Abstract
Aim: The goal is to explore available evidence and provide greater clarity to what is described as psychosocial intervention to improve cognitive function among older population with MCI as well as identifying areas for future research. Methods: An electronic literature search of PubMed, Cochrane, Ebscohost, Medline, Scopus, and gray resource was conducted to find articles published in English language between 2010 and September 2020. This review focused on research undertaken using randomized clinical trials study design. We extracted information regarding the publication date, geographical location, study setting, intervention mechanism, type of cognitive measurement used, and outcome of the studies. References of this literature were also reviewed to ensure comprehensive search. Result: Out of 240 potential records found, a total of 27 articles were identified following the first round of screening and deletion of duplicates. Full-text article reviews and analysis in the second round of screening narrowed the selection down to four articles. Another three relevant articles obtained from references were also included making a total of seven articles in the final analysis. Findings: Psychosocial intervention strategies for improvement of cognitive function, done in various setting all over the globe, covered a range of approaches including art therapy, visual art therapy, therapeutic writing therapy, reminiscence activity, and cognitive behavioral approach. Most were conducted in weekly basis within 1-to-2-hour duration of session. Cognitive function of older adult in psychosocial intervention group was significantly improved in two studies. Three studies showed no significant improvement at all in the cognitive function, and another one reported success in improving cognitive function over time in the intervention group than in control group. One study did not describe the interaction effect. Different types of cognitive measurement also were used to quantify different domains of cognitive function in the reviewed studies. Conclusion: The idea of using psychosocial intervention for improving cognitive function has begun to increasingly accepted recently. Findings from the limited studies are encouraging, although the outcome of the cognitive function was mixed. Large-scale and longer duration of psychosocial intervention with bigger sample size is warranted for future studies.
Keywords: psychosocial intervention, cognitive function, older adult, randomized controlled trial
Introduction
An individual is said to be cognitively impaired when he/she “has trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life” (Center of Disease Control and Prevention [CDC], 2011). It ranges from mild (apparent changes in cognitive function but still able to live normal live) to severe stage (inability to live independently due to the loss of most of cognitive functions) (CDC, 2011). Mild cognitive impairment (MCI), a pre-dementia condition, is one of the two and the key criterion for cognitive frailty. Kelaiditi et al. (2013) proposed that the MCI is defined by a score of 0.5 in the clinical dementia rating (CDR), without Alzheimer’s disease or another progressive brain dysfunction that would lead to dementia. It is characterized by a significant decline of the cognitive function but intact functional status, more than what is expected for one’s level of age and education (Gauthier et al., 2006; Petersen et al., 2014). MCI is such an intricate, yet golden stage of life as the older adult with MCI are a vulnerable “at-risk” group (Mahendran et al., 2018) but, by aggressive intervention during this stage, it can delay or reverse the occurrence of dementia.
Roberts et al. (2014) found that there is a quite significant risk, up till 29%, for a person to develop MCI and dementia later in their life. Annually, the conversion rate of an MCI person to develop dementia is 13% in clinical sample and 3% in community sample (Farias et al., 2009) and even reach to more than 14% after 1 year and half of follow up (Hussin et al., 2019) This is alarming, in addition to the significant health care burden for dementia treatment (Wong, 2020). The prevalence rate of cognitive frailty has become more compelling. It was range from 35.1% till 80.9% in three samples of De Roeck et al. (2019) study and 13.3% for Liu et al. (2018). Cognitive frailty has taken a terrible toll on the quality of life of its sufferer, as well as giving rise to forms of disability and death (Sugimoto et al., 2018; Panza et al., 2018). Thus, it is considered a worthwhile effort for researchers to explore this aspect of geriatric study.
Cooper et al. (2013) carried out a systematic review on the treatment for MCI, and concluded that pharmacological intervention for this population is of no benefit. As such, this directs attention to non-pharmacological approaches, such as physical, cognitive, and psychosocial intervention. The advantages of this non-pharmacological approach over the pharmaceutical program for the cognitively challenging population has been widely reported in previous studies (Baker et al., 2010; Gates et al., 2011; Ishizaki et al., 2002). Likewise, psychosocial intervention, in particular, has been well recognized as a successful alternative treatment program for persons with dementia (Patel et al., 2014) and Alzheimer (Duan et al., 2018). Aside from the cognitive function, the psychosocial intervention has the advantage of improving social interaction and quality of life of the subjects (McDermott et al., 2019). However, it has only recently been developed as a stand-alone or having the ability to integrate with multidomain intervention for mild cognitive impaired subjects.
Psychosocial intervention is defined as “interpersonal or informational activities, techniques, or strategies that target biological, behavioral, cognitive, emotional, interpersonal, social, or environmental factors with the aim of improving health functioning and well-being.” (Institute of Medicine, 2015: IOM: p. 31). This definition incorporates three main concepts: action, mediators, and outcomes, which if translated into our context, is ANY non-pharmacological intervention aims to change cognitive function and eventually bring improvement in the health symptoms and functioning as well as the wellbeing of an individual.
Vasse et al. (2011) systemically reviewed guidelines and consensus of psychosocial intervention for people with dementia among European countries and concluded that physical activity and carer interventions were recommended the most across all guidelines. Other psychosocial interventions recommended in the guidelines were, (i) Reminiscence (Caltagirone et al., 2005; National Collaborating Centre for Mental Health (UK), 2007), (ii) cognitive behavioral therapy (National Collaborating Centre for Mental Health (UK), 2007; Netherlands Institute for Health Services Research, 2004), (iii) music therapy (Caltagirone et al., 2005; National Collaborating Centre for Mental Health (UK), 2007), (iv) aromatherapy (Caltagirone et al., 2005; National Collaborating Centre for Mental Health (UK), 2007), (v) animal assisted therapy (National Collaborating Centre for Mental Health (UK), 2007), and (vi) massage/touch (National Collaborating Centre for Mental Health (UK), 2007). Whereas World Health Organization (2012), in its guideline for the care of persons with dementia, recommended to consider cognitive and psychosocial interventions applying principles of reality orientation, cognitive stimulation, and/or reminiscence therapy.
For individual with at risk of cognitive decline, few psychosocial interventions have been tried on them. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) trial was a multidomain intervention consists of nutritional guidance, exercise, cognitive training, and social activity (Kivipelto et al., 2013). Numerous group meetings of all intervention components are considered as stimuli for social participation and connectedness. Participants were also had a visit to their local Alzheimer Society offices. Multidomain Alzheimer Preventive Trial (MAPT study) also offered almost similar types of intervention (except for social activity) for their at-risk participants in France (Vellas et al., 2014). A more recent multidomain intervention offered for cognitively impaired older adult was done by Murukesu et al. (2020) by the delivery of WE-RISE Trial which consist of the prescription of physical exercise, cognitive training, dietary counseling, and promotion of psychosocial support. Meanwhile, Schechter et al. (2020) offered a 4-day retreat of coaching on the healthy lifestyle choices, including cooking, stress management, sleep, exercise programs, and an introduction to brain stimulation activities.
