Abstract
Background
Doctors‐in‐training report elevated rates of mental disorders and high levels of stress. Whilst a number of work‐related sources of stress have been identified in the medical profession, it remains unclear as to the relative importance of workplace stressors for mental ill‐health in junior doctors.
Aims
To examine workplace stressors reported by junior doctors and identify variables associated with adverse mental health outcomes.
Methods
Cross‐sectional analysis of national 2013 survey of Australian doctors focussing on junior medical officers (N = 3053; 24.9% of total sample). Primary outcomes were caseness of common mental disorder (CMD) and suicidal ideation in the past year.
Results
Perceived level of conflict between study/career and family/personal responsibility (OR = 3.76, 95% CI: 2.61–5.43; P < 0.01) and sleep deprivation (OR = 2.19, 95% CI: 1.46–3.28; P < 0.01) were significantly associated with CMD, while perceived level of conflict between study/career and family/personal responsibility (OR = 3.13, 95% CI: 1.78–5.50; P < 0.01) and bullying (OR = 2.92, 95% CI: 1.42–6.03; P < 0.01) were most strongly associated with suicidal ideation in adjusted models.
Conclusion
This study identifies modifiable workplace variables that are influential in junior doctors' mental health, and in doing so, provides meaningful evidence‐informed targets for future interventions to prevent suicide and mental disorder in this population.
Keywords: mental disorder, doctors, work, stress, suicide, suicidal ideation
Introduction
Internationally, doctors report substantial rates of mental health problems, including depression,1 anxiety,2 burnout and suicide.3 Doctors' mental ill‐health has considerable negative impacts, not only for the individual, but for the quality of patient care and the healthcare system.4 Of particular concern are the elevated rates of mental disorders and suicide seen among doctors early in their career,5 especially in the first few years of post‐registration training.1 A recent review of longitudinal studies showed a significant increase of 15.8% in depressive symptoms among junior doctors within a year of beginning residency.1 In the UK, one‐quarter of surveyed junior doctors working in the National Health Service (NHS) reported that their mental health is often adversely affected by their job.6 Elevated rates of suicidal ideation are also reported in medical students and junior doctors7, 8 with prospective data demonstrating a marked increase in suicidal ideation after the start of residency.9
To date, a substantial body of literature has identified a range of potential sources of stress experienced by doctors. Long working hours, shift work, insecurity regarding career progression, excessive workload, high job demands, fatigue, work−life imbalance and bullying have been suggested as important in understanding doctors' mental health.5, 10, 11, 12 Gender has also been identified by some studies as a moderator of the relationship between workplace stressors and mental health in physicians. While such studies are informative, there is a central problem in that they generate a long list of potential variables associated with mental health problems in doctors, yet it remains unclear which factors are the most important in determining junior doctors' mental health. Examination of the relative importance of these factors, and identification of those that could be modifiable, is crucial to develop more effective, targeted interventions for this group.
This study examines data from a national survey of doctors in Australia to establish which work‐related factors are most important for understanding rates of common mental disorder and suicidal ideation among junior doctors.
Methods
Sampling strategy
This study utilised data collected as part of the 2013 Australian Beyond Blue National Mental Health Survey of Doctors and Medical Students. A detailed methodology of the survey has been published previously.13 Briefly, between February and April 2013, a randomly selected sample of 42 942 doctors was invited to participate in an online or paper survey assessing mental health and wellbeing. Participation was voluntary and anonymous, and a total of 12 252 doctors completed the survey (response rate approximately 27%). For the purposes of this study, medical students, and doctors who had completed training (consultants) or were retired, were excluded from this analysis. The population of interest was employed Junior Medical Officers (JMO), including interns, pre‐vocational trainees and vocational trainees, across all specialities and training programmes. A total of 3053 JMO representing 24.9% of the available sample comprised the final sample used for analyses. The recruitment and data collection in the original survey was approved by Monash University Human Research Ethics Office and Committee (CF12/2295–2 012 001 228). This study has been approved by University of New South Wales Human Research Ethics Office (HC190896).
