Abstract
From 1999 through 2017, age-adjusted suicide rates in the United States rose by 33% (from 10.5 to 14.0 per 100 000 population). Social capital, a key social determinant of health, could protect against suicide, but empirical evidence on this association is limited. Using multilevel data from the Centers for Disease Control and Prevention, we explored state- and county-level social capital as predictors of age-adjusted suicide rates pooled from 2010 through 2017 across 2112 US counties. In addition, we tested for causal mediation of these associations by state-level prevalence of depression. A 1-standard deviation increase in state-level social capital predicted lower county-level suicide mortality rates almost 2 decades later (0.87 fewer suicides per 100 000 population; P = .04). This association was present among non-Hispanic Black people and among men but not among non-Hispanic White people and women. We also found evidence of partial mediation by prevalence of depression. Our findings suggest that elevating state- and county-level social capital, such as through policy and local initiatives, may help to reverse the trend of rising suicide rates in the United States.
Keywords: suicide, social capital, multilevel, United States
From 1999 through 2017, age-adjusted suicide mortality rates in the United States increased by 33% (from 10.5 to 14.0 per 100 000 population), making suicide 1 of the top 10 leading causes of death across all ages.1,2 Knowledge of the proximal determinants of suicide has informed suicide prevention interventions at the micro level (eg, crisis lines) and the macro level (eg, the 2012 National Strategy for Suicide Prevention).3 However, identifying and addressing the upstream causes of suicide (ie, its social determinants) is essential to attenuating its overall burden.
An underexplored yet plausible root cause of suicide is social capital—characteristics of and resources within social networks, such as interpersonal trust and civic participation, that facilitate collective action.4 Area-level social capital has been inversely linked to suicide rates in Europe,5 the United Kingdom,6 and the United States.7,8 However, thus far, only contemporaneous associations between social capital and suicide have been examined despite the underlying pathway likely involving repeated exposure and processes spanning several years.9 Furthermore, this association has yet to be explored with social capital measured at multiple geographic levels. We addressed these gaps by using multilevel data to investigate the lagged associations of both state- and county-level social capital with county-level suicide mortality rates, controlling for state- and county-level factors.
Methods
Outcome
We obtained county-level suicide mortality data across all ages from 2010 through 2017 for the 48 contiguous US states from the Centers for Disease Control and Prevention’s (CDC’s) Wide-ranging Online Database for Epidemiologic Research.10 Because county-level suicide rates were low in some counties in a given year, we pooled age-standardized suicide rates. CDC considers data from counties with <20 suicides in all years during the 8-year study period to be unreliable; therefore, we excluded these data from analysis.
Predictor Variables
We used an updated version of Putnam’s state-level social capital index4 by Kim et al11 as our main predictor variable. Kim et al derived this index from 14 indicators of social capital measured in the 1990s, including formal and informal social participation, political participation, and trust. The authors did not calculate this index for Alaska and Hawaii because of the inadequate sample size in the data set used by Putnam.4 At the county level, we used a social capital index developed by Rupasingha et al.12 This index was initially created for the year 1990 using 13 variables, including the total density of nonprofit, social, civic, and religious organizations in a county; percentage of population that voted in presidential elections; and response rate to the decennial census. Principal component analysis was used to create a single index from these variables. Rupasingha et al12 then updated this index for the years 1997, 2005, 2009, and 2014.
State- and County-Level Covariates
We used the following demographic and socioeconomic covariates obtained from the 2000 US Census at both the state and county levels: unemployment rate, median annual household income, population density, and the percentage of the population that was non-Hispanic Black, aged ≥65, below the federal poverty level, and high school graduates.13 At the state level, we also controlled for the firearm ownership rate14 and marriage rate15 corresponding to the year 2000.
