Abstract
Background
Atopic dermatitis has been linked to increased risk of many comorbidities. However, the risks of certain comorbidities are still debated.
Objective
To better characterize the basic demographics, treatment patterns, and associations between atopic dermatitis and comorbidities and to further investigate the influence of severity on comorbidities.
Methods
We used a sample cohort of 999,992 people from the National Health Insurance Research Database of Taiwan to evaluate atopic dermatitis in the general population.
Results
A total of 12,780 patients with atopic dermatitis in 2010 were identified. The prevalence was 1.28%. The proportions of severe and moderate cases were 7.43% and 19.26%, respectively. The most commonly used systemic treatment was corticosteroids. Compared with the general population, atopic dermatitis patients showed increased risks of all 9 groups of comorbidities, including autoimmune disorders, atopic disorders, chronic urticaria, ocular disorders, metabolic disorders, hypertensive disorders, ischemic heart disorders, cerebrovascular disorders, and psychiatric disorders. The severity and persistence of atopic dermatitis were correlated with the development of certain comorbidities.
Limitations
Miscoding and misclassification might have occurred, and only patients with active disease were enrolled.
Conclusion
Patients with atopic dermatitis have higher risks of various comorbidities. Comprehensive monitoring and treatment plans are needed to better manage these patients.
Key words: atopic dermatitis, comorbidities, National Health Insurance Research Database, prevalence, severity, Taiwan, treatment
Abbreviation used: ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification
Graphical abstract
Capsule Summary.
-
•
Atopic dermatitis is a prevalent disease, at 1.28% in Taiwan.
-
•
One-fourth of atopic dermatitis patients have moderate to severe disease requiring systemic treatments, and such patients generally have increased risk of multiple medical comorbidities. The severity and persistence of atopic dermatitis is associated with the presence of certain comorbidities.
Introduction
Atopic dermatitis is an inflammatory skin disease characterized by recurrent pruritic skin eruptions that are typically located in certain areas but can extend to the whole surface of the body.1 The lifetime prevalence of atopic dermatitis is estimated to be approximately 10% to 20%.2 The disease may cause discomfort and impairment, leading to disability in daily activities, reduced performance in learning, decreased productivity in work, and worsened financial burdens both for individual patients and entire health care systems.3
In addition, atopic dermatitis has been shown to be associated with many other diseases, such as allergic diseases, autoimmune disorders, ocular abnormalities, psychiatric problems, and cardiovascular and cerebrovascular diseases.4, 5, 6, 7 These associations have even led some to categorize atopic dermatitis as a systemic inflammatory disorder.8 However, most of these associations have been identified mainly on the basis of case-control studies or small-scale cohort studies. Large-scale cohort studies of the comorbidities of atopic dermatitis are still scant, such that some of the previously reported associations remain controversial.5,6
To better characterize the disease burden of atopic dermatitis, we used a population-based database to evaluate the prevalence, severity, treatment patterns, and comorbidities of atopic dermatitis and to further investigate the influence of disease severity on comorbidities.
Materials and methods
Setting
The National Health Insurance program in Taiwan was put into effect in March 1995. It is primarily funded by payroll taxes, with additional subsidies from general government revenues, and covers 99.9% of the total population of Taiwan with a comprehensive benefits package (including outpatient and inpatient services, prescription drugs, preventive medicine, dental care services, and Chinese herbal remedies). Health care providers are reimbursed by the National Health Insurance program for their services. Patients are free to select the health care providers of their choice, although they are required to make co-payments for their health care services and drugs consumed.
Data sources
The data used in this study were obtained from the National Health Insurance Research Database, which was established by the National Health Research Institute in cooperation with the National Health Insurance Administration, with the aim of promoting research into current and emerging medical issues in Taiwan. The 2010 sample cohort files, which contain all the relevant medical records from 2003 to the end of 2013 for a sample cohort of 999,992 enrollees representative of the Taiwanese population in 2010, were used to identify the study cases and to construct the Taiwanese standard population in this study. Confidentiality assurances were addressed by abiding by the data regulations of the National Health Insurance Administration.
