Abstract
Background
Multidimensional Prognostic Index (MPI) is recognized as a prognostic tool in hospitalized patients, but data on the value of MPI in community-dwelling older persons are limited. Using data from a representative cohort of community-dwelling persons, we tested the hypothesis that MPI explains mortality during 15 years of follow-up.
Methods
A standardized comprehensive geriatric assessment was used to calculate the MPI and to categorize participants in low-, moderate-, and high-risk classes. The results were reported as hazard ratios (HRs) and the accuracy was evaluated with the area under the curve (AUC), with 95% confidence intervals (CIs) and the C-index. We also reported the median survival time by standard age groups.
Results
All 1453 participants (mean age 68.9 years, women = 55.8%) enrolled in the InCHIANTI study at baseline were included. Compared to low-risk group, participants in moderate (HR = 2.10; 95% CI: 1.73–2.55) and high-risk MPI group (HR = 4.94; 95% CI: 3.91–6.24) had significantly higher mortality risk. The C-index of the model containing age, sex, and MPI was 82.1, indicating a very good accuracy of this model in explaining mortality. Additionally, the time-dependent AUC indicated that the accuracy of the model incorporating MPI to age and sex was excellent (>85.0) during the whole follow-up period. Compared to participants in the low-risk MPI group across different age groups, those in moderate- and high-risk groups survived 2.9–7.0 years less and 4.3–8.9 years less, respectively.
Conclusions
In community-dwelling individuals, higher MPI values are associated with higher risk of all-cause mortality with a dose–response effect.
Keywords: InCHIANTI, Mortality, Multidimensional prognostic index, Prognosis
In geriatric medicine, increasing attention is given to the development of tools that can explain mortality or other adverse health outcomes. Information provided by these tools can greatly help in clinical decision making on alternative therapeutics choices, particularly in frail older persons (1). A limited number of prognostic tools for geriatric patients meet the requirements of accuracy and calibration required to be used in clinical practice (2,3).
The Comprehensive Geriatric Assessment (CGA) that explores multiple domains of health is generally considered an effective tool to stratify the prognosis of older patients (4). The Multidimensional Prognostic Index (MPI) is a product of the CGA, which uses a mathematic algorithm including information about 8 domains: functional status as assessed by basal and instrumental activities of daily living (IADL), cognitive status, nutritional status, mobility, multi-morbidity, polypharmacy, and cohabitation status (5,6). Multidimensional Prognostic Index is generally considered a well-calibrated tool with good discrimination accuracy for both short- and long-term mortality and other adverse health outcomes (7,8). Multidimensional Prognostic Index is derived from information on health, functional, cognitive, and nutritional domains, as well as cohabitation status, using standardized and extensively validated rating assessment tools that are often well known and routinely used by clinicians (3). There is strong evidence that the MPI explains mortality in hospitalized older patients (7–15). There is also some initial evidence that the MPI provides information on the risk of new hospitalization, days spent in the hospital, and the risk of mortality in community-dwelling older persons (16). However, the value of the MPI has not been tested in a cohort representative of the general population with adequate follow-up.
Here, we tested the hypothesis that the MPI explains mortality in the community-dwelling older persons who participated in the “Invecchiare in Chianti” (ie, Aging in the Chianti area; InCHIANTI) study, a population-based cohort study of adults conducted in 2 municipalities of Tuscany, Italy. InCHIANTI is the ideal setting for this analysis because it was conducted in a representative population, with a high response rate and collected all the data required for the calculation of the MPI (17,18).
Given this background, the aim of this study was to evaluate whether the implementation of the CGA-based MPI in the InCHIANTI study setting could be useful to identify different mortality risk groups of people during 15 years of follow-up.
Materials and Methods
Study Sample
The InCHIANTI study is an ongoing prospective population-based cohort study among adults (age range 20–102 years) living in Tuscany, Italy. In 1998, participants were randomly selected from the population living in the 2 municipalities of Greve in Chianti and Bagno a Ripoli. The data collection included a home interview and clinical measurements at the study clinic. Other details on the sampling and design of InCHIANTI have been published in previous work (19), and they are available at http://inchiantistudy.net/wp/lo-studio/.
