioeconomic status and might have resources necessary to access facilities that provide CS and possibly be less likely to tolerate long labor pains, particularly in primiparous mothers. The increased CS rates over time have also been observed elsewhere in India [16,17]. This trend is likely due to the increase in institutional births that occurred following JSY implementation. Maternal anemia is a risk factor for having preterm and low birth weight babies making all three characteristics more likely to result in smaller babies that are easier to deliver vaginally [23].
This study has several strengths. First, this study is a large, pregnancy and newborn, population-based registry that has included standardized, prospectively-collected data since 2009. Second, to our knowledge, this is one of the only studies in India to map the growth of progressively increasing CS rates and attempt to determine drivers of the increase. Finally, over 95% of the pregnant women in the four included districts are enrolled into the registry and follow-up for the study population exceeds 99%. Enrollment of almost all pregnant women in the catchment areas likely helps to reduce selection bias.
This study also has some limitations. First, mapping aggregate data assumes that the data is evenly distributed across both time and the sub-districts, which may not be the case. Second, our subdistrict CS rates were calculated based on where a woman lives, but it is possible that women travel to different subdistricts in order to give birth. More information on individual-level healthcare access is necessary to further explain the increase in CS rates. Third, we did not have data on medical indication for CS for the entire study period (only collected in 2010–2013 as reported in Patel et al [23]). An increase in medical risk factors for CS could explain the increase in CS rate. For this reason, we also could not classify CS as being elective or emergent. Fourth, we did not have information on previous CS and therefore were unable to include this important risk factor in our analysis. While previous CS is an important driver of CS rates, including previous CS rates in our study would only help to understand CS rates in multiparous mothers. Fifth, we did not have information on participant’s socioeconomic status and included maternal education as a proxy. There could be some residual confounding present in our estimates as a result. Finally, we were not able to account for patient preference for type of delivery or amount paid for services as these variables were not available in our dataset, which could create some endogeneity in our independent variable.
Conclusions
Our study found that CS rates in both private and public facilities in four districts of eastern Maharashtra increased between 2010 and 2017, with rates from women delivering in private facilities consistently higher than those of women delivering in public facilities. A map of the spatial distribution of subdistrict-based CS rates indicates an increase in CS rates more rapidly in northern and eastern subdistricts of the study area. These maps could help both researchers and government officials better understand the patterns of CS deliveries and target future resources appropriately. Further investigation into why these clusters have formed is warranted. Additional research is needed to understand these clusters of rapidly increasing CS rates in order to fully understand patterns of CS deliveries in the study area. Future qualitative studies are required to gather information on reasons for CS in order to formulate policies to reduce unnecessary CS.
Supporting information
(CSV)
Data Availability
GIS data cannot be shared publicly because of privacy concerns for study participants. The GIS data was used to create maps (Figs 1 and 4) for this manuscript and is not necessary to replicate the analyses. All other relevant data are contained within the manuscript and its Supporting Information files.
Funding Statement
PLH; 5UG1HD078439-09; NIH’S Global Network for Women’s and Children’s Health Research; https://www.nichd.nih.gov/research/supported/globalnetwork The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Appropriate technology for birth. Lancet. 1985;326: 436–437. doi: 10.1016/S0140-6736(85)92750-3 [DOI] [PubMed] [Google Scholar]
- 2.Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. The Lancet. Lancet Publishing Group; 2018. pp. 1341–1348. doi: 10.1016/S0140-6736(18)31928-7 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Statement on Caesarean Section Rates. Geneva, Switzerland; 2015. doi: 10.1016/j.rhm.2015.07.007 [DOI] [Google Scholar]