Aim and Review Question
This scoping review aimed to explore the psychosocial intervention undertaken in addition to its key mechanism, leading to its efficacy in bettering the cognitive function in cognitively impaired older adult population. The research question established for the scoping review was formulated as follows: “What are the psychosocial interventions readily available in literature for improving cognitive function among mild cognitive impaired older adults?”. The research question formulated through an iterative approach that reflected the population, concepts, and context of interest in the review (Peters et al., 2020).
Method
The current study was undertaken to identify and map the available evidence on recent psychosocial intervention carried out in a randomized controlled trial to improve the cognitive function among older adults with no known neurodegenerative and dysfunction condition. We are also looking into the gap from previous researches as well as the potential area of exploration in psychosocial intervention for MCI older adult in future studies. In order to produce a thorough and systematic overview, the framework from Arksey and O’Malley (2005) was adopted, except the optional step, the step 6 (consultation with stakeholders). A comprehensive search to identify primary studies published between 2010 and September 2020 was performed using different sources namely PubMed, COCHRANE, Scopus, and Ebscohost Medline. We also searched the gray literature, namely Google Scholar for information. Key search terms, including synonyms were entered into these databases in systematic manner. The searches included the following terms: (“psychosocial intervention” OR “psychosocial approach” OR “psychosocial modality” OR “psychosocial participation”) AND (“improve” OR “correct” OR “enhance” OR “promote” OR “better”) AND (“cognitive frailty” OR “cognitive impairment” OR “cognitive decline”) NOT “dementia” NOT “Alzheimer” NOT “cognitive stimulation therapy”. These terms were searched as keywords, titles, and abstracts.
In the second stage, we screened the literature, searching for papers that included the use and application of any form of psychological intervention, undertaken only in a randomized control trial (RCT) designed study, aiming for bettering the cognitive function in an ageing population. Reference tracking was also carried out (i.e., checking reference lists of included sources) to identify additional articles to ensure no information was omitted that was considered valuable to the study. The third stage, selection of studies, was guided by applying the researcher’s inclusion and exclusion criteria for the articles.
Eligibility Criteria
The inclusion criteria included: (1) primary, randomized controlled trial studies, (2) passive (waitlist or no-training) or active control group(s), (3) participants aged 55 and above, (4) subjects showing either no cognitive impairment or with MCI as diagnosed by standard, generally accepted diagnostic criteria or no known and reported neurodegenerative condition (e.g., Dementia, Alzheimer, Parkinsonian Dementia, Schizophrenia and stroke), and (5) cognitive function in one or more domains or global cognition function as a primary or secondary outcome. The exclusion criteria included: (1) protocol for RCT or Quasi RCT, (2) studies involving cognitive training like cognitive stimulation, cognitive rehabilitation and cognitive remediation therapy, (3) physical and nutritional intervention, and (4) mixed samples where data cannot be extracted for a subgroup of an older adult.
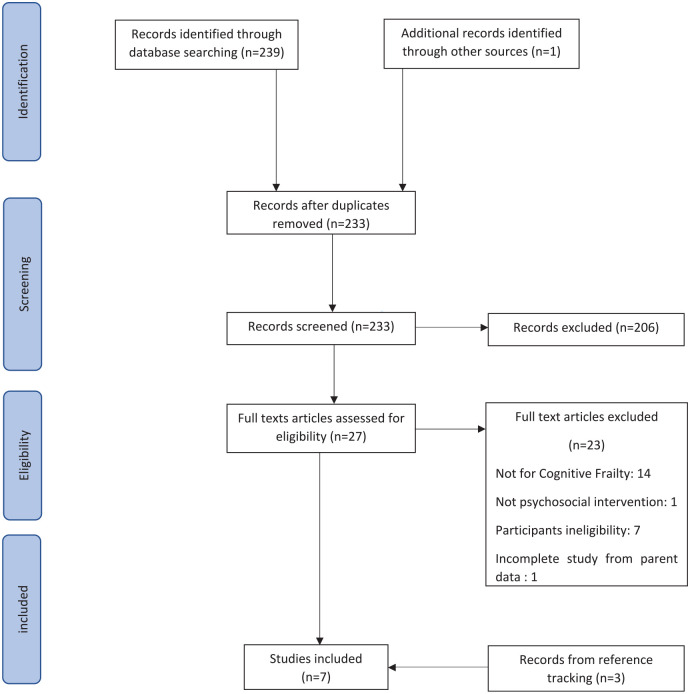
A reviewer screened the titles and abstracts against the specified inclusion and exclusion criteria independently. Any duplicates were subsequently removed. The same reviewer then independently screened the full-text articles to determine relevant articles for analysis. Any confusion regarding the selection of studies or articles during the screening process were resolved through discussion with senior members in the research team. When several articles were published from the same parent study or dataset, all articles were screened, and only one would be included in the analysis based on the completeness of the report. Search results were limited to English language journals, and only articles written in English were selected for final analysis. PRISMA extension for scoping review (PRISMA-ScR) guidelines were followed, as illustrated in the flow chart in Figure 1.
Figure 1.
PRISMA flow diagram.
Following the extraction of the data, the studies were categorized and tabulated based on (i) the study purpose, (ii) participants criteria, (iii) study setting and location, (iv) baseline of the cognitive function, (v) type of intervention, (vi) intervention duration and intensity, (vii) background of the treatment provider, (viii) measure of the cognitive outcome, and (ix) efficacy of the intervention (see Table 1). Scoping reviews did not require a rigorous quality assessment as compared to systematic reviews (Arksey & O’Malley, 2005).
Table 1.
Summary of the Available Evidence on Psychosocial Intervention for Improving Cognitive Function among Older Adult.