Briefly, for the aims of this work, we considered as baseline evaluation made in 1998–2000 a total of 1453 participants, with 1155 (79.5%) aging more than 65 years. Follow-up measurements were then conducted every 3 years. At the last evaluation, 900 participants were included, but it was possible to evaluate the MPI only for 877 participants due to the presence of missing data.
The InCHIANTI study was approved by the ethical committee of the Italian National Institute of Research and Care on Aging. All study participants provided written informed consent.
Multidimensional Prognostic Index
The MPI was calculated as established in previous studies (6), with some minor modification based on available information in the InCHIANTI study (Supplementary Table 1):
Functional status was evaluated by Activities of Daily Living (ADL) index (20), which defines the level of dependence/independence in 6 daily personal care activities (bathing, toileting, feeding, dressing, urine and bowel continence, and transferring [in and out of bed or chair]).
Independence in the IADL (21), which assesses independence in 8 activities that are more cognitively and physically demanding than ADL, that is, managing finances, using the telephone, taking medications, shopping, using transportation, preparing meals, doing housework, and washing.
Cognitive status through the Mini-Mental State Examination (MMSE) (22), a 30-item questionnaire investigating different domains of cognition.
Comorbidity was examined using the Charlson Comorbidity Index (23).
Nutritional status was investigated with the Mini Nutritional Assessment—short form (24).
Participant’s level of mobility, assessed as the ability to get in and out of bed/chair, walk, and go up and down the stairs. The ability to do these activities was categorized as yes (1 point) or no (0 point).
The number of medications regularly taken by the participant.
The cohabitation status was assessed by a questionnaire and coded as, that is, living alone, living in a residential facility, or living with a family member.
For each domain, a tripartite hierarchy was used, with a score of 0 indicating no problems, 0.5 minor problems, and 1.0 major problems. This scoring is based on the literature for the specific instrument. The optimal location of cutoff points was determined using an optimization algorithm in which the optimal points were defined as the ones with the most significant (likelihood ratio test or log-rank test) split, that is, the ones that maximize the difference among the groups respect to their mean survival probability (25). The sum of these 8 domains was then divided by 8 in order to obtain a final MPI-InCHIANTI risk score, ranging from 0 (no risk) to 1 (high risk). Moreover, as for the individual covariates that explore each domain, also MPI-InCHIANTI was categorized into 3 different risk groups: MPI-1 low risk 0.00–0.25, MPI-2 moderate risk 0.26–0.50, and MPI-3 severe risk 0.51–1.00.
Vital Status
Vital status, date of death, and cause of death were retrieved from regional and municipality registers, through administrative data.
Statistical Methods
Time to event was defined as the time from baseline to death; otherwise, the patient was considered censored at the last contact. Descriptive statistics were presented as means and standard deviations (SDs) for quantitative measures and as percentages for all categorical variables. Univariate tests were performed to explore the association between each variable and death. Kaplan–Meier estimator was used to explore 15-year mortality rates across MPI risk groups and a statistical comparison across groups was performed by the long-rank test. Hazard ratios (HRs) related to MPI as both continuous (as an increase in 0.1 points) and categorical variables were obtained by fitting a “2-stage” model in order to adjust the estimate for the longitudinal trajectory of MPI during the follow-up period. In the first stage, the longitudinal trajectory of MPI was modeled by a Mixed Model with random intercept and slopes including time from baseline, age, and sex for each patient. The estimated value of MPI for each participant at each time point was estimated by the first stage and then these values were used in the second stage in a Cox model as time-varying covariates, adjusting for age and sex. The performance was estimated by using the time-dependent AUCs at different cutoff (3, 6, 9, 12, and 15 years from the baseline) while the overall capability was measured by using the Harrell’s C-index and relative 95% confidence interval (CI). The improvement due to the addition of MPI in a model with age and sex only was tested by the comparison of C-indexes. Median time to death for moderate and high MPI risk groups and 95% CIs were calculated, in comparison to the MPI low-risk group using Laplace regression (26), adjusted for age and gender. All analyses were stratified by widely known cutoffs for defining older age (<65, 65–74, 75–84, and ≥85 years). All tests were 2-tailed, with an I-type error set at 0.05. The analysis was performed using STATA software (Stata Corp LP, College Station, TX).