Measures
Demographics
Demographic variables of interest were gender (male, female), age in years, stage of training (intern, pre‐vocational trainee, vocational trainee), number of children living at home (none vs one or more children), location of primary place of work (metropolitan vs rural/regional/remote), location of undergraduate training (overseas vs in Australia) and estimated average working hours per week (0–168 h).
Workplace stressors
Each participant was asked the degree to which they had felt stressed by a list of 23 work‐related events. Responses were provided on a three‐point Likert scale ranging from 0 ('not at all stressed'), 1 ('not that stressed') and 2 ('very stressed'). Higher scores indicate a greater degree of stress perceived by the individual in relation to that particular workplace event. A full list of the 23 workplace stressors is provided in Figure 1.
Figure 1.
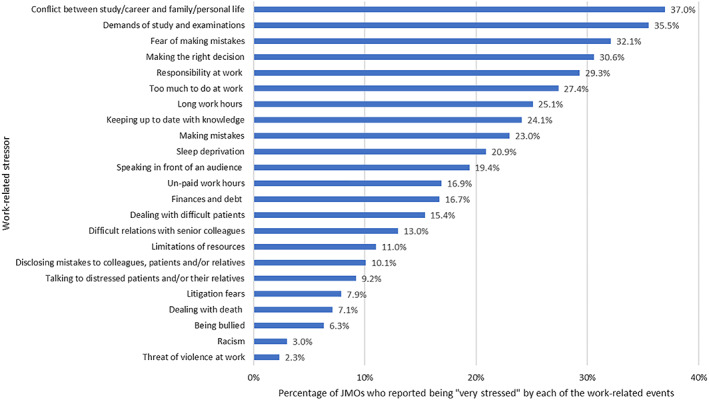
Frequency of different work‐related events being reported as 'very stressful' by junior medical officers (N = 3053).
Mental health outcomes
Caseness of common mental disorder (CMD) was assessed using the 28‐item General Health Questionnaire (GHQ‐28).14 A cut‐off of 4 on the total GHQ‐28 score was used as the threshold, with a score of 5 or above indicating a likely case of CMD. The binary scoring method was used (0–0–1‐1),14 which is comparable to clinician‐delivered diagnostic assessment.15 The presence of suicidal ideation (SI) in the past year was assessed using a single yes/no item asking: 'During the last 12 months, have you had thoughts of taking your own life?' where a positive response indicated presence of suicidal thoughts.
Statistical analysis
All analyses were performed using the IBM SPSS and STATA software programmes (v24). Descriptive statistics and logistic regression were used to describe the sample and frequency of stressful work‐related events, estimate prevalence of CMD and SI, and to identify any demographic variables that were significantly associated with CMD status and SI. In the subsequent regression analyses, a dichotomised variable for each stressor was used ('not at all stressed' and 'not that stressed' (0) vs 'very stressed' (1)).
A three‐step process was used to investigate the associations between each of the 23 workplace variables and the mental health outcomes. First, a series of univariate logistic regression analyses were performed to assess the relationship of each individual workplace stressor with CMD status, and with presence of SI. Second, a series of unadjusted and adjusted logistic regressions were conducted to investigate the associations between each workplace stressor and each outcome. A set of potential confounders to account for in the adjusted models was established a priori in light of existing research, including age, gender, stage of training, location of primary place of work, number of children living at home, and whether medical training was undertaken overseas. Third, adjusted backwards stepwise logistic regression analyses were conducted using Likelihood Ratio method and excluding variables from the model if P > 0.10. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated as adjusted estimates of effect size. To investigate if relative importance of workplace risk factors differed according to gender, adjusted backwards stepwise analyses were re‐run separately for male and female JMO. Finally, to examine the potential importance of each variable as a target for future interventions, we computed the population attributable fractions (PAF) using the punaf command in STATA for CMD and SI.
