Abstract
Objectives
The global COVID-19 pandemic has affected various populations differently. We investigated the relationship between socioeconomic determinants of health obtained from the Robert Wood Johnson Foundation County Health Rankings and COVID-19 incidence and mortality at the county level in Georgia.
Methods
We analyzed data on COVID-19 incidence and case-fatality rates (CFRs) from the Georgia Department of Public Health from March 1 through August 31, 2020. We used repeated measures generalized linear mixed models to determine differences over time in Georgia counties among quartile health rankings of health outcomes, health behaviors, clinical care, social and economic factors, and physical environment.
Results
COVID-19 incidence per 100 000 population increased across all quartile county groups for all health rankings (range, 23.1-51.6 in May to 688.4-1062.0 in August). COVID-19 CFRs per 100 000 population peaked in April and May (range, 3312-6835) for all health rankings, declined in June and July (range, 827-5202), and increased again in August (range, 1877-3310). Peak CFRs occurred later in counties with low health rankings for health behavior and clinical care and in counties with high health rankings for social and economic factors and physical environment. All interactions between the health ranking quartile variables and month were significant (P < .001). County-level Gini indices were associated with significantly higher rates of COVID-19 incidence (P < .001) but not CFRs.
Conclusions
From March through August 2020, COVID-19 incidence rose in Georgia’s counties independent of health rankings categorization. Differences in time to peak CFRs differed at the county level based upon key health rankings. Public health interventions should incorporate unique strategies to improve COVID-19–related patient outcomes in these environments.
Keywords: COVID-19, socioeconomic determinants of health, mortality, Georgia
The COVID-19 pandemic has created unprecedented challenges globally. First detected in the United States on January 21, 2020, COVID-19 has affected various regions differently.1 Efforts by state and local governments and the federal government to mitigate the transmission of SARS-CoV-2, the virus that causes COVID-19, have also varied.2 As the COVID-19 pandemic progresses, attention has been directed to understanding disparities in its incidence, prevalence, and outcomes at a granular level.
Georgia was one of the first states to permit the reopening of businesses, restaurants, and other service-oriented industries on May 1, 2020, after a period of state-level government-mandated restrictions.3 Subsequently, the cumulative number of people with COVID-19 in Georgia rose; the number of diagnosed people totaled 843 645, and 16 171 people had died as of March 23, 2021.4 COVID-19 incidence and case-fatality rates vary at the county level. Because Georgia is known to have substantial heterogeneity in health outcomes across the state, we hypothesized that COVID-19 incidence and case-fatality rates may be predicted not only by clinical and demographic characteristics but also by socioeconomic variables, as defined and ranked by the Robert Wood Johnson Foundation (RWJF) County Health Rankings database, at the county level over time.5-7 The RWJF County Health Rankings system aggregates clinical, socioeconomic, and environmental data to create a composite ranking system of each US county. The 2 broad categories of health outcomes and health factors incorporate a broad spectrum of variables known to influence a population’s overall health.5-7 Indexed at a national level, these 6 key categories are available for each US county for a given year. To better describe the role clinical and socioeconomic variables play in COVID-19 incidence and mortality in Georgia, we selected this well-validated population health tool for incorporation into our predictive models.
Methods
Data Sources and Description of County-Level Indicators
We obtained Georgia population health data from the RWJF 2020 County Health Rankings at the county level.7 These health rankings are categorized as health outcomes measures or health factor measures. Health outcomes measures include length of life and quality of life. Health factor measures include health behaviors, clinical care, social and economic factors, and physical environment. We obtained data on COVID-19 incidence and case-fatality rates in Georgia from the USA Facts website8 and the Georgia Department of Public Health website9 from March 1 through August 31, 2020, permitting the inclusion of 4 months of COVID-19 epidemiologic data after termination of Georgia’s mandated shelter-in-place order on May 1, 2020.3 Institutional review board approval was not required for this study because of the publicly available nature of de-identified population-level data included in this analysis.
We derived indicators of rural county status, population density, and percentage male from the Georgia Department of Public Health and the US Census Bureau.8-11 Beyond conventional indices of economic viability, we also included the Gini index, which quantifies economic inequality on a numerical scale ranging from 0 (complete equality) to 1 (complete inequality).12,13 We obtained Gini index data from the Small Area Income and Poverty Estimates program. These data represent a 5-year average from 2014 through 2018 converted to a percentage. Variables included rurality, percentage male, Gini index, population density, and RWJF health rankings.
Statistical Methods
We performed all statistical analyses using SAS version 9.4 (SAS Institute, Inc), and we assessed significance at α = .05. We determined descriptive statistics for all variables overall and during the study period (March 1 through August 31, 2021) for the COVID-19 monthly incidence rate or case-fatality rate. We categorized counties into health ranking quartiles (0%-25%, 26%-50%, 51%-75%, and 76%-100%), with 0%-25% representing the quartile with the most favorable ranking. We calculated incident cases and case fatalities as the number of new cases or new fatalities each month. We used generalized linear mixed models to examine whether incident rates or case-fatality rates differed over time between the 2020 RWJF rankings of health behaviors, clinical care, social and economic factors, and physical environment repeated measures. Fixed effects in all models included month, the 2020 RWJF health ranking variables, and the 2-factor interaction between these fixed effects. We considered county to be a random effect. We used the Wald χ2 test for the 2-factor interaction.
