Abstract
The patellar tendon is an integral part of the knee extensor mechanism and has been historically described as a single tendon. A doubled patellar tendon is an exceedingly rare finding. We present a case of a crossed doubled patellar tendon in a 70-year-old male with a history of right knee pain, which to our knowledge has only been reported once before in the literature. The presence of a doubled patellar tendon has a potential influence on surgical planning and in the etiology of anterior knee pain.
Keywords: Knee, Cross over, Patella tendon, Anatomical variant
Introduction
The patellar tendon is an integral part of the knee extensor mechanism, transmitting force generated by the quadriceps muscles onto the tibia, using the patella as a fulcrum. The patellar tendon originates from the anterior aspect of the distal end of the patella, coursing anterior to the knee joint, and inserts on the tibial tuberosity. It consists of bands of collagenous, fibrous connective tissue aligned parallel to the longitudinal axis and is surrounded by a tendon sheath which is composed of extracellular matrix [1].
The patellar tendon is typically described as a single, straight tendon with parallel tendon fibers. Doubled patellar tendons have only been reported twice before, one with crossed and the other with uncrossed anatomy [2,3]. Here we present a second case of crossed double patellar tendon, and discuss its anatomy, embryology and potential clinical implications.
Case report
The patient is a 70-year-old male with hypertension and knee pain and no prior history of knee surgery or trauma. There was no other contributory medical history.
MRI imaging of the right knee without contrast using a standard MRI imaging protocol of coronal T1 and fat suppressed FSE T2 weighted images, sagittal proton density (PD) and fat suppressed FSE T2 weighted images, and axial fat suppressed FSE T2 weighted images, performed using a 1.5 Tesla General Electric scanner with a flexible knee coil. Images revealed 2 patella tendons, both originating from the inferior patella, with the deep bundle positioned slightly lateral to the superficial bundle. The deep bundle crosses the superficial bundle as it courses inferomedially towards the tibial tuberosity, and the superficial bundle coursing inferolaterally to the tibial tuberosity (Fig. 1). Sagittal images depict two distinct bundles, with the superficial bundle coursing inferiorly from the lower pole of the patella with some contribution from the distal rectus femoris tendon, and the deeper bundle originating from the lower pole of the patella coursing deep to the superficial bundle (Fig. 2). There was no evidence of patella tendinosis or tear. Of note, there was one patella with a Wiberg type B morphology (small medial and larger lateral facet), and no evidence of duplicated patella or patella hypoplasia/aplasia. There was also no trochlea hypoplasia or dysplasia and no patellar maltracking. There was tricompartmental osteoarthritis worse in the medial compartment with no disproportionate patellofemoral chondrosis, and there was a degenerative tear of the medial meniscus, likely accounting for the patient's presenting pain.
Fig. 1.
Sequential (proximal to distal) axial fat suppressed T2 weighted images starting at the femoral condyle (a) reveals two distinct patellar tendons coursing inferiorly towards the tibial tuberosity (e). The deeper component originates slightly lateral to the superficial tendon, crossing the superficial tendon and inserting at the tibial tuberosity medial to the superficial tendon (a-e).
Fig. 2.
Sagittal fat suppressed T2 weighted images demonstrates two separate patellar tendons. The superficial bundle appears as an extension of the rectus femoris tendon. The second bundle is positioned deep to the superficial bundle, coursing from the patella to the tibial tuberosity (a,b).
Discussion
The patellar tendon is a flattened, band-like structure that connects the inferior aspect of the patella, a large triangular sesamoid bone located at the anterior knee joint, to the tibial tuberosity [1]. It serves primarily as a ligament, though it is often referred to as a tendon since part of its fibers is a continuation of the rectus femoris tendon. Its patella attachment site is wider compared to the tibia attachment site, and the fibers converge and narrow before inserting into the superior tip of the tibial tuberosity [4].