Study population
Patients were identified as having atopic dermatitis for each year from 2003 to 2013 if they fulfilled at least 1 of the following criteria: had at least 2 outpatient visits with a primary or secondary diagnosis of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of 691 (atopic dermatitis and related conditions), or had 1 outpatient visit with a primary or secondary ICD-9-CM code of 691 and at least 1 visit with a primary or secondary ICD-9-CM of 692.9 (contact dermatitis and other eczema, unspecified cause). We estimated the annual prevalence of atopic dermatitis from 2003 through 2010 but not for the years after 2010 because children born after that date were not included in this sample cohort.
Definition of severity and persistence of atopic dermatitis
To further investigate the severity of atopic dermatitis, we classified patients with the disease into mild, moderate, and severe cases based on their treatments according to the national treatment guidelines for atopic dermatitis.9 First, a patient with severe atopic dermatitis was defined as one who had received at least 3 prescriptions for systemic immunosuppressants (cyclosporine, azathioprine, methotrexate, and mycophenolate mofetil) or systemic corticosteroids, or at least 3 prescriptions for superpotent topical corticosteroids (ie, clobetasol) combined with at least 3 prescriptions for phototherapy in the year. Second, a patient with moderate atopic dermatitis was defined as one who had received at least 1 prescription for systemic corticosteroids, or at least 3 prescriptions for superpotent topical corticosteroids, or at least 1 prescription for phototherapy in the year. Third, patients who did not fulfill the above-mentioned criteria were defined as having mild cases.
In addition, the atopic dermatitis patients identified in 2010 were chosen as a sample cohort to evaluate the persistence of the disease; that is, the persistence of atopic dermatitis was determined according to the number of years in which a certain patient was identified as having atopic dermatitis during the investigation period (from 2003 to 2013). The patients with atopic dermatitis were separated into 3 categories: those who had the disease for only 1 year, those who had the disease for 2 to 5 years, and those who had the disease for greater than or equal to 6 years.
Definition of comorbidities
There were 9 groups of comorbidities that were assessed according to the previous literature,4, 5, 6, 7, 8,10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 and they were defined according to whether the given atopic dermatitis patient had at least 3 outpatient visit claims with principal or secondary diagnoses of the following diseases (ICD-9-CM code): autoimmune disorders, including systemic lupus erythematosus (710), rheumatoid arthritis (714), and ankylosing spondylitis (720); atopic disorders, including asthma (493) and allergic rhinitis (477); chronic urticaria (708.8 and 708.9); ocular disorders, including glaucoma (365), cataracts (366), and conjunctivitis (372); metabolic disorders, including diabetes mellitus (250) and disorders of lipid metabolism (272); hypertensive disorders, including essential hypertension (401) and hypertensive heart disease (402); ischemic heart disorders, including acute myocardial infarction (410), angina pectoris (413), and other forms of chronic ischemic heart disease (414); cerebrovascular disorders, including occlusion and stenosis of precerebral arteries (433) and occlusion of cerebral arteries (434); and psychiatric disorders, including episodic mood disorders (296), anxiety, dissociative and somatoform disorders (300), specific disorders of sleep of nonorganic origin (307.4), adjustment reaction (309), depressive disorder, not elsewhere classified (311), and attention-deficit/hyperactivity disorder (314.01).
Statistical analysis
Pearson χ2 tests were performed to examine differences in age, sex, and persistence among the atopic dermatitis patients with the 3 disease severity levels. The observed prevalence of the atopic dermatitis–related comorbidities was calculated. The standardized prevalence ratios (that is, the ratios of the observed to the expected atopic dermatitis–related comorbidities) were used to estimate the relative risk. The expected number of comorbid cases among the atopic dermatitis patients was calculated by multiplying the number of persons accumulated in each stratum of age and sex by the corresponding specific rate of the Taiwanese standard population; 95% confidence intervals of these ratios were calculated with the assumption that the observed numbers of comorbidity cases followed a Poisson distribution. All analyses were performed with SAS/Stat (version 9.3, SAS Institute, Inc, Cary, NC).
Results
Demographics, severity, and treatment patterns of atopic dermatitis in Taiwan
A total of 12,780 patients with atopic dermatitis in 2010 was identified. The overall prevalence of atopic dermatitis in 2010 was 1.28%, and the prevalence remained consistent during the whole investigation period (data not shown). With respect to age, children younger than 2 years had the highest prevalence (16.93%).