Results
Baseline Characteristics
The study population included 1453 participants (mean age 68.9 years, women = 55.8%) who participated in the InCHIANTI study.
Table 1 presents the baseline characteristics of the included participants, by vital status during 15 years of follow-up. As expected, participants who died during the 15-year follow-up (681; 46.9% of the baseline population) were significantly older, reported more disability in ADL and IADL, were more likely to have lower MMSE scores, consumed more medications, and had more severe multi-morbidity than those who remained alive (p < .001 for all comparisons; Table 1).
Table 1.
Descriptive Characteristics by Survival Status at 15 Years in the InCHIANTI Study
| Overall | Death at 15 Years | ||||
|---|---|---|---|---|---|
| No | Yes | ||||
| 1453 (100.0%) | 772 (53.1%) | 681 (46.9) | p Value | ||
| MPI, mean (SD) | 0.11 (0.15) | 0.05 (0.07) | 0.17 (0.19) | <.001 | |
| MPI risk group, n (%) | Low [0–0.25] | 1309 (90.1) | 766 (99.2) | 543 (79.7) | <.001 |
| Moderate [0.26–0.50] | 89 (6.1) | 6 (0.8) | 83 (12.2) | ||
| Severe [0.51–1.00] | 55 (3.8) | 0 (0.0) | 55 (8.1) | ||
| Age, mean (SD) | 68.9 (15.7) | 60.5 (15.8) | 78.4 (8.3) | <.001 | |
| Sex, n (%) | Female | 811 (55.8) | 457 (59.2) | 354 (52.0) | .006 |
| Male | 642 (44.2) | 315 (40.8) | 327 (48.0) | ||
| ADL, n (%) | 5–6 | 1376 (94.7) | 770 (99.7) | 606 (89.0) | <.001 |
| 3–4 | 28 (1.9) | 2 (0.3) | 26 (3.8) | ||
| 0–2 | 49 (3.4) | 0 (0.0) | 49 (7.2) | ||
| IADL, n (%) | 6–8 | 1271 (87.5) | 762 (98.7) | 509 (74.7) | <.001 |
| 4–5 | 56 (3.9) | 8 (1.0) | 48 (7.1) | ||
| 0–3 | 126 (8.7) | 2 (0.3) | 124 (18.2) | ||
| MMSE, n (%) | 16–30 | 1380 (95.0) | 770 (99.7) | 610 (89.6) | <.001 |
| 9–15 | 42 (2.9) | 2 (0.3) | 40 (5.9) | ||
| 0–8 | 31 (2.1) | 0 (0.0) | 31 (4.5) | ||
| Mobility, n (%) (1 missing) | 2–3 | 1353 (93.2) | 770 (99.7) | 583 (85.7) | <.001 |
| 1 | 39 (2.7) | 2 (0.3) | 37 (5.4) | ||
| 0 | 60 (4.1) | 0 (0.0) | 60 (8.8) | ||
| Drugs, n(%) | 0–3 | 1159 (79.8) | 692 (89.6) | 467 (68.6) | <.001 |
| 4–6 | 233 (16.0) | 70 (9.1) | 163 (23.9) | ||
| >6 | 61 (4.2) | 10 (1.3) | 51 (7.5) | ||
| MNA, n(%) (142 missing) | 12–14 | 877 (66.9) | 550 (74.8) | 327 (56.8) | <.001 |
| 8–11 | 371 (28.3) | 177 (24.1) | 194 (33.7) | ||
| 0–7 | 63 (4.8) | 8 (1.1) | 55 (9.6) | ||
| Comorbidity, n (%) | 0–3 | 1089 (75.0) | 679 (88.0) | 410 (60.2) | <.001 |
| 4–6 | 319 (21.9) | 88 (11.4) | 231 (33.9) | ||
| >6 | 45 (3.1) | 5 (0.6) | 40 (5.9) | ||
| Cohabitation status, n (%) | With family | 1221 (84.0) | 680 (88.1) | 541 (79.4) | <.001 |
| Nursing home | 17 (1.2) | 1 (0.1) | 16 (2.4) | ||
| Alone | 215 (14.8) | 91 (11.8) | 124 (18.2) | ||
Notes: ADL = activities of daily living; IADL = instrumental activities of daily living; MMSE = Mini-Mental State Examination; MNA = Mini Nutritional Assessment; MPI = Multidimensional Prognostic Index. p values were referred to a t test for mean and Fisher’s exact test for frequencies.