| Author year country | Participants | Setting | Psychosocial intervention | Duration and frequency | Measurement for cognitive outcomes | Findings |
|---|---|---|---|---|---|---|
| Mahendran et al. (2018) Singapore | A total of 68 elderly people, aged 60 to 85 years, (M = 71.1) both genders, fulfill Petersen’s criteria for MCI |
Community dwelling | AT: two components: (1) Guided viewing and cognitive evaluation of art works at the respective sites, involved narration of thoughts and inner experiences (2) visual art production (physical creation of themed artwork was followed by image appreciation activities to gain insight and discuss feelings, and took place at the research center) MRA: Listening and recalling memories and experiences related to the music. |
weekly for 3 months, then fortnightly for 6 months Average: 1 hour |
Memory: Rey auditory verbal learning test (RAVLT) List Learning, Delayed Recall, Recognition Trial Visuospatial abilities: Wechsler Adult Intelligence Scale-third edition (WAIS-III) Block design Attention and working memory: Digit span forward executive function: Color trails test 2 |
Mean of all neurocognitive domains in AT is significantly higher than CG at the third month Significant improvement only seen in List Learning and Digit Span Forward in AT compared to CG from baseline to 3 months assessment (estimated mean change) The effect of AT on memory domain was also sustained at 9 months. |
| Pitkala et al. (2011) Finland | A total of 235 participants (≥75 years) (M = 80, SD = 3.6) MMSE ≥ 19 CDR ≤ 1 |
Seven daycare centers | Art group: various artists (musicians, actors, artists, etc.) attended the meetings, and participants visited cultural events and sights, also actively producing their own art. They discussed their experiences in their group. therapeutic writing groups: the participants wrote about their past, their loneliness, and their feelings about the group meetings. They shared their writings and experiences in discussions with their group members and reminisced about their pasts. All interventions were solely use to stimulate social engagement of the partcipants Participants had breakfast together, engaged in activity, discussion of the activity, continued with lunch in the group, again engaged with activity, followed by discussion about it over coffee. |
Weekly session for 3 months (12 sessions) 6 hours/session |
Alzheimer’s Disease Assessment Scale (ADAS-Cog) | ADAS Cog scale improved more in the intervention group than in the control group within 3 months period. When compared between groups, subgroup therapeutic writing showed significant improvement in ADAS-Cog scale compared to their control groups, where the difference between art and exercise interventions and their controls were not significant. Dimension “mental function” in 15D showed significant improvement at 12 months in the IV compared to control group |
| Masika et al. (2021) Tanzania | A toal of 39 participants, 60 years or older (M = 72.7, SD = 7.1) and diagnosed with MCI by a psychiatrist using DSM (V). | community dwelling | Visual Art Therapy using Zentangle Method the first two sessions focused on understanding the basic ingredients of Zentangle art, that is, a dot, line, circle, and curved lines, and how to put together these elements to make shapes, space, form, texture, color intensity, and value. During the third session, participants made some attempts by following the principles learned in sessions 1 and 2 to draw some patterns and simple objects. To enhance participants’ socializations and build their other cognitive and social skills, they used session 4 to present their work in plenary, to evaluate one another’s work, and to provide feedback to each other. Sessions 5 and 6 were the repeat of sessions 3 and 4 to enhance the basic skills. The second part of VAT involved expression of life experiences into art. This included making the drawings using the principles of Zentangle art learned in sessions 1 to 6 to narrate their memorable objects, their life experiences, and portraits of their loved people and then sharing the art and the story behind such moments in session 7 to 12 |
Twice weekly for 6 weeks (12 sessions) | Montreal Cognitive Assessment-5-minute protocol (MoCA-5-minutes) Focus Group Discussion (FGD) |
Both VAT and HE showed significant improvement in cognitive scores in post intervention assessment. But Insignificant improvement of MoCA-5-min scores between VAT and HE groups (group × time effect) FGD: Perceived brain challenges and improved memory “. . .it is a good brain exercise for old people. . .” (P4) “in the past, I would be home, then I would go to kitchen to pick somethings. . ...i would stand still having forgotten what I have gone to the kitchen for. . ...nowadays I don’t forget as before.” (P12) |
| Belleville et al. (2018) Canada | A 145 older adults aged above 55 years old (Mean = 72.2 ± 7.2) meeting criteria Petersen criteria for amnestic MCI | memory clinics | Psychosocial intervention based on the cognitive-behavioral approach, and aims to improve general psychological well-being. Session 1 focuses on psychoeducation, exploring the links between activities, aging, and psychological well-being. Participants are also invited to identify satisfactory aspects of their lives and to find ways to increase positive situations. Session 2 focuses on cognitive restructuring of thoughts, beliefs, and attitudes to help participants understand their relationships and modify thoughts that cause unhelpful emotions and includes diaphragmatic breathing. Sessions 3 and 4 consist of behavioral activation to increase the level of daily activities. Session 5 introduces participants to problem-solving skills, for instance, ways to manage stressful life events. In Session 6, participants learn to manage their anger and frustration Sessions 7 and 8 review key concepts and consolidate knowledge |
Weekly session for 2 months (eight sessions) 2 hours A booster dose 1 week after 3 months |
immediate and delayed composite performance memory score | No significant improvement on cognition in psychosocial intervention as compared to CT |
| Nakatsuka et al. (2015) Japan | A 127 older adult aged ≥75 years (mean CI = 82.2 ± 3.8, PA = 81.3 ± 3.8, GRA-RO = 81.2 ± 4.0) and evaluated as having a CDR of 0.5 | community-dwelling | About 12 group sessions and 12 home assignments, weekly session. Home assignments were designed according to the intervention methods and contained tasks that require about 1 hour to be completed. Group Reminiscence Approach-Reality Orientation: talks about the current days and events of daily life (reality orientation) and discussions about memories of earlier days (reminiscence approach). The timetable of each session contained a reality orientation part (10 minutes) and a set of reminiscence approach parts (50 minutes in total). Topics included activities, jobs, events, and experiences from earlier days including childhood and adolescence. Pictures or items that related to these topics were also presented as an aid to discussion |
Weekly for 3 months (12 sessions) 1 hour | MMSE word fluency (WF) Trail Making Test part A (TMT-A) |
Significant improvement for MMSE, Word Fluency (WF) and Trail Making Test Part A (TMT-A) between IG (GRA, Physical Activity group, Cognitive Intervention group) and CG after 3 months. Post Hoc: significant improvement of MMSE only in CI and PA group only |
| Zhao et al. (2018) China | A total of 93 participants aged 60 years or older (M = 69.2, SD = 6.3) MCI (by Chinese guideline for cognitive impairment and dementia) |
hospital | Creative Expressive Therapy group 25 sessions over 16 weeks, facilitated by a group of professional therapists. All sessions began with a 5 to 10 minutes warm-up of an interaction game, followed by a 10 minutes drawing and then a 30 minutes core CrExp. Session ended with a 5 to 10 minutes discussion and a 5 minutes conclusion. Storytelling is used to strengthen memory. Conducted in group setting, CrExp program involves five steps of functional tasks related to the presentation of a picture, including the topic of the picture, the background scenery, the development of a story, the actions of the leading character, and the ending of the story. Symbols, graphs, lines, numbers, and colors can be used to express feelings or emotions in order to narrate a vivid and complete story during the task. |
16 weeks 25 sessions (Average: 1 hour) | Chinese-Changsha version of Montreal Cognitive Assessment (MoCA) Chinese Version of the Auditory Verbal Learning Test Chinese Version of the Category Verbal Fluency Test Digital Span Test Chinese version of the Trail Making Test A and B |
At postintervention, patients receiving CrExp therapy scored significantly higher than patients receiving standard cognitive training, in general cognitive functioning, memory, executive function, functional status, and everyday living ability. At 6 months follow up, significant group differences remained in MoCA, memory, executive function, and attention functioning |
| Ciasca et al. (2018) Brazil | A 56 older adult aged 60 years or older (mean CG 69.8 ± 6.4, IG 66.1 ± 5.7), ability to read and write, lifetime DSM-5 diagnosis of MDD, female, participants had to be stable on pharmacotherapy for depression, that is, with no change in medication regimen (agent or dosage) throughout the study period MMSE score above 25 for people with 1 to 4 years of formal schooling or above 27 for people with 5 years or more of schooling |
hospital | Art Therapy Relaxation and guided imagery by inducing the participants to imagine a nature setting of their choice. Then, the topic for artistic creation during the session was proposed After the guided imagery activity, the art therapist instructed the participants to work out the topic that had been proposed, using the art supplies available. Techniques such as painting, drawing, clay modeling, weaving, and collage. Example of activity; fashion a mandala out of grains and seeds glued onto a piece of cardboard, and were told that each grain or seed was to represent a quality they recognized in their personality. “Difficulty in dealing with difficult situations” was worked through by providing participants with rocks, which they were instructed to “place in a more beautiful context” within their artworks, thus helping them change their outlook on the situation. Once the artworks were completed, each participant was invited to verbally express her reflections and any feelings that surfaced during the activity. |
Weekly session for 20 weeks Average: 1.5 hour |
MMSE Verbal Fluency Test (animal category) Trail Making Test Rey Complex Figure (Rey CF) task |
Significant higher score of MMSE and Rey DR from baseline to post intervention in IG. No significant difference between IG and CG in terms of the change in cognitive battery scores (group × time) |
Data Analysis
The results were summarized applying a narrative descriptive synthesizing approach. As there was heterogeneity in the study’s inclusion criteria, interventions, frailty assessment tools, and outcomes, a pooled analysis was considered not appropriate to be conducted.
