Abstract
Background and Objectives
Fear of falling (FoF) is associated with decreased physical functioning and an increased fall risk. Interventions generally demonstrate moderate effects and optimized interventions are needed. Intervention characteristics, such as setting or delivery method may vary. We investigated which overarching intervention characteristics are associated with a reduction in FoF in community-dwelling older people.
Research Design and Methods
A systematic review and meta-analysis of randomized controlled trials (RCTs) in community-dwelling older people without specific diseases was performed. Associations between intervention characteristics and standardized mean differences (SMD) were determined by univariate meta-regression. Sensitivity analyses were performed.
Results
Data on 62 RCTs were extracted, 50 intervention groups were included in the meta-analysis. Most intervention characteristics and intervention types were not associated with the intervention effect. Supervision by a tai chi instructor (SMD: −1.047, 95% confidence interval [CI]: −1.598; −0.496) and delivery in a community setting (SMD: −0.528, 95% CI: −0.894; −0.161) were—compared to interventions without these characteristics—associated with a greater reduction in FoF. Holistic exercise, such as Pilates or yoga (SMD: −0.823, 95% CI: −1.255; −0.392), was also associated with a greater reduction in FoF. Delivery at home (SMD: 0.384, 95% CI: 0.002; 0.766) or with written materials (SMD: 0.452, 95% CI: 0.088; 0.815) and tailoring were less effective in reducing FoF (SMD: 0.687, 95% CI: 0.364; 1.011).
Discussion and Implications
Holistic exercise, delivery with written materials, the setting and tailoring potentially represent characteristics to take into account when designing and improving interventions for FoF in community-dwelling older people. PROSPERO international prospective register of systematic reviews, registration ID CRD42018080483.
Keywords: Accidental falls, Intervention effectiveness, Falls self-efficacy
Falls are a major cause of morbidity and mortality among older people and they account for a large share of health care costs (World Health Organization, 2018). Up to 90% of all fractures result from a fall and in the Netherlands, for example, injurious falls constitute 41% of costs related to home and leisure injuries (Peeters, van Schoor, & Lips, 2009; Polinder et al., 2016). In addition, falls can have psychological consequences, such as fear of falling (FoF). Historically, FoF has been used to refer to cognitive constructs (e.g., balance confidence or fall-related self-efficacy) and affect-based constructs (e.g., concern or worry about falling). FoF is common among older people. Depending on the population and measure, prevalence rates vary between 21% and 85% (Malini, Lourenço, & Lopes, 2016; Scheffer, Schuurmans, Van Dijk, Van Der Hooft, & De Rooij, 2008; Tomita et al., 2018). It also occurs in those who have not previously fallen (Scheffer et al., 2008). Consequences of FoF include avoidance of activities, decreased physical functioning, an increased risk of falls, and lower social participation, and it represents a problem for independence and independent living (van der Meulen, Zijlstra, Ambergen, & Kempen, 2014; Scheffer et al., 2008; Yardley & Smith, 2002). Given these consequences, FoF is a public health problem that requires attention and effective interventions to reduce FoF in community-dwelling older people are necessary.
Different types of interventions, such as tai chi, active video games, and cognitive behavioral therapy (CBT) (Liu & Frank, 2010; Liu, Ng, Chung, & Ng, 2018; Taylor, Kerse, Frakking, & Maddison, 2016), have already demonstrated reductions in FoF in older people. Studies show that effects do not only vary between types of interventions, but can also vary within intervention types. For example, Logghe and colleagues (2009) reported a tai chi chuan intervention had no effects on FoF, whereas Zhang, Ishikawa-Takata, Yamazaki, Morita, and Ohta (2006) demonstrated a tai chi chuan intervention caused a significant reduction in FoF. This variation in intervention effects may be partly explained by differences in content; for example, 24 tai chi positions were used in the study by Zhang and colleagues (2006), whereas only 10 were used in the study by Logghe and colleagues (2009). However, according to Peters, de Bruin, and Crutzen (2015) and Mahoney (2010), the effectiveness of interventions can also be determined by other characteristics, such as how the intervention content is delivered and to whom. Several reviews and meta-analyses have been performed to identify characteristics that could be contributing to the effectiveness of FoF interventions in community-dwelling older people. For instance, Liu and colleagues (2018) and Kendrick and colleagues (2014) studied the effectiveness of interventions in relation to the group format, that is, interventions delivered in groups or individually. Liu and colleagues (2018) showed a small effect for group CBT interventions (n = 4) and a small-to-moderate effect for individual CBT interventions (n = 2). Kendrick and colleagues (2014) studied the effect of exercise interventions and found no difference between group and individual interventions in a meta-analysis of 24 studies. Other characteristics often studied in reviews and meta-analyses are duration of the intervention (Büla, Monod, Hoskovec, & Rochat, 2011; Kendrick et al., 2014; Liu et al., 2018; Whipple, Hamel, & Talley, 2018), frequency or number of intervention sessions (Kendrick et al., 2014; Liu et al., 2018; Logghe et al., 2010), and location (Jung, Lee, & Lee, 2009; Logghe et al., 2010).
Despite the existence of several reviews on the subject of intervention characteristics, characteristics like tailoring, type of supervisor, and delivery method (e.g., face-to-face, telephone, or internet) are frequently not taken into account. Moreover, reviews assessing intervention characteristics are often limited to one type of intervention, for example, only video games or strength training, or include only a small number of trials (Dennett & Taylor, 2015; Fisseha, Janakiraman, Yitayeh, & Ravichandran, 2017; Jung et al., 2009; Liu et al., 2018; Logghe et al., 2010; Neri et al., 2017; Rodrigues, Valderramas, Rossetin, & Gomes, 2014; Wong, Wong, Yeung, & Chang, 2017). Consequently, a patchwork of information and recommendations emerges. The current knowledge base lacks an overview of all types of interventions and insight into overarching effective intervention characteristics. Furthermore, small-to-moderate effect sizes may be an indication that optimization of FoF interventions is possible. Presumably, effect sizes could increase by strengthening effective characteristics and removing or attenuating ineffective ones (Collins, Murphy, Nair, & Strecher, 2005; West & Aiken, 1997). This warrants a comprehensive and in-depth analysis into the relationship between characteristics of FoF interventions and intervention effectiveness. We conducted a review and meta-analysis of randomized controlled trials (RCTs) to determine which overarching characteristics of interventions are effective in reducing FoF in community-dwelling older people.
Methods
A systematic review and meta-analysis was performed. This study was registered at the PROSPERO international prospective register of systematic reviews, registration ID CRD42018080483.
The reporting of this review is in accordance with the PRISMA guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009); see Supplementary File S1.
Search Strategy
In 2007, Zijlstra et al. published a systematic review on RCTs assessing interventions to reduce FoF. This study was used as starting point for the current study. Based on the search by Zijlstra and colleagues (2007), an updated search was performed in the databases PubMed, EMBASE, PsycINFO, CINAHL, and CENTRAL on July 19, 2019. Keywords relating to outcome (FoF), design (randomized controlled trial), and population (older people) were combined with AND (full search strategy available at: https://osf.io/4vwtc/?view_only=b3241161660043e3a704bd6fca10485f). Searches were restricted to publications written in English or Dutch and, given the updated search, to articles published after July 1, 2005. Articles from before July 2005 were obtained from the review by Zijlstra and colleagues (2007). Additional search strategies included consulting international experts who recently published in the domain of FoF or falls, manually searching reference lists of previous reviews and meta-analyses, and searching for published articles when a potentially relevant protocol was found.
Outcome of Interest
FoF was first conceptualized as “low perceived self-efficacy at avoiding falls” in 1990, when the Falls Efficacy Scale (FES) was developed by Tinetti, Richman, and Powell (1990). Since then, FoF has been used to refer to cognitive constructs (e.g., balance confidence or fall-related self-efficacy) and affect-based constructs (e.g., concern or worry about falling) and they are used interchangeably. We used the term “fear of falling” as an umbrella term including all of these aspects.
Eligibility Criteria
To select studies, the following inclusion criteria were used:
The article reported on results of an RCT evaluating an intervention, including cluster-randomized controlled trials (at least three clusters per arm) and randomized crossover trials, with assessments at similar moments in time (e.g., after the intervention) for all intervention arms.