Results
Data were available for 3053 JMO, of whom more than half were enrolled in a specialist or vocational training programme (n = 1883; 61.7%). The majority were female (n = 1861; 61%), aged between 26 and 30 (n = 1010; 33.1%) or 31 and 40 years of age (n = 1174; 38.5%), and worked largely in hospital (n = 2299; 75.3%) or group‐based practice (593; 19.4%) settings. Most JMO reported being married (n = 1450; 47.5%) or in a committed relationship (n = 780, 25.5%), and 64.7% reported having no children living at home (n = 1975; 64.7%). Just over one‐quarter of the sample (28.8%) had undertaken their medical training overseas.
Of the 3053 doctors in training, 35.8% (n = 1054) reported symptom levels indicative of CMD. Rates of CMD were significantly higher among younger JMO (P = 0.012) and females (P < 0.01). In addition, overseas training (P < 0.01), location (P = 0.03) and number of children living at home (P = 0.02) were significantly associated with CMD. 12.4% (n = 378) JMO reported having experienced SI during the past 12 months, with overseas training (P < 0.01) and location (P = 0.04) significantly associated with this outcome. Supporting Information Tables S1 and S2 summarise key demographic characteristics and their associations with CMD and SI respectively.
Figure 1 shows the work‐related events that were most frequently reported to be perceived as 'very stressful' by JMO. The work‐related events most commonly described as being very stressful were: (i) conflict between study/career and family/personal responsibilities; (ii) demands of study and examinations; (iii) fear of making mistakes; and (iv) making the right decision.
The subjective level of stress reported for each of the workplace events was significantly positively associated with CMD caseness (P < 0.01) and with the presence of suicidal thoughts in the past year among JMO (P < 0.01). In the adjusted logistic regression model (Table S3), the two workplace variables that had the largest effect on the likelihood of a JMO displaying case‐level symptoms of CMD were the level of conflict between study/career and family/personal responsibility (OR = 7.04, 95% CI: 5.32–10.04; P < 0.001) and sleep deprivation (OR = 5.14, 95% CI: 3.65–7.23; P < 0.01). Difficult relations with senior colleagues, responsibility at work, and long work hours also demonstrated pronounced positive associations with CMD among JMO. Conflict between study/career and family/personal responsibility (OR = 4.64, 95% CI: 2.75–7.81; P < 0.01), bullying (OR = 3.69, 95% CI:1.99–6.84, P < 0.01) and fear of litigation (OR = 3.21, 95%CI: 1.79–5.75; P < 0.01)were most strongly associated with presence of SI in JMO over the past 12 months (Table S4).
Tables 1 and 2 outline the risk factors identified in the final adjusted backwards logistic regression model and their associated estimated OR, 95% CI and PAF, for CMD and SI respectively. On the basis of the final adjusted multivariate model, PAF for CMD and SI were estimated. Assuming causality and a lack of residual confounding, these results suggest 36% of new cases of CMD in JMO could be prevented through the elimination of conflict between the demands of study/career and family/personal responsibility (PAF = 0.36, 95% CI: 0.25–0.45; P < 0.001) and 10% of new CMD cases could be prevented if the stress of study and exams (PAF = 0.10, 95% CI: 0.21–0.35; P < 0.001) was removed. Assuming causality and a lack of residual confounding, the PAF suggest that 47% of cases of SI in JMO (PAF = 0.47; 95% CI: 0.25–0.63) could be prevented through the elimination of conflict between the demands of study/career and family/personal responsibility, and 14% of instances of SI could be prevented by the elimination of stress associated with finances and debt (PAF = 0.14; 95% CI: 0.001–0.26).
Table 1.
