Introduction
Low back pain (LBP) is a very common complaint and is now the number one cause of disability across the globe [5,13]. Both the supraspinous ligament (SSL) and interspinous ligament (ISL) form part of the posterior ligamentous complex, which is believed to play an integral role in the stability of the thoracolumbar spine [8]. The SSL begins at the C7 spinous process and extends to L3 and L4 in 22% and 74% of adults, respectively [11]. In contrast, the ISL is formed by a fibrous sheet of dense connective tissue that connects the spinous process of adjacent vertebrae and is most developed in the lumbar region [8,4]. Historically, SSL and ISL injuries have been grouped together with strains and sprains of the lumbar spine [6].
With the improvement of imaging modalities, we now have the ability to more specifically diagnose SSL and ISL sprains that lead to acute and chronic lower back pain [8]. Through the novel technique of ultrasound-guided leukocyte-rich platelet-rich plasma (LR-PRP) injection targeted to the SSL and ISL, treatment of SSL and ISL sprains is possible when other conservative treatments—such as over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, rest, and physical therapy (PT)—fail.
This case report highlights the clinical value of ultrasound as both a diagnostic and therapeutic tool. Here, we present 2 cases of SSL and ISL injuries that failed multimodal treatment plans and had success with ultrasound-guided LR-PRP injections.
Case Report
Case 1
A 28-year-old former collegiate runner presented with achy LBP for 2 years; his complaints began after increasing his running volume. The LBP intensity ranged from 3 to 9/10 and was worse with prolonged standing, sitting, or running. He reported no improvement with 3 prior courses of PT, NSAIDs, and use of a seat cushion. Physical examination revealed mild right thoracolumbar curvature. Tenderness was appreciated over the L5 spinous process and interspinous region above and below L5. Strength, sensation, and reflexes were normal.
Radiographs were unremarkable. Magnetic resonance imaging (MRI) revealed remodeling of an old left L5 pars stress fracture without spondylolisthesis, stenosis, or disk herniation. Bedside ultrasound confirmed maximal tenderness at the tip of the L5 spinous process. The SSL appeared hypoechoic and thickest at L3 and L4 levels.
Next, he underwent a diagnostic injection. Using ultrasound guidance, the SSL at L5 and ISL at L4-L5 were injected with 2 to 3 mL of 1% lidocaine total. He reported 100% relief of symptoms during the anesthetic phase and improvement for 1 week, after which symptoms returned. Given the positive diagnostic response, he then underwent an injection of LR-PRP to the same site. Under ultrasound guidance, the needle was then guided to the SSL and ISL as previously described. Autologous LR-PRP (3.5 mL) was injected at these sites. At 6 weeks postinjection, he reported >70% reduction in pain and improved function but had not returned to running. At 6 months postinjection, he was running and exercising with no limitations (Fig. 1).
Fig. 1.
Ultrasound of L4–L5 region using a high frequency linear transducer in short axis in Case 1. (a) Ultrasound-guided injection showing needle tip at the interspinous space of the L4–L5 vertebrae targeting the ISL. (b) Ultrasound-guided injection showing needle tip at the supraspinous ligament superior to the L5 vertebra.
Case 2
A 29-year-old man presented with intermittent LBP for 8 months; his complaints began during an extension maneuver. Prior workup led to PT emphasizing core strengthening, but his LBP persisted. Magnetic resonance imaging was unremarkable. A previous palpation-guided cortisone injection offered 75% relief for 1 week before LBP returned to baseline.
At our initial consultation, the LBP was described as sharp/achy/dull and rated 5/10 at its worst and 3/10 at its best. Bending forward or backward exacerbated the pain. Physical examination findings revealed approximately 20% motion restriction on lumbar flexion. The ISLs were focally tender at L1–L3, and the neurological examination was normal. First, a fluoroscopically guided interspinous steroid injection at L1–L2 and L2–L3 was performed. At 1 month postinjection, he reported >50% relief of symptoms for 2 to 3 weeks after the injection, after which the LBP returned to baseline.
Next, he underwent an LR-PRP injection. The L1–L2 and L2–L3 spinous process and ISLs in between them, at areas of maximal tenderness to palpation, were marked and autologous LR-PRP (1.5 mL) was injected at each site. He reported some pain, but the procedure was tolerated well. At 1 month postinjection, he reported 10% improvement and was advised to continue his home exercise program to restore range of motion and improve core strength. At 6 weeks postinjection, he reported 75% improvement with near-full range of motion and minimal pain. At 9 months postinjection, he reported nearly 100% improvement (Fig. 2).