The mean age of the total population was 65 years or over.
Study participants were older people living at home (non-institutionalized).
FoF was included as a primary or secondary outcome of the study and the article reported on results of this outcome.
The control group received either care as usual or no intervention (including wait list controls). An educational booklet for the control group or other sham interventions were also seen as interventions.
The following exclusion criteria were used:
The article was written in a language other than Dutch or English. Even though searches were restricted to English and Dutch articles, this was used as an exclusion criterion as well. Full-text articles are sometimes written in other languages than the abstract and search filters do not always recognize these other languages.
The study was performed in a specific patient group characterized by a disease or medical condition (e.g., Parkinson’s disease, stroke, hip fracture) or a population that had recently received treatment for a medical condition (e.g., hip arthroplasty).
No criteria regarding the type of intervention were formulated.
Study Selection Process
Title and abstract screening
To facilitate a systematic comparison of titles and abstracts against criteria, criteria were applied in the following order: design, age of the population, living situation of the population, health of the population, outcome, and language. For practical reasons, the control group was not yet assessed in the title and abstract phase. When titles and abstracts met inclusion criteria or when doubt remained after checking titles and abstracts, articles proceeded to the next phase: full-text screening.
The first 200 titles and abstracts were screened independently by two authors (M.K. and G.A.R.Z.). There was 95.5% agreement on whether full-text screening was required; kappa was 0.67 (95% confidence interval [CI]: 0.462; 0.869), indicating good interrater reliability (Higgins & Green, 2011a). This agreement was considered sufficient for one author to screen the remaining titles and abstracts (M.K.). As this study concerns an update from the review by Zijlstra and colleagues (2007) and we added one extra criterion regarding the control group, articles from this review were screened against eligibility criteria as well.
Full-text screening
Full texts were checked against criteria in the following order: language, design, control group, age of the population, living situation of the population, health of the population, and outcome. Full-text articles were screened by one reviewer (M.K.). When an article lacked information on a criterion (e.g., the living situation of the population was not reported), the study was excluded. In cases of doubt with respect to inclusion, a second reviewer was consulted to achieve consensus (G.I.J.M.K., R.C., or G.A.R.Z.).
Data Extraction
A data extraction form was developed and pilot-tested among six of the authors (M.K., K.D., G.I.J.M.K., K.-L.C., D.K., and S.I.). Data from one study were extracted independently by teams of two authors. Completed data extraction forms were checked to see whether similar data had been extracted. In addition, suggestions by authors were used to improve the data extraction form. Subsequently, data from each study were extracted independently by teams of two authors. Extracted data included bibliographical information and details on the design of the study, participant characteristics, FoF measures, intervention content and delivery, and results. The final extraction form can be viewed at https://osf.io/vczg5/?view_only=ce9dae90f3a842e38d2aa29f6abcfb8e. FoF results were extracted for all intervention arms for the first available assessment after the intervention and at the last assessment available. For crossover RCTs, the data before the crossover were extracted. After the data extraction, intervention types were determined by two authors (M.K. and G.A.R.Z.) based on the focus indicated in the title, abstract, introduction, and methods section of an article. Risk of bias was assessed in a separate extraction form with the Cochrane Collaboration’s Tool for assessing risk of bias in randomized trials (Higgins et al., 2011), which covers selection bias (two items), performance bias, detection bias, attrition bias, reporting bias, and other types of bias. Each of the seven items in the tool was scored with a low, high, or unclear risk of bias. This form was pilot-tested as well. Disagreements in extracted information were resolved in consensus meetings between authors M.K. and R.C. or G.A.R.Z.
Protocols and design articles were checked for additional intervention details when a reference to such a paper was included. When information from protocols was contradictory to effect articles, the effect article had priority. When results were not reported in a format that could be analyzed (e.g., in figures only or no measure of variance), authors were contacted for additional information. When data could not be provided, studies were excluded from the meta-analysis, but included in the systematic review section of this study.
Analysis
For each study, a standardized mean difference (SMD) was estimated by the method of Cohen, resulting in the sample estimate Cohen’s d. Standardization of effects is appropriate when different scales are used (Higgins & Green, 2011b). To calculate Cohen’s d, the number of participants, follow-up means, and standard deviations for the intervention and control group were used. A complete overview of formulas is available at https://osf.io/v89an/?view_only=8711c954c6b746428cec4d06ef5cfd08. SMDs were interpreted as follows: 0.2 a small effect, 0.5 a moderate effect, and 0.8 a large effect (Cohen, 1988). A random effects meta-analysis model was used to summarize SMDs for the first available follow-up after the intervention. Whereas fixed effects meta-analysis attributes heterogeneity in effect estimates only to random sampling error, a random effects approach also allows for between-study heterogeneity.
First, main effects on FoF were estimated, without focus on intervention characteristics. Second, associations between intervention characteristics and the effects of FoF interventions were determined by univariate meta-regression. Meta-regressions included categorical intervention characteristics which compared studies with an intervention characteristic (coded as 1) with all studies without that characteristic (coded as 0). The regression coefficient obtained from a meta-regression analysis using this 0–1 coding scheme is the difference in predicted outcome variable (i.e., difference in the SMD) between interventions with and without the characteristic in question. Furthermore, we analyzed continuous intervention characteristics which investigated change in the SMD for a one unit change in the intervention characteristic. The type of intervention (e.g., exercise, education, cognitive behavioral) was also analyzed with meta-regression in the same way. The following categorical variables were investigated: intervention type, whether FoF was a primary outcome of the study, whether FoF was a topic of the intervention, setting (where the intervention was delivered, i.e., at home, in the community, or both), delivery method (e.g., face-to-face, written materials—such as manuals and exercise diaries—or telephone), tailoring (adaptation of the intervention to the individual based on a formal or informal assessment by the supervisor), group format (individual, group, or both), presence of supervision, type of supervisor, whether the supervisor participated in intervision sessions and whether the supervisor had experience in working with older people. Intervision sessions were defined as meetings or phone calls during the intervention, either between a group of supervisors or between supervisors and an investigator or manager. The following continuous variables were investigated: contact time with a facilitator and duration of the intervention. The number of intervention sessions is presented in the results, but not analyzed with meta-regression. Whether the number of sessions is related to an outcome can be dependent on the intervention content. Therefore, the number of sessions was not considered suitable for analysis.
When a study had multiple intervention arms, only one intervention arm was included in meta-analysis in order to avoid correlated data in the meta-analysis. The arm used in the primary analysis was always the intervention arm mentioned first in the abstract. Heterogeneity (variability in intervention effects) was quantified with I2 and tested by Q test statistics. The following interpretations for I2 from the Cochrane handbook were used: “0%–40%: might not be important; 30%–60%: may represent moderate heterogeneity; 50%–90%: may represent substantial heterogeneity; 75%–100%: considerable heterogeneity” (Higgins & Green, 2011c). As we investigated overarching characteristics and included a wide range of intervention types, we expected heterogeneity to be high. Part of the heterogeneity could possibly be explained by one or more of the characteristics. Publication bias was assessed by visual inspection of funnel plots and Egger’s test. Outliers were determined by visual inspection of the forest plot and funnel plot.
Sensitivity analyses were performed to assess the influence of methodological decisions which were made. The following sensitivity analyses were performed:
(a) performing meta-analysis and meta-regressions without outliers;
(b) performing a meta-analysis on cognitive-based FoF measures (e.g., FES, Activities-specific Balance Confidence scale [ABC]), and affect-based FoF measures (e.g., Falls Efficacy Scale—International [FES-I], the Survey of Activities and Fear of Falling in the Elderly [SAFFE]) separately;
(c) repeating meta-regressions with the other intervention arm of a study (in case more than one intervention arm was involved);
(d) repeating meta-regressions without cluster RCTs;
(e) repeating meta-regressions with the results of the latest assessment (to evaluate long-term effects instead of the effects at the first follow-up after the intervention);
(f) performing a meta-regression of the association of study quality (the number of risk of bias items scored as high risk, as a continuous variable) with the SMD.
