According to the Center for Disease Control (CDC), 49.7% of the United States (U.S.) population has been fully vaccinated (165, 081, 416 million people) and 57.9% has received at least 1 dose (192, 120, 576 million people) as of August 3rd, 2021 [1], which is below the national goal of at least 80% [2]. The recent emergence of new SARS-CoV-2 variants emphasizes the importance of vaccinations and increasing vaccination efforts to provide sufficient protection against COVID-19 and a possible upcoming wave [3,4]
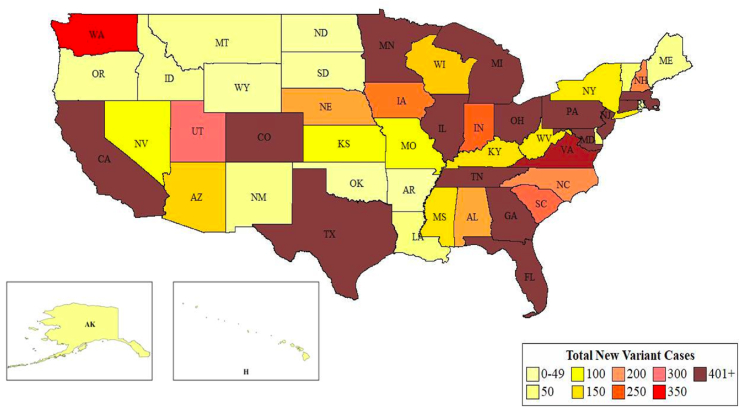
Within the plethora of SARS-CoV-2 variants identified, the most commonly referenced in the literature include B.1.1.7 (Alpha), B.1.351 (Beta), P.1, and B.1.617.2 (Delta) [5]. These variants have led to increased viral transmission, hospitalizations, and severity of disease [6], with the Delta variant being declared the most transmissible [4]. Recent data published by the CDC shows the number of variant cases, per state, for variants Alpha, Beta, and P.1 (Fig. 1) [7]. The states with the highest number of variant cases (401+) were clustered around the East, with the Alpha variant being mostly responsible. There is no available data regarding the number of variant Delta cases distributed by state as of today, but it is known to be present in the largest proportion [8].
Fig. 1.
Total Cases of New SARS-CoV-2 Variants (B.1.1.7+B.1.351+P1).
Data Source: US COVID-19 Cases Caused by Variants. Centers for Disease Control and Prevention. April 12, 2021. Accessed July 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-cases.html).
The total number of cases due to three new SARS-CoV-2 variants (B1.1.7, B.1.351, & P1) are shown (Data as of April 12, 2021).
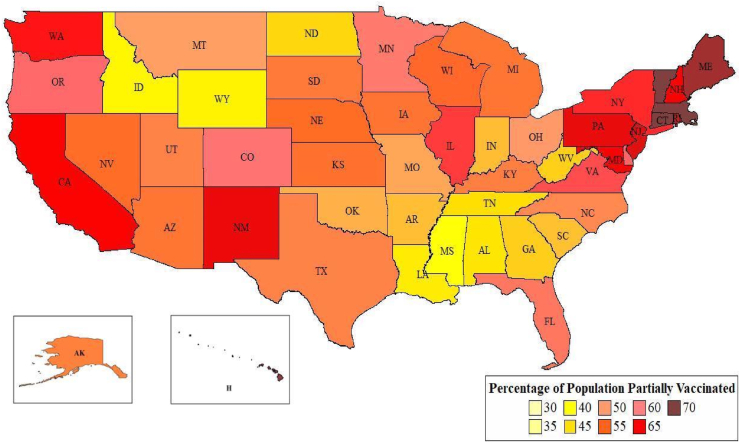
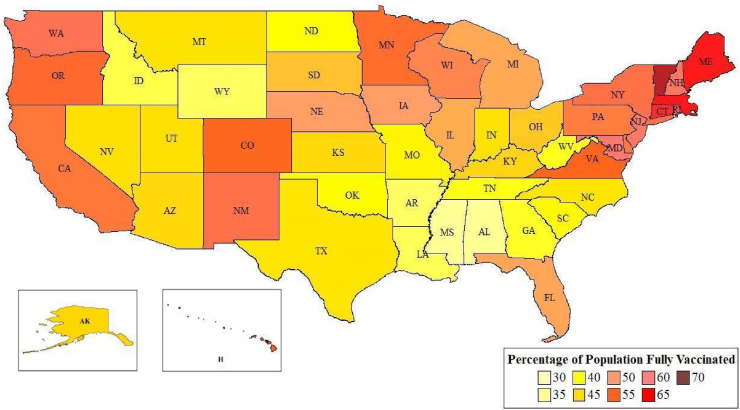
In addition to differences in variant distribution, there are differences in vaccination rates throughout the U.S. Fig. 2A and Fig. 2B demonstrate these geographic differences and highlight that few states have over 50% of their population fully vaccinated. This is concerning because receiving a single dose for vaccines which require two doses may not sufficiently protect against SARS-CoV-2 and its variants [9].
Fig. 2A.
Percentage of State Population Partially Vaccinated Against COVID-19 (Data as of August 4, 2021). Average percentage of the population partially vaccinated is 56.1%. Top five states with the highest percentage of their population partially vaccinated: Vermont, Massachusetts, Hawaii, Connecticut, and Maine. Bottom five states with the least percentage of their population partially vaccinated: Idaho, Louisiana, Wyoming, Alabama, and Mississippi. Data Source: U.S. COVID-19 Vaccine Tracker. Mayo Clinic. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker. Accessed August 4, 2021).
Fig. 2B.
Percentage of State Population Fully Vaccinated Against COVID-19 (Data as of August 4, 2021). Average percentage of the population fully vaccinated is 48.9%. Top five states with the highest percentage of their population fully vaccinated: Vermont, Massachusetts, Maine, Connecticut, Rhode Island. Bottom five states with the least percentage of their population fully vaccinated: Louisiana, Wyoming, Arkansas, Alabama, and Mississippi.
Data Source: U.S. COVID-19 Vaccine Tracker. Mayo Clinic. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker. Accessed August 4, 2021).
In the 5 states with the lowest vaccination rates, there was no clear relationship with the number of variant cases (Table 1A). However, only 2 of the 5 states with the highest vaccination rates exhibited high variant cases (401+), and the other 3 did not even feature in the top 15 states with the most variant cases (Table 1B). This suggests a correlation between high vaccination rates and a low frequency of variant cases. Although Massachusetts and Connecticut were exceptions, their percentage of population vaccinated has increased since the time the variant case numbers were acquired by 37.3% and 33.4%, respectively [10,11]. Another possible explanation as to why Massachusetts and Connecticut have a high number of variant cases despite high vaccination rates could be the time it has taken to vaccinate their population. While the mutation rate for SARS-CoV-2 viral strains is slow and vaccines are effective against variants [14,15], transmission occurs rapidly [12]. When transmission does occur, it often goes undetected, and mutations can occur in the time prior to vaccination [13]. Vaccination efforts must match or exceed transmission rates in order to avoid extensive mutations.
Table 1A.
Bottom 5 states with lowest percentage of population vaccinated and corresponding variant case numbers. Vaccination rate is reported as of July 20, 2021. Variant case numbers are reported as of April 12, 2021.
| Bottom 5 States | Vaccination Rate (% of population) | B.1.1.7 (alpha) | P1 | B.1.351 (beta) | Total Variants |
|---|---|---|---|---|---|
| Louisiana | 36.2 | 51 | 0 | 0 | 51 |
| Wyoming | 36 | 9 | 0 | 0 | 9 |
| Arkansas | 35.4 | 8 | 1 | 0 | 9 |
| Alabama | 33.74 | 186 | 0 | 2 | 188 |
| Mississippi | 33.8 | 147 | 3 | 1 | 151 |
Data Sources: U.S. COVID-19 Vaccine Tracker. Mayo Clinic. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker. Accessed July 20, 2021.
US COVID-19 Cases Caused by Variants. Centers for Disease Control and Prevention. April 12, 2021. Accessed July 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-cases.html.
Table 1B.
Top 5 states with highest percentage of population vaccinated and corresponding variant case numbers. Vaccination rate is reported as of July 20, 2021. Variant case numbers are reported as of April 12, 2021.
| Top 5 States | Vaccination Rate (% of population) | B.1.1.7 (alpha) | P1 | B.1.351 (beta) | Total Variants |
|---|---|---|---|---|---|
| Vermont | 67.0 | 56 | 0 | 0 | 56 |
| Massachusetts | 63.2 | 1100 | 102 | 12 | 1214 |
| Maine | 62.8 | 27 | 2 | 5 | 34 |
| Connecticut | 62.4 | 792 | 10 | 14 | 816 |
| Rhode Island | 60.5 | 25 | 1 | 0 | 26 |
Data Sources: U.S. COVID-19 Vaccine Tracker. Mayo Clinic. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker. Accessed July 20, 2021.
US COVID-19 Cases Caused by Variants. Centers for Disease Control and Prevention. April 12, 2021. Accessed July 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-cases.html.
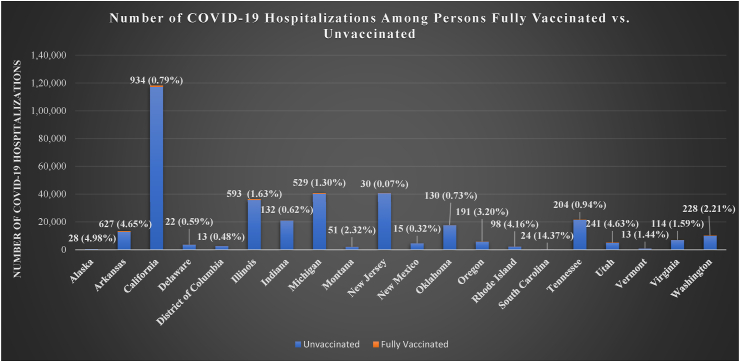
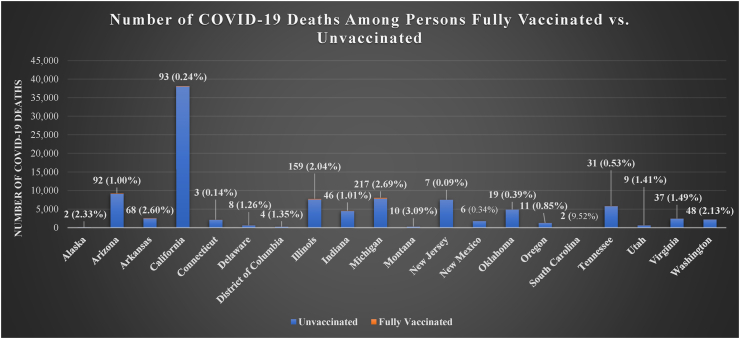
Moreover, current research indicates that vaccines are effective against current variants due to preserved neutralization by Pfizer and Moderna against emerging strains [14,15]. An article published on July 21, 2021 estimated that the two-dose Pfizer vaccine retains its effectiveness against the newly emerging Delta variant (88%) based on a test-negative case-control study [9]. Concurrently, a report of a breakout of Delta variant cases in a gymnastics facility in Oklahoma found that 85% of persons with outbreak-associated COVID-19 had not yet received a single dose of a COVID-19 vaccine [16]. In addition, it was reported that vaccinations reduce the number of cases, emergency department (ED) visits, hospital admissions (Fig. 3A), and fatalities (Fig. 3B) caused by SARS-CoV-2 overall [17]. This emphasizes the need to increase vaccinations, especially for vulnerable populations. However, variant cases are increasing in the U.S while vaccination rates are lagging.
Fig. 3A.
COVID-19 Hospitalizations Among Persons Fully Vaccinated vs. Unvaccinated.
The labeled numerical values refer to the number and percentage of the state's COVID-19 hospitalizations among persons who are fully vaccinated.
Data Source: Coronavirus Resource Center. Johns Hopkins University of Medicine. https://coronavirus.jhu.edu/map.html. Accessed August 4, 2021.
Kates, J et al. COVID-19 Vaccine Breakthrough Cases: Data from the States. July 30, 2021. https://www.kff.org/policy-watch/covid-19-vaccine-breakthrough-cases-data-from-the-states/. Accessed August 4, 2021.
Fig. 3B.
COVID-19 Deaths Among Persons Fully Vaccinated vs. Unvaccinated.
The labeled numerical values refer to the number and percentage of the state's COVID-19 deaths among persons who are fully vaccinated.
Data Source: Coronavirus Resource Center. Johns Hopkins University of Medicine. https://coronavirus.jhu.edu/map.html. Accessed August 4, 2021.
Kates J. et al. COVID-19 Vaccine Breakthrough Cases: Data from the States. July 30, 2021. https://www.kff.org/policy-watch/covid-19-vaccine-breakthrough-cases-data-from-the-states/. Accessed August 4, 2021.
In the current era that is governed by technology, it is not uncommon for misinformation to spread across multiple websites and make several false claims pertaining to the efficacy of vaccines against the Delta variant [18]. However, they often do not include properly cited evidence-based studies, whereas the entities advocating for vaccinations are based on evidence. For example, a SARS-CoV-2 microneutralization assay was recently developed in Israel to test the neutralization capacity of variants of concern in two cohorts of healthcare workers (HCW). After testing serum samples collected from one cohort of 19 HCW, they found a two-fold reduction in neutralization of the Delta variant compared to the original virus in vaccinated persons [19]. The other cohort consisting of 15 HCW was tested against the original virus and variants Alpha, Beta and Gamma, also showing decreased neutralization. Nevertheless, it was still concluded that the Pfizer-BioNTech vaccine retains protection against the Delta strain and other variants of concern, as well as their associated complications.
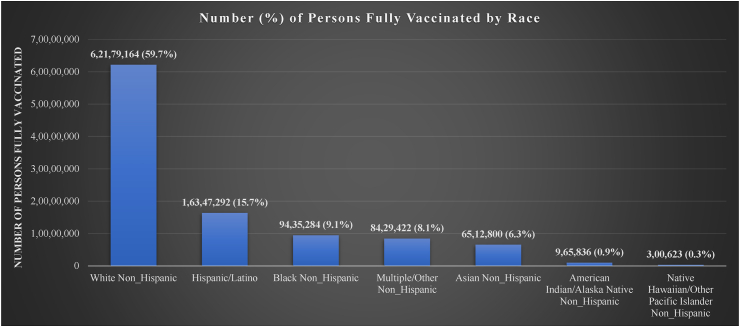
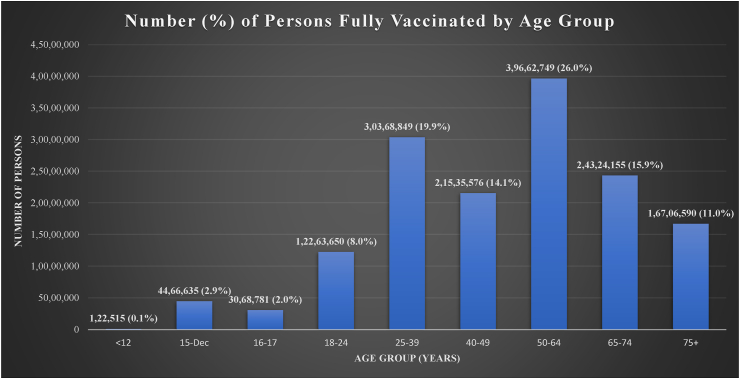
According to the CDC, the highest vaccination rates are currently among the white, non-Hispanic population. Racial minority groups have shown the lowest rates of vaccination (Fig. 4A), as well as a disproportionately high number of COVID-19-related hospitalizations and deaths [20]. Current vaccination rates among the U.S population also vary by age, with individuals aged 50–64 making up the highest proportion of the vaccinated population while those under 25 are a much smaller proportion of the vaccinated population (Fig. 4B) [21,22]. To combat these low rates we must focus on reducing barriers to access and vaccine hesitancy [23]. Vaccine hesitancy in particular has been exacerbated by disinformation on social media platforms and statements lacking scientific evidence [18]. It is crucial to increase the monitoring of social-media platforms to swiftly detect and correct disinformation [24].
Fig. 4A.
Comparison of the Number of Persons who are Fully Vaccinated, by Race. Reported as the number of fully vaccinated individuals in each racial group and percentage of all persons who are fully vaccinated. (Data Source: Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic. Accessed August 4, 2021).
Fig. 4B.
Comparison of the Number of Persons who are Fully Vaccinated, by Age Group. Reported as the number of fully vaccinated individuals in each racial group and percentage of all persons who are fully vaccinated. (Data Source: Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic. Accessed August 4, 2021).
While current COVID-19 vaccines are effective against recent variants, continued viral transmission may lead to the emergence of resistant strains [25]. Increased variant transmission and sudden spikes in COVID-19 infections may lead to an increase in hospitalizations, emergency department visits, intensive care unit utilization, thus depleting hospital resources and potentially overwhelming healthcare systems [26]. This could further reduce medical supply stocks and result in the shortage of medications and blood bank products [27,28]. Moreover, considerable financial strain has been placed on the healthcare system, compounded by the cost of reducing elective surgeries and financial impact inflicted by the pandemic [29,30]. Vaccines have been shown to be highly effective, as only 2.6% of fully vaccinated HCWs (a very high risk group) have contracted a breakthrough COVID case [31]. Thus, encouraging and increasing access to vaccinations in HCWs and populations with low vaccination rates may be an avenue to pursue. For example, as of August 4, 2021, children <18 years old only comprise only 5% of all fully vaccinated individuals, whereas vaccination rates in all adult age groups are many magnitudes greater (Fig. 4B). In addition, from July 22–29, 2021, children comprised 19% of the weekly COVID cases [32]. In a span of 2 weeks, the percentage of pediatric COVID-19 cases increased by 3% [32]. It is likely that the low vaccination rates observed in children plays a role in the increase in the percentage of COVID cases occupied by children [32].
There needs to be stronger emphasis on decreasing disparities in vaccination rates and combatting the amount of misinformation circulating online. Public health and medical institutions/healthcare systems must avoid being only reactive to ongoing COVID-19 surges and instead take proactive approaches going forward in order to prevent the imminent collapse of health care systems and move steadily towards sustainable mitigation and preventive strategies to end the COVID-19 pandemic [33]. These approaches include, but are not limited to: significantly increasing vaccination rates among healthcare workers and patients, effective marketing and community outreach strategies that highlight vaccination benefits, clearly illustrating morbidities and mortalities associated with COVID-19 infections, and doing so by utilizing balanced educational initiatives that consider varying socioeconomic and literacy levels of communities. Then and only then will we be able to successfully fight misinformation related to the COVID-19 vaccines, and eventually increase vaccination rates in these communities.
Funding
None.
Ethical approval
Not applicable.
Sources of funding
None.
Author contribution
Author contributions: Study design and conception: AE, Data collection, interpretation and analysis: SA, AE, BS, MM, Manuscript preparation: SA, BS, AE, MM, Critical revision of manuscript: SA, AE, BS, MM, All authors read and approved the final manuscript.
Research registration Unique Identifying number (UIN)
-
1.
Name of the registry:
-
2.
Unique Identifying number or registration ID:
-
3.
Hyperlink to the registration (must be publicly accessible):
Not applicable.
Guarantor
Adel Elkbuli, Mark McKenney.
Declaration of competing interest
Authors disclose no competing interest.