For both incidence rates and case-fatality rates, we assumed the underlying distribution to be Poisson with a log link. We used an offset parameter of the natural log of the population within the county for incidence rates or the natural log of the total number of positive COVID-19 cases for case-fatality rates. The correlation structure that provided the best fit to the correlation between months in incident cases was autoregressive order 1 and for case fatality was compound symmetric. All models corrected for overdispersion. Each model controlled for whether the county was considered nonrural or rural, percentage male in the county, average Gini index from 2014 through 2018, population density, and 2020 RWJF health rankings for length of life and quality of life. The percentage male, average Gini index from 2014 through 2018, and population density of the county were centered to their mean when used in modeling. We assessed potential multicollinearity among all independent variables using variance inflation factors. We found no multicollinearity, because all variance inflation factors were <5. We examined post hoc pairwise comparisons of interest within month between health ranking quartiles and used a Bonferroni adjustment to the overall α level to account for the multiple tests performed.
Results
COVID-19 incidence rates increased from March to August (Table 1). COVID-19 incidence rates per 100 000 population were significantly lower in March (42.7) than in all other months (all P < .001). COVID-19 incidence rates were significantly lower in April (299.3) and May (252.8) than in June (392.2), July (995.3), and August (989.0) (all P < .001); the rate in June was significantly lower than the rates in July and August (all P < .001); and the rate in July was significantly higher than the rate in August (P = .01). In the simple models (supplemental material available from authors), which did not control for demographic or health outcomes, the interaction of each health ranking quartile with time was significant.
Table 1.
Descriptive statistics for county-level COVID-19 incidence and case-fatality rates and demographic and health rankings, Georgia, March 1–August 31, 2020
| Variable | Mean (SD)a |
|---|---|
| County-level outcome variables | |
| COVID-19 incidence per 100 000 population | |
| March | 42.7 (124.7) |
| April | 299.3 (583.2) |
| May | 252.8 (570.5) |
| June | 392.2 (722.6) |
| July | 995.3 (1831.8) |
| August | 989.0 (1359.1) |
| COVID-19 case-fatality rates per 100 000 population | |
| March | 2557.0 (9546.8) |
| April | 4470.3 (4421.0) |
| May | 5120.0 (7261.9) |
| June | 3555.7 (5980.4) |
| July | 1370.1 (1567.3) |
| August | 2947.3 (2266.2) |
| County-level independent variables | |
| Rurality, no. (%) | |
| Nonrural | 41 (25.8) |
| Rural | 118 (74.2) |
| Percentage male | 49.6 (3.2) |
| Gini index 2014-2018, %b | 19.7 (6.8) |
| Population density per 100 000 population | 200.5 (378.0) |
| Health rankings quartiles, no. (%) of countiesc | |
| 0%-25% | 40 (25.1) |
| 26%-50% | 40 (25.1) |
| 51%-75% | 39 (24.5) |
| 76%-100% | 40 (25.1) |
aAll values are mean (SD) unless otherwise indicated.
bThe Gini index is a summary measure that quantifies economic inequality on a numerical scale ranging from 0 (complete equality) to 1 (complete inequality).12 Data are reported as Gini index x 100.
cIncludes the following: length of life, quality of life, health behaviors, clinical care, social and economic factors, and physical environment. Rankings were classified such that quartile 0%-25% represents counties ranking most favorably of all quartiles for the measure of interest and quartile 76%-100% represents counties demonstrating the worst outcomes for the measure of interest.7
Case-fatality rates increased from March to May, decreased from June to July, and then increased in August, with the peak occurring in May (Table 2). Case-fatality rates per 100 000 population were significantly lower in March (2557.0) than in April (4470.3) and May (5120.0) but significantly higher than in July (1370.1); rates were significantly higher in April and May (5120.0) than in June (3555.7), July, and August (2947.3); and rates in June and August were significantly higher than in July (all P < .001). Similar to incidence rates, in these simple models, which did not control for demographic or health outcomes, the interaction of each health ranking quartile with time was significant, indicating that the change in COVID-19 case-fatality rates across the 6 months was different between the quartiles of health rankings.
Table 2.