All analyses were performed with STATA version 15. The significance level was set at 0.05 for meta-regressions. Syntaxes and data can be viewed at: https://osf.io/v89an/?view_only=8711c954c6b746428cec4d06ef5cfd08.
Results
Search Results
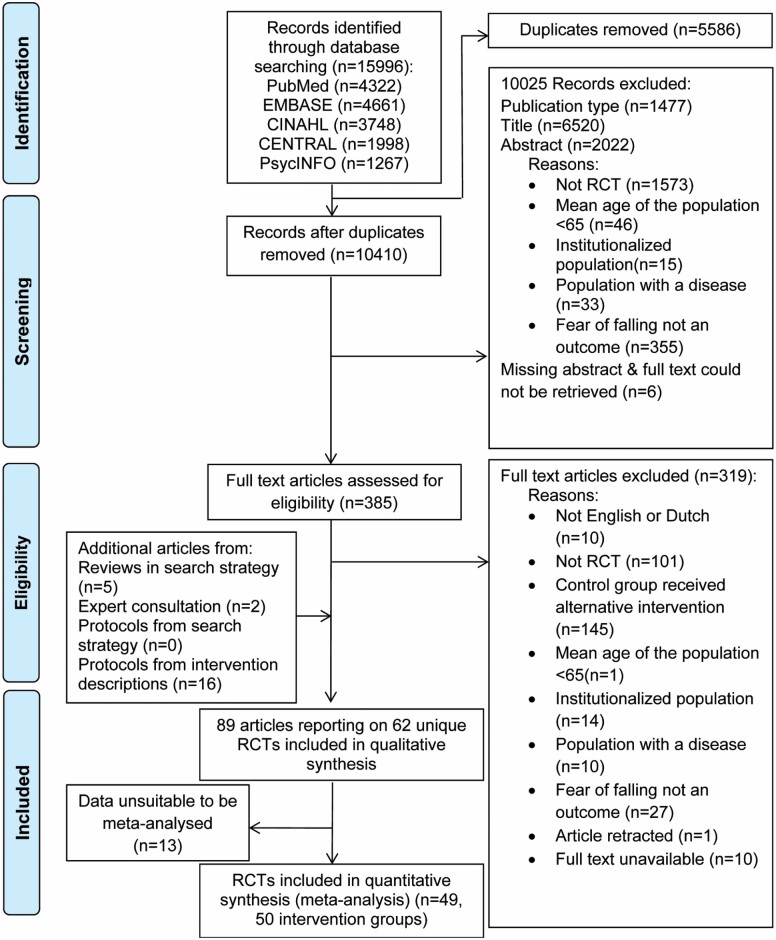
The process of article selection is shown in Figure 1. Searching literature databases resulted in 10,410 unique hits of which 385 full-text articles remained after title and abstract screening. Full-text screening resulted in 66 articles suitable for inclusion. Screening of reviews, expert consultation, and protocols from intervention descriptions yielded 23 additional articles. In total, 89 articles providing data on 62 unique RCTs were included in qualitative synthesis. Forty-nine studies provided data that were suitable for inclusion in meta-analysis.
Figure 1.
Flow-chart of study selection process.
Description of Studies
Studies were conducted in 18 different countries, often in Europe (n = 21) or North America (n = 12). Most studies were parallel-group RCTs (n = 53), of which the majority had two study arms (n = 39). The mean age of the population varied from 65 to 86 years. One study recruited only women. Five studies recruited participants with FoF, five with a fall risk, five with a history of falls, three without a history of falls, and two with FoF or a history of falls. Other criteria on which participants were selected related to physical activity—including prior participation in exercise and activity avoidance—or were related to health, such as physical functioning, frailty, mobility complaints, and perceived general health. Some studies did not report on basic information, such as the country in which the study was conducted (n = 8), or the number of women included in the study (n = 1). Three studies did not report on the mean age, but only reported a minimum age as part of their inclusion criteria. A table with an overview of the study characteristics is available at: https://osf.io/57j8c/?view_only=ba523b0cfa92477690f12e38b9dc8b21.
FoF was a primary outcome in eight studies. Other primary outcomes that were used often were falls or fall risk (n = 13) and balance or balance performance (n = 21). Seven studies used more than one outcome measure to measure FoF. The first available measurement was often directly after the intervention (n = 53), other studies assessed FoF for the first time between 4 and 48 weeks after the intervention (n = 8). One study only assessed FoF at the halfway point of the intervention. Nineteen studies measured FoF more than one time. The last available assessment for these studies ranged from 12 to 96 weeks after the end of the intervention. The majority of studies (n = 61) used scales with multiple items and five studies used a one-item question to assess FoF.
The number of items on which studies scored a high risk of bias ranged from two to four out of seven. Items three and four of the Cochrane risk of bias tool, regarding blinding of participants and personnel (performance bias) and blinding of outcome assessment (detection bias), scored a high risk of bias in all studies. This was due to the nature of the interventions, as it was not possible to blind participants and personnel to group allocation in, for example, exercise interventions. Furthermore, self-reported FoF measures were used and as participants were not blinded, participants were aware of their allocation when reporting their FoF. The risk of bias scoring per item for all studies can be viewed at: https://osf.io/57j8c/?view_only=ba523b0cfa92477690f12e38b9dc8b21.
Description of Interventions
Sixty-two studies described 79 interventions. In Supplementary File S2, a description of intervention characteristics is given. For references of studies included in this review, see Supplementary File S2. Most interventions were exercise interventions (n = 61). Strength training and balance training were often combined (n = 20), sometimes in combination with endurance training (n = 9). Other types included assessment-based care (n = 6), in which care is delivered based on a formal assessment, assessment-based home modification (n = 4), cognitive behavioral programs (n = 3), a referral protocol for emergency ambulance visits (n = 1), nutritional supplementation (n = 2), and mental imagery (n = 1), in which a stable position is visualized. Five studies focused on education. Of the interventions included in meta-analysis, eight interventions specifically addressed FoF as a topic in the intervention (Dorresteijn et al., 2016; Faes et al., 2011; Freiberger, Haberle, Spirduso, & Zijlstra, 2012; van Haastregt et al., 2000; Markle-Reid et al., 2010; Parry et al., 2016; Siegrist et al., 2016; Zijlstra et al., 2009).
Interventions were often delivered in a home setting (n = 25), community setting (n = 27), or in a combination of home and community settings (n = 14). Ten interventions did not report on the setting and for three interventions the setting could vary per individual. Most interventions delivered at least one of their components face to face (n = 62, excluding introductory sessions), yet components were also delivered via written materials (n = 34), game technology (n = 10), and telephone contact (n = 12). About two thirds of the interventions were tailored (n = 51) and about half delivered individually (n = 36). Most interventions were supervised (n = 71) and a range of different supervisors delivered the interventions. All had received training to deliver the intervention or had expertise in delivering the intervention from their professional background. The most common supervisors were physiotherapists (n = 19), nurses (n = 8), tai chi instructors (n = 6), and occupational therapists (n = 6). For 10 interventions, it was specifically reported that the supervisor had experience in working with older people. For 22 interventions, intervision for the supervisor, via meetings with peer supervisors or managers, was reported. The duration of interventions varied from 1 week to 1 year, the number of planned intervention sessions varied from 1 to 336, and the planned contact time with the supervisor varied from 0.5 to 56 hours.
Some studies did not report where the intervention was performed (n = 10), whether it was performed in a group or individually (n = 7), whether supervision was available (n = 2), the type of supervisor (n = 10), number of planned sessions (n = 9), or contact time with a facilitator (n = 25). Study authors reported that the intervention was effective in reducing FoF for 40 interventions. No study reported a significant increase in FoF for the first available follow-up.