Deceased participants had significantly higher baseline MPI values than those alive (0.17 ± 0.19 vs 0.05 ± 0.07, p < .001).
Survival Analyses
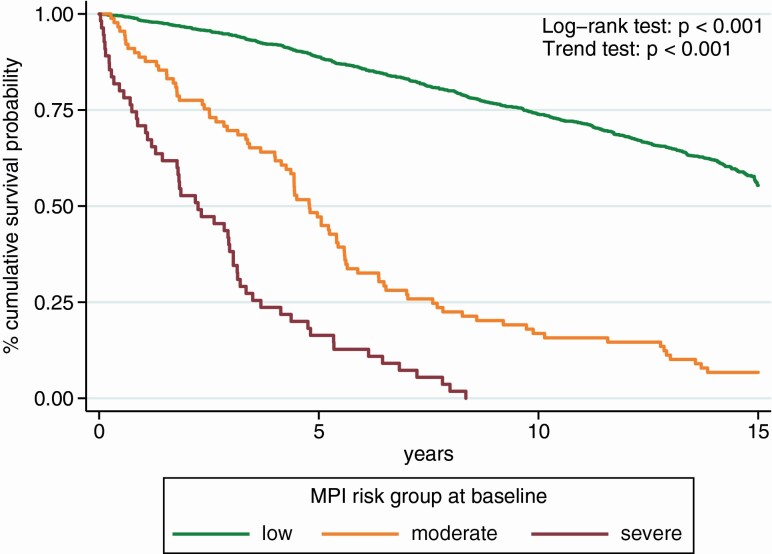
Figure 1 shows the association between MPI categories and mortality during 15 years of follow-up. Participants in the most severe risk group experienced significantly higher mortality than the other 2 groups (log-rank test and p for trend: <.001). In fact, compared to MPI-1 low-risk group, participants in MPI-2 moderate-risk (HR = 2.10; 95% CI: 1.73–2.55; p < .001) and MPI-3 high-risk group (HR = 4.94; 95% CI: 3.91–6.24; p < .001) experienced a significantly higher risk of mortality.
Figure 1.
Survival curves by Multidimensional Prognostic Index categories in the InCHIANTI study.
As given in Table 2, similar results were obtained using MPI as an ordinal variable based on increments of 0.10 points (HR = 1.42; 95% CI: 1.36–1.49; p < .001). As given in Table 2, the C-index for the model containing age, sex, and MPI in explaining mortality was very good (82.1; 95% CI: 80.6–83.5). The time-dependent AUC assessed every 3 years indicated that the accuracy of the model incorporating MPI to sex and age in explaining mortality was, again, excellent (ranging from 86.1 to 88.2) at both short- (3 years) and long-term (15 years) prospective and also during the intermediate assessments. The addition of the MPI to a model with age and sex for the prediction of the 15-year mortality involved a mean increase on C-index of 1.5% (p < .001). Despite a little improvement, even if significant, a stronger increase was related to the age of the participants. In particular, the improvement was of 2.5% (p = .023), 4.5% (p = .002), and 14.4% (p < .001) when age was stratified in 66–75, 76–85, and 85 and older years, respectively.
Table 2.