Patient and Public Involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research. Dissemination of the result of this study for these groups is also not applicable.
Results
Participants
The scope of the review only covered psychosocial interventions carried out among older adults with MCI. The interventions involving senior subjects suffering from neurodegenerative diseases such as dementia, Alzheimer, Parkinsonian Dementia were excluded. Any intervention involving schizophrenia and stroke patients was also omitted from the analysis since schizophrenia is a neurocognitive dysfunctional disease (Rund, 2009). Ong et al. (2017) asserted that stroke attack would undoubtedly lead to a neurodegenerative like condition at the site of the initial infarction. Both conditions would, therefore interfere with our subjects’ cognitive functions and the outcome.
The participants for the interventions included in the analysis were comparatively at a similar level of cognitive function, although the measurements varied. Three of the studies engaged as MCI labeled participants, all measured differently. Each person was labeled or “tagged” applying the Petersen criteria (Mahendran et al., 2018), Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (Masika et al., 2021), and applying the Chinese guideline for cognitive impairment and dementia (Zhao et al., 2018). In Belleville et al.’s (2018) study, the participants were those who were amnestic MCI applying Petersen’s criteria, while the rest three studies used MMSE and CDR as baseline measurement of their participants. Subjects in Nakatsuka et al.’s (2015) study scored 0.5 in their CDR scale, while Pitkala et al. (2011) allowed only subjects with a score of 19 and above for Mini-Mental State Exam (MMSE) and score one (1) and below for CDR to participate in their study. It is interesting to note that in Ciasca et al.’s (2018) study, formal education received determined the MMSE score for the inclusion criteria. Only those participants who scored above 25 and having between 1 and 4 years of formal schooling or scoring above 27 for people with 5 years or more of schooling in MMSE testing were eligible to participate in the study. The age range for all participants ranged from 55 years and above. A special condition of the participants was related to illiterate subjects (Masika et al., 2021) and participants diagnosed with major or chronic depression disorder (Ciasca et al., 2018).
Study Location and Setting
All studies ranged from various countries, namely, Asia (3), Europe (2), Africa (1), and South America (1). The studies conducted in Asia were from Japan (Nakatsuka et al., 2015), China (Zhao et al., 2018), and Singapore (Mahendran et al., 2018). One study was conducted in Canada (Belleville et al., 2018), Finland (Pitkala et al., 2011), Tanzania (Masika et al., 2021), and Brazil (Ciasca et al., 2018). Regarding the setting, the MCI participants in three studies were community-dwelling older adults (Mahendran et al., 2018; Masika et al., 2021; Nakatsuka et al., 2015) totaling 201 participants (28% of total subjects). However, the majority of subjects were from day centers (Pitkala et al., 2011), accounting for 32% of all participants (235 subjects). The remainder were recruited from hospitals (Ciasca et al., 2018; Zhao et al., 2018) and memory and cognition clinics (Belleville et al., 2018).
Cognitive Measurement
Surprisingly, even though all of the interventions aimed to improve the cognitive function, they differed in the respective domain under examination in addition to the measurement employed. Some studies attempted to address as many domains as possible, as seen in Mahendran et al. (2018) and Zhao et al. (2018). Mahendran et al. measured (1) memory outcome using the Rey Auditory Verbal Learning Test (RAVLT), List Learning, Delayed Recall, Recognition Trial; (2) Visuospatial abilities using the Block Design subtest of the Wechsler Adult Intelligence Scale-third edition (WAIS-III); (3) Attention and working memory by the Digit Span Forward subtest of WAIS-III; and (4) Executive function through Color Trails Test 2.
Meanwhile, Zhao et al. (2018) quantified the cognitive functions by the Chinese-Changsha version of the Montreal Cognitive Assessment (MoCA), Chinese Version of the Auditory Verbal Learning Test, Chinese Version of the Category Verbal Fluency Test, Digital Span Test, the Chinese version of the Trail Making Test (A and B) in addition to the Chinese Version of Activities of Daily Living scale (CVADL). The remaining studies measured cognitive outcome either using a stand-alone global cognitive measurement, such as the Alzheimer’s Disease Assessment Scale (ADAS-Cog) in Pitkala et al. (2011) or as a combination with another measurement mechanism; Montreal Cognitive Assessment-5-minute protocol (MoCA-5-min) and via Focus Group Discussion (FGD) (Masika et al., 2021); MMSE, word fluency (WF) and Trail Making Test part A (TMT-A) (Nakatsuka et al., 2015); MMSE, Verbal Fluency Test (animal category), Trail Making Test, and the Rey Complex Figure (Rey CF) task (Ciasca et al., 2018). Belleville et al. (2018) used some aspects of different measurements when they opted for the immediate and delayed composite performance memory score.
Intervention
In this scoping review, a diverse range of intensity and duration of the interventions were employed by the researchers for MCI subject in their studies. Most were conducted weekly, but differed in the duration, range from 2 until 5 months (Belleville et al., 2018; Ciasca et al., 2018; Nakatsuka et al., 2015; Pitkala et al., 2011). The intervention in Mahendran et al.’s (2018) study was also performed via weekly sessions for 3 months but continued fortnightly for the next 6 months. A more intensive, but shorter duration intervention was undertaken by Masika et al. (2021) twice weekly for 6 weeks. Zhao et al. (2018), on the other hand, administered their intervention within 25 sessions over 16 weeks. All of the sessions lasted between 1 and 2 hours except in Pitkala et al.’s (2011) study where each intervention session lasted around 6 hours on average. Masika et al. (2021) did not mention the duration of the session.
The psychosocial intervention used to improve the cognitive function in this MCI older adult population was quite diverse with respect to using art as therapy. The more recent study by Masika et al. (2021) utilized visual art therapy in achieving this aim. The training was undertaken using an exclusively developed approach for illiterate subjects, namely the Zentangle method. The basic ingredients of Zentangle art method are how to put together a dot, line, circle, and curved lines, into shapes, space, form, texture, color intensity, and value. MCI participants were asked to draw using the principles of Zentangle art learned to narrate their memorable objects, their life experiences, and portraits of their loved one’s before sharing the art and the story behind such moments in the session.
Nakatsuka et al. (2015) conducted a group reminiscence approach with reality orientation (GRA-RO) as their intervention against a control group. The approach was a combination of discussion of daily life activities (Reality Orientation) with memories of earlier days with pre-planned themes. Picture and items related to the themes were also presented to facilitate the session. Another reminiscence approach was employed by Mahendran et al. (2018) as one of its two psychosocial arm interventions. Music was also used as a tool for a recalling session and subsequent discussion. However, only one study used a cognitive behavioral approach in their intervention (Belleville et al., 2018), where the aim was to enhance the general psychological well-being of the MCI subject. The elements included (1) psychoeducation on the links between activities, ageing, and psychological well-being; (2) cognitive restructuring of thoughts, beliefs, and attitudes; (3) behavioral activation; (4) problem-solving skills; and (5) anger management.