Outcomes of Analyses
Meta-analysis
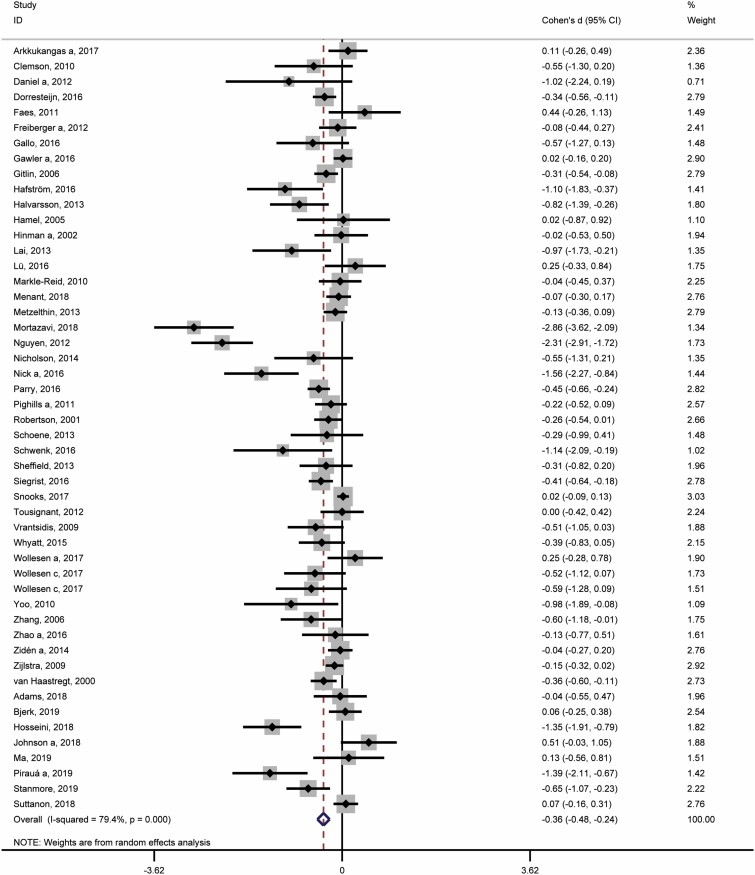
Fifty study arms were pooled in a meta-analysis (Figure 2). The number of participants included in the studies at the first available follow-up after the intervention ranged from 7 to 634 in the intervention groups and from 5 to 600 in the control groups. Pooling all interventions together resulted in an estimate of the SMD of −0.36 (95% CI: −0.48; −0.24), indicating a significant small-to-moderate reduction in FoF. There was considerable between-study variability (I2: 79.4%; p < .001). Visual inspection of the funnel plot and Egger’s test for publication bias revealed significant publication bias (p < .001). Six outliers could be identified from the funnel plot (Hafström, Malmström, Terdèn, Fransson, & Magnusson, 2016; Hosseini et al., 2018; Mortazavi, Tabatabaeichehr, Golestani, Armat, & Yousefi, 2018; Nguyen & Kruse, 2012; Nick, Petramfar, Ghodsbin, Keshavarzi, & Jahanbin, 2016; Pirauá et al., 2019). Meta-analysis without these six outliers resulted in a pooled SMD of −0.20 (95% CI: −0.28; −0.12) and heterogeneity was 53.6% (p < .001). The overall estimates for affect-based and cognitive-based measures were −0.36 (95% CI: −0.50; −0.21, I2: 78.0%) and −0.37 (95% CI: −0.57; −0.17, I2: 80.9%), respectively. For the funnel plot and the forest plots of the sensitivity analyses, see: https://osf.io/57j8c/?view_only=ba523b0cfa92477690f12e38b9dc8b21.
Figure 2.
Forest plot of the 50 intervention arms included in meta-analysis of the first available follow-up after the intervention.
Meta-regression
The characteristics “FoF as a primary outcome” or “FoF as a topic of the intervention” were not significantly associated with the SMD in FoF for the first follow-up after the intervention (Table 1). Similarly, no significant associations with the SMD were found for most types of interventions. Only holistic exercise (i.e., tai chi, yoga, ving tsun, or Pilates) yielded a significant association with the SMD of −0.823 (95% CI: −1.255; −0.392, p < .001). This indicates holistic exercise interventions were more effective in reducing FoF than all other interventions combined.
Table 1.
Meta-Regression Results for Intervention Characteristics and Types of Interventions for the First Available Follow-Up After the Intervention
| Characteristics | Studies (n) | Studies with characteristic (n) | Ba | SE | 95% CI | p-value | Residual heterogeneity (%) |
|---|---|---|---|---|---|---|---|
| Primary outcome is FoF | 50 | 7 | −0.160 | 0.241 | −0.645; 0.325 | .511 | 79.12 |
| FoF as topic | 47 | 7 | 0.249 | 0.244 | −0.243; 0.740 | .313 | 79.19 |
| Type of intervention | |||||||
| Exercise | 50 | 37 | −0.294 | 0.185 | −0.666; 0.078 | .119 | 79.20 |
| Strength training | 50 | 16 | 0.202 | 0.184 | −0.168; 0.572 | .277 | 79.52 |
| Balance training | 50 | 18 | 0.189 | 0.179 | −0.170; 0.548 | .296 | 79.66 |
| Endurance training | 50 | 11 | 0.290 | 0.207 | −0.126; 0.707 | .167 | 78.64 |
| Strength, balance and endurance training | 50 | 6 | 0.447 | 0.242 | −0.041; 0.934 | .072 | 78.44 |
| Strength and balance training | 50 | 4 | −0.105 | 0.322 | −0.752; 0.542 | .746 | 79.45 |
| Strength and endurance training | 50 | 2 | 0.391 | 0.507 | −0.628; 1.410 | .444 | 79.49 |
| Holistic exercise (tai chi, yoga, ving tsun, Pilates) | 50 | 8 | −0.823 | 0.215 | −1.255; −0.392 | <.001* | 74.28 |
| ADL exercisesb | 50 | 1 | 0.843 | 0.658 | −0.480; 2.166 | .206 | 79.50 |
| Feldenkrais | 50 | 1 | −0.117 | 0.626 | −1.376; 1.141 | .852 | 79.67 |
| Dual tasking | 50 | 4 | 0.058 | 0.334 | −0.614; 0.730 | .863 | 79.76 |
| Cognitive behavioral program | 50 | 3 | 0.091 | 0.336 | −0.585; 0.766 | .789 | 79.57 |
| Education | 50 | 2 | 0.642 | 0.427 | −0.217; 1.500 | .139 | 79.11 |
| Psychological education | 50 | 1 | 0.843 | 0.658 | −0.480; 2.166 | .206 | 79.50 |
| Mental imagery | 50 | 1 | 0.425 | 0.732 | −1.047; 1.897 | .564 | 79.76 |
| Assessment-based intervention | 50 | 9 | 0.304 | 0.209 | −0.116; 0.724 | .151 | 79.59 |
| Assessment-based care | 50 | 6 | 0.275 | 0.246 | −0.220; 0.770 | .269 | 79.74 |
| Assessment-based home modification | 50 | 3 | 0.230 | 0.346 | −0.466; 0.926 | .510 | 79.72 |
| Referral | 50 | 1 | 0.423 | 0.555 | −0.693; 1.539 | .450 | 78.15 |
| Setting | |||||||
| Home | 43 | 17 | 0.384 | 0.189 | 0.002; 0.766 | .049* | 77.27 |
| Community | 43 | 19 | −0.528 | 0.181 | −0.894; −0.161 | .006* | 77.96 |
| Both home and community | 43 | 7 | 0.252 | 0.262 | −0.278; 0.782 | .342 | 79.53 |
| Tailoring | 49 | 31 | 0.687 | 0.161 | 0.364; 1.011 | <.001* | 72.73 |
| Delivery method | |||||||
| Face-to-face | 45 | 42 | 0.411 | 0.422 | −0.440; 1.261 | .335 | 79.54 |
| Written materials | 45 | 20 | 0.452 | 0.180 | 0.088; 0.815 | .016* | 77.34 |
| Telephone | 45 | 9 | 0.340 | 0.227 | −0.117; 0.797 | .141 | 78.79 |
| Game technology | 45 | 5 | −0.022 | 0.311 | −0.649; 0.605 | .944 | 79.81 |
| Audio cassette | 45 | 3 | 0.259 | 0.401 | −0.549; 1.066 | .522 | 80.04 |
| Video | 45 | 3 | 0.274 | 0.362 | −0.457; 1.004 | .454 | 79.97 |
| Nutritional supplement | 45 | 0 | — | — | — | — | — |
| Sensor-based technology | 45 | 1 | −0.721 | 0.770 | −2.274; 0.831 | .354 | 79.73 |
| Group format | |||||||
| Individual | 46 | 23 | 0.328 | 0.177 | −0.029; 0.686 | .071 | 77.34 |
| Group | 46 | 18 | −0.369 | 0.183 | −0.738; −0.000 | .050 | 78.07 |
| Combination of group and individual | 46 | 5 | 0.040 | 0.297 | −0.559; 0.640 | .892 | 78.54 |
| Supervision | |||||||
| Supervision present | 48 | 47 | 0.701 | 0.682 | −0.671; 2.074 | .309 | 78.54 |
| Experience | 41 | 7 | 0.418 | 0.264 | −0.116; 0.951 | .121 | 80.82 |
| Intervision | 43 | 16 | 0.232 | 0.197 | −0.166; 0.630 | .247 | 80.42 |
| Supervisor type | |||||||
| Physical therapist | 38 | 14 | 0.249 | 0.219 | −0.194; 0.693 | .262 | 81.49 |
| Occupational therapist | 38 | 5 | 0.275 | 0.303 | −0.341; 0.900 | .371 | 81.61 |
| Nurse | 40 | 7 | 0.267 | 0.251 | −0.240; 0.775 | .293 | 80.66 |
| Healthcare assistant | 38 | 1 | −0.035 | 0.629 | −1.310; 1.240 | .956 | 81.40 |
| Homecare | 38 | 1 | 0.951 | 0.661 | −0.389; 2.291 | .159 | 80.99 |
| Social worker | 38 | 1 | 0.391 | 0.626 | −0.880; 1.661 | .537 | 81.43 |
| Case manager | 38 | 1 | 0.388 | 0.652 | −0.933; 1.710 | .555 | 81.65 |