- 4.WHO, UNFPA, UNICEF, AMDD. Monitoring emergency obstetric care: A handbook. Geneva, Switzerland; 2009. [Google Scholar]
- 5.Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392: 1341–1348. doi: 10.1016/S0140-6736(18)31928-7 [DOI] [PubMed] [Google Scholar]
- 6.Betrán AP, Temmerman M, Kingdon C, Mohiddin A, Opiyo N, Torloni MR, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392: 1358–1368. doi: 10.1016/S0140-6736(18)31927-5 [DOI] [PubMed] [Google Scholar]
- 7.Benova L, Macleod D, Footman K, Cavallaro F, Lynch CA, Campbell OMR. Role of the private sector in childbirth care: cross-sectional survey evidence from 57 low- and middle-income countries using Demographic and Health Surveys. Trop Med Int Heal. 2015;20: 1657–1673. doi: 10.1111/tmi.12598 [DOI] [PubMed] [Google Scholar]
- 8.Singh P, Hashmi G, Swain PK. High prevalence of cesarean section births in private sector health facilities- analysis of district level household survey-4 (DLHS-4) of India. BMC Public Health. 2018;18: 613. doi: 10.1186/s12889-018-5533-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vieira GO, Fernandes LG, de Oliveira NF, Silva LR, Vieira T de O. Factors associated with cesarean delivery in public and private hospitals in a city of northeastern Brazil: A cross-sectional study. BMC Pregnancy Childbirth. 2015;15: 1–9. doi: 10.1186/s12884-015-0429-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alonso BD, Silva FMB da, Latorre M do RD de O, Diniz CSG, Bick D. Caesarean birth rates in public and privately funded hospitals: a cross-sectional study. Rev Saude Publica. 2017;51. doi: 10.11606/S1518-8787.2017051007054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brach DW, Silver RM. Managing the Primary Cesarean Delivery Rate. Clin Obstet Gynecol. 2012;55: 946–960. doi: 10.1097/GRF.0b013e318263c547 [DOI] [PubMed] [Google Scholar]
- 12.Sandall J, Tribe RM, Avery L, Mola G, Visser GHA, Homer CSE, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018;392: 1349–1357. doi: 10.1016/S0140-6736(18)31930-5 [DOI] [PubMed] [Google Scholar]
- 13.Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010;8: 71. doi: 10.1186/1741-7015-8-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bogg L, Diwan V, Vora KS, DeCosta A. Impact of Alternative Maternal Demand-Side Financial Support Programs in India on the Caesarean Section Rates: Indications of Supplier-Induced Demand. Matern Child Health J. 2016;20: 11–15. doi: 10.1007/s10995-015-1810-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Health Portal of India. Janani Suraksha Yojana (JSY). 2015 [cited 20 Oct 2019]. Available: https://www.nhp.gov.in/janani-suraksha-yojana-jsy-_pg.
- 16.International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005–06: India: volume I. Mumbai; 2007. doi: 10.1108/ijhcqa.2005.06218gab.007 [DOI]
- 17.Indian Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015–16: India. Int Inst Popul Sci ICF. Mumbai; 2017. doi:kwm120 [pii] Doi: 10.1093/aje/kwm120 [DOI]
- 18.Goudar SS, Carlo WA, McClure EM, Pasha O, Patel A, Esamai F, et al. The Maternal and Newborn Health Registry Study of the Global Network for Women’s and Children’s Health Research. Int J Gynecol Obstet. 2012;118: 190–193. doi: 10.1016/j.ijgo.2012.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NICHD Data and Specimen Hub. Global Network’s Maternal Newborn Health Regsitry (MNHR). 2020 [cited 14 Jun 2021]. Available: https://dash.nichd.nih.gov/study/20225.
- 20.Directorate General of Health Services, Ministry of Health and Family Welfare. Indian Public Health Standards (IPHS) Guidelines for Primary Health Centres: Revised 2012. New Delhi, India; 2012.
- 21.Leone T. Demand and supply factors affecting the rising overmedicalization of birth in India. Int J Gynecol Obstet. 2014;127: 157–162. doi: 10.1016/j.ijgo.2014.05.018 [DOI] [PubMed] [Google Scholar]
- 22.Neuman M, Alcock G, Azad K, Kuddus A, Osrin D, More NS, et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. 2014;4: e005982–e005982. doi: 10.1136/bmjopen-2014-005982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel A, Pusdekar YV, Prakash AA, Simmons E, Waikar M, Rao SR, et al. Trends and determinants of increasing caesarean sections from 2010 to 2013 in a prospective population-based registry in eastern rural Maharashtra, India. BMJ Open. 2019;9. doi: 10.1136/bmjopen-2018-024654 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(CSV)
Data Availability Statement
GIS data cannot be shared publicly because of privacy concerns for study participants. The GIS data was used to create maps (Figs 1 and 4) for this manuscript and is not necessary to replicate the analyses. All other relevant data are contained within the manuscript and its Supporting Information files.