Final adjusted Poisson generalized linear mixed model results on county-level COVID-19 incidence rates per 100 000 population, Georgia, March 1–August 31, 2020
| Effect | Monthly adjusted least-squares mean (95% CI) | χ2a | P valueb | |||||
|---|---|---|---|---|---|---|---|---|
| March | April | May | June | July | August | |||
| Rurality | — | — | — | — | — | — | 5.5 | .02 |
| Percentage male | — | — | — | — | — | — | 0.3 | .59 |
| Gini index 2014-2018c | — | — | — | — | — | — | 12.4 | <.001 |
| Population density | — | — | — | — | — | — | 2.4 | .12 |
| Length-of-life health ranking | — | — | — | — | — | — | 1.0 | .80 |
| Quality-of-life health rankingd | — | — | — | — | — | — | 8.5 | .04 |
| Month | — | — | — | — | — | — | 62 351.3 | <.001 |
| Health behaviors health ranking | — | — | — | — | — | — | 5.7 | .12 |
| Clinical care health ranking | — | — | — | — | — | — | 1.9 | .60 |
| Social and economic health ranking | — | — | — | — | — | — | 12.3 | .01 |
| Physical environment health ranking | — | — | — | — | — | — | 3.0 | .40 |
| Health ranking x month | 2519.6 | <.001 | ||||||
| 0%-25% | 34.8 (27.0-44.9) | 325.6 (256.6-413.1) | 280.7 (221.1-356.3) | 268.6 (211.8-340.6) | 932.7 (736.5-1181.0) | 935.4 (738.6-1185.0) | ||
| 26%-50% | 32.5 (26.8-39.4) | 193.4 (163.1-229.2) | 164.7 (138.8-195.3) | 255.0 (215.6-301.7) | 1014.0 (859.5-1197.0) | 980.7 (831.0-1157.0) | ||
| 51%-75% | 23.1 (19.2-28.0) | 163.5 (138.6-192.9) | 144.6 (122.5-170.8) | 320.0 (271.8-376.8) | 844.2 (718.1-992.5) | 855.5 (727.7-1006.0) | ||
| 76%-100% | 32.8 (26.4-40.8) | 219.7 (181.0-266.7) | 182.5 (150.2-221.8) | 456.8 (376.9-553.5) | 937.5 (774.8-1134.0) | 699.4 (577.8-846.6) | ||
| Clinical care health ranking x month | 1620.7 | <.001 | ||||||
| 0%-25% | 48.0 (40.4-56.9) | 211.0 (179.4-248.2) | 145.5 (123.6-171.2) | 266.7 (226.9-313.5) | 1016.0 (865.3-1193.0) | 926.9 (789.4-1089.0) | ||
| 26%-50% | 31.7 (26.5-37.8) | 218.1 (186.1-255.7) | 150.0 (127.8-176.0) | 314.1 (268.3-367.8) | 828.4 (708.6-968.4) | 749.3 (640.9-876.0) | ||
| 51%-75% | 25.6 (21.1-31.2) | 245.5 (207.5-290.4) | 246.0 (207.9-291.0) | 324.8 (274.8-383.9) | 993.6 (842.5-1172.0) | 938.7 (795.9-1107.0) | ||
| 76%-100% | 22.0 (17.8-27.3) | 200.1 (167.2-239.4) | 227.4 (190.0-272.1) | 368.0 (308.2-439.4) | 895.4 (751.3-1067.0) | 842.0 (706.4-1004.0) | ||
| Social and economic health ranking x month | 3012.3 | <.001 | ||||||
| 0%-25% | 24.8 (19.1-32.2) | 147.0 (114.9-188.0) | 166.1 (129.9-212.4) | 410.9 (321.8-524.7) | 891.2 (698.6-1137.0) | 806.5 (632.2-1029.0) | ||
| 26%-50% | 40.7 (34.0-48.7) | 217.5 (184.6-256.3) | 248.2 (210.7-292.4) | 551.3 (468.9-648.2) | 1196.0 (1018.0-1404.0) | 931.2 (792.6-1094.0) | ||
| 51%-75% | 16.5 (13.0-20.9) | 231.6 (192.1-279.2) | 199.3 (165.2-240.4) | 310.0 (257.7-373.0) | 1121.0 (934.1-1346.0) | 1062.0 (884.6-1275.0) | ||
| 76%-100% | 51.6 (39.7-66.9) | 305.3 (239.8-388.9) | 148.5 (116.3-189.6) | 142.6 (111.9-181.7) | 626.7 (493.3-796.3) | 688.4 (541.8-874.6) | ||
| Physical environment health ranking x month | 81.0 | <.001 | ||||||
| 0%-25% | 24.1 (19.7-29.4) | 208.7 (175.4-248.4) | 202.3 (170.1-240.8) | 334.3 (281.5-397.2) | 1042.0 (878.4-1235.0) | 950.5 (801.6-1127.0) | ||
| 26%-50% | 44.3 (37.1-52.9) | 265.3 (225.5-312.1) | 186.9 (158.7-220.2) | 298.8 (254.1-351.4) | 814.3 (693.7-956.0) | 872.5 (743.3-1024.0) | ||
| 51%-75% | 27.9 (23.7-32.9) | 198.4 (170.4-231.0) | 205.0 (176.1-238.7) | 387.4 (333.1-450.6) | 1007.0 (866.8-1170.0) | 874.5 (752.5-1016.0) | ||
| 76%-100% | 28.8 (24.1-34.4) | 205.8 (174.6-242.4) | 157.3 (133.4-185.5) | 258.7 (219.7-304.6) | 876.5 (745.5-1030.0) | 756.9 (643.7-890.0) | ||
aUsing the Wald χ2 test.