| Geriatric psychologist | 38 | 1 | 0.869 | 0.706 | −0.562; 2.301 | .226 | 81.39 |
| Tai chi instructor | 38 | 5 | −1.047 | 0.272 | −1.598; −0.496 | .000* | 76.49 |
| Yoga instructor | 38 | 1 | −1.169 | 0.702 | −2.592; 0.254 | .104 | 80.47 |
| Feldenkrais practitioner | 38 | 1 | −0.097 | 0.681 | −1.478; 1.284 | .888 | 81.66 |
| Fitness instructor | 38 | 2 | −0.339 | 0.573 | −1.499; 0.826 | .561 | 81.58 |
| Fall prevention instructor | 38 | 1 | 0.341 | 0.644 | −0.965; 1.647 | .600 | 81.66 |
| Dietician | 38 | 1 | 0.388 | 0.652 | −0.933; 1.710 | .555 | 81.65 |
| Peer mentor | 38 | 1 | 0.446 | 0.620 | −0.811; 1.702 | .477 | 80.83 |
| Caregiver | 38 | 1 | 0.869 | 0.706 | −0.562; 2.301 | .226 | 81.39 |
| Postural stability instructor | 38 | 1 | 0.390 | 0.672 | −0.973; 1.752 | .565 | 81.68 |
| Researcher | 38 | 3 | −0.285 | 0.394 | −1.085; 0.515 | .474 | 81.21 |
| Research assistant | 38 | 1 | 0.408 | 0.672 | −0.955; 1.772 | .547 | 81.67 |
| Physical education student | 38 | 1 | 0.686 | 0.683 | −0.699; 2.070 | .322 | 81.47 |
| Ving tsun coach | 38 | 1 | 0.555 | 0.712 | −0.888; 1.998 | .440 | 81.63 |
| Contact hours with a facilitator | NA | NA | −0.017 | 0.009 | −0.036; 0.002 | .083 | 81.35 |
| Duration of intervention (weeks) | NA | NA | 0.002 | 0.011 | −0.019; 0.023 | .857 | 79.57 |
Note: CI = confidence interval; NA = nonapplicable.
*p < .05.
aThe regression coefficient. For categorical variables, the regression coefficient represents the difference in the SMD between interventions with and without the characteristic in question. For continuous variables, the regression coefficient is the change in the SMD for a one unit change in the intervention characteristic.bActivities of Daily Living.
The setting of interventions was significantly associated with the SMD. Delivery in a community setting was significantly associated with a SMD of −0.528 (95% CI: −0.894; −0.161, p = .006; Table 1), indicating that interventions delivered in the community were more effective in reducing FoF than those that are delivered at home or in a combination of home and community setting. Furthermore, delivery at home (SMD: 0.384, 95% CI: 0.002; 0.766, p = .049) was significantly less effective in reducing FoF, as were written materials (SMD: 0.452, 95% CI: 0.088; 0.815, p = .016). In addition, tailoring resulted in a statistically significant association with the SMD of 0.687 (95% CI: 0.364; 1.011, p < .001), meaning that interventions which were delivered in a tailored format were significantly less effective than those that were not. In general, whether supervision was present, whether the supervisor was experienced in working with older adults or participated in intervision yielded no significant associations, as did most supervisor types. However, supervision by a tai chi instructor was significantly associated with a SMD of −1.047 (95% CI: −1.598; −0.496, p < .001), indicating that interventions which were supervised by a tai chi instructor were more effective in reducing FoF than those that did not include supervision by a tai chi instructor. Duration of the intervention yielded no significant association, but contact time with a facilitator approached significance (SMD: −0.017, 95 % CI: −0.036; 0.002, p = .083), meaning each hour increase in contact time was associated with a decrease in the SMD in FoF of 0.017.
Similar results were obtained when performing meta-regressions without cluster RCTs and with the second (n = 15) or third arm (n = 2) of the intervention (Supplementary File S3). In a meta-regression of study quality—as scored with the Cochrane risk of bias tool—and the SMD, no significant association was found. When performing meta-regressions without outliers, supervision by home care professionals and a combination of strength, balance, and endurance training were significantly less effective in reducing FoF (SMD homecare supervision: 0.725, 95% CI: 0.051; 1.399, p = .036, n = 1 out of 33; SMD strength, balance, endurance: 0.227, 95% CI: 0.018; 0.437, p = .034, n = 6 out of 44). Holistic exercise, supervision by a tai chi instructor, written materials, tailoring, or setting are no longer significantly associated. When performing meta-regressions with a smaller sample of studies which assessed FoF at a long-term follow-up (n = 17), previously mentioned significant results of the main analysis disappear, yet ambulance referral to falls services is significantly less effective in reducing FoF (SMD referral: 0.273, 95% CI: 0.034; 0.511, p = .028, n = 1 out of 17).
Discussion
Main Findings
The present meta-analysis of 50 intervention arms showed that interventions in general, conducted in community-dwelling older people, are associated with a significant small-to-moderate reduction in FoF at the first available follow-up after the intervention (SMD: −0.36, 95% CI: −0.48; −0.24). Most intervention types (e.g., cognitive-behavioral, assessment-based, education, etc.) and overarching characteristics (e.g., supervisor, delivery method, group format, etc.) were not significantly associated with the SMD in FoF at the first follow-up after the intervention. However, interventions with holistic exercise, supervision by a tai chi instructor and delivery of the intervention in a community setting were more effective than interventions without these characteristics. Interventions delivered at home or with written materials and tailoring were significantly less effective in reducing FoF at the first follow-up after the intervention. Sensitivity analysis revealed that these significant results disappear when six outliers are removed, four of which were holistic exercise interventions without tailoring or written materials, delivered in a community setting.
All included studies scored a high risk of bias on two (out of seven) items: blinding of participants and personnel and blinding of outcome assessment. However, blinding of participants is usually impossible in these types of studies, and when the measurement of FoF is based on self-report by unblinded participants, the risk of detection bias is high. As this occurred in all studies, it is unlikely to have had an impact on the findings of this specific analysis.