Adjusted Survival Analyses in the InCHIANTI Study by Using a 2-Stage Model for Including the Longitudinal Evolution of MPI During the Follow-up Period in the Estimation of the Cox Model
| AUC (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | 3 years | 6 years | 9 years | 12 years | 15 years | C-index (95% CI) | |
| MPI (×0.10 increase) | 1.42 (1.36–1.49) | <.001 | 86.1 (83.0–89.2) | 87.9 (86.1–89.8) | 88.1 (86.4–89.8) | 88.2 (86.4–89.9) | 86.1 (84.2–88.1) | 82.1 (80.6–83.5) |
| Sex (M vs F) | 2.03 (1.74–2.37) | <.001 | ||||||
| Age (×5 years increase) | 1.54 (1.47–1.61) | <.001 | ||||||
Note: AUC = area under than curve; HR = hazard ratio; MPI = Multidimensional Prognostic Index.
Table 3 reports the median time to death, according to the MPI, age at baseline (stratified in <65, 65–74, 75–84, and ≥85 years). The median survival of people in moderate-risk MPI groups varied across age groups from 2.9 to 7.0 years earlier than for those in the low-risk MPI group (p < .0001), and the median survival of people in high-risk MPI groups varied by age from 4.3 to 8.9 years earlier than for those in the low-risk MPI group (p < .0001; Table 3). No analysis in those younger than 65 years was possible because all the participants dying during the follow-up were included in the low-risk MPI group.
Table 3.
Median Time to Death in Years, by Multidimensional Prognostic Index (MPI) Group and Age
| <65 | 65–74 | 75–84 | ≥85 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 17/298 (5.7%) | 210/610 (34.4%) | 279/366 (76.2%) | 175/179 (97.8%) | |||||||||
| MPI Group | Years | 95% CI | p Value | Years | 95% CI | p Value | Years | 95% CI | p Value | Years | 95% CI | p Value |
| Low | Excluded because no patients in moderate- and high-risk classes | Ref. | — | <.001 | Ref. | — | <.001 | Ref. | — | <.001 | ||
| Moderate | −7.0 | −12.5 to −1.5 | −3.9 | −6.0 to −1.9 | −2.9 | −4.1 to −1.6 | ||||||
| High | −8.9 | −12.9 to −4.8 | −6.7 | −8.7 to 4.7 | −4.3 | −5.3 to −3.3 | ||||||
Note: Adjusted for age and gender.
Discussion
In this community-based prospective observational study including a large cohort of people living in Tuscany, Italy, we found that higher MPI values were significantly associated with mortality during 15 years of follow-up. Multidimensional Prognostic Index showed a very high discriminatory power and accuracy in explaining mortality in the InCHIANTI study.
The prognostic value of the MPI has been widely demonstrated in more than 50 000 older patients with acute or chronic conditions (such as pneumonia, heart failure, gastrointestinal bleeding, chronic renal disease, transient ischemic attack, dementia, atrial fibrillation, and coronary artery disease) (8). However, most of these studies included hospitalized patients or long-term care facility residents and patients receiving home care services (8). Our findings are consistent with a study conducted in Sweden on a population-based cohort of 2472 community-dwelling older persons that found that higher MPI values were associated with more days spent in hospital and higher mortality risk, across different settings and ages (16).
To calculate the MPI from the data collected on the InCHIANTI study, we used a slightly modified version of the original MPI, namely, we used the MMSE and Charlson Comorbidity Index instead of the Short Portable Mental Status Questionnaire and the Cumulative Illness Rating Scale, respectively, which are included in the original version of the MPI. This approach was possible thanks to the “plasticity” of the MPI, that is, the capacity of the CGA-based MPI to maintain its prognostic properties even if derived from different tools (27,28). In this regard, values to define risks are specific for each population/setting and to the outcome of interest. Indeed, very recently MPI was recognized as one of the most used tools in clinical practice to assess frailty in older participants (29).