bP < .05 was considered significant.
cThe Gini index is a summary measure that quantifies economic inequality on a numerical scale ranging from 0 (complete equality) to 1 (complete inequality).12 Data are reported as Gini index x 100.
dThe Robert Wood Johnson Foundation Quality of Life rankings include measures of healthfulness including percentage low birth weight, indices of mental and physical wellness (health and distress), and clinical conditions such as percentage of population aged ≥20 years with diabetes and HIV prevalence.7
All interactions between the health ranking quartile variables (health behaviors, clinical care, social and economic factors, and physical environment) and month were significant at P < .001 (Tables 2 and 3). Nonrural counties had significantly higher incidence per 100 000 population (300.8; 95% CI, 248.7-264.0) than rural counties (226.0; 95% CI, 205.7-248.2), controlling for all other variables in the final model (Figure 1). However, nonrural counties had significantly lower case-fatality rates per 100 000 population (231.6; 95% CI, 201.8-265.7) than rural counties (284.3; 95% CI, 252.9-319.7), controlling for all other variables in the final model (Figure 2).
Table 3.
Final adjusted Poisson generalized linear mixed model results on COVID-19 case-fatality rates per 100 000 population, Georgia, March 1–August 31, 2020
| Effect | Monthly adjusted least squares mean (95% CI) | χ2a | P valueb | |||||
|---|---|---|---|---|---|---|---|---|
| March | April | May | June | July | August | |||
| Rurality | — | — | — | — | — | — | 4.6 | .03 |
| Percentage male | — | — | — | — | — | — | 1.6 | .21 |
| Gini index 2014-2018c | — | — | — | — | — | — | 1.6 | .21 |
| Population density | — | — | — | — | — | — | 0.1 | .75 |
| Length-of-life health ranking | — | — | — | — | — | — | 7.0 | .07 |
| Quality-of-life health rankingd | — | — | — | — | — | — | 4.3 | .23 |
| Month | — | — | — | — | — | — | 540.4 | <.001 |
| Health behaviors health ranking | — | — | — | — | — | — | 2.9 | .42 |
| Clinical care health ranking | — | — | — | — | — | — | 24.1 | <.001 |
| Social and economic health ranking | — | — | — | — | — | — | 12.9 | .004 |
| Physical environment health ranking | — | — | — | — | — | — | 12.3 | .01 |
| Health behaviors health ranking x month | 52.0 | <.001 | ||||||
| 0%-25% | 1649 (905-3008) | 4483 (3163-6353) | 6675 (4738-9403) | 4010 (2821-5700) | 1105 (819-1492) | 2223 (1713-2884) | ||
| 26%-50% | 3904 (2247-6783) | 5867 (4345-7921) | 4365 (3010-6331) | 2215 (1409-3481) | 1054 (795-1398) | 2202 (1754-2764) | ||
| 51%-75% | 1639 (731-3675) | 3958 (3090-5070) | 4133 (3144-5432) | 2190 (1534-3125) | 992 (748-1316) | 2262 (1794-2852) | ||
| 76%-100% | 1984 (1095-3597) | 4969 (3681-6707) | 3943 (2703-5752) | 1408 (1002-1979) | 1113 (883-1404) | 3310 (2738-4001) | ||
| Clinical care health ranking x month | 36.8 | <.001 | ||||||
| 0%-25% | 3789 (2545-5642) | 5646 (4643-6865) | 6425 (5205-7931) | 3493 (2759-4424) | 1096 (929-1293) | 2578 (2225-2987) | ||
| 26%-50% | 1822 (1112-2986) | 4708 (3750-5911) | 5044 (4100-6206) | 2518 (1690-3752) | 1313 (1011-1705) | 2710 (2182-3367) | ||
| 51%-75% | 1828 (790-4230) | 4488 (3182-6330) | 4424 (3147-6219) | 2280 (1415-3674) | 1083 (855-1371) | 2794 (2332-3348) | ||
| 76%-100% | 1659 (944-2917) | 4336 (3209-5860) | 3312 (2371-4626) | 1366 (982-1899) | 827 (650-1051) | 1877 (1467-2402) | ||
| Social and economic health ranking x month | 58.0 | <.001 | ||||||
| 0%-25% | 3667 (2109-6376) | 5842 (3873-8811) | 4248 (2851-6330) | 1581 (1023-2445) | 1234 (923-1651) | 3000 (2399-3752) | ||
| 26%-50% | 2399 (1442-3992) | 4923 (3948-6139) | 3607 (2645-4919) | 1449 (1060-1980) | 1073 (847-1359) | 2865 (2361-3477) | ||
| 51%-75% | 999 (356-2809) | 3616 (2704-4837) | 5380 (3880-7461) | 2298 (1579-3344) | 862 (671-1107) | 2397 (1911-3007) | ||
| 76%-100% | 2382 (1379-4115) | 4974 (3667-6745) | 5759 (3892-8523) | 5202 (3545-7635) | 1128 (836-1521) | 1778 (1346-2348) | ||
| Physical environment health ranking x month | 41.4 | <.001 | ||||||
| 0%-25% | 2120 (1131-3973) | 5370 (3833-7523) | 4061 (2930-5626) | 2529 (1734-3688) | 1010 (783-1305) | 2585 (2092-3195) | ||
| 26%-50% | 2052 (1222-3446) | 4132 (3236-5275) | 3995 (3138-5085) | 1617 (1160-2253) | 1025 (784-1341) | 2278 (1850-2804) | ||
| 51%-75% | 1533 (991-2373) | 4497 (3510-5762) | 4283 (3524-5205) | 2210 (1612-3029) | 1161 (957-1407) | 2221 (1927-2560) | ||
| 76%-100% | 3140 (2123-4642) | 5184 (4105-6547) | 6835 (5177-9025) | 3031 (2234-4111) | 1071 (861-1332) | 2802 (2353-3336) | ||
aUsing the Wald χ2 test.
