To the Editor: We read with interest the case report by Mieczkowska et al1 describing skin findings in multisystem inflammatory syndrome in adults (MIS-A). We hope to contribute to this discussion by presenting corresponding histopathologic features in 2 patients with MIS-A with similar dermatologic manifestations.
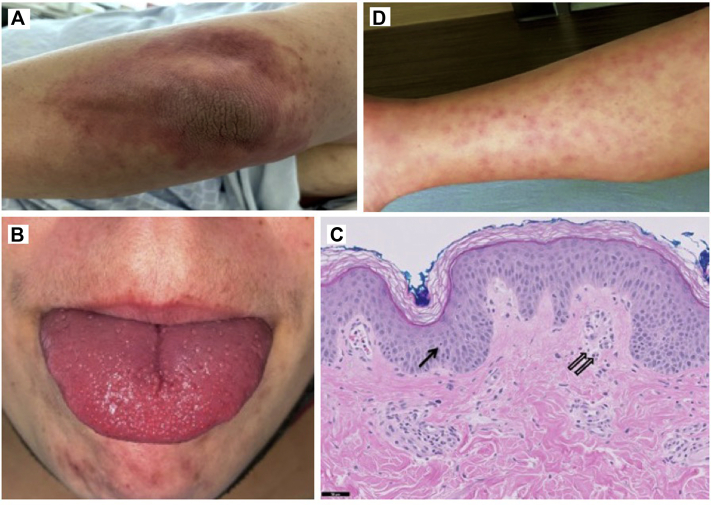
Patient 1, a 31-year-old woman, with a history of hypertension, type 2 diabetes, and obesity, recently tested positive for COVID-19 by polymerase chain reaction testing with associated dyspnea, fatigue, and myalgias; these symptoms self-resolved. Twenty-one days after testing positive, she presented with fevers, vomiting, diarrhea, arthralgias, hand swelling, and a pruritic, mildly tender rash involving the trunk and extremities. The skin examination revealed erythematous, urticarial macules coalescing into patches on intertriginous areas, extensors, dorsal aspect of hands, and feet. She had cervical lymphadenopathy and an erythematous tongue with accentuated lingual papillae (Fig 1, A and B). Skin biopsy showed superficial perivascular lymphocytic infiltrate with rare neutrophils and extravasated erythrocytes (Fig 1, C) with negative in situ hybridization for SARS-CoV-2 spike protein.
Fig 1.
Cutaneous and histologic findings of COVID-19–associated multisystem inflammatory syndrome in adults. A, Urticarial-like erythematous patch on the elbow. B, Tongue erythema with accentuated lingual papillae. C, Biopsy from the right arm showed mild epidermal spongiosis with a rare necrotic keratinocyte (closed arrow). There was also a mild superficial perivascular lymphocytic infiltrate with occasional neutrophils (open arrows). D, Erythematous papules on the lower portion of leg.
Patient 2, a 28-year-old woman with rheumatoid arthritis on intermittent treatment with adalimumab, presented 6 weeks after reverse transcriptase polymerase chain reaction–confirmed asymptomatic COVID-19 infection with fevers, fatigue, arthralgias, dyspnea, and a pruritic, mildly tender rash. Examination revealed edematous urticarial papules on the extremities coalescing to form plaques on the trunk, acral edema, conjunctivitis, and cervical lymphadenopathy (Fig 1, D). Similar to patient 1, the histologic analysis showed superficial and deep perivascular and periadnexal lymphocytic infiltrate with negative in situ hybridization for SARS-CoV-2. Both patients had laboratory workup notable for elevated levels of inflammatory markers. Rheumatologic studies demonstrated elevated levels of antinuclear antibody in both patients but were otherwise unremarkable. Infectious workup was largely negative. Both patients were treated with aspirin, intravenous immunoglobulin, and oral and topical steroids with improvement of symptoms, including rash.
As noted here and in prior reports, dermatologic findings in MIS-A are varied, including a polymorphous rash with urticarial or targetoid erythematous papules and plaques with variable mucosal involvement; an erythematous, morbilliform eruption; palmar desquamation; and conjunctivitis.1, 2, 3 To date, there has been little histopathologic characterization of MIS-A–related skin manifestations described in the literature. Based on the 2 cases of our patients, skin biopsies demonstrate nonspecific histologic findings of perivascular dermatitis with negative in situ hybridization for SARS-CoV-2 spike protein as well as negative lesional direct immunofluorescence, consistent with patterns seen in viral exanthems. We suggest that skin biopsy should only be considered in suspected MIS-A cases in contexts where it may be helpful in excluding a likely alternative diagnosis. We hope this builds upon Mieczkowska et al's1 work and prompts further study on MIS-A–related skin manifestations.
Conflicts of interest
Dr Kwong received consulting fees from Oncoderm and Happy2ndBirthday. Drs N. A. So, Centkowski, Rana, Aleshin, Rieger, Zaba, and Chiou and Author J. So have no conflicts of interest to declare.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Mieczkowska K., Zhu T.H., Hoffman L. Two adult cases of multisystem inflammatory syndrome associated with SARS-CoV-2. JAAD Case Rep. 2021;10:113–115. doi: 10.1016/j.jdcr.2021.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaigany S., Gnirke M., Guttmann A. An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19. Lancet. 2020;396(10246):e8–e10. doi: 10.1016/S0140-6736(20)31526-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sokolovsky S., Soni P., Hoffman T., Kahn P., Scheers-Masters J. COVID-19 associated Kawasaki-like multisystem inflammatory disease in an adult. Am J Emerg Med. 2021;39:253.e1–253.e2. doi: 10.1016/j.ajem.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]