In two-thirds of the population, the patellar tendon attaches to the anterior distal two-thirds of the patella as in this case; however, in one-third of the population, the tendon originates from the posterior aspect of the distal patella [4]. In the sagittal plane, the patellar tendon fascicules are aligned in parallel. It is thin and broad proximally and becomes thick and narrow distally as fascicules converge toward their tibial attachment site [5]. The patella itself also has variations, with its distal inferior pole appearing in either a pointed or blunt configuration. The blunt variant is associated with longer patellar tendon fibers attaching at the anterior surface and shorter fibers at the posterior surface. Shorter posterior fibers may result in disproportionate elongation of the anterior tendon fibers during knee flexion, contributing to tears during knee injuries and the development of tendinosis [4]. Patella variations in the patellar length, articulation surface length, and the length of the patellar tendon also occur [6].
Examination of the embryological development of the patella and patellar tendon may provide insights into the sequence of events that led to the formation of a doubled patellar tendon. During the prenatal period, the quadriceps tendon, patellar ligament, and the patella appear together as a complex band of fibrous connective tissue spanning the anterior aspect of the knee [1]. The patellar ligament becomes visible around 7 weeks of gestation. At 9 weeks, the patellar ligament can be identified and is seen as part of the quadriceps tendon extending across the superficial aspect of the patella to attach to the upper epiphysis of the tibia [7,8]. As gestational age increases, the mean length of the patellar ligament increases on average from 3.48 mm initially to 17.45 mm. The proximal and distal widths increase as well, though disproportionately, with a larger increase in the proximal width compared to the distal width [9]. The tendons continue to mature and the organization of the knee joint ligaments is complete by week 13 [7]. As for the development of the patella, some models have proposed that it develops within that initial band of connective tissue in response to the mechanical signals generated by the attached tendons, and becomes completely cartilaginous by 14 weeks of gestation [1,10]. Other research models have proposed that the patella develops as an extension of the femur not associated with the tendon structures and is signaled by the TGFβ and BMP4 molecular pathways, and only later becomes fused with the quadriceps tendon, leading to the formation of the patellar ligament [10].
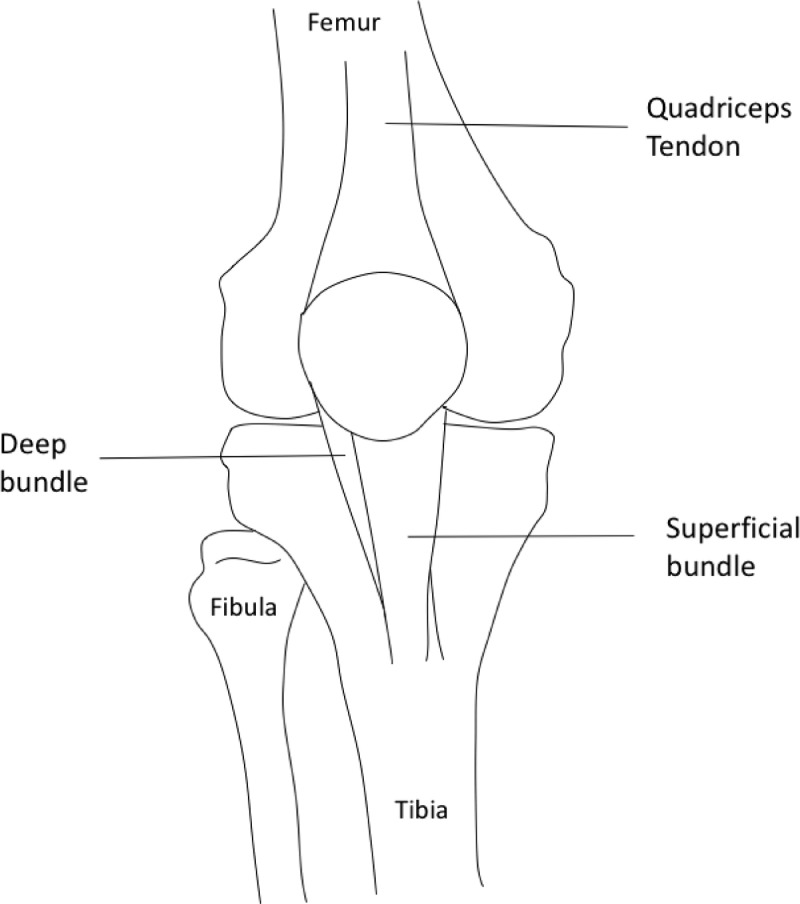
The formation of a doubled patellar tendon may be explained by a change during one of the embryological developmental events described above. Aberrant molecular signaling is one possible etiology in which a slight change in the signaling pathway might have caused the formation of two different patellar ligament attachment sites during the development of the patella. Tears in the patellar tendon due to injuries during development is another possible mechanism that might have led to the formation of two distinct crossed patellar ligaments (Fig. 3).