Statistical Analysis
After excluding data from counties with unreliable suicide mortality rates for the 2010-2017 period, we included 2112 counties in our analyses. We first compared data from counties that were excluded from the analysis with data from counties that were included in the analysis on all county-level covariates and on population size using 2-sample t tests. We then estimated multivariate linear regression models with state- and county-level social capital as predictors of the pooled county-level age-adjusted suicide mortality rates, controlling for state- and county-level covariates. In addition, we estimated models for major racial/ethnic (non-Hispanic Black, non-Hispanic White) and sex (male, female) groups. We assessed multicollinearity using variance inflation factors; we removed the state-level percentage of population below the federal poverty level from all models because of a variance inflation factor >10. Furthermore, we conducted a sensitivity analysis by removing data from counties with population size less than or equal to the median value of the originally omitted counties (counties with <20 suicides) to assess for the potential presence of selection bias. All estimates are rescaled to reflect a 1-standard deviation (1-SD) change (eg, a change of 0.64 units for state-level social capital and 1.35 units for county-level social capital in 1990).
We also tested for mediation of state-level social capital associations separately by county-level social capital and by state-level prevalence of depression for the year 2004-2005 (obtained from the Substance Abuse and Mental Health Services Administration),16 using a causal mediation analysis approach, as described by Yung et al.17 To achieve model convergence, the causal mediation models did not account for the state- and county-level unemployment rate, median annual household income, county-level population density, or state firearm ownership rates and marriage rates.
We assessed significance at a level of .05 (2-tailed). We based robust standard errors on Huber–White robust sandwich estimators18 and weighted the model estimates by county population size. We conducted all analyses using SAS version 9.4 (SAS Institute Inc). Because we used de-identified data, institutional review board review was not required.
Results
The average pooled county-level age-adjusted suicide mortality rate was 16.8 suicides per 100 000 population. Suicide mortality rates per 100 000 population were higher among men than among women (20.9 vs 6.1) and among non-Hispanic White people than among non-Hispanic Black people (23.7 vs 11.1). Overall, we found significant differences between counties that were included in the analysis and counties that were excluded from the analysis on all characteristics except for the percentage of the population that was non-Hispanic Black (data available from authors upon request).
Living in a state with higher social capital was associated with lower county-level age-adjusted suicide mortality rates roughly 2 decades later. A 1-SD increase in state-level social capital in 1990 predicted a 0.87 per 100 000 population lower county-level age-adjusted pooled suicide mortality rate from 2010 through 2017 (P = .04) (Table). This association was significant among non-Hispanic Black people (1.78 fewer suicides per 100 000 population, P < .001) and among men (0.95 fewer suicides per 100 000 population, P = .03) but not among non-Hispanic White people or women. In sensitivity analyses, our results remained robust after excluding 77 counties with population size equal to or below the median for the original excluded counties (0.90 fewer suicides per 100 000 population, P = .04). Higher rates of firearm ownership at the state level were also significantly associated with higher rates of age-adjusted suicide at the county level. In causal mediation analyses, the prevalence of state-level depression for 2004-2005 mediated approximately 64% of the overall association (P = .01), whereas county-level social capital for 1997 mediated nearly 50% of the association (P = .04).
Table.