Although the key mechanism of each study differed slightly, the most adopted psychosocial intervention in a reversal of cognitive impairment observed in this scoping review was using art as therapy, either labeled as art therapy as in Mahendran et al. (2018) and Ciasca et al. (2018), visual art therapy as in Masika et al. (2021) and creative expressive therapy in Zhao et al. (2018). Art therapy in Mahendran et al.’s (2008) study, comprised of two components, viewing and cognitive evaluation of existing artwork and visual art production. Both components were accompanied by thought narration and discussion on the subject’s feelings after the sessions.
On the other hand, art therapy in Ciasca et al.’s (2018) study was slightly differed, involving the imagination of a nature setting and determining the artistic output based on the proposed topic, using a series of techniques, such as painting, drawing, clay modeling, weaving, using materials available such as grains, rock, seeds, and straw. MCI participants were invited to express their feelings and reflections once the artwork was verbally completed in their minds. The use of drawing in the intervention continued in Zhao et al.’s (2018) study, though involved a more detailed process in the presentation of the picture. Storytelling was used for the presentation, involving five functional steps; (1) topic of the picture; (2) background scenery; (3) development of the story; (4) actions of the leading character; and the (5) ending of the story.
Art therapy was also used in Pitkala et al.’s (2011) study, but solely as the stimuli for group discussion, and not as the key intervention. The participants in the art group visited cultural events and sights as well as actively producing their own art. These activities served as a tool to enhance active communication between the participants. Moreover, they experienced newly developed friendships from the interaction as they began to share their feelings on sensitive issues and matters, giving critique to each other and supporting each other. Notably, Pitkala et al.’s study was conducted on average, 6 hours per session. The participants ate breakfast together, engaged in the activity, discussed the activity, continued with lunch engaging in the activity, followed by a group discussion over tea and coffee. No unique cognitive stimulating approach was made, and all sessions were planned openly allowing group members to have the opportunity to influence the program.
Intervention Outcomes
Multiple methods have been employed to analyze and interpret the data obtained in this study, though the results varied. The art therapy group in Mahendran et al. (2018) showed significant improvement in all of its neurocognitive domain compared to the control group after 3 months of applying the intervention. However, when examining the estimated mean change, this significant improvement was only evident in List Learning and Digit Span Forward. Relatively similar findings were observed in another study by Masika et al. (2021) when their art therapy groups obtained a significantly higher score in the cognitive battery from the baseline to post-intervention in comparison to the control group, but this effect abolished when the group-time interaction effect is considered.
However, a qualitative report by one of the participants in Masika et al. (2021) cited that, “in the past, I would be home, then I would go to the kitchen to pick something. . .I would stand still having forgotten what I had gone to the kitchen for. . .nowadays I don’t forget as before”. Whereas Zhao et al. (2018) only reported that at post-intervention, MCI patients receiving their creative expression therapy scored a significantly higher compared to the patients receiving standard cognitive training, in general, cognitive functioning, memory, executive function, functional status, and everyday living ability, in which this effect lasted after 6 months follow-up in MoCA, memory, executive function, attention functioning, ADL, and memory satisfaction. Meanwhile, improvement of ADAS-Cog within 3 months’ time in Pitkala et al. (2011) was significantly mediated in a therapeutic writing group compared to the other intervention as compared to their control groups. Follow-up assessment after 12 months of 15D also revealed a significant improvement in the intervention group in the “mental function” dimension as compared to the control. However, no significant improvement on cognition by the psychosocial intervention was evident as compared to the control group in three studies (Belleville et al., 2018; Ciasca et al., 2018; Nakatsuka et al., 2015)
Discussion
The principal strength of this scoping review solely rests on its selection of only randomized controlled trial (RCT) designed studies. A RCT is considered a favored design to evaluate the effects of an intervention onto the subject since it controls selection bias occurred in any clinical trial and nullify its influence from being mistakenly considered as a treatment effect. Therefore, RCT is the best way to rule out biases that could underestimate or over-estimate the true effects of the intervention. In the current review, RCT interventions investigated were undertaken in several countries that included Asia, Europe, South America, and Africa. As such, this is not a western country type approach which may be viewed as a superior concept. The difference between the studies is evident on the type of control groups, as they are either a waitlist group (passive control) or receive other interventions (active control) such as health education (as in Masika et al., 2021), standard cognitive training (as in Zhao et al., 2018) or cognitive and physical intervention (as in Nakatsuka et al., 2015).
Even though there is ongoing contention between the effect of using these two groups (passive and active control groups) and the advantages of passive control over another, significant cognitive improvement of the subject in the experimental group compared to the active control group can be considered to be a strong indicator for psychosocial intervention effectiveness, especially if the active control group directly stimulates the cognitive function. Notably, all studies included in this scoping review were only recently undertaken (2010–2020). In addition, only-RCTs were selected; thus, the study could not describe and explore the growth of psychosocial interventions in the MCI older adult population from its earliest time.
Wherever possible and feasible, a study on the effect of the psychosocial intervention among the MCI older adult population should focus on the special needs’ subpopulation. In this scoping review, two special conditions relating to MCI subjects were mentioned; illiteracy (Masika et al., 2021) and major depressive disorder (MDD) (Ciasca et al., 2018). The inability to write and read, resulting from having no formal or informal education may exemplify the needs of the psychosocial intervention since it offers a broader range of approaches. Likewise, the limitation of formal education has a strong relationship with low cognitive function in older adults in previous studies (Brigola et al., 2019; Mohd Zulkifly et al., 2016; Razali et al., 2012) which offer strong justification on the use and application of the psychosocial intervention in this subpopulation.
Positive relationship between depression and level of cognitive function has been well demonstrated by previous studies (Ganguli, 2009; Rivan et al., 2020). Even though MDD does not impact the cognitive function directly, several core symptoms, such as psychomotor retardation, motivation, fatigue, insomnia, and mood disturbances may mediate for cognitive dysfunction later for these patients (Lam et al., 2014). Hence, the needs for such intervention in this subpopulation. It can be argued that the use of medication for MDD may have intruded on the judgement for intervention efficacy. However, researchers should attempt to minimize this confusion by ensuring there is no change in medication regiment, regarding dosage or agent, throughout the study period and patients are in their best condition under the current dose, as what was achieved by Ciasca et al. (2018). Also, while only two special conditions were examined in this study, future research should explore other disabilities, such as disabled veterans or MCI older adults with the post-traumatic disorder. Further, none of the interventions examined the effect of gender and ethnicity/culture on the intervention, which may serve as the foundation for future investigation.