bP < .05 was considered significant.
cThe Gini index is a summary measure that quantifies economic inequality on a numerical scale ranging from 0 (complete equality) to 1 (complete inequality).12 Data are reported as Gini index x 100.
dThe Robert Wood Johnson Foundation Quality of Life rankings include measures of healthfulness including percentage low birth weight, indices of mental and physical wellness (health and distress), and clinical conditions such as percentage of population aged ≥20 years with diabetes and HIV prevalence.7
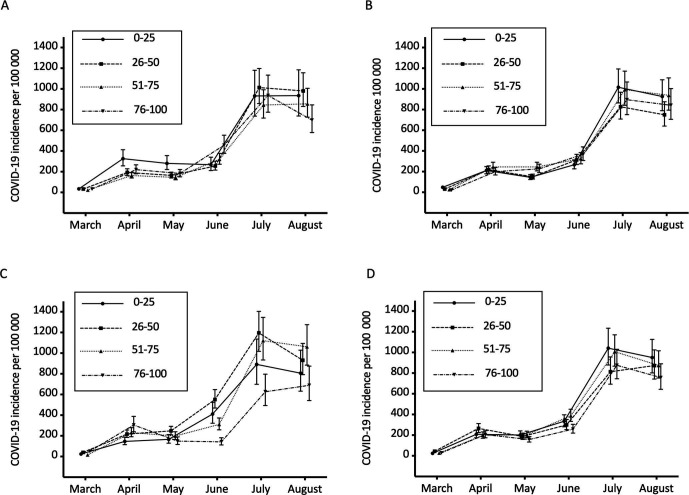
Figure 1.
Adjusted least squares mean COVID-19 incidence per 100 000 population by month and health rankings for (A) health behaviors, (B) clinical care, (C) social and economic factors, and (D) physical environment, Georgia, March 1–August 31, 2020. Error bars indicate 95% CIs.
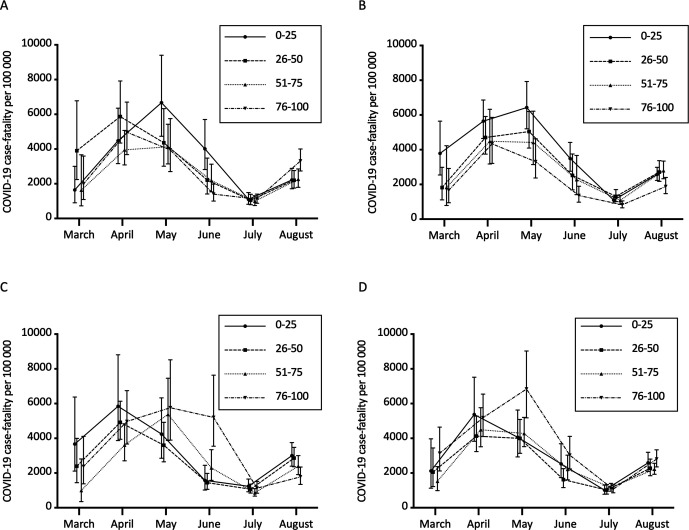
Figure 2.
Adjusted least squares mean COVID-19 case-fatality rate per 100 000 population by month and health rankings for (A) health behaviors, (B) clinical care, (C) social and economic factors, and (D) physical environment, Georgia, March 1–August 31, 2020. Error bars indicate 95% CIs.
COVID-19 Incidence
We found slight differences in COVID-19 incidence over time for the quartiles of each health ranking (Table 2). For health behaviors, the lowest quartile showed slight increases in incidence from March to April, a leveling off from April to June, a large increase from June to July, and another leveling off in August (Figure 1). All other health behavior quartiles showed fairly level COVID-19 incidence from March to May, a slight increase in June, a larger increase in July, and either a leveling off (26%-50% and 51%-75% quartiles) or decrease (76%-100% quartile) in August.