An interesting and original finding of this study is that the prognostic value of the MPI for mortality became progressively higher at older ages, as reported by the median time to death that shows significant findings only after 65 years of age. Even if this result is somewhat expected, we believe that is relevant since one of the most important questions in actual geriatric medicine, is: “when does the geriatric year begin?” We can define “old age” as the age nearing or surpassing the life expectancy of human beings. Traditionally, older age begins after 65 years, that is, in many Western countries, the age of retirement (30), but more precisely older age is the age after that expected mortality significantly increases. Our work might suggest that a reliable answer to this question is the geriatric era begins when the component “multidimensional fragility” (as measured with MPI) is relevant, that is, after 65 years.
The findings of our study must be interpreted within its limitations. First, we validated MPI in the InCHIANTI study only for mortality which may not be the most important outcome considered in geriatric medicine. Future outcomes should address the ability of the MPI to explain other adverse outcomes important for older patients, including falls, disability, health care utilization, and nursing home admission (31).
In conclusion, in community-dwelling individuals participating in the InCHIANTI study, higher MPI values were associated with higher mortality risk. This finding was particularly evident in older people, indicating the possibility of using MPI also in older community dwellers. The association between MPI and mortality was evident only in people older than 65 years, indicating that this age should be considered the starting point for CGA. Future research in this topic should cover the MPI’s ability to explore biological, genetic, and environmental factors of aging, a topic of great interest in geriatric medicine.
Funding
The study was supported in part by the Intramural Research Program of the National Institute on Aging, NIH, Baltimore, MD and by the MPI_AGE European project co-funded by the Consumers, Health, Agriculture, and Food Executive Agency (CHAFEA) in the frame of the European Innovation Partnership on Active and Healthy Ageing Second Health Programme 2008–2013. The contents of this article are the sole responsibility of the authors and can under no circumstances be regarded as reflecting the position of the European Union. The funding agencies had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The study was based on administrative data sets, and the participants were not identifiable to the authors.
Conflict of Interest
None declared.
Author Contributions
Statistical analysis: G.S.; data collection: L.F. and S.B.; data analysis: N.V. and T.T.; draft of the manuscript: A.P., N.V., and A.C.; and critical revision: L.F., S.B., and T.T.
Supplementary Material
References
- 1.Lee SJ, Leipzig RM, Walter LC. Incorporating lag time to benefit into prevention decisions for older adults. JAMA. 2013;310:2609–2610. doi: 10.1001/jama.2013.282612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenborn NL, Bowman TL 2nd, Cayea D, Pollack CE, Feeser S, Boyd C. Primary care practitioners’ views on incorporating long-term prognosis in the care of older adults. JAMA Intern Med. 2016;176:671–678. doi: 10.1001/jamainternmed.2016.0670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307:182–192. doi: 10.1001/jama.2011.1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gill TM. The central role of prognosis in clinical decision making. JAMA. 2012;307:199–200. doi: 10.1001/jama.2011.1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pilotto A, Ferrucci L, Franceschi M, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 2008;11:151–161. doi: 10.1089/rej.2007.0569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pilotto A, Rengo F, Marchionni N, et al. ; FIRI-SIGG Study Group . Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS One. 2012;7:e29090. doi: 10.1371/journal.pone.0029090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pilotto A, Veronese N, Daragjati J, et al. ; MPI_AGE Investigators . Using the multidimensional prognostic index to predict clinical outcomes of hospitalized older persons: a prospective, multicenter, international study. J Gerontol A Biol Sci Med Sci. 2019;74:1643–1649. doi: 10.1093/gerona/gly239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pilotto A, Custodero C, Maggi S, Polidori MC, Veronese N, Ferrucci L. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020;60:101047. doi: 10.1016/j.arr.2020.101047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilotto A, Addante F, Ferrucci L, et al. The multidimensional prognostic index predicts short-and long-term mortality in hospitalized geriatric patients with pneumonia. J Gerontol A Biol Sci Med Sci. 2009;64:880–887. doi: 10.1093/gerona/glp031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Volpato S, Daragjati J, Simonato M, Fontana A, Ferrucci L, Pilotto A. Change in the multidimensional prognostic index score during hospitalization in older patients. Rejuvenation Res. 2016;19:244–251. doi: 10.1089/rej.2015.1715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pilotto A, Sancarlo D, Pellegrini F, et al. ; FIRI-SIGG Study Group . The Multidimensional Prognostic Index predicts in-hospital length of stay in older patients: a multicentre prospective study. Age Ageing. 2016;45:90–96. doi: 10.1093/ageing/afv167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volpato S, Bazzano S, Fontana A, Ferrucci L, Pilotto A; MPI-TriVeneto Study Group . Multidimensional Prognostic Index predicts mortality and length of stay during hospitalization in the older patients: a multicenter prospective study. J Gerontol A Biol Sci Med Sci. 2015;70:325–331. doi: 10.1093/gerona/glu167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pilotto A, Sancarlo D, Panza F, et al. The Multidimensional Prognostic Index (MPI), based on a comprehensive geriatric assessment predicts short-and long-term mortality in hospitalized older patients with dementia. J Alzheimers Dis. 2009;18:191–199. doi: 10.3233/JAD-2009-1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pilotto A, Addante F, Franceschi M, et al. Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short-term mortality in older patients with heart failure. Circ Heart Fail. 2010;3:14–20. doi: 10.1161/CIRCHEARTFAILURE.109.865022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sancarlo D, D’Onofrio G, Franceschi M, et al. Validation of a Modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging. 2011;15:169–173. doi: 10.1007/s12603-010-0293-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angleman SB, Santoni G, Pilotto A, Fratiglioni L, Welmer AK; MPI_AGE Project Investigators . Multidimensional Prognostic Index in association with future mortality and number of hospital days in a population-based sample of older adults: results of the EU funded MPI_AGE Project. PLoS One. 2015;10:e0133789. doi: 10.1371/journal.pone.0133789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cesari M, Leeuwenburgh C, Lauretani F, et al. Frailty syndrome and skeletal muscle: results from the Invecchiare in Chianti study. Am J Clin Nutr. 2006;83:1142–1148. doi: 10.1093/ajcn/83.5.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stenholm S, Ferrucci L, Vahtera J, et al. Natural course of frailty components in people who develop frailty syndrome: evidence from two cohort studies. J Gerontol A Biol Sci Med Sci. 2019;74:667–674. doi: 10.1093/gerona/gly132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x [DOI] [PubMed] [Google Scholar]
- 20.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20 [DOI] [PubMed] [Google Scholar]
- 21.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. doi: 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Robins LN, Helzer JE. The Mini-Mental State Examination. Arch Gen Psychiatry. 1983;40:812. doi: 10.1001/archpsyc.1983.01790060110016 [DOI] [PubMed] [Google Scholar]
- 23.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5 [DOI] [PubMed] [Google Scholar]
- 24.Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment Short-Form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13:782. doi: 10.1007/s12603-009-0214-7 [DOI] [PubMed] [Google Scholar]
- 25.Chang C, Hsieh M-K, Chang W-Y, Chiang AJ, Chen J. Determining the optimal number and location of cutoff points with application to data of cervical cancer. PLoS One. 2017;12:e0176231. doi: 10.1371/journal.pone.0176231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bottai M, Zhang J. Laplace regression with censored data. Biom J. 2010;52:487–503. doi: 10.1002/bimj.200900310 [DOI] [PubMed] [Google Scholar]
- 27.Cruz-Jentoft AJ, Daragjati J, Fratiglioni L, et al. Using the Multidimensional Prognostic Index (MPI) to improve cost-effectiveness of interventions in multimorbid frail older persons: results and final recommendations from the MPI_AGE European Project. Aging Clin Exp Res. 2020;32:1–8. doi: 10.1007/s40520-020-01516-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Veronese N, Siri G, Cella A, et al. The multidimensional prognostic index predicts falls in older people: an 8-year longitudinal cohort study of the osteoarthritis initiative. J Am Med Dir Assoc. 2020;21:669–674. doi: 10.1016/j.jamda.2019.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394:1376–1386. doi: 10.1016/S0140-6736(19)31785-4 [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Definition of an older or elderly person. https://www.who.int/healthinfo/survey/ageingdefnolder/en/. Accessed April 4, 2020. [Google Scholar]
- 31.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–762. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.