Presently, the majority of evidence has shown a preference for art (in a broader category, e.g., including drawing, music, storytelling, writing, etc.) as the central concept in psychosocial intervention for MCI older adult population. A typical art session that involves art production, reminiscence, output presentation as well as a cognitive process during interpretation, evaluation, and discussion after the session is believed will physiologically, cognitively, and socially stimulate cognitive and functional improvement. The production of the art itself has benefited the participants cognitively through the stimulation of fine motor skill coordination, visual-spatial memory, abstract thinking, and executive function (Safar, 2014). Verbal presentation of the output relies on the “dual coding theory” of the memory task, which suggests that both visual and verbal data are used to organize memories, either to act upon, to store, and retrieve for subsequent use (Katz, 2017).
Social participation theoretically gives rise to cognitive stimulation by its stimulating environment, engagement, and sense of self-efficacy perceived by the participants (Park et al., 2007). Reminiscence therapy, in whatever techniques employed, directly acts on the memory function of the brain; thus, it can be argued that it is rather a cognitive training, than psychosocial therapy. The only study that differed significantly from the other studies in this scoping review was that of Belleville et al. (2018), which opted for the cognitive behavioral approach as their psychosocial intervention.
The method based on psychoeducation and cognitive restructuring to modify the behavior among participants is believed to improve the cognitive function in several ways. First, CBT is emphasized on complex brain tasks, such as learning and retaining new cognitive and social coping skills and strategies, recognizing and challenging problematic cognitions, which then, hopefully, form a new set of healthy behaviors. However, most of these may not be possible for a person who has attention/concentration deficit and/or difficulties in inhibiting his/her behaviors (Carroll et al., 2011). Hence, CBT is a worthy option for researchers to consider in achieving their aim to find the best intervention for the MCI older adult population. However, such imbalance in these types of psychosocial intervention, along with other unexplored options, for the MCI older adult population raises the “why?” question, which needs to be responded to in future studies.
It should also be highlighted, that the choice of outcome measures employed by researchers has a level of heterogeneity even within similar interventions, either by single general cognitive measurement, mixed-method with qualitative analysis or several cognitive measurements, each to different cognitive function. However, it is unclear if this is derived by the researcher’s preference or as consideration for the participants who might not like answering long, complicated questionnaires. MCI subjects also defined by different criteria and measures at the baseline and this gives rise to the validity of the comparison between outcomes. One study even used their own definition of cognitive dysfunction. Zhao et al. (2018) employed Chinese guideline for cognitive impairment and dementia which requires the participant to fit in these requirements; (1) memory/cognitive complaint reported by the patient or a caregiver within the past year, (2) clinical record of probable MCI according to the Diagnostic and Statistical Manual of Mental Disorders, fourth Edition (DSM-IV), (3) objective cognitive impairment in one or more domains as revealed by neuropsychological assessments, and (4) normal personal self-care and daily living ability. The significant lower baseline score using only one measure even predicts significant improvement, as seen in Nakatsuka et al.’s (2015) study, let alone if comparing the outcome between studies using different means. The other gap found in the literature resides in the lack of long-term follow-up following the intervention. Here, only three of the seven studies investigated this aspect.
Having said that, post-trial follow-up is vital in order to observe if the effect persists long after cessation of the treatment (Heart Protection Study Collaborative Group, 2011). Some barriers, which may interfere with the treatment, are only visible after quite some time, thereby making it more crucial for researchers to conduct follow-up assessments. The nature of RCT which can only accommodate a relatively small sample in the study, in addition to the fact that two were only pilot studies, may not represent a similar outcome if conducted in a larger sample size for MCI older adult population. Another limitation of the study is that all retrieved articles were not subjected to a quality assessment and also, no information was reported on the economic evaluation of the psychosocial intervention in the studies (except in Pitkala et al., 2011), despite the apparent human resource and societal cost derived from it.
It would be useful to compare the costs in conducting the psychosocial intervention compared to conventional and control groups as it will provide the stakeholder with the costs generated besides the gained benefits. All of these gaps could be addressed by researchers going forward. Medical and social support practitioners may also benefit from these findings by screening and incorporating the best type of psychosocial therapy in their interventions since one size does not fit all, and every target population is in itself, quite unique.
Conclusion
We were able to identify several gaps in conducting the psychosocial intervention among MCI older adult population including the unexplored growth of the psychosocial intervention over time due to the limited designed scope, scarcity in the type of approach used, non-repeatability of the intervention in diverse subpopulation and limited methodological aspects which warrant for more rigorous study among researchers. This also means uniqueness for future studies as well as enrichment in adding to the existing pool of knowledge in this domain. Lastly, options and the effectiveness of psychosocial interventions should be presented clearly so that the geriatric therapist can acquire a better understanding of the intervention in better serving their MCI subjects.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is part of a larger project named Multi-domain Intervention for Reversal of Cognitive Frailty: Towards Personalized Approaches (My-AGELESS Trial) funded by the Ministry of Higher Education of Malaysia under the LongTerm Research Grant Scheme (LRGS/1/2019/UM-UKM/1/4).
Ethical Statement: This study has obtained ethical approval from Research Ethics Committee National University of Malaysia (UKM/PPI/111/8/JEP-2020-34).
ORCID iDs: A’isyah Mohd Safien  https://orcid.org/0000-0001-7522-0356
https://orcid.org/0000-0001-7522-0356
Ponnusamy Subramaniam  https://orcid.org/0000-0002-2361-4780
https://orcid.org/0000-0002-2361-4780
Arimi Fitri Mat Ludin  https://orcid.org/0000-0003-1517-2115
https://orcid.org/0000-0003-1517-2115
Reference