Coefficient estimates from multivariate linear regression analysis assessing state-level social capital (1990s) as a predictor of county-level age-adjusted pooled suicide mortality rates (2010-2017) in the United Statesa
| Characteristics | βb,c (95% CI) [P value]d | Adjusted R 2 | No. of counties included |
|---|---|---|---|
| State-level social
capital (overall sample) |
−0.87 (−1.72 to −0.03) [.04] | 0.48 | 2112 |
| State-level covariates | |||
| Median annual household income | −0.0001 (−0.0003 to 0) [.06] | ||
| Population density | 0.001 (−0.002 to 0.003) [.68] | ||
| Unemployment rate | −177.76 (−292.17 to −63.06) [.002] | ||
| Percentage non-Hispanic Black population | −1.82 (−7.08 to 3.43) [.49] | ||
| Percentage aged ≥65 | −33.88 (−68.24 to 0.47) [.05] | ||
| Percentage high school graduates | 0.15 (−0.02 to 0.33) [.08] | ||
| Firearm ownership rate | 16.02 (11.85 to 20.19) [<.001] | ||
| Marriage rate | 0.06 (−0.02 to 0.15) [.15] | ||
| County-level covariates | |||
| Median annual household income | −0.0001 (−0.0001 to −0.0001) [<.001] | ||
| Population density | −0.00008 (−0.00015 to −0.00002) [.01] | ||
| Unemployment rate | 53.65 (−3.97 to 111.28) [.07] | ||
| Percentage non-Hispanic Black population | −8.39 (−11.69 to −5.09) [<.001] | ||
| Percentage aged ≥65 | 13.01 (1.19 to 24.82) [.03] | ||
| Percentage high school graduates | 10.09 (2.25 to 17.95) [.01] | ||
| Percentage below federal poverty level | −3.95 (−15.84 to 7.94) [.51 | ||
| State-level social capital (non-Hispanic Black) | −1.78 (−2.19 to −1.37) [<.001] | 0.65 | 1342 |
| State-level social capital (non-Hispanic White) | −0.57 (−1.66 to 0.52) [.30] | 0.53 | 1984 |
| State-level social capital (men) | −0.95 (−1.78 to −0.11) [.03] | 0.63 | 2000 |
| State-level social capital (women) | −0.26 (−0.76 to 0.25) [.32] | 0.31 | 1523 |
aData sources: Centers for Disease Control and Prevention,10 Kim et al,11 Rupasingha et al,12 US Census Bureau,13 Schell et al,14 and Centers for Disease Control and Prevention.15
bAll reported β estimates for state-level social capital are rescaled to reflect a 1-standard deviation change.
cAll models are adjusted for unemployment rate, median annual household income, percentage of non-Hispanic Black population, percentage of population aged ≥65, percentage of high school graduates, and population density at both county and state levels; firearm ownership rate and marriage rate at the state level; and percentage of population below the federal poverty level at the county level.
dUsing a 2-tailed t test, with P < .05 considered significant.
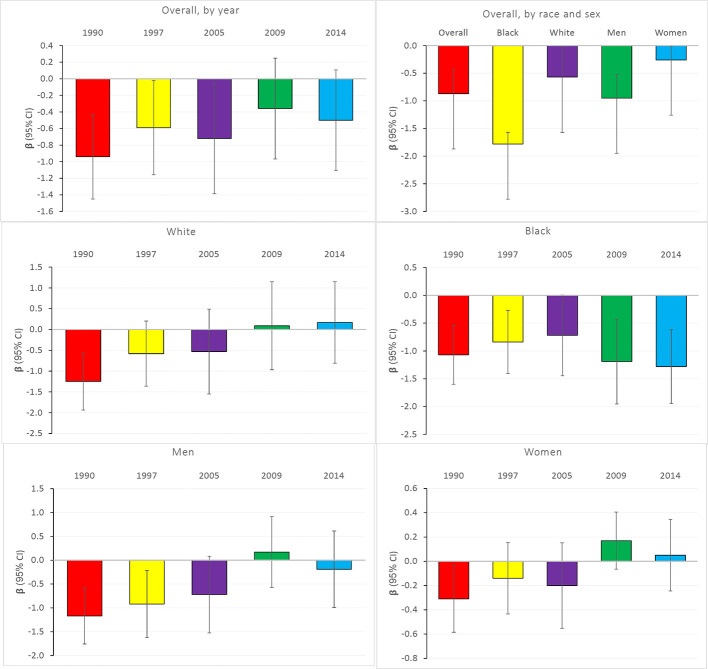
At the county level, a 1-SD increase in county-level social capital in 1990 predicted a 0.94 per 100 000 population lower county-level age-adjusted pooled suicide mortality rate (P < .001) (Figure). The associations of county-level social capital measured in 1997, 2005, 2009, and 2014 were weaker than associations for county-level social capital measured in 1990, suggesting a stronger effect of a county’s level of social capital on suicide mortality with a longer (vs shorter) lag period. The county-level associations were also stronger among non-Hispanic Black people than among non-Hispanic White people and among men than among women (data available from authors upon request).
Figure.