The proportions of severe and moderate cases of atopic dermatitis in 2010 were 7.43% and 19.26%, respectively, and these remained consistent during the entire investigation period (Table I). The proportion of moderate to severe cases in adults was higher than that in children. In addition, the sex distributions were significantly different among patients with different severity levels (P < .001). Among patients with severe atopic dermatitis, the number of male patients was greater than the number of female ones (Table I).
Table I.
Demographics of patients with atopic dermatitis in 2010
| Total |
Mild |
Moderate |
Severe |
P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| 12,780 | 9369 | 73.31 | 2462 | 19.26 | 949 | 7.43 | |||
| Age, mean ± SD, y | 25.11 ± 25.95 | 21.52 ± 25.34 | 33.04 ± 24.67 | 39.96 ± 25.26 | <.001 | ||||
| 0–9 | 5804 | 40.86 | 5042 | 49.49 | 604 | 19.13 | 158 | 12.01 | |
| 10–19 | 1302 | 7.50 | 833 | 7.16 | 351 | 8.61 | 118 | 7.90 | |
| 20–29 | 1073 | 8.40 | 646 | 6.90 | 311 | 12.63 | 116 | 12.22 | |
| 30–39 | 1031 | 8.07 | 622 | 6.64 | 297 | 12.06 | 112 | 11.80 | |
| 40–49 | 957 | 7.49 | 604 | 6.45 | 249 | 10.11 | 104 | 10.96 | |
| 50–59 | 923 | 7.22 | 577 | 6.16 | 239 | 9.71 | 107 | 11.28 | |
| 60–69 | 613 | 4.80 | 381 | 4.07 | 154 | 6.26 | 78 | 8.22 | |
| 70–79 | 624 | 4.88 | 360 | 3.84 | 163 | 6.62 | 101 | 10.64 | |
| ≥80 | 453 | 3.54 | 304 | 3.24 | 94 | 3.82 | 55 | 5.80 | |
| Sex | <.001 | ||||||||
| Women | 6798 | 53.19 | 5024 | 53.62 | 1339 | 54.39 | 435 | 45.84 | |
| Men | 5982 | 46.81 | 4345 | 46.38 | 1123 | 45.61 | 514 | 54.16 | |
| Persistence of AD, y | <.001 | ||||||||
| 1 | 5093 | 39.85 | 3910 | 41.73 | 939 | 38.14 | 244 | 25.71 | |
| 2–5 | 6609 | 51.71 | 4867 | 51.95 | 1251 | 50.81 | 491 | 51.74 | |
| ≥6 | 1078 | 8.44 | 592 | 6.32 | 272 | 11.05 | 214 | 22.55 | |
AD, Atopic dermatitis, SD, standard deviation.
Among the systemic treatments, systemic corticosteroids had been prescribed for 22.43% of all the atopic dermatitis patients in 2010, and were more commonly used for adult patients than for children (31.70% vs 14.48%). Phototherapy was used for 0.26% of the atopic dermatitis patients, including 0.51% of the adults and 0.04% of the children. Among the immunosuppressants other than corticosteroids, azathioprine (0.17%) was the most frequently prescribed agent, followed by methotrexate (0.13%) and cyclosporine (0.05%). The rates at which these systemic treatments for atopic dermatitis were used also remained consistent during the investigation period (data not shown).