- Arksey H., O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory & Practice, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Baker L. D., Frank L. L., Foster-Schubert K., Green P. S., Wilkinson C. W., McTiernan A., Plymate S. R., Fishel M. A., Watson G. S., Cholerton B. A., Duncan G. E., Mehta P. D., Craft S. (2010). Effects of aerobic exercise on mild cognitive impairment: A controlled trial. Archives of Neurology, 67(1), 71–79. 10.1001/archneurol.2009.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belleville S., Hudon C., Bier N., Brodeur C., Gilbert B., Grenier S., Ouellet M. C., Viscogliosi C., Gauthier S. (2018). MEMO+: Efficacy, durability and effect of cognitive training and psychosocial intervention in individuals with mild cognitive impairment. Journal of the American Geriatrics Society, 66(4), 655–663. 10.1111/jgs.15192 [DOI] [PubMed] [Google Scholar]
- Brigola A. G., Alexandre T., Inouye K., Yassuda M. S., Pavarini S., Mioshi E. (2019). Limited formal education is strongly associated with lower cognitive status, functional disability and frailty status in older adults. Dementia & Neuropsychologia, 13(2), 216–224. 10.1590/1980-57642018dn13-020011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caltagirone C., Bianchetti A., Di Luca M., Mecocci P., Padovani A., Pirfo E., Scapicchio P., Senin U., Trabucchi M., Musicco M., & Italian Association of Psychogeriatrics. (2005). Guidelines for the treatment of Alzheimer’s disease from the Italian Association of Psychogeriatrics. Drugs & Aging, 22 Suppl 1, 1–26. 10.2165/00002512-200522001-00002 [DOI] [PubMed] [Google Scholar]
- Carroll K. M., Kiluk B. D., Nich C., Babuscio T. A., Brewer J. A., Potenza M. N., Ball S. A., Martino S., Rounsaville B. J., Lejuez C. W. (2011). Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Substance Use & Misuse, 46(1), 23–34. 10.3109/10826084.2011.521069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (2011). Cognitive impairment: A call for action, Now! Is. Retrieved December 22, 2020, from www.cdc.gov/aging/healthybrain/index.htm
- Ciasca E. C., Ferreira R. C., Santana C. L. A., Forlenza O. V., dos Santos G. D., Brum P. S., Nunes P. V. (2018). Art therapy as an adjuvant treatment for depression in elderly women: A randomized controlled trial. Revista Brasileira de Psiquiatria, 40(3), 256–263. 10.1590/1516-4446-2017-2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Li R., Lyketsos C., Livingston G. (2013). Treatment for mild cognitive impairment: Systematic review. The British Journal of Psychiatry, 203(3), 255–264. 10.1192/bjp.bp.113.127811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Roeck E. E., van der Vorst A., Engelborghs S., Zijlstra G. A. R., Dierckx E. (2019). Exploring cognitive frailty: Prevalence and associations with other frailty domains in older people with different degrees of cognitive impairment. Gerontology, 66(1), 55–64. 10.1159/000501168 [DOI] [PubMed] [Google Scholar]
- Duan Y., Lu L., Chen J., Wu C., Liang J., Zheng Y., Wu J., Rong P., Tang C. (2018). Psychosocial interventions for Alzheimer’s disease cognitive symptoms: A Bayesian network meta-analysis. BMC Geriatrics, 18(1), 175. 10.1186/s12877-018-0864-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias S. T., Mungas D., Reed B. R., Harvey D., DeCarli C. (2009). Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Archives of Neurology, 66(9), 1151–1157. 10.1001/archneurol.2009.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli M. (2009). Depression, cognitive impairment and dementia: Why should clinicians care about the web of causation? Indian Journal of Psychiatry, 51(Suppl1), S29–S34. [PMC free article] [PubMed] [Google Scholar]
- Gates N. J., Sachdev P. S., Fiatarone Singh M. A., Valenzuela M. (2011). Cognitive and memory training in adults at risk of dementia: A systematic review. BMC Geriatrics, 11, 55. 10.1186/1471-2318-11-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauthier S., Reisberg B., Zaudig M., Petersen R. C., Ritchie K., Broich K., Belleville S., Brodaty H., Bennett D., Chertkow H., Cummings J. L., de Leon M., Feldman H., Ganguli M., Hampel H., Scheltens P., Tierney M. C., Whitehouse P., Winblad B., & International Psychogeriatric Association Expert Conference on Mild Cognitive Impairment. (2006). Mild cognitive impairment. The Lancet (London, England), 367(9518), 1262–1270. 10.1016/S0140-6736(06)68542-5 [DOI] [PubMed] [Google Scholar]
- Heart Protection Study Collaborative Group. (2011). Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: A randomised controlled trial. The Lancet (London, England), 378(9808), 2013–2020. 10.1016/S0140-6736(11)61125-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussin N. M., Shahar S., Yahya H. M., Din N. C., Singh D. K. A., Omar M. A. (2019). Incidence and predictors of mild cognitive impairment (MCI) within a multi-ethnic Asian populace: A community-based longitudinal study. BMC Public Health, 19, 1159 10.1186/s12889-019-7508-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2015). Psychosocial interventions for mental and substance use disorders: A framework for establishing evidence-based standards. The National Academies Press; [PubMed] [Google Scholar]
- Ishizaki J., Meguro K., Ohe K., Kimura E., Tsuchiya E., Ishii H., Sekita Y., Yamadori A. (2002). Therapeutic psychosocial intervention for elderly subjects with very mild Alzheimer disease in a community: The tajiri project. Alzheimer Disease and Associated Disorders, 16(4), 261–269. 10.1097/00002093-200210000-00008 [DOI] [PubMed] [Google Scholar]
- Katz A. (2017). Allan Urho Paivio (1925–2016). The American Psychologist, 72(5), 497. 10.1037/amp0000145 [DOI] [PubMed] [Google Scholar]
- Kelaiditi E., Cesari M., Canevelli M., van Kan G. A., Ousset P. J., Gillette-Guyonnet S., Ritz P., Duveau F., Soto M. E., Provencher V., Nourhashemi F., Salvà A., Robert P., Andrieu S., Rolland Y., Touchon J., Fitten J. L., Vellas B., & IANA/IAGG. (2013). Cognitive frailty: Rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. The Journal of Nutrition, Health & Aging, 17(9), 726–734. 10.1007/s12603-013-0367-2 [DOI] [PubMed] [Google Scholar]
- Kivipelto M., Solomon A., Ahtiluoto S., Ngandu T., Lehtisalo J., Antikainen R., Bäckman L., Hänninen T., Jula A., Laatikainen T., Lindström J., Mangialasche F., Nissinen A., Paajanen T., Pajala S., Peltonen M., Rauramaa R., Stigsdotter-Neely A., Strandberg T., Tuomilehto J., . . . Soininen H. (2013). The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): Study design and progress. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 9(6), 657–665. 10.1016/j.jalz.2012.09.012 [DOI] [PubMed] [Google Scholar]
- Lam R. W., Kennedy S. H., Mclntyre R. S., Khullar A. (2014). Cognitive dysfunction in major depressive disorder: Effects on psychosocial functioning and implications for treatment. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 59(12), 649–654. 10.1177/070674371405901206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. K., Chen C. H., Lee W. J., Wu Y. H., Hwang A. C., Lin M. H., Shimada H., Peng L. N., Loh C. H., Arai H., Chen L. K. (2018). Cognitive frailty and its association with all-cause mortality among community-dwelling older adults in Taiwan: Results from I-Lan longitudinal aging study. Rejuvenation Research, 21(6), 510–517. 10.1089/rej.2017.2038 [DOI] [PubMed] [Google Scholar]
- Mahendran R., Gandhi M., Moorakonda R. B., Wong J., Kanchi M. M., Fam J., Rawtaer I., Kumar A. P., Feng L., Kua E. H. (2018). Art therapy is associated with sustained improvement in cognitive function in the elderly with mild neurocognitive disorder: Findings from a pilot randomized controlled trial for art therapy and music reminiscence activity versus usual care. Trials, 19(1), 615. 10.1186/s13063-018-2988-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masika G. M., Yu D., Li P. (2021). Can visual art therapy be implemented with illiterate older adults with mild cognitive impairment? A pilot mixed-method randomized controlled trial. Journal of Geriatric Psychiatry and Neurology, 34(1), 76–86. 10.1177/0891988720901789 [DOI] [PubMed] [Google Scholar]