Work‐related risk factors for CMD among JMO with adjusted estimates for effect size (OR; 95% CI) using backwards stepwise regression and their population attributable fractions (PAF) in the final model† (N = 997)
| Adjusted‡ OR (95% CI) | P‐value | PAF (95% CI) | |
|---|---|---|---|
| Conflict between study/career and family/personal responsibility | 3.76 (2.61–5.43)** | <0.001 | 0.36 (0.25–0.45) |
| Difficult relations with senior colleagues | 2.74 (1.65–4.57)** | <0.001 | 0.05 (0.02–0.08) |
| Sleep deprivation | 2.19 (1.46–3.28)** | <0.001 | 0.09 (0.04–0.14) |
| Demands of study and examinations | 1.62 (1.14–2.30)** | 0.007 | 0.10 (0.02–0.17) |
| Finances and debt | 1.68 (1.14–2.49)* | 0.01 | 0.05 (0.01–0.10) |
| Long work hours | 1.58 (1.07–2.33)* | 0.02 | 0.06 (0.01–0.11) |
| Fear of making mistakes | 1.43 (0.98–2.08) | 0.06 | 0.05 (−0.005–0.09) |
Dependent variable: Likely case of common mental disorder, as defined by a total score of 5 or above on the GHQ‐28.
Adjusting for age, gender, location (metropolitan vs rural/regional/remote), stage of training, number of children living at home (none vs one or more) and whether training was undertaken overseas (yes vs no).
* Significant at P < 0.05. **Significant at P < 0.001. CI, confidence interval; OR, odds ratio; PAF, population attributable fractions.
Table 2.
Work‐related risk factors for SI among JMO with adjusted estimates for effect size (OR; 95% CI) using backwards stepwise regression (likelihood ratio method of entry), and their population attributable fractions (PAF) in the final model† (N = 1035)
| Adjusted‡ OR (95% CI) | P‐value | PAF (95% CI) | |
|---|---|---|---|
| Conflict between study/career and family/personal responsibility | 3.13 (1.78–5.50)** | <0.01 | 0.47 (0.25–0.63) |
| Bullying | 2.92 (1.42–6.03)** | <0.01 | 0.10 (0.02–0.16) |
| Litigation fears | 2.13 (1.14–4.00)* | 0.02 | 0.08 (−0.001–0.15) |
| Finances and debt | 1.76 (1.07–2.90)* | 0.03 | 0.14 (0.001–0.26) |
| Sleep deprivation | 1.56 (0.93–2.60) | 0.09 | 0.11 (−0.03–0.24) |
| Racism | 0.27 (0.06–1.13) | 0.08 | −0.05 (−0.10 ‐ ‐0.008) |
SI: Suicidal ideation in the past 12 months, indicated by a positive response to a single item.
Adjusting for age, gender, location (metropolitan vs rural/regional/remote), stage of training, number of children living at home (none vs one or more) and whether training was undertaken overseas (yes vs no). * Significant at P < 0.05. **Significant at P < 0.001. CI, confidence interval; OR, odds ratio; PAF, population attributable fractions.
Backwards stepwise regression models were repeated for male and female JMO separately in relation to CMD (Table S5) and SI (Table S6). In general, similar sets of work‐related variables emerged as important for both genders in relation to both mental health outcomes.
Discussion
This is the first study to examine the relative importance of a range of work‐related variables for understanding the risk of CMD and SI among junior doctors using national‐level data. Importantly, this study identified several work‐related factors that contribute to the risk for CMD and/or SI in junior doctors. These results pinpoint modifiable variables that emerge as risk factors for adverse mental health outcomes in junior doctors and identify the potential for improvements at a population‐level.
Overall, the results attest to the multifactorial nature of doctors' mental health. The findings highlight that individual, team‐level and organisation‐level variables all influence junior doctors' wellbeing and suggest that a single‐level approach will not be sufficient to address this complexity. This is consistent with recent models of workplace mental health,16 which advocate for a multiple‐level approach, and with the medical community's call for the adoption of a wholistic multi‐level approach to doctors' wellbeing across the entire career.17 A systematic review and meta‐analysis of controlled trials to reduce mental illness in doctors18 identified no trials of organisational‐level interventions that assessed symptoms of CMD in physicians, despite evidence for the benefits of organisational interventions for other measures of employee wellness burnout.19 Both organisational and individual strategies warrant further research in trials to address mental illness and suicide in junior doctors. For instance, Cognitive Behavioral Therapy and mindfulness interventions have demonstrated positive outcomes for perceived stress and mental ill‐health in doctors18, 20 and our results suggest these could be utilised in junior doctors.