Fig. 3.
Illustration of the crossed doubled patellar tendon of the right knee. Note the origin of the deep bundle more lateral to the superficial bundle.
MRI is a commonly used imaging modality to assess for knee pathology, and a varying imaging appearance of the patellar tendon has been reported. In a normal MRI of the knee joint, the patellar tendon appears as a low-intensity band on all pulse sequences, with well-defined margins. It is flattened proximally and assumes a semilunar convexity distally as it approaches the tibia attachment site. Buckling of the tendon during knee extension may alter the signal intensity at multiple foci, partly due to magic angle effect [4]. Magic angle effect is an artifact that results in high signal intensity at variable positions within tendons or articular cartilage during short TE sequences, e.g. T1 and PD sequences, due to spin-spin interactions between protons at different angles when the tendon is approximately 55 degrees to the main magnetic field [11]. The artifact disappears on long TE sequences. Joint effusions and anterior cruciate ligament tears may also result in similar buckling and secondarily affect signal intensity [12].
Despite the subtle variations in the anatomical and MRI presentations of the patellar tendon, the patellar tendon has important clinical applications, one of which is the reconstruction of the anterior cruciate ligament (ACL) [2,13]. Approximately 300,000 ACL reconstructions are performed in the U.S. annually. Bone patellar tendon bone (BPTB) autograft has often been used for ACL reconstruction and has demonstrated excellent clinical results, low failure rates, and high patient satisfaction. It is considered the “gold standard”, superior to synthetic grafts [13]. During reconstruction, the central one-third of the native patellar tendon is often removed and used as the graft. However, postoperative morbidities such as anterior knee pain, patellar tendon tear, patellar fracture, and possible graft mismatch exist [14]. A doubled patellar tendon may potentially have surgical implications in ACL reconstruction surgeries, given the presence of two independent tendons, although more data is needed regarding its application and possible post-operative complications.
Interestingly, the two previously reported doubled patellar tendon cases by Haydar et al and Loizides et al are both associated with knee pain, either subacute or chronic in nature [2,3]. A potential contribution of the doubled patellar tendon to the pathology of knee pain remains a possibility, though confounding factors exist. Wang K et al demonstrated in their study that during knee flexion and slow and fast walking, the central proximal posterior region of the patellar tendon experienced the highest strain and stress, followed by the central distal posterior, central distal anterior, and central proximal anterior regions. The higher loading stress at the central proximal posterior region also corresponds to a higher incidence of tendinopathy at that site (jumper's knee) [15]. The anatomical structure of a doubled patellar tendon differs from that of a single patellar tendon, which likely results in a different magnitude and location of loading stress and strain as compared to those demonstrated by Wang K et al. The influence of a doubled patellar tendon on patella tendinopathy and internal derangement as a result of altered mechanics is currently unknown and requires further investigation.
Conclusion
While normal anatomical and MRI variants of the patella and patellar tendon are well documented in the literature, a doubled patellar tendon is an exceedingly rare finding that should be noted on routine imaging and during pre-operative planning [2,3]. With the report of two cases of doubled patellar tendon by Loizide et al and Haydar et al only within the last 5 years, the existence of a doubled patellar tendon might be under recognized and/or more common than originally reported, and its potential contribution to chronic knee pain remains a possibility.
Patient consent
Informed consent has been obtained from the patient for publication of his case.
Footnotes
Competing interests: The authors declare that they have no conflict of interest.