Coefficient estimates from multivariate linear regression analysis of county-level social capital (for years 1990, 1997, 2005, 2009, and 2014) and county-level age-adjusted pooled suicide rates (2010-2017), United States. All reported β estimates are rescaled to reflect a 1-standard deviation change. All models are adjusted for unemployment rate, median annual household income, percentage of non-Hispanic Black population, percentage of population aged ≥65, percentage of high school graduates, and population density at both the county and state levels; firearm ownership rate and marriage rate at the state level only; and percentage of population below the federal poverty level at the county level. Significance was measured using a 2-tailed t test, with P < .05 considered significant. Data sources: Centers for Disease Control and Prevention,10 Kim et al,11 Rupasingha et al,12 US Census Bureau,13 Schell et al,14 and Centers for Disease Control and Prevention.15
Discussion
In this multilevel study, we found that higher state- and county-level social capital was linked to lower county-level age-adjusted suicide rates, with county-level associations becoming more salient with longer lag periods. Across population subgroups, we found no evidence of a state-level association among non-Hispanic White people or women. In addition, we found evidence that depression and county-level social capital partially mediated the state-level association by social capital.
Higher levels of civic and political participation at the state level might influence policies related to income inequality and availability of mental health services. Furthermore, our county-level findings are consistent with the ecological findings of Recker and Moore,8 who observed an inverse association. Social capital at the county level may reflect the capacity for local social organizations to foster social support among their residents. In addition to offering people an opportunity to discuss their suicidal thoughts and intervene in the situation of a suicidal crisis, cognitive social capital (eg, trust and sense of belonging) could protect against both depression19 and suicide risk.20
The absence of an association between state-level social capital and suicide mortality among women has been described7,21 and may be explained by family relationships promoting women’s mental health better than social relationships outside the home.22 Our findings contrast with the findings of Smith and Kawachi,7 who observed no association between state-level social capital and suicide mortality among non-Hispanic Black men but a significant association among non-Hispanic White men and women. These conflicting findings call for further inquiry into the relationships by racial/ethnic lines.
One strength of our study was that, to our knowledge, it is the first to examine the lagged multilevel associations of state- and county-level social capital with county-level suicide rates. Another strength is that we controlled for key state- and county-level factors, thereby minimizing residual confounding, and we used time lags to explore the most salient time periods for effects. Finally, the temporal order of our data reduced the risk of reverse causation.
Our study also had several limitations. First, our findings may not be generalizable to counties with low or unreliable suicide rates, including counties with small populations, although our sensitivity analysis did not support the presence of selection bias. Second, our models did not account for individual-level characteristics, which could have contributed to residual confounding. Finally, our causal mediation models excluded several covariates to achieve convergence, which may have contributed to model misspecification.
Overall, our findings suggest several future directions to strengthen the evidence base on the association between social capital and the occurrence of suicide mortality. First, our results call for evaluating the causal nature and underlying individual mechanisms of the relationship between social capital and suicide. Second, we observed lagged associations for both state- and county-level social capital, which may suggest various mechanisms operating at various geographic levels. Delineating such mechanisms would be useful. Lastly, our findings point to the need to develop and evaluate policies and initiatives that promote social capital at more local geographic levels (eg, initiatives that increase civic engagement and social trust), which may serve as effective levers to address the growing suicide epidemic in the United States.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Saloni Dev, MA https://orcid.org/0000-0003-3385-7249