Comorbidities in patients with atopic dermatitis
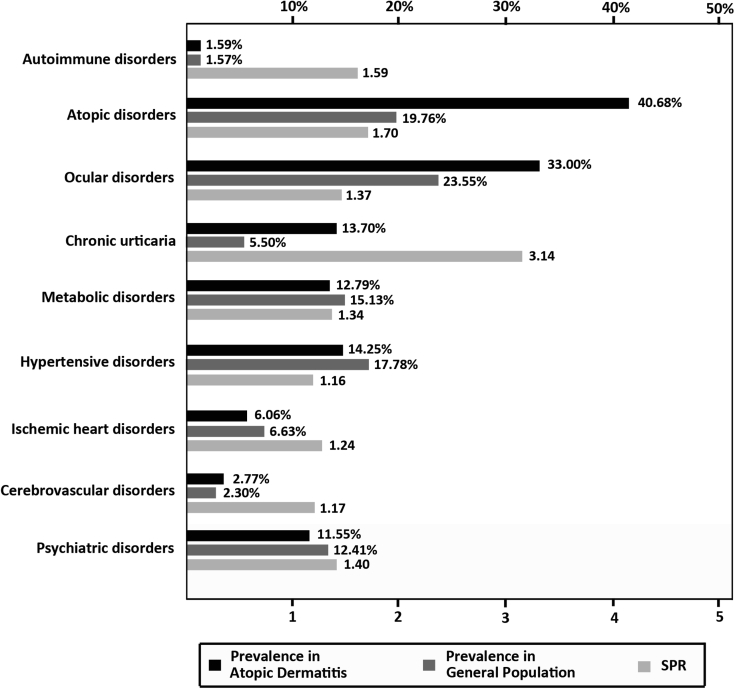
We examined the period prevalence of 27 comorbid diseases in the atopic dermatitis patients, grouping them into 9 disease categories. The most commonly encountered comorbidities were atopic disorders, followed by ocular disorders, hypertensive disorders, chronic urticaria, and metabolic disorders (Fig 1). In comparison with the standard population, the atopic dermatitis patients showed increased risks for all 9 of the categories of comorbidities. Among these comorbidities, chronic urticaria showed the highest standardized prevalence ratio, followed by atopic disorders and autoimmune disorders (Fig 1).
Fig 1.
Prevalence and standardized prevalence ratios of multiple comorbidities in patients with atopic dermatitis. Among these associated diseases in patients with atopic dermatitis, atopic disorders showed the highest prevalence, followed by ocular disorders and hypertensive disorders. In regard to standardized prevalence ratios, chronic urticaria showed the highest ones, followed by atopic disorders and autoimmune disorders. SPR, Standardized prevalence ratio.
Correlations of comorbidities with the severity or persistence of atopic dermatitis
The prevalence of autoimmune disorders, atopic disorders, ocular disorders, chronic urticaria, ischemic heart disorders, and cerebrovascular disorders was higher in patients with higher severities of atopic dermatitis (Table II).
Table II.
Prevalence of comorbidities among patients with different severities of atopic dermatitis
| Total |
Mild |
Moderate |
Severe |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 12,780) |
(N = 9369) |
(N = 2462) |
(N = 949) |
|||||||||
| N | SPR | 95% CI | N | SPR | 95% CI | N | SPR | 95% CI | N | SPR | 95% CI | |
| Autoimmune disorders | ||||||||||||
| All | 203 | 1.59 | (1.57–1.61) | 109 | 1.34 | (1.32–1.36) | 46 | 1.46 | (1.44–1.48) | 48 | 3.31 | (3.28–3.34) |
| Rheumatoid arthritis | 92 | 1.46 | (1.43–1.49) | 53 | 1.32 | (1.30–1.35) | 22 | 1.37 | (1.34–1.39) | 17 | 2.53 | (2.50–2.57) |
| Systemic lupus erythematosus | 39 | 2.43 | (2.36–2.50) | 11 | 0.92 | (0.88–0.97) | 12 | 3.03 | (2.96–3.11) | 16 | 10.36 | (10.21–10.51) |
| Ankylosing spondylitis | 89 | 1.64 | (1.61–1.67) | 53 | 1.54 | (1.52–1.57) | 20 | 1.54 | (1.51–1.57) | 16 | 2.13 | (2.10–2.17) |
| Atopic disorders | ||||||||||||
| All | 5199 | 1.70 | (1.69–1.70) | 3788 | 1.67 | (1.67–1.68) | 989 | 1.78 | (1.77–1.78) | 422 | 2.05 | (2.04–2.05) |
| Asthma | 2538 | 1.99 | (1.98–2.00) | 1792 | 1.82 | (1.81–1.83) | 497 | 2.31 | (2.30–2.32) | 249 | 3.31 | (3.30–3.32) |
| Allergic rhinitis | 4498 | 1.72 | (1.71–1.73) | 3249 | 1.69 | (1.68–1.70) | 872 | 1.82 | (1.81–1.83) | 377 | 2.15 | (2.14–2.16) |
| Ocular disorders | ||||||||||||
| All | 4218 | 1.37 | (1.37–1.37) | 2930 | 1.35 | (1.35–1.36) | 905 | 1.44 | (1.43–1.44) | 383 | 1.48 | (1.48–1.49) |
| Conjunctivitis | 4071 | 1.39 | (1.38–1.39) | 2846 | 1.38 | (1.37–1.38) | 867 | 1.45 | (1.45–1.46) | 358 | 1.49 | (1.48–1.49) |
| Cataracts | 857 | 1.27 | (1.26–1.27) | 518 | 1.23 | (1.22–1.24) | 208 | 1.25 | (1.24–1.26) | 131 | 1.49 | (1.49–1.50) |
| Glaucoma | 238 | 1.69 | (1.67–1.71) | 143 | 1.62 | (1.60–1.64) | 56 | 1.60 | (1.58–1.62) | 39 | 2.39 | (2.36–2.41) |
| Chronic urticaria | 1751 | 3.14 | (3.12–3.15) | 975 | 2.53 | (2.52–2.55) | 507 | 3.87 | (3.86–3.89) | 269 | 5.10 | (5.09–5.12) |
| Metabolic disorders | ||||||||||||
| All | 1634 | 1.34 | (1.33–1.34) | 1017 | 1.34 | (1.33–1.34) | 422 | 1.37 | (1.36–1.38) | 195 | 1.27 | (1.26–1.27) |
| Diabetes mellitus | 942 | 1.46 | (1.45–1.47) | 578 | 1.45 | (1.44–1.46) | 243 | 1.48 | (1.47–1.48) | 121 | 1.47 | (1.47–1.48) |
| Lipid disorders | 1289 | 1.29 | (1.28–1.30) | 794 | 1.28 | (1.27–1.29) | 335 | 1.34 | (1.33–1.34) | 160 | 1.27 | (1.26–1.27) |
| Hypertensive disorders | ||||||||||||
| All | 1821 | 1.16 | (1.16–1.17) | 1121 | 1.15 | (1.15–1.16) | 470 | 1.22 | (1.22–1.23) | 230 | 1.12 | (1.12–1.13) |
| Essential hypertension | 1695 | 1.17 | (1.17–1.18) | 1044 | 1.16 | (1.16–1.17) | 435 | 1.23 | (1.23–1.24) | 216 | 1.14 | (1.13–1.14) |
| Hypertensive heart disease | 761 | 1.24 | (1.23–1.25) | 465 | 1.20 | (1.19–1.21) | 197 | 1.32 | (1.31–1.33) | 99 | 1.28 | (1.27–1.29) |
| Ischemic heart diseases | ||||||||||||
| All | 774 | 1.24 | (1.23–1.25) | 466 | 1.19 | (1.18–1.19) | 195 | 1.31 | (1.30–1.32) | 113 | 1.36 | (1.35–1.37) |
| Acute myocardial infarction | 123 | 1.33 | (1.31–1.35) | 70 | 1.21 | (1.19–1.23) | 28 | 1.34 | (1.32–1.37) | 25 | 1.77 | (1.75–1.80) |
| Angina pectoris | 246 | 1.28 | (1.26–1.30) | 147 | 1.19 | (1.18–1.21) | 60 | 1.32 | (1.30–1.33) | 39 | 1.54 | (1.52–1.56) |
| Other forms of chronic ischemic heart disease | 612 | 1.25 | (1.24–1.26) | 369 | 1.22 | (1.21–1.23) | 156 | 1.31 | (1.30–1.32) | 87 | 1.35 | (1.34–1.36) |
| Cerebrovascular disorders | ||||||||||||
| All | 354 | 1.17 | (1.16–1.18) | 219 | 1.15 | (1.13–1.16) | 87 | 1.23 | (1.21–1.24) | 48 | 1.34 | (1.33–1.35) |
| Occlusion of cerebral arteries | 286 | 1.09 | (1.07–1.10) | 178 | 1.10 | (1.08–1.11) | 67 | 1.05 | (1.03–1.06) | 41 | 1.30 | (1.29–1.32) |
| Occlusion and stenosis of precerebral arteries | 104 | 1.82 | (1.78–1.85) | 56 | 1.55 | (1.51–1.58) | 32 | 2.36 | (2.32–2.40) | 16 | 2.21 | (2.17–2.25) |
| Psychiatric disorders | ||||||||||||
| All | 1476 | 1.40 | (1.40–1.41) | 907 | 1.35