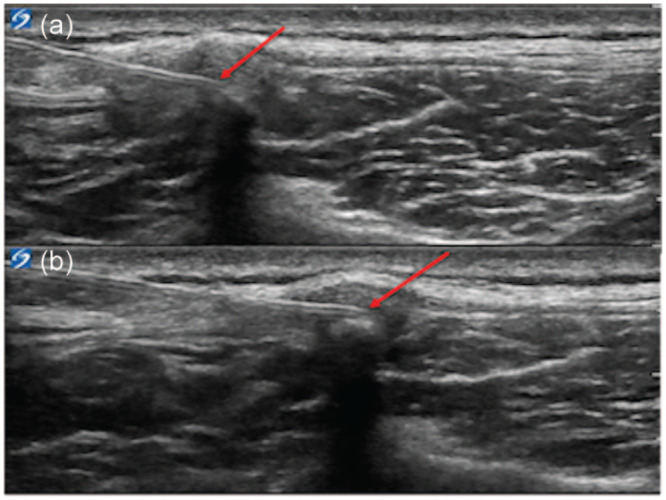
Fig. 2.

Ultrasound of L1–L2 and L2–L3 region using a high frequency linear transducer in long axis in Case 2. (a) Ultrasound-guided injection showing needle tip at the interspinous space of L1–L2 targeting the ISL. (b) Ultrasound-guided injection showing needle tip at the interspinous space of L2–L3.
Discussion
The cause of LBP can be challenging to diagnose and treat. By using imaging modalities, specifically ultrasound, it is evident that the SSL and ISL can be a source of LBP. Ultrasound can be used to guide diagnostic and therapeutic injections for SSL and ISL injuries. After identifying an injury to the SSL and/or ISL a multimodal approach is often initiated, including PT, medications, and steroid injections. To our knowledge, there are no reports of an ultrasound-guided PRP injection to treat SSL and ISL pathology.
In these 2 reported cases, the patients did not respond to traditional multimodal approaches. Injections of LR-PRP were found to be successful in treating SSL and ISL injuries. The literature is scarce regarding the diagnosis and treatment of pain generated from the SSL and ISL. Heylings [7] analyzed 28 cadaveric specimens by dissection and histological examination and demonstrated that the SSL and ISL are connected and play an important role in spinal stability, opposing lumbar flexion. With flexion, loading of the spine shifts to the posterior elements, which become denser with greater load bearing [14]. According to Solomonow [12], ligaments are able to monitor relevant kinesthetic and proprioceptive information. Ligaments can be acutely inflamed from long-term exposure to static or cyclic high loads, long load duration, and high number and frequency of load repetitions. MRI is considered the modality of choice in assessing ligamentous pathology [14]. However, a study by Zhao et al [15] showed that ultrasound can be a reliable complementary diagnostic tool for evaluating the posterior ligamentous complex. In case 1, ultrasound was used to guide the diagnostic block. In both cases, ultrasound was used to guide the therapeutic injection that gave the patient significant pain relief.
Platelet-rich plasma (PRP) includes numerous growth factors, such as transforming growth factor-β1, insulin-like growth factors 1 and 2, and vascular endothelial growth factor [15]. Several studies have demonstrated success with injecting PRP to treat ligaments. Podesta et al analyzed 34 athletes who received ultrasound-guided LR-PRP injections for the treatment of grade I and II ulnar collateral ligament sprains [9,10]. By 6 months, 88% of athletes had returned to play without complaints at the same level, had improvement in outcomes scores, and showed decreases in medial elbow joint space gapping from 7 to 2.5 mm. Bagwell et al [1] reported a case of a series of LR-PRP injections, along with early rehabilitation, that showed promise in treating an acute grade III medial collateral ligament injury. Given the reported success of PRP in treating ligaments, and the fact that the patients in our cases had exhausted other conservative treatment modalities, PRP was considered a reasonable next step in treatment.
Although an extensive review of the literature has uncovered no reports of an ultrasound-guided PRP injection for treating specifically SSL and/or ISL pathology, Darrow et al [3] showed the benefits of injecting PRP into the back in 1, 2, or 3 injections. However, these injections were not image-guided and were instead performed at patient-reported areas of tenderness [1]. In the current cases, MRI was nondiagnostic, but ultrasound allowed for the identification of the site of pain with sonopalpation and identification of abnormal hypoechoic areas in the SSL and ISL corresponding to the patients’ pain. Ultrasound was not only helpful with diagnosis, but it also served a therapeutic role by allowing for needle guidance to the site of ligament injury, thus facilitating positive outcomes.