References
- 1.COVID-19 Vaccinations in the United States. Center for Disease Control and Prevention; 2021. https://covid.cdc.gov/covid-data-tracker/#vaccinations [Google Scholar]
- 2.U.S. COVID-19 vaccine tracker: See Your State’s Progress. Mayo Clinic; 2021. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker [Google Scholar]
- 3.Herd Immunity and COVID-19 (Coronavirus): what You Need to Know. Mayo Clinic; June 9, 2021. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/herd-immunity-and-coronavirus/art-20486808 Accessed on July 20th, 2021. [Google Scholar]
- 4.Callaway E. Delta coronavirus variant: scientists brace for impact. Nature (London) 2021;595(7865):17–18. doi: 10.1038/d41586-021-01696-3. [DOI] [PubMed] [Google Scholar]
- 5.SARS-CoV-2 variant classifications and definitions. Center for Disease Control and Prevention. 2021 https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html [Google Scholar]
- 6.Zeyaullah M., AlShahrani A.M., Muzammil K. COVID-19 and SARS-CoV-2 variants: current challenges and health concern. Front. Genet. 2021;12:693916. doi: 10.3389/fgene.2021.693916. https://search.proquest.com/docview/2548401488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US COVID-19 Cases Caused by Variants. Center for Disease Control and Prevention; April 12, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-cases.html Accessed July 20th, 2021. [Google Scholar]
- 8.Estimated Proportions of SARS-CoV-2 Lineages. Center for Disease Control and Prevention; August 3, 2021. https://covid.cdc.gov/covid-data-tracker/#variant-proportions Accessed August 4th, 2021. [Google Scholar]
- 9.Lopez Bernal J., Andrews N., Gower C. Effectiveness of covid-19 vaccines against the B.1.617.2 (delta) variant. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2108891. [DOI] [PubMed] [Google Scholar]
- 10.Daily COVID-19 Vaccine Report. Massachusetts Department of Public Health; April 12, 2021. https://www.mass.gov/doc/daily-covid-19-vaccine-report-april-12-2021/download Accessed July 20th, 2021. [Google Scholar]
- 11.Governor Lamont Provides Update on Connecticut's Coronavirus Response Efforts. Office. Governor. Ned Lamont.; April 15, 2021. https://portal.ct.gov/Office-of-the-Governor/News/Press-Releases/2021/04-2021/Governor-Lamont-Coronavirus-Update-April-15 Accessed July 20th, 2021. [Google Scholar]
- 12.Dearlove B., Lewitus E., Bai H. A SARS-CoV-2 vaccine candidate would likely match all currently circulating variants. Proceedings of the National Academy of Sciences - PNAS. 2020;117(38):23652–23662. doi: 10.1073/pnas.2008281117. https://www.ncbi.nlm.nih.gov/pubmed/32868447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weisblum Y., Schmidt F., Zhang F. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. eLife. 2020;9 doi: 10.7554/elife.61312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.mRNA-1273 COVID-19 Vaccine Effectiveness against the B.1.1.7 and B.1.351 Variants and Severe COVID-19 Disease in qatar. Nature Medicine; 2021. https://search.proquest.com/docview/2550264733 [DOI] [PubMed] [Google Scholar]
- 15.Abu-Raddad L.J., Chemaitelly H., Butt A.A. Effectiveness of the BNT162b2 covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N. Engl. J. Med. 2021;385(2):187–189. doi: 10.1056/NEJMc2104974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dougherty K., Mannell M., Naqvi O., Matson D., Stone J. SARS-CoV-2 B.1.617.2 (Delta) variant COVID-19 outbreak associated with a gymnastics facility — Oklahoma, April–May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1004–1007. doi: 10.15585/mmwr.mm7028e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roest S., Hoek R.A.S., Manintveld O.C., Barda N., Dagan N., Balicer R.D. BNT162b2 mRNA covid-19 vaccine in a nationwide mass vaccination setting. N. Engl. J. Med. 2021;384(20):1968–1970. doi: 10.1056/NEJMc2104281. [DOI] [PubMed] [Google Scholar]