For clinical care quartiles, the 2 lowest quartiles (0%-25% and 26%-50%) had slight increases in COVID-19 incidence from March to April, slight decreases in May, increases in June and July, and slight decreases in August (Figure 1). The 2 highest quartiles had slight increases in COVID-19 incidence from March to April, level incidence from April through June, large increases in July, and slight decreases in August.
In the social and economic quartiles, COVID-19 incidence increased in the highest quartile from March to April, decreased from April through June, and then increased in July and August (Figure 1). The other quartiles had a slight increase in COVID-19 incidence from March through May, larger increases in June and July, and slight decreases in August. For physical environment, all counties had similar incidence rates from March through May, with slight increases in June and larger increases in July. In August, COVID-19 incidence rates decreased in quartiles 0%-25%, 51%-75%, and 76%-100% and increased in quartile 26%-50%.
COVID-19 Case Fatality
We found differences in peak case-fatality rates among quartiles of each health ranking (Figure 2). For health behaviors, the case-fatality rate peaked in the lowest quartile in May and peaked in all other quartiles in April. All case-fatality rates converged in July but then increased again in August. For clinical care, case-fatality rates for the 2 lowest quartiles peaked in May and for the 2 highest quartiles peaked in April. All case-fatality rates converged in July but then increased again in August. For social and economic quartiles, the case-fatality rate peaked for the 2 lowest quartiles in April and for the 2 highest quartiles in May. All case-fatality rates converged in July but then increased again in August. Finally, for physical environment, the case-fatality rate of counties in the highest quartile peaked in May and for all other quartiles in April. All case-fatality rates converged in July but then increased again in August.
Discussion
Indices of County Health and COVID-19 in Georgia
Our analysis indicated that COVID-19 incidence and case-fatality rates in Georgia are associated with indices of socioeconomic and clinical health over time.
Health Outcome Measures and COVID-19 in Georgia
The RWJF health outcome metric comprises 2 variables: length of life (mortality) and quality of life (morbidity). In our study, at the county level, neither variable was significant in the COVID-19 case-fatality multivariable model. Only quality of life was significant in the COVID-19 incidence multivariable model. Other studies have suggested a relationship between COVID-19 clinical outcomes and indices of underlying health conditions.14-17 In early April, the Centers for Disease Control and Prevention COVID-19 Response Team alerted the medical community of an observed association between chronic diseases, such as diabetes, cardiovascular disease, and chronic lung disease, and worsened COVID-19 outcomes.18 Since then, research has found that patients with underlying cardiopulmonary disease have challenging clinical courses when infected with COVID-19.19,20 Although the effect of underlying health conditions may play a role in the pathogenesis of COVID-19 infection and its clinical outcomes, we determined that at a county level, only the RWJF quality-of-life metric predicted COVID-19 incidence in Georgia over time.
Socioeconomic Predictors of COVID-19 Incidence in Georgia
Our analysis found that an increase in COVID-19 incidence was significantly associated with rurality and adverse socioeconomic status at the county level in adjusted models. Rural county status and higher economic inequality as defined by the Gini index both predicted higher COVID-19 incidence in multivariable modeling. Of the health outcome measures, worse quality of life was associated with elevated levels of COVID-19 incidence at the county level. Our findings mirror the findings of Shaw et al,14 who found that poorer US counties demonstrate worse chronic disease outcomes than wealthier counties. These findings suggest a disproportionate risk of COVID-19 incidence among people who may lack access to health care because of financial or geographic barriers. Moore et al15 also found that in Georgia, COVID-19 mortality rates were higher in poorer counties than in more affluent counties. We found increased COVID-19 incidence in counties with a high degree of income inequality as assessed by the Gini index. These findings support an analysis by Clarke and Whiteley,16 who similarly predicted worsened COVID-19 outcomes in US regions characterized by greater income inequality than in regions characterized by lower income inequality. The interaction among all 4 health factor metrics and time was significant. These findings suggest the important relationship between differing socioeconomic determinants of health and COVID-19 incidence during the beginning of the pandemic in Georgia.
Socioeconomic Predictors of COVID-19 Case Fatality in Georgia
COVID-19 case-fatality rates were significantly associated with rural county status. However, although inequality as assessed by the Gini index was significantly associated with COVID-19 incidence, its relationship with the COVID-19 case-fatality rate was not significant. In the adjusted model, the COVID-19 case-fatality rate was significantly associated with all 4 health factors over time. Case-fatality rates for all 4 health factor indices declined and converged in July 2020. However, for all quartiles of county rankings, the COVID-19 case-fatality rate increased in August 2020. These findings suggest a lag between increased COVID-19 incidence noted in July 2020 across all 4 quartiles of counties for each health factor index and the COVID-19 case-fatality rate.