References
- 1.Fox AJ, Wanivenhaus F, Rodeo SA. The basic science of the patella: structure, composition, and function. J Knee Surg. 2012;25(2):127–141. doi: 10.1055/s-0032-1313741. May. [DOI] [PubMed] [Google Scholar]
- 2.Loizides A, Messina C, Glodny B. A case of crossed-doubled patellar tendon: an atavistic variant, simple mutation or pathologic finding? Surg Radiol Anat. 2017;39(1):111–114. doi: 10.1007/s00276-016-1706-x. Published online 2016 Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haydar SMA, Miles J, Hargunani R. The uncrossed-doubled patellar tendon: A novel imaging finding. Radiol Case Rep. 2019;14(12):1509–1512. doi: 10.1016/j.radcr.2019.09.029. DecPublished online 2019 Oct 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flores DV, Gómez CM, Pathria MN. Layered Approach to the Anterior Knee: Normal Anatomy and Disorders Associated with Anterior Knee Pain. Radiographics. Nov-Dec 2018;38(7):2069–2101. doi: 10.1148/rg.2018180048. [DOI] [PubMed] [Google Scholar]
- 5.Basso O, Johnson DP, Amis AA. The anatomy of the patellar tendon. Knee Surg Sports Traumatol Arthrosc. 2001;9(1):2–5. doi: 10.1007/s001670000133. [DOI] [PubMed] [Google Scholar]
- 6.Grelsamer RP, Proctor CS, Bazos AN. Evaluation of patellar shape in the sagittal plane. A clinical analysis. Am J Sports Med. Jan-Feb 1994;22(1):61–66. doi: 10.1177/036354659402200111. [DOI] [PubMed] [Google Scholar]
- 7.Mérida-Velasco JA, Sánchez-Montesinos I, Espín-Ferra J. Development of the human knee joint ligaments. Anat Rec. 1997;248(2):259–268. doi: 10.1002/(SICI)1097-0185(199706)248:2<259::AID-AR13>3.0.CO;2-O. Jun. [DOI] [PubMed] [Google Scholar]
- 8.Gardner E, O'Rahilly R. The early development of the knee joint in staged human embryos. J Anat. 1968 Jan; 102;(Pt 2):289–299. [PMC free article] [PubMed] [Google Scholar]
- 9.Koyuncu E, Cankara N, Sulak O. The morphometry of patella and patellar ligament during the fetal period. Clinical Anatomy. 2011;24(2):225–231. doi: 10.1002/ca.21075. Mar. [DOI] [PubMed] [Google Scholar]
- 10.Eyal S, Blitz E, Scwartz Y. On the development of the patella. Development. 2015;142(10):1831–1839. doi: 10.1242/dev.121970.11. May 15. [DOI] [PubMed] [Google Scholar]
- 11.Harantanas AH, Zibis AH, Papanikolaou N. Increased signal intensity on fat-suppressed three-dimensional T1-weighted pulse sequences in patellar tendon: magic angle effect? Skeletal Radiol. 2001;30(2):67–71. doi: 10.1007/s002560000307. Feb. [DOI] [PubMed] [Google Scholar]
- 12.Schweitzer ME, Mitchell DG, Ehrlich SM. The patellar tendon: thickening, internal signal buckling, and other MR variants. Skeletal Radiol. 1993;22(6):411–416. doi: 10.1007/BF00538442. Aug. [DOI] [PubMed] [Google Scholar]
- 13.Dhammi IK, Rehan-UI-Haq Kumar S. Graft choices for anterior cruciate ligament reconstruction. Indian J Orthop. 2015;49(2):127–128. doi: 10.4103/0019-5413.152393. Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frank RM, Higgins J, Bernardoni E. Anterior Cruciate Ligament Reconstruction Basics: Bone-Patellar Tendon-Bone Autograft Harvest. Arthrosc Tech. 2017;6(4):e1189–e1194. doi: 10.1016/j.eats.2017.04.006. AugPublished online 2017 Jul 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang K, Hosseinnejad SH, Jabran A. A biomechanical analysis of 3D stress and strain patterns in patellar tendon during knee flexion. Int J Numer Method Biomed Eng. 2020;36(9):e3379. doi: 10.1002/cnm.3379. Sep. [DOI] [PubMed] [Google Scholar]