The findings suggest that stress associated with conflict between career and personal responsibility may be one of the most important factors to target at a population level as it demonstrated the largest PAF in the final adjusted models. This is similar to the concept of work‐life balance, a common stressor reported by doctors worldwide.21, 22, 23 Poor work‐life balance and high levels of occupational stress have been associated with adverse mental and physical health outcomes such as burnout11 and poorer self‐rated health24 in cross‐sectional studies of doctors. Prospective studies suggest poor working conditions and psychosocial work stressors have a detrimental effect on the future health of doctors.24, 25
What is unique here is that the current study identifies the association between work/life conflict and poorer mental health in junior doctors at the beginning of their career, suggesting that this struggle begins early and is ongoing. Conversely, this also suggests that if equipped with skills early on, and crucially, if embedded within a work system and training environment that allows for healthier work−life balance, junior doctors may be able to manage these conflicts effectively throughout their career. Measures promoting healthy work‐study‐life balance for junior doctors need to be considered by workplaces and medical colleges, including appropriate staffing and rostering practices, regulating healthy work hours and protected study time within rosters.5 Similarly, sleep deprivation was highlighted as a risk factor for CMD and may be aided by improving shift scheduling and protecting time off‐duty, strategies that have demonstrated reductions in occupational stress in healthcare workers.26
Difficult relations with senior colleagues were associated with CMD among junior doctors, consistent with research showing inadequate peer and supervisor support is associated with poor mental health in physicians.27 An unsupportive work environment has been prospectively associated with later psychiatric symptoms in general workers and physicians.28 Further, bullying was associated with SI in this study, highlighting the need for team‐based strategies to prevent bullying at all levels of seniority, and for provision of adequate support for both individuals who have personally experienced bullying, and for colleagues who may have been vicariously impacted by such incidents, given that the detrimental impact of workplace aggression has been demonstrated in the wider team.29, 30 More generally, the degree of social support in a workplace has been established as critical for employee wellbeing and stress,31 a relationship also identified here in junior doctors.
This study has some limitations. First, multicollinearity between work‐related variables may mean the effect sizes in the adjusted models are underestimations of the true effect. Second, the stressors assessed in the study are subjective and open to differences in interpretation. The use of cross‐sectional data limits conclusion around causality. There is potential for reverse causation and residual confounding, which may have affected effect size estimates. Prospective studies assessing cohorts of junior doctors throughout postgraduate training to assess effects of workplace stressors over time, and to evaluate whether the current findings hold in relation to risk of future mental health outcomes and suicidality, are needed. Other unexamined factors may also contribute to the risk for CMD symptoms and SI that were not assessed in the survey. While the set of 23 variables assessed by the original survey is not an exhaustive list of stressors experienced by junior doctors, the survey included variables identified in previous literature as important to doctors' mental health. The survey did not ask participants to report on frequency of occurrence. The results may not be generalisable to other countries or timepoints and were collected in 2013. This study uses the most recent national dataset assessing doctors' mental health to our knowledge, and adds to the limited literature on Australian samples.
Conclusion
The study identifies key modifiable work‐related factors that are significantly associated with CMD and SI among junior doctors. These results can inform the development of targeted interventions to reduce mental illness and suicide among this population. In particular, the findings suggest that reducing stress associated with the work‐study‐life conflict, and addressing relations with senior colleagues, bullying and sleep deprivation must be given priority in future research. There is a pressing need to evaluate interventions to improve the mental health of junior doctors. This study hopes to stimulate and inform such efforts.
Supporting information
Table S1. Sociodemographic factors and association with CMD status (N = 3053).
Table S2. Sociodemographic factors associated with presence of suicidal ideation among JMO (N = 3048).
Table S3. Associations between a range of potentially stressful work‐related events and CMD in JMO, with unadjusted and adjusted estimates for effect size (OR; 95% CI), using logistic regression (N = 2948).
Table S4. Associations between a range of potentially stressful work‐related events and SI in JMO, with unadjusted and adjusted estimates for effect size (OR; 95% CI), using logistic regression (N = 2948).