The relationship between COVID-19 case-fatality rate and multiple socioeconomic indices was underscored by their significant associations in adjusted multivariable analysis. The significant correlation of numerous socioeconomic indicators on both the incidence and case-fatality rates of COVID-19 mirrors previous research demonstrating the adverse effect of poverty and economic inequality on the association of non–COVID-19–related health conditions and patient outcomes.21,22 Rural counties and counties with low rankings in clinical care, social and economic health, and physical environment fared poorly in the adjusted multivariable model examining COVID-19 case-fatality rates over time. Data on US county-level economic environments and COVID-19 mortality rates are limited. However, individuals residing in these counties and their potential lack of entry into the health care system because of financial barriers (also known as financial toxicity) may obscure their COVID-19–related mortality rates.23,24 The relationship between COVID-19 mortality and socioeconomic indices reported at a geographic level may guide public health interventions, such as enhanced vaccination strategies targeting populations at high risk of COVID-19 morbidity and mortality. In addition, awareness of these relationships may guide public health activities and funding designed to increase access to COVID-19 vaccines and other therapeutic treatment strategies such as novel immunotherapies for socioeconomically disadvantaged and medically underserved populations.25
A similar study that examined the relationship between socioeconomic determinants of health and COVID-19 cumulative case rates at the county level in Georgia used the RWJF community health rankings at the county level to describe a significant relationship between COVID-19 cumulative rates and indices of socioeconomic determinants of health. However, our analysis and the analysis by Richmond et al26 differ in several key areas. First, our analysis included both incidence and case-fatality rates of COVID-19 as outcomes of interest. Another key difference is the methodology used. The study by Richmond et al used penalized regression techniques on total cumulative cases, whereas our analysis examined the relationship between key socioeconomic determinants of health and monthly COVID-19 incidence and case-fatality rates using repeated measures/longitudinal methods under a Poisson distribution assumption and accounted for the county-level population. The selection of longitudinal analysis techniques examining changes in outcomes by month may allow for better detection of the effect of policy and public health interventions that occurred early in the pandemic in Georgia. Finally, our analysis included other variables of interest, such as the Gini index. The Gini index is a widely accepted indicator of economic inequality, and our analysis detected a key relationship between historically large inequality and COVID-19 incidence rates at the county level in Georgia. This finding further augments both groups’ findings of adverse relationships between COVID-19 incidence and mortality in Georgia’s counties characterized by poor socioeconomic determinants of health.
Limitations
This study had several limitations. First, it was a retrospective study. We included data only through August 31, 2020. Although including data beyond this date could have altered our findings because of the dynamic, unpredictable nature of a pandemic, the 6-month study period may provide public health insights on current and future prevention, testing, and treatment strategies. Second, although every effort was made to include the most current population-level data possible, the variables included in our modeling were sampled from different years. Although these differences could have confounded our analysis, we consistently ensured that data for each variable were available for all 159 counties in Georgia for the sample year. Third, differences in access to COVID-19 testing are described elsewhere.27,28 COVID-19 testing availability has varied in Georgia. Fourth, selection bias may have resulted from these heterogeneous and evolving COVID-19 testing practices. Nevertheless, our analysis adds to the literature on the effect of major clinical, demographic, and socioeconomic indices on COVID-19 incidence and case-fatality rates in Georgia at a granular county level, using well-validated national-level indexed measures of population health.
Conclusions
In Georgia, rural and socioeconomically disadvantaged counties had different patterns of increasing and decreasing COVID-19 incidence and case-fatality rates compared with nonrural and more affluent counties during the study period. Although COVID-19 incidence in Georgia increased from March to August 2020, COVID-19 case-fatality rates declined at the county level toward the end of the 6-month study period. Importantly, the relationship among all 4 RWJF health factor categories and time was significant for COVID-19 incidence and case-fatality rates at the county level. Our analysis of the factors influencing the epidemiology of COVID-19 in Georgia’s counties may enhance our understanding of the challenges in future COVID-19 prevention, testing, and therapeutic efforts across what has been termed “the 2 Georgias.”29
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Adam E. Berman, MD, MSc, MPH https://orcid.org/0000-0002-9023-1130
References
- 1.Holshue ML., DeBolt C., Lindquist Set al. Washington State 2019-nCoV Case Investigation Team. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936. 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC COVID-19 Response Team . Geographic differences in COVID-19 cases, deaths, and incidence—United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):465-471. 10.15585/mmwr.mm6915e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gov. Kemp extends protections for vulnerable Georgians, releases guidance for businesses [press release] . Office of the Governor of the State of Georgia; April 30, 2020. Accessed May 10, 2020. https://gov.georgia.gov/press-releases/2020-04-30/gov-kemp-extends-protections-vulnerable-georgians-releases-guidance