- 18.Gill S., Kinslow K., Mckenney M., Elkbuli A. Twitter and the credibility of disseminated medical information during the COVID-19 pandemic. Am. Surg. 2020;87(5):705. doi: 10.1177/0003134820973391. [DOI] [PubMed] [Google Scholar]
- 19.Lustig Y., Zuckerman N., Nemet I. Neutralising capacity against Delta (B.1.617.2) and other variants of concern following Comirnaty (BNT162b2, BioNTech/Pfizer) vaccination in health care workers. Israel. Euro Surveill. 2021;26(26) doi: 10.2807/1560-7917.ES.2021.26.26.2100557. 10.2807/1560-7917.ES.2021.26.26.2100557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boserup B., McKenney M., Elkbuli A. Disproportionate impact of COVID-19 pandemic on racial and ethnic minorities. Am. Surg. 2020;86(12):1615–1622. doi: 10.1177/0003134820973356. https://journals.sagepub.com/doi/full/10.1177/0003134820973356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demographic Characteristics of People Receiving COVID-19 Vaccinations in the united states. Center for Disease Control and Prevention; 2021. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic Accessed August 4. [Google Scholar]
- 22.COVID-19 Vaccines for Children and Teens. Center for Disease Control and Prevention; 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/adolescents.html Accessed July 20th. [Google Scholar]
- 23.Unintended consequences of COVID-19 mitigation strategies. Centers for disease control and prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-impact.html December 10. Accessed July 20th, 2021.
- 24.Rosenberg H., Syed S., Rezaie S. The twitter pandemic: the critical role of twitter in the dissemination of medical information and misinformation during the COVID-19 pandemic. CJEM. 2020;22(4):418–421. doi: 10.1017/cem.2020.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.New Variants of Coronavirus: what You Should Know. John Hopkins Medicine; 2021. https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/a-new-strain-of-coronavirus-what-you-should-know Accessed July 23th. [Google Scholar]
- 26.Sen-Crowe B., Sutherland M., McKenney M., Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J. Surg. Res. 2021;260:56–63. doi: 10.1016/j.jss.2020.11.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sen-Crowe B., McKenney K., McKenney M., Elkbuli A. Challenges associated with blood banks and blood donations during the COVID-19 pandemic. Am. J. Emerg. Med. 2021;43:281–282. doi: 10.1016/j.ajem.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sen-Crowe B., McKenney M., Elkbuli A. Medication shortages during the COVID-19 pandemic: saving more than COVID lives. Am. J. Emerg. Med. 2021;45:557–559. doi: 10.1016/j.ajem.2020.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ehrlich H., Sen-Crowe B., McKenney M., Elkbuli A. Trends in top cancer diagnosis and challenges related to COVID-19 pandemic. Am. Surg. 2020;86(11):1515–1517. doi: 10.1177/0003134820949522. [DOI] [PubMed] [Google Scholar]
- 30.Boserup B., McKenney M., Elkbuli A. The financial strain placed on America's hospitals in the wake of the COVID-19 pandemic. Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bergwerk M., Gonen T., Lustig Y. Covid-19 breakthrough infections in vaccinated health care workers [published online ahead of print, 2021 jul 28] N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2109072. 10.1056/NEJMoa2109072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Children and COVID-19: State Data Report. American Academy of Pediatrics; July 29, 2021. https://downloads.aap.org/AAP/PDF/AAP%20and%20CHA%20-%20Children%20and%20COVID-19%20State%20Data%20Report%207.29%20FINAL.pdf [Google Scholar]
- 33.Elkbuli A., Herrera M., Awan M., Elassad C. Striving towards an effective emergency preparedness and disaster management response: lessons learned and future directions [published online ahead of print, 2021 Mar 15] Am. J. Emerg. Med. 2021;S0735–6757(21) doi: 10.1016/j.ajem.2021.03.036. 00221-00227. [DOI] [PMC free article] [PubMed] [Google Scholar]