Table S5. Final models obtained using backwards stepwise regression, stratified by gender, and listed in order of magnitude for each group, with adjusted estimates for effect size (OR; 95% CI) for CMD.
Table S6. Final adjusted models obtained using backwards stepwise regression, stratified by gender, and listed in order of magnitude for each group, with adjusted estimates for effect size (OR; 95% CI) for SI.
Acknowledgements
Acknowledgements are due to Beyond Blue, the Project Advisory Group and members of the research team for undertaking the initial 'National Mental Health Survey of Doctors and Medical Students' survey in 2013, and to the participants involved for their time.
Funding for this study was provided by the Health Workforce Programme, Commonwealth Department of Health, Australian Government, iCare Foundation and NSW Health. K. Petrie is supported by an Australian Government Research Training Program Scholarship and a scholarship supported by NSW Health.
Conflict of interest: None.
Disclosure: S. B. Harvey, F. Shand and J. Crawford are employed by the Black Dog Institute, a not for profit research institute that provides mental health training to a range of organisations; all other co‐authors declare no other relationships or potential conflicts of interest.
Contributor Information
Katherine Petrie, Email: katherine.petrie@unsw.edu.au.
Joanna Crawford, Email: joanna.crawford@blackdog.org.au.
Fiona Shand, Email: fionas@unsw.edu.au.
Samuel B. Harvey, Email: s.harvey@unsw.edu.au
References
- 1.Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio Eet al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta‐analysis. JAMA 2015; 314: 2373–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruitenburg MM, Frings‐Dresen MH, Sluiter JK. The prevalence of common mental disorders among hospital physicians and their association with self‐reported work ability: a cross‐sectional study. BMC Health Serv Res 2012; 12: 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio‐economic, demographic and psychiatric differences. Psychol Med 2007; 37: 1131–40. [DOI] [PubMed] [Google Scholar]
- 4.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VWet al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 2008; 336: 488–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tyssen R, Vaglum P. Mental health problems among young doctors: an updated review of prospective studies. Harv Rev Psychiatry 2002; 10: 154–65. [DOI] [PubMed] [Google Scholar]
- 6.Tweedie J, Goh Y, Postlethwaite C, Choudry M, Cantelo G, Dacre Jet al. Current challenges facing junior doctors in the NHS: a quantitative survey. Clin Med 2017; 17(Suppl 3): s31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brazeau CM, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier Cet al. Distress among matriculating medical students relative to the general population. Acad Med 2014; 89: 1520–5. [DOI] [PubMed] [Google Scholar]
- 8.Tyssen R, Vaglum P, Grønvold NT, Ekeberg Ø. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord 2001; 64: 69–79. [DOI] [PubMed] [Google Scholar]
- 9.Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter Jet al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry 2010; 67: 557–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loretto W, Popham F, Platt S, Pavis S, Hardy G, MacLeod Let al. Assessing psychological well‐being: a holistic investigation of NHS employees. Int Rev Psychiatry 2005; 17: 329–36. [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele Det al. Burnout and satisfaction with work‐life balance among US physicians relative to the general US population. Arch Intern Med 2012; 172: 1377–85. [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Sloan JA, Habermann TM. The well‐being of physicians. Am J Med 2003; 114: 513–9. [DOI] [PubMed] [Google Scholar]
- 13.Beyondblue . National mental health survey of doctors and medical students. Melbourne: beyondblue; 2013. [Google Scholar]
- 14.Goldberg D, Williams P. A Users Guide to the General Healthcare Questionnaire: GHQ, Vol. 1988. Windsor, UK: NFER‐NELSON; 1991. [Google Scholar]
- 15.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje Oet al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27: 191–7. [DOI] [PubMed] [Google Scholar]