Previous Research
The majority of interventions included in this study were exercise interventions. In a review which included 41 exercise studies, Büla and colleagues (2011) identified no clear superiority of one type of exercise over others. This was confirmed in a large meta-analysis of 24 exercise studies by Kendrick and colleagues (2014), in which subgroup analyses indicated no significant difference in effect on FoF by different exercise types. These findings were not confirmed in the present study, in which holistic exercise (tai chi, yoga, ving tsun, or Pilates) was significantly associated with the effect, indicating that holistic exercise interventions were more effective in reducing FoF than all other interventions combined. This discrepancy may be due to differences in inclusion criteria and the inclusion of more recent studies, such as the inclusion of the highly effective tai chi intervention by Mortazavi and colleagues (2018). Results correspond with those of a meta-analysis by Rand, Miller, Yiu, and Eng (2011) including 24 studies, in which tai chi was associated with a significant moderate effect size of 0.47 (95% CI: 0.30; 0.63), whereas small significant effects were found for exercise and multifactorial interventions. In addition, effects did not vary with exercise frequency, duration of the intervention, group format, primary aim, and method of outcome measurement in the previously mentioned meta-analysis by Kendrick and colleagues (2014). This is partly confirmed by the results of the current study in which duration of the intervention and primary outcome were not significantly associated with the SMD and similar meta-analytical effects were found for cognitive- and affect-based outcome measures.
Other characteristics which have been investigated previously are setting, delivery method and group format. In a meta-analysis of FoF treatment programs by Jung and colleagues (2009), including six studies, community (n = 2)- and home-based interventions (n = 1) were significantly effective in reducing FoF and facility-based interventions (n = 3) were not. In the current study, interventions delivered in a community setting were significantly more effective than those not solely delivered in the community. No distinction was made between interventions delivered in the community or a facility, such as an outpatient department, in the current study. A few previous reviews investigated the use of virtual reality games. In a review of nine virtual reality studies, Neri and colleagues (2017) found that virtual reality games were superior compared to conventional interventions for reducing FoF. In contrast, in the current study, a meta-regression of delivery through video games yielded no significant association. This is in line with a systematic review and meta-analysis of three studies by Dennett and colleagues (2015) in which computer-based interventions did not differ from physiotherapy in improving falls efficacy or balance confidence in adults. In a meta-analysis of six CBT interventions, individual-based interventions achieved bigger effects than group-based interventions (Liu et al., 2018). In the present study, one of our sensitivity analyses indicated a benefit of group interventions above those delivered individually or in a combination of group and individual. However, the analysis on group format was not limited to CBT interventions in the present study. Finally, a tailored format and delivery with written materials were less effective in reducing FoF when compared to interventions without these characteristics. Tailoring based on an assessment may result in increased awareness of personal risk factors for falls or a confrontation with a poor physical condition, and this may lead to an increase in the perception of vulnerability. Similarly, this may be the case if participants self-monitor themselves by the use of written materials such as an exercise diary. When appropriate tools or skills are not offered to help individuals to cope with this, tailoring may be counterproductive in reducing the FoF. Importantly, the type of tailoring was not considered in this review and may have an influence (Schepens, Panzer, & Goldberg, 2011). In addition, what exactly was delivered through written materials, that is, self-monitoring or exercise instruction, could matter for intervention effectiveness.
Strengths and Limitations
We were able to include 62 unique RCTs. This review is one of the largest overviews of RCTs with FoF as outcome in community-dwelling older people to date. Data extraction was done with a pilot-tested form, ensuring systematic extraction. However, systematic reviews are reliant on published research, which makes them susceptible to publication bias. By searching a wide range of databases and consulting experts worldwide, attempts were made to limit publication bias, but there was evidence of publication bias from the funnel plot and Egger’s test. If studies which show increases in FoF were not included in this meta-analysis, effect sizes may be overestimated. Furthermore, reporting on whether facilitators followed the intervention protocol in practice and whether participants adhered to the intervention program was limited; therefore, these elements were not considered in the current review.
Meta-regressions were conducted with only one independent variable per analysis. Because of small numbers of studies in some of the categories, more extended analysis with several independent variables were not suitable. Furthermore, the small number of studies in some of the categories may have led to insufficient power to detect associations between some of the characteristics and the intervention effects. In addition, due to the exploratory nature of this study, no multiple-testing correction was performed and the significance level was set at 0.05. However, many meta-regressions were performed and this may lead to an increased risk of a type 1 error.
Furthermore, only community-dwelling older people without specific diseases were included. The results of this review may not be generalizable to other populations, such as those with hip fracture or Parkinson’s disease.
Implications and Future Research
The RCTs included in this review were mostly exercise interventions. Additional benefits of holistic exercise interventions versus all other interventions combined were found with meta-regression. Guidelines for falls prevention in, for example, the Netherlands heavily rely on exercise interventions to reduce fall risk (Federatie Medisch Specialisten, n.d.) and tai chi is not yet recommended for those older people with FoF, who may benefit more from tai chi than other types of interventions. Furthermore, intervention effectiveness could also be determined by the people to whom the intervention is delivered. Characteristics of intervention participants may determine whether parameters or conditions for effectiveness of behavioral change methods are fulfilled (Peters et al., 2015). Evidence also indicates that people with poor vision or depressive symptoms are more likely to be severely afraid of falling (van Haastregt, Zijlstra, van Rossum, van Eijk, & Kempen, 2008; Kempen, van Haastregt, McKee, Delbaere, & Zijlstra, 2009). Such persons may require different intervention strategies and the impact of characteristics of participants on intervention effects is understudied. Future research may focus more on the impact of such characteristics, for example, with individual patient data meta-analysis, which would have greater power to detect differences in effect between different patient characteristics. In addition, a limited set of characteristics relating to the supervisor was investigated in the current study. All supervisors were trained to deliver the intervention or had expertise from their professional background, but reporting on years of experience and training was generally lacking and not considered in this review. An analysis on supervisor type was performed, but as some types of supervisors only deliver some types of interventions (e.g., the tai chi supervisor that only delivers tai chi interventions), a categorization based on profession was not always distinctive. Future studies may focus more specifically on supervisor characteristics and intervention effectiveness, for example, by taking into account levels of education and experience, and soft skills, such as communication and empathy. Furthermore, interactions between characteristics and content were not investigated in this review, but may represent an area for future research.
Moreover, the content of interventions is often divided into broad categories. For example, several reviews and meta-analyses investigated the effectiveness of multifactorial or multicomponent interventions (Büla et al., 2011; Whipple et al., 2018). This type of categorization gives rise to several problems. First of all, the term “multifactorial” is used inconsistently; for example, to indicate combinations of exercise and other components or multicomponent interventions in general. Second, this type of categorization may result in interventions appearing similar to each other, whereas in reality there is much variety in intervention components. Although the content of interventions in the current study was categorized in more detail than in several previous reviews, the categorization was still rather broad. A more detailed examination of intervention components is warranted. This would require well-designed RCTs with very detailed reporting on intervention content. Steps in this direction have been made with the TIDieR template for intervention descriptions (Hoffmann et al., 2014), but reporting still leaves much to be desired. Finally, we ideally implement interventions that have an effect on a range of outcomes and individual studies have already shown that next to FoF, multiple outcomes can be affected (e.g., Tomita et al., 2016; Zijlstra et al., 2009). Future meta-analyses may want to evaluate whether, for example, falls risk decreases in those studies in which FoF decreases.
In conclusion, interventions with holistic exercise, supervision by a tai chi instructor, or delivery of the intervention in a community setting were significantly more effective than interventions without these characteristics at the first follow-up after the intervention. Interventions delivered at home or with written materials and tailoring were significantly less effective than interventions without these characteristics. These are potential characteristics to take into account when designing and improving interventions for FoF in community-dwelling older people. Researchers have to weigh to what extent they would like to incorporate these characteristics into their interventions, also considering feasibility and cost-effectiveness.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the following people for acting as an expert during expert consultation: Dr. Will Young, Dr. Nimali Jayasinghe, Prof. Christophe Büla, Prof. Helen Lach, Prof. Elizabeth Walker Peterson, and Prof. Stephen Lord. The authors would like to thank Dr. Estelle Gallo, Dr. Silke Metzelthin, Dr. Ellen Freiberger, Dr. Monika Siegrist, Dr. Steve Parry, and Dr. Yves Lajoie for providing data. The authors would like to thank Gregor Franssen for providing advice on the search strategy and Arthur Loonen and Mae Lim for assisting with data extraction.
Funding
This study was funded by Maastricht University in The Netherlands. The authors received no specific further funding.
Conflict of Interest
None reported.