- McDermott O., Charlesworth G., Hogervorst E., Stoner C., Moniz-Cook E., Spector A., Csipke E., Orrell M. (2019). Psychosocial interventions for people with dementia: A synthesis of systematic reviews. Aging & Mental Health, 23(4), 393–403. 10.1080/13607863.2017.1423031 [DOI] [PubMed] [Google Scholar]
- Mohd Zulkifly M. F., Ghazali S. E., Che Din N., Singh D. K., Subramaniam P. (2016). A review of risk factors for cognitive impairment in stroke survivors. The Scientific World Journal, 2016. 10.1155/2016/3456943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murukesu R. R., Singh D. K. A., Shahar S., Subramaniam P. (2020). A multi-domain intervention protocol for the potential reversal of cognitive frailty: “WE-RISE” randomized controlled trial. Frontiers in Public Health, 8, 471. 10.3389/fpubh.2020.00471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatsuka M., Nakamura K., Hamanosono R., Takahashi Y., Kasai M., Sato Y., Suto T., Nagatomi R., Meguro K. (2015). A cluster randomized controlled trial of nonpharmacological interventions for old-old subjects with a clinical dementia rating of 0.5: The Kurihara Project. Dementia and Geriatric Cognitive Disorders Extra, 5(2), 221–232. 10.1159/000380816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health (UK). (2007). Dementia: A NICE-SCIE guideline on supporting people with dementia and their carers in health and social care. British Psychological Society. [PubMed] [Google Scholar]
- Netherlands Institute for Health Services Research. (2004). Het begeleiden van mensen met dementie die apathisch zijn. Richtlijn voor verzorgenden. [Supporting people with dementia who are apathetic. Guideline for formal caregivers. In Dutch]. NIVEL; Verpleeghuis Waerthove. [Google Scholar]
- Ong L. K., Walker F. R., Nilsson M. (2017). Is stroke a neurodegenerative condition? A critical review of secondary neurodegeneration and amyloid-beta accumulation after stroke. AIMS Medical Science, 4(1): 1–16. 10.3934/medsci.2017.1.1 [DOI] [Google Scholar]
- Panza F., Lozupone M., Solfrizzi V., Sardone R., Dibello V., Di Lena L., D’Urso F., Stallone R., Petruzzi M., Giannelli G., Quaranta N., Bellomo A., Greco A., Daniele A., Seripa D., Logroscino G. (2018). Different cognitive frailty models and health- and cognitive-related outcomes in older age: From epidemiology to prevention. Journal of Alzheimer’s Disease, 62(3), 993–1012. 10.3233/JAD-170963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park D. C., Gutchess A. H., Meade M. L., Stine-Morrow E. A. (2007). Improving cognitive function in older adults: Nontraditional approaches. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(Spec No 1), 45–52. 10.1093/geronb/62.special_issue_1.45 [DOI] [PubMed] [Google Scholar]
- Patel B., Perera M., Pendleton J., Richman A., Majumdar B. (2014). Psychosocial interventions for dementia: From evidence to practice. Advances in Psychiatric Treatment, 20(5), 340–349. 10.1192/apt.bp.113.011957 [DOI] [Google Scholar]
- Petersen R. C., Caracciolo B., Brayne C., Gauthier S., Jelic V., Fratiglioni L. (2014). Mild cognitive impairment: A concept in evolution. Journal of Internal Medicine, 275(3), 214–228. 10.1111/joim.12190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M. D. J., Godfrey C., McInerney P., Baldini Soares C., Khalil H., Parker D. (2020). Scoping reviews. In Aromataris E., Munn Z. (Eds.), JBI manual for evidence synthesis. JBI. https://synthesismanual.jbi.global. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- Pitkala K. H., Routasalo P., Kautiainen H., Sintonen H., Tilvis R. S. (2011). Effects of socially stimulating group intervention on lonely, older people’s cognition: A randomized, controlled trial. The American Journal of Geriatric Psychiatry, 19(7), 654–663. 10.1097/JGP.0b013e3181f7d8b0 [DOI] [PubMed] [Google Scholar]
- Razali R., Baharudin A., Jaafar N. R. N., Sidi H., Rosli A. H. (2012). Factors associated with mild cognitive impairment among elderly patients attending medical clinics in Universiti Kebangsaan Malaysia Medical Centre. Sains Malaysiana, 41, 641–647. [Google Scholar]
- Rivan N., Shahar S., Rajab N. F., Singh D., Che Din N., Mahadzir H., Mohamed Sakian N. I., Ishak W. S., Abd Rahman M. H., Mohammed Z., You Y. X. (2020). Incidence and predictors of cognitive frailty among older adults: A community-based longitudinal study. International Journal of Environmental Research and Public Health, 17(5), 1547. 10.3390/ijerph17051547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts R. O., Knopman D. S., Mielke M. M., Cha R. H., Pankratz V. S., Christianson T. J., Geda Y. E., Boeve B. F., Ivnik R. J., Tangalos E. G., Rocca W. A., Petersen R. C. (2014). Higher risk of progression to dementia in mild cognitive impairment cases who revert to normal. Neurology, 82(4), 317–325. 10.1212/WNL.0000000000000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rund B. R. (2009). Is there a degenerative process going on in the brain of people with Schizophrenia? Frontiers in Human Neuroscience, 3, 36. 10.3389/neuro.09.036.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safar L. T. (2014). Use of art making in treating older patients with dementia. Virtual Mentor, 16(8), 626–630. 10.1001/virtualmentor.2014.16.8.stas1-1408. [DOI] [PubMed] [Google Scholar]
- Schechter G., Azad G. K., Rao R., McKeany A., Matulaitis M., Kalos D. M., Kennedy B. K. (2020). A comprehensive, multi-modal strategy to mitigate Alzheimer’s disease risk factors improves aspects of metabolism and offsets cognitive decline in individuals with cognitive impairment. Journal of Alzheimer’s Disease Reports, 4(1), 223–230. 10.3233/ADR-200185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugimoto T., Sakurai T., Ono R., Kimura A., Saji N., Niida S., Toba K., Chen L. K., Arai H. (2018). Epidemiological and clinical significance of cognitive frailty: A mini review. Ageing Research Reviews, 44, 1–7. 10.1016/j.arr.2018.03.002 [DOI] [PubMed] [Google Scholar]
- Vasse E., Vernooij-Dassen M., Cantegreil I., Franco M., Dorenlot P., Woods B., Moniz-Cook E. (2011). Guidelines for psychosocial interventions in dementia care: A European survey and comparison. International Journal of Geriatric Psychiatry, 27(1), 40–48. 10.1002/gps.2687 [DOI] [PubMed] [Google Scholar]
- Vellas B., Carrie I., Gillette-Guyonnet S., Touchon J., Dantoine T., Dartigues J. F., Cuffi M. N., Bordes S., Gasnier Y., Robert P., Bories L., Rouaud O., Desclaux F., Sudres K., Bonnefoy M., Pesce A., Dufouil C., Lehericy S., Chupin M., Mangin J. F., . . . Andrieu S. (2014). MAPT study: A multidomain approach for preventing Alzheimer’s disease: Design and baseline data. The Journal of Prevention of Alzheimer’s Disease, 1(1), 13–22. [PMC free article] [PubMed] [Google Scholar]
- Wong W. (2020). Economic burden of Alzheimer disease and managed care considerations. The American Journal of Managed Care, 26, S177-S183. 10.37765/ajmc.2020.88482 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2011). Cognitive and psychosocial intervention. Author. https://www.who.int/mental_health/mhgap/evidence/dementia/q5/en/ [Google Scholar]
- Zhao J., Li H., Lin R., Wei Y., Yang A. (2018). Effects of creative expression therapy for older adults with mild cognitive impairment at risk of Alzheimer’s disease: A randomized controlled clinical trial. Clinical Interventions in Aging, 13, 1313–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]