- 4.Georgia Geospatial Information Office . COVID-19 Georgia geospatial data hub. Accessed September 25, 2020. https://covid-hub.gio.georgia.gov
- 5.Remington PL., Catlin BB., Gennuso KP. The County Health Rankings: rationale and methods. Popul Health Metr. 2015;13:11. 10.1186/s12963-015-0044-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson TJ., Saman DM., Lipsky MS., Lutfiyya MN. A cross-sectional study on health differences between rural and non-rural U.S. counties using the County Health Rankings. BMC Health Serv Res. 2015;15:441. 10.1186/s12913-015-1053-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.University of Wisconsin Population Health Institute . 2020 County Health Rankings national data. Accessed May 11, 2020. https://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation
- 8.USA Facts . US coronavirus cases and deaths by state. Updated 2021. Accessed May 11, 2020. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map
- 9.Georgia Department of Public Health, Office of Health Indicators for Planning . Online Analytical Statistical Information System (OASIS): population statistics. 2020. Accessed May 15, 2020. https://oasis.state.ga.us/oasis/webquery/qryPopulation.aspx
- 10.US Department of Commerce, Bureau of Economic Analysis . Regional data. 2018. Accessed May 13, 2020. https://apps.bea.gov/itable/iTable.cfm?ReqID=70&step=1
- 11.US Census Bureau . Small area income and poverty estimates (SAIPE). 2020. Accessed May 12, 2020. https://www.census.gov/data-tools/demo/saipe/#/?map_geoSelector=aa_c&s_measures=aa_snc&s_state=13
- 12.US Census Bureau . Gini index of income inequality. Accessed May 13, 2020. https://data.census.gov/cedsci/table?q=B19083%3A%20GINI%20INDEX%20OF%20INCOME%20INEQUALITY&hidePreview=true&g=0400000US13.050000&tid=ACSDT1Y2018.B19083&y=2018
- 13.Organization for Economic Cooperation and Development . Income inequality, 2020. Accessed June 2, 2020. https://data.oecd.org/inequality/income-inequality.htm
- 14.Shaw KM., Theis KA., Self-Brown S., Roblin DW., Barker L. Chronic disease disparities by county economic status and metropolitan classification, Behavioral Risk Factor Surveillance System, 2013. Prev Chronic Dis. 2016;13:E119. 10.5888/pcd13.160088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore JX., Langston ME., George V., Coughlin SS. Epidemiology of the 2020 pandemic of COVID-19 in the state of Georgia: inadequate critical care resources and impact after 7 weeks of community spread. J Am Coll Emerg Physicians Open. 2020;1(4):527-532. 10.1002/emp2.12127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke H., Whiteley P. Economic inequality can help predict COVID-19 deaths in the US. LSE US Centre. 2020. Accessed June 4, 2020. https://blogs.lse.ac.uk/usappblog/2020/05/06/economic-inequality-can-help-predict-covid-19-deaths-in-the-us/
- 17.CDC COVID-19 Response Team . Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382-386. 10.15585/mmwr.mm6913e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDC COVID-19 Response Team . Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343-346. 10.15585/mmwr.mm6912e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aggarwal G., Cheruiyot I., Aggarwal Set al. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: a meta-analysis. Curr Probl Cardiol. 2020;45(8):100617. 10.1016/j.cpcardiol.2020.100617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo T., Fan Y., Chen Met al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811-818. 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adler NE., Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) .2002;21(2):60-76. 10.1377/hlthaff.21.2.60 [DOI] [PubMed] [Google Scholar]
- 22.Bor J., Cohen GH., Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389(10077):1475-1490. 10.1016/S0140-6736(17)30571-8 [DOI] [PubMed] [Google Scholar]
- 23.Smith KT., Monti D., Mir N., Peters E., Tipirneni R., Politi MC. Access is necessary but not sufficient: factors influencing delay and avoidance of health care services. MDM Policy Pract. 2018;3(1):2381468318760298. 10.1177/2381468318760298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Philippe P., Mansi O. Nonlinearity in the epidemiology of complex health and disease processes. Theor Med Bioeth. 1998;19(6):591-607. 10.1023/A:1009979306346 [DOI] [PubMed] [Google Scholar]
- 25.Chen P., Nirula A., Heller Bet al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with COVID-19. N Engl J Med. 2021;384(3):229-237. 10.1056/NEJMoa2029849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richmond HL., Tome J., Rochani H., Schwind JS., Shah GH., Schwind JS. The use of penalized regression analysis to identify county-level demographic and socioeconomic variables predictive of increased COVID-19 cumulative case rates in the state of Georgia. Int J Environ Res Public Health. 2020;17(21):8036. 10.3390/ijerph17218036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lieberman-Cribbin W., Tuminello S., Flores RM., Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am J Prev Med. 2020;59(3):326-332. 10.1016/j.amepre.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan TQ., Kullar R., Swartz TH., Mathew TA, Piggott DA, Berthaud V. Location matters: geographic disparities and impact of coronavirus disease 2019. J Infect Dis. 2020;222(12):1951-1954. 10.1093/infdis/jiaa583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nelson GD. The two Georgias: disparities in rural health and healthcare. J Ga Public Health Assoc. 2016;5(4):294-296. 10.21633/jgpha.5.401 [DOI] [Google Scholar]