References
- Büla, C. J., Monod, S., Hoskovec, C., & Rochat, S. (2011). Interventions aiming at balance confidence improvement in older adults: An updated review. Gerontology, 57, 276–286. doi: 10.1159/000322241 [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Collins, L. M., Murphy, S. A., Nair, V. N., & Strecher, V. J. (2005). A strategy for optimizing and evaluating behavioral interventions. Annals of Behavioral Medicine, 30(1), 65–73. doi: 10.1207/s15324796abm3001_8 [DOI] [PubMed] [Google Scholar]
- Dennett, A. M., & Taylor, N. F. (2015). Machines that go “ping” may improve balance but may not improve mobility or reduce risk of falls: A systematic review. Journal of Rehabilitation Medicine, 47, 18–30. doi: 10.2340/16501977-1899 [DOI] [PubMed] [Google Scholar]
- Dorresteijn, T. A., Zijlstra, G. R., Ambergen, A. W., Delbaere, K., Vlaeyen, J. W., & Kempen, G. I. (2016). Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: Results of a randomized controlled trial. BMC Geriatrics, 16, 2. doi: 10.1186/s12877-015-0177-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faes, M. C., Reelick, M. F., Melis, R. J., Borm, G. F., Esselink, R. A., & Rikkert, M. G. (2011). Multifactorial fall prevention for pairs of frail community-dwelling older fallers and their informal caregivers: A dead end for complex interventions in the frailest fallers. Journal of the American Medical Directors Association, 12, 451–458. doi: 10.1016/j.jamda.2010.11.006 [DOI] [PubMed] [Google Scholar]
- Federatie Medisch Specialisten (n.d.). Valrisico verlagende interventies bij thuiswonenden. Retrieved from https://richtlijnendatabase.nl/richtlijn/preventie_van_valincidenten_bij_ouderen/verlaging_valrisico_bij_thuiswonende_ouderen.html
- Fisseha, B., Janakiraman, B., Yitayeh, A., & Ravichandran, H. (2017). Effect of square stepping exercise for older adults to prevent fall and injury related to fall: Systematic review and meta-analysis of current evidences. Journal of Exercise Rehabilitation, 13, 23–29. doi: 10.12965/jer.1734924.462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freiberger, E., Häberle, L., Spirduso, W. W., & Zijlstra, G. A. (2012). Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: A randomized controlled trial. Journal of the American Geriatrics Society, 60, 437–446. doi: 10.1111/j.1532-5415.2011.03859.x [DOI] [PubMed] [Google Scholar]
- van Haastregt, J. C., Diederiks, J. P., van Rossum, E., de Witte, L. P., Voorhoeve, P. M., & Crebolder, H. F. (2000). Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: Randomised controlled trial. BMJ (Clinical Research ed.), 321, 994–998. doi: 10.1136/bmj.321.7267.994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haastregt, J. C., Zijlstra, G. A., van Rossum, E., van Eijk, J. T., & Kempen, G. I. (2008). Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. The American Journal of Geriatric Psychiatry, 16, 186–193. doi: 10.1097/JGP.0b013e3181591c1e [DOI] [PubMed] [Google Scholar]
- Hafström, A., Malmström, E. M., Terdèn, J., Fransson, P. A., & Magnusson, M. (2016). Improved balance confidence and stability for elderly after 6 weeks of a multimodal self-administered balance-enhancing exercise program: A randomized single arm crossover study. Gerontology & Geriatric Medicine, 2, 2333721416644149. doi: 10.1177/2333721416644149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D.,…Sterne, J. A.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research ed.), 343, d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Green, S. (Eds.) (2011a). Cochrane handbook for systematic reviews of interventions. Version 5.1.0. 7.2.6 Measuring agreement. Retrieved from https://handbook-5-1.cochrane.org/chapter_7/7_2_6_measuring_agreement.htm [Google Scholar]
- Higgins, J. P. T., & Green, S. (Eds.) (2011b). Cochrane handbook for systematic reviews of interventions. Version 5.1.0. 9.2.3.2. The standardized mean difference. Retrieved from https://handbook-5-1.cochrane.org/chapter_9/9_2_3_2_the_standardized_mean_difference.htm [Google Scholar]
- Higgins, J. P. T., & Green, S. (Eds.) (2011c). Cochrane handbook for systematic reviews of interventions. Version 5.1.0. 9.5.2. Identifying and measuring heterogeneity. Retrieved from https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm [Google Scholar]
- Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D.,…Michie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ (Clinical Research ed.), 348, g1687. doi: 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- Hosseini, L., Kargozar, E., Sharifi, F., Negarandeh, R., Memari, A. H., & Navab, E. (2018). Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: A randomized control trial. Journal of Exercise Rehabilitation, 14, 1024–1031. doi: 10.12965/jer.1836488.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, D., Lee, J., & Lee, S.-M. (2009). A meta-analysis of fear of falling treatment programs for the elderly. Western Journal of Nursing Research, 31(1), 6–16. doi: 10.1177/0193945908320466 [DOI] [PubMed] [Google Scholar]
- Kempen, G. I., van Haastregt, J. C., McKee, K. J., Delbaere, K., & Zijlstra, G. A. (2009). Socio-demographic, health-related and psychosocial correlates of fear of falling and avoidance of activity in community-living older persons who avoid activity due to fear of falling. BMC Public Health, 9, 170. doi: 10.1186/1471-2458-9-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick, D., Kumar, A., Carpenter, H., Zijlstra, G., Skelton, D., Cook, J.,…Gawler, S. J. (2014). Exercise for reducing fear of falling in older people living in the community. Cochrane Database of Systematic Reviews, 1, Cd009848. doi: 10.1002/14651858.CD009848.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H., & Frank, A. (2010). Tai chi as a balance improvement exercise for older adults: A systematic review. Journal of Geriatric Physical Therapy (2001), 33, 103–109. doi: 10.1002/14651858.CD009848.pub2 [DOI] [PubMed] [Google Scholar]
- Liu, T. W., Ng, G. Y. F., Chung, R. C. K., & Ng, S. S. M. (2018). Cognitive behavioural therapy for fear of falling and balance among older people: A systematic review and meta-analysis. Age and Ageing, 47, 520–527. doi: 10.1093/ageing/afy010 [DOI] [PubMed] [Google Scholar]
- Logghe, I. H., Verhagen, A. P., Rademaker, A. C., Bierma-Zeinstra, S. M., van Rossum, E., Faber, M. J., & Koes, B. W. (2010). The effects of Tai Chi on fall prevention, fear of falling and balance in older people: A meta-analysis. Preventive Medicine, 51, 222–227. doi: 10.1016/j.ypmed.2010.06.003 [DOI] [PubMed] [Google Scholar]
- Logghe, I. H., Zeeuwe, P. E., Verhagen, A. P., Wijnen-Sponselee, R. M., Willemsen, S. P., Bierma-Zeinstra, S. M.,…Koes, B. W. (2009). Lack of effect of Tai Chi Chuan in preventing falls in elderly people living at home: A randomized clinical trial. Journal of the American Geriatrics Society, 57, 70–75. doi: 10.1111/j.1532-5415.2008.02064.x [DOI] [PubMed] [Google Scholar]
- Mahoney, J. E. (2010). Why multifactorial fall-prevention interventions may not work: Comment on “Multifactorial intervention to reduce falls in older people at high risk of recurrent falls”. Archives of Internal Medicine, 170, 1117–1119. doi: 10.1001/archinternmed.2010.193 [DOI] [PubMed] [Google Scholar]
- Malini, F. M., Lourenço, R. A., & Lopes, C. S. (2016). Prevalence of fear of falling in older adults, and its associations with clinical, functional and psychosocial factors: The Frailty in Brazilian Older People-Rio de Janeiro study. Geriatrics & Gerontology International, 16, 336–344. doi: 10.1111/ggi.12477 [DOI] [PubMed] [Google Scholar]
- Markle-Reid, M., Browne, G., Gafni, A., Roberts, J., Weir, R., Thabane, L.,…Henderson, S. (2010). The effects and costs of a multifactorial and interdisciplinary team approach to falls prevention for older home care clients “at risk” for falling: A randomized controlled trial. Canadian Journal of Aging, 29(1), 139–161. doi: 10.1017/s0714980809990377 [DOI] [PubMed] [Google Scholar]