References
- 1.Hedegaard H., Curtin SC., Warner M. Suicide mortality in the United States, 1999-2017. NCHS Data Brief. 2018;330:1-8. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control . Fatal injury reports, national, regional and state, 1981-2018. 2019. Accessed September 27, 2020. https://webappa.cdc.gov/sasweb/ncipc/mortrate.html
- 3.Office of the Surgeon General, National Action Alliance for Suicide Prevention . 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the US Surgeon General and of the National Action Alliance for Suicide Prevention . US Department of Health and Human Services; 2012. [PubMed] [Google Scholar]
- 4.Putnam RD. Bowling Alone: The Collapse and Revival of American Community. Simon and Schuster; 2001. [Google Scholar]
- 5.Kelly BD., Davoren M., Mhaoláin AN., Breen EG., Casey P. Social capital and suicide in 11 European countries: an ecological analysis. Soc Psychiatry Psychiatr Epidemiol. 2009;44(11):971-977. 10.1007/s00127-009-0018-4 [DOI] [PubMed] [Google Scholar]
- 6.Congdon P. Latent variable model for suicide risk in relation to social capital and socio-economic status. Soc Psychiatry Psychiatr Epidemiol. 2012;47(8):1205-1219. 10.1007/s00127-011-0429-x [DOI] [PubMed] [Google Scholar]
- 7.Smith NDL., Kawachi I. State-level social capital and suicide mortality in the 50 U.S. states. Soc Sci Med. 2014;120:269-277. 10.1016/j.socscimed.2014.09.007 [DOI] [PubMed] [Google Scholar]
- 8.Recker NL., Moore MD. Durkheim, social capital, and suicide rates across US counties. Health Sociol Rev. 2016;25(1):78-91. 10.1080/14461242.2015.1101703 [DOI] [Google Scholar]
- 9.Kawachi I., Kennedy BP., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491-1498. 10.2105/ajph.87.9.1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control . About underlying cause of death, 1999-2017. 2018. Accessed September 27, 2020. https://wonder.cdc.gov/ucd-icd10.html
- 11.Kim D., Subramanian SV., Gortmaker SL., Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: a multilevel, multivariable analysis. Soc Sci Med. 2006;63(4):1045-1059. 10.1016/j.socscimed.2006.02.017 [DOI] [PubMed] [Google Scholar]
- 12.Rupasingha A., Goetz SJ., Freshwater D. The production of social capital in US counties. J Socio Econ. 2006;35(1):83-101. 10.1016/j.socec.2005.11.001 [DOI] [Google Scholar]
- 13.US Census Bureau . Summary file 1. 2000. Accessed June 15, 2020. https://www.census.gov/data/developers/data-sets/decennial-census.2000.html
- 14.Schell TL., Peterson S., Vegetabile BG., Scherling A., Smart R., Morral AR. State-Level Estimates of Household Firearm Ownership. Rand Corporation; 2020. [Google Scholar]
- 15.Centers for Disease Control and Prevention. National Center for Health Statistics . Marriage rates by state: 1990, 1995, and 1999-2018. Accessed June 15, 2020. https://www.cdc.gov/nchs/nvss/marriage-divorce.htm
- 16.Substance Abuse and Mental Health Services Administration . Substance Abuse and Mental Health Data Archive. 2005-2006. Accessed November 20, 2019. https://pdas.samhsa.gov
- 17.Yung YF., Lamm M., Zhang W. Causal mediation analysis with the CAUSALMED procedure. Paper presented at: SAS Global Forum 2018 Conference; April 8-11, 2018; Cary, North Carolina.
- 18.Huber PJ. The Behavior of Maximum Likelihood Estimates Under Nonstandard Conditions. University of California Press; 1967. [Google Scholar]
- 19.Fujiwara T., Kawachi I. A prospective study of individual-level social capital and major depression in the United States. J Epidemiol Community Health. 2008;62(7):627-633. 10.1136/jech.2007.064261 [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services . Does depression increase the risk for suicide? 2014. Accessed December 11, 2019. https://www.hhs.gov/answers/mental-health-and-substance-abuse/does-depression-increase-risk-of-suicide/index.html
- 21.Kunst AE., van Hooijdonk C., Droomers M., Mackenbach JP. Community social capital and suicide mortality in the Netherlands: a cross-sectional registry-based study. BMC Public Health. 2013;13:969. 10.1186/1471-2458-13-969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferlander S., Stickley A., Kislitsyna O., Jukkala T., Carlson P., Mäkinen IH. Social capital—a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow [published erratum appears in BMC Psychol. 2017;5(10):20. doi:10.1186/s50359-017-0190-3]. BMC Psychol. 2016;4(1):37. 10.1186/s40359-016-0144-1 [DOI] [PMC free article] [PubMed] [Google Scholar]