- 16.Petrie K, Joyce S, Tan L, Henderson M, Johnson A, Nguyen Het al. A framework to create more mentally healthy workplaces: a viewpoint. Aust N Z J Psychiatry 2018; 52: 15–23. [DOI] [PubMed] [Google Scholar]
- 17.Gerada C. Doctors and mental health. Occupational Medicine. 2017; 67: 660–1. [DOI] [PubMed] [Google Scholar]
- 18.Petrie K, Crawford J, Baker ST, Dean K, Robinson J, Veness BGet al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta‐analysis. Lancet Psychiatry 2019; 6: 225–34. [DOI] [PubMed] [Google Scholar]
- 19.Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew‐Graham Cet al. Controlled interventions to reduce burnout in physicians: a systematic review and meta‐analysis. JAMA Intern Med 2017; 177: 195–205. [DOI] [PubMed] [Google Scholar]
- 20.Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta‐analysis. J Nerv Ment Dis 2014; 202: 353–9. [DOI] [PubMed] [Google Scholar]
- 21.Buddeberg‐Fischer B, Klaghofer R, Buddeberg C. Stress at work and well‐being in junior residents. Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie 2005; 51: 163–78. [DOI] [PubMed] [Google Scholar]
- 22.Mache S, Bernburg M, Vitzthum K, Groneberg DA, Klapp BF, Danzer G. Managing work–family conflict in the medical profession: working conditions and individual resources as related factors. BMJ Open 2015; 5: e006871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wainwright E, Fox F, Breffni T, Taylor G, O'Connor M. Coming back from the edge: a qualitative study of a professional support unit for junior doctors. BMC Med Educ 2017; 17: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milner A, Witt K, Spittal MJ, Bismark M, Graham M, LaMontagne AD. The relationship between working conditions and self‐rated health among medical doctors: evidence from seven waves of the medicine in Australia balancing employment and life (Mabel) survey. BMC Health Serv Res 2017; 17: 609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper CL, Rout U, Faragher B. Mental health, job satisfaction, and job stress among general practitioners. Br Med J 1989; 298: 366–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health 2008; 34: 169–78. [DOI] [PubMed] [Google Scholar]
- 27.Firth‐Cozens J. Individual and organizational predictors of depression in general practitioners. Br J Gen Pract 1998; 48: 1647–51. [PMC free article] [PubMed] [Google Scholar]
- 28.Fridner A, Belkić K, Minucci D, Pavan L, Marini M, Pingel Bet al. Work environment and recent suicidal thoughts among male university hospital physicians in Sweden and Italy: the health and organization among university hospital physicians in Europe (HOUPE) study. Gend Med 2011; 8: 269–79. [DOI] [PubMed] [Google Scholar]
- 29.Carter M, Thompson N, Crampton P, Morrow G, Burford B, Gray Cet al. Workplace bullying in the UKNHS: a questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ Open 2013; 3: e002628. [Google Scholar]
- 30.Sprigg CA, Niven K, Dawson J, Farley S, Armitage CJ. Witnessing workplace bullying and employee well‐being: a two‐wave field study. J Occup Health Psychol 2019; 24: 286–96. [DOI] [PubMed] [Google Scholar]
- 31.Netterstrøm B, Conrad N, Bech P, Fink P, Olsen O, Rugulies Ret al. The relation between work‐related psychosocial factors and the development of depression. Epidemiol Rev 2008; 30: 118–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Sociodemographic factors and association with CMD status (N = 3053).
Table S2. Sociodemographic factors associated with presence of suicidal ideation among JMO (N = 3048).
Table S3. Associations between a range of potentially stressful work‐related events and CMD in JMO, with unadjusted and adjusted estimates for effect size (OR; 95% CI), using logistic regression (N = 2948).
Table S4. Associations between a range of potentially stressful work‐related events and SI in JMO, with unadjusted and adjusted estimates for effect size (OR; 95% CI), using logistic regression (N = 2948).
Table S5. Final models obtained using backwards stepwise regression, stratified by gender, and listed in order of magnitude for each group, with adjusted estimates for effect size (OR; 95% CI) for CMD.
Table S6. Final adjusted models obtained using backwards stepwise regression, stratified by gender, and listed in order of magnitude for each group, with adjusted estimates for effect size (OR; 95% CI) for SI.