- van der Meulen, E., Zijlstra, G. A., Ambergen, T., & Kempen, G. I. (2014). Effect of fall-related concerns on physical, mental, and social function in community-dwelling older adults: A prospective cohort study. Journal of the American Geriatrics Society, 62, 2333–2338. doi: 10.1111/jgs.13083 [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G.; PRISMA Group . (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortazavi, H., Tabatabaeichehr, M., Golestani, A., Armat, M. R., & Yousefi, M. R. (2018). The effect of tai chi exercise on the risk and fear of falling in older adults: A randomized clinical trial. Materia Socio-medica, 30, 38–42. doi: 10.5455/msm.2018.30.38-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neri, S. G., Cardoso, J. R., Cruz, L., Lima, R. M., de Oliveira, R. J., Iversen, M. D., & Carregaro, R. L. (2017). Do virtual reality games improve mobility skills and balance measurements in community-dwelling older adults? Systematic review and meta-analysis. Clinical Rehabilitation, 31, 1292–1304. doi: 10.1177/0269215517694677 [DOI] [PubMed] [Google Scholar]
- Nguyen, M. H., & Kruse, A. (2012). A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clinical Interventions in Aging, 7, 185–190. doi: 10.2147/CIA.S32600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nick, N., Petramfar, P., Ghodsbin, F., Keshavarzi, S., & Jahanbin, I. (2016). The effect of yoga on balance and fear of falling in older adults. PM & R, 8, 145–151. doi: 10.1016/j.pmrj.2015.06.442 [DOI] [PubMed] [Google Scholar]
- Parry, S. W., Bamford, C., Deary, V., Finch, T. L., Gray, J., MacDonald, C.,…McColl, E. M. (2016). Cognitive-behavioural therapy-based intervention to reduce fear of falling in older people: Therapy development and randomised controlled trial—the Strategies for Increasing Independence, Confidence and Energy (STRIDE) study. Health Technology Assessment (Winchester, England), 20, 1–206. doi: 10.3310/hta20560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters, G., van Schoor, N. M., & Lips, P. (2009). Fall risk: The clinical relevance of falls and how to integrate fall risk with fracture risk. Best Practice & Research. Clinical Rheumatology, 23, 797–804. doi: 10.1016/j.berh.2009.09.004 [DOI] [PubMed] [Google Scholar]
- Peters, G. J., de Bruin, M., & Crutzen, R. (2015). Everything should be as simple as possible, but no simpler: Towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychology Review, 9, 1–14. doi: 10.1080/17437199.2013.848409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirauá, A. L. T., Cavalcante, B. R., de Oliveira, V. M. A., Beltrão, N. B., de Amorim Batista, G., Pitangui, A. C. R.,…de Araújo, R. C. (2019). Effect of 24‐week strength training on unstable surfaces on mobility, balance, and concern about falling in older adults. Scandinavian Journal of Medicine & Science in Sports. 29, 1805–1812. doi: 10.1111/sms.13510 [DOI] [PubMed] [Google Scholar]
- Polinder, S., Haagsma, J., Panneman, M., Scholten, A., Brugmans, M., & Van Beeck, E. (2016). The economic burden of injury: Health care and productivity costs of injuries in the Netherlands. Accident; Analysis and Prevention, 93, 92–100. doi: 10.1016/j.aap.2016.04.003 [DOI] [PubMed] [Google Scholar]
- Rand, D., Miller, W. C., Yiu, J., & Eng, J. J. (2011). Interventions for addressing low balance confidence in older adults: A systematic review and meta-analysis. Age and Ageing, 40, 297–306. doi: 10.1093/ageing/afr037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues, E. V., Valderramas, S. R., Rossetin, L. L., & Gomes, A. R. S. (2014). Effects of video game training on the musculoskeletal function of older adults: A systematic review and meta-analysis. Topics in Geriatric Rehabilitation, 30(4), 238–245. doi: 10.1097/TGR.0000000000000040 [DOI] [Google Scholar]
- Scheffer, A. C., Schuurmans, M. J., van Dijk, N., van der Hooft, T., & de Rooij, S. E. (2008). Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing, 37, 19–24. doi: 10.1093/ageing/afm169 [DOI] [PubMed] [Google Scholar]
- Schepens, S. L., Panzer, V., & Goldberg, A. (2011). Randomized controlled trial comparing tailoring methods of multimedia-based fall prevention education for community-dwelling older adults. The American Journal of Occupational Therapy, 65, 702–709. doi: 10.5014/ajot.2011.001180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist, M., Freiberger, E., Geilhof, B., Salb, J., Hentschke, C., Landendoerfer, P.,…Blank, W. A. (2016). Fall prevention in a primary care setting. Deutsches Arzteblatt International, 113, 365–372. doi: 10.3238/arztebl.2016.0365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, L., Kerse, N., Frakking, T., & Maddison, R. (2016). Active video games for improving physical performance measures in older people: A meta-analysis. Journal of Geriatric Physical Therapy (2001), 41(2), 108–123. doi: 10.1519/JPT.0000000000000078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti, M. E., Richman, D., & Powell, L. (1990). Falls efficacy as a measure of fear of falling. Journal of gerontology, 45(6), P239–P243. doi: 10.1093/geronj/45.6.P239 [DOI] [PubMed] [Google Scholar]
- Tomita, Y., Arima, K., Tsujimoto, R., Kawashiri, S. Y., Nishimura, T., Mizukami, S.,…Aoyagi, K. (2018). Prevalence of fear of falling and associated factors among Japanese community-dwelling older adults. Medicine, 97, e9721. doi: 10.1097/MD.0000000000009721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita, M. R., Fisher, N. A., Ramsey, D., Stanton, K., Bierdeman, L., Kocher, L.,...Wilding, G. (2016). Effects of virtual-group exercise at home (V-GEAH) on adherence and fall risks in older adults with a history of falling. Gerontology & Geriatrics Research, 2(3), 1018. [Google Scholar]
- West, S. G., & Aiken, L. S. (1997). Toward understanding individual effects in multicomponent prevention programs: Design and analysis strategies. In K. J. Bryant, M. Windle, & S. G. West (Eds.), The science of prevention: Methodological advances from alcohol and substance abuse research (p. 167–209). American Psychological Association. doi: 10.1037/10222-006 [DOI] [Google Scholar]
- Whipple, M. O., Hamel, A. V., & Talley, K. M. C. (2018). Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatric Nursing (New York, N.Y.), 39, 170–177. doi: 10.1016/j.gerinurse.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, K. C., Wong, F. K. Y., Yeung, W., & Chang, K. (2017). The effect of complex interventions on supporting self-care among community-dwelling older adults: A systematic review and meta-analysis. Age and Ageing, 47(2), 185–193. doi: 10.1093/ageing/afx151 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2018). Falls fact sheet. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
- Yardley, L., & Smith, H. (2002). A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. The Gerontologist, 42, 17–23. doi: 10.1093/geront/42.1.17 [DOI] [PubMed] [Google Scholar]
- Zhang, J. G., Ishikawa-Takata, K., Yamazaki, H., Morita, T., & Ohta, T. (2006). The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: An intervention study for preventing falls. Archives of Gerontology and Geriatrics, 42, 107–116. doi: 10.1016/j.archger.2005.06.007 [DOI] [PubMed] [Google Scholar]
- Zijlstra, G. A., van Haastregt, J. C., Ambergen, T., van Rossum, E., van Eijk, J. T., Tennstedt, S. L., & Kempen, G. I. (2009). Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: Results of a randomized controlled trial. Journal of the American Geriatrics Society, 57, 2020–2028. doi: 10.1111/j.1532-5415.2009.02489.x [DOI] [PubMed] [Google Scholar]
- Zijlstra, G. A., van Haastregt, J. C., van Rossum, E., van Eijk, J. T., Yardley, L., & Kempen, G. I. (2007). Interventions to reduce fear of falling in community-living older people: A systematic review. Journal of the American Geriatrics Society, 55, 603–615. doi: 10.1111/j.1532-5415.2007.01148.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.