There were a few limitations to these cases. As the injected LR-PRP for each patient was not sent to a laboratory, cell counts were not analyzed. In addition, there was no ultrasound imaging in follow-up visits. Needle tenotomy was performed while injecting the LR-PRP, and it is unknown whether simply tenotomizing the ligament without injecting LR-PRP could have given similar results. Finally, the appropriate postinjection rehabilitation protocol is unknown, which also could have an impact on the treatment results. Overall, these cases highlight the importance of considering the SSL and ISL as potential pain generators. They also highlight a potentially effective interventional treatment option in atypical cases of LBP and in refractory cases of lumbar ligament sprains. Further work should include prospective studies aimed at determining the optimal cell counts in the LR-PRP sample, at answering whether needle tenotomy to the ligaments can be as effective as LR-PRP, and at identifying the optimal postinjection rehabilitation protocol.
Supplemental Material
Supplemental material, sj-zip-1-hss-10.1177_1556331621992312 for Successful Treatment of Supraspinous and Interspinous Ligament Injury With Ultrasound-Guided Platelet-Rich Plasma Injection: Case Series by Andrew Creighton, Roger A. Sanguino, Jennifer Cheng and James F. Wyss in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was waived from the patients included in this case study.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
References
- 1.Bagwell MS, Wilk KE, Colberg RE, Dugas JR. The use of serial platelet rich plasma injections with early rehabilitation to expedite grade III medial collateral ligament injury in a professional athlete: a case report. Int J Sports Phys Ther. 2018;13(3):520–525. 10.26603/ijspt20180520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behrsin JF, Briggs CA.Ligaments of the lumbar spine: a review. Surg Radiol Anat. 1988;10(3):211–219. 10.1007/BF02115239. [DOI] [PubMed] [Google Scholar]
- 3.Darrow M, Shaw B, Nicholas S, Li X, Boeger G.Treatment of unresolved lower back pain with platelet-rich plasma injections. Cogent Med. 2019;6(1):1–10. 10.1080/2331205x.2019.1581449. [DOI] [Google Scholar]
- 4.Dickey JP, Bednar DA, Dumas GA.New insight into the mechanics of the lumbar interspinous ligament. Spine. 1996;21(23):2720–2727. [DOI] [PubMed] [Google Scholar]
- 5.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. 10.1016/S0140-6736(18)30480. [DOI] [PubMed] [Google Scholar]
- 6.Hebert JJ, Koppenhaver SL, Walker BF.Subgrouping patients with low back pain: a treatment-based approach to classification. Sports Health. 2011;3(6):534–542. 10.1177/1941738111415044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heylings DJ.Supraspinous and interspinous ligaments of the human lumbar spine. J Anat. 1978;125(pt 1):127–131. [PMC free article] [PubMed] [Google Scholar]
- 8.Lee JY, Vaccaro AR, Schweitzer KM, et al. Assessment of injury to the thoracolumbar posterior ligamentous complex in the setting of normal-appearing plain radiography. Spine J. 2007;7(4):422–427. 10.1016/j.spinee.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 9.Paoloni J, De Vos RJ, Hamilton B, Murrell GA, Orchard J.Platelet-rich plasma treatment for ligament and tendon injuries. Clin J Sport Med. 2011;21(1):37–45. 10.1097/JSM.0b013e31820758c7. [DOI] [PubMed] [Google Scholar]
- 10.Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA.Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689–1694. 10.1177/0363546513487979. [DOI] [PubMed] [Google Scholar]
- 11.Rissanen PM.The surgical anatomy and pathology of the supraspinous and interspinous ligaments of the lumbar spine with special reference to ligament ruptures. Acta Orthop Scand. 1960;46:1–100. 10.3109/ort.1960.31.suppl-46.01. [DOI] [PubMed] [Google Scholar]
- 12.Solomonow M.Sensory-motor control of ligaments and associated neuromuscular disorders. J Electromyogr Kinesiol. 2006;16(6):549–567. 10.1016/j.jelekin.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. 10.1016/S0140-6736(16)31678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang JF, Liu C, Yu HJ, Ma JJ, Cai HX, Fan SW.Degenerative changes in the interspinous ligament. Acta Orthop Traumatol Turc. 2014;48(6):661–666. 10.3944/AOTT.2014.13.0149. [DOI] [PubMed] [Google Scholar]
- 15.Zhao JW, Liu Y, Yin RF, Wang JC, Yang YH, Liu P.Ultrasound assessment of injury to the posterior ligamentous complex in patients with mild thoracolumbar fractures. J Int Med Res. 2013;41(4):1252–1257. 10.1177/0300060513483407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-zip-1-hss-10.1177_1556331621992312 for Successful Treatment of Supraspinous and Interspinous Ligament Injury With Ultrasound-Guided Platelet-Rich Plasma Injection: Case Series by Andrew Creighton, Roger A. Sanguino, Jennifer Cheng and James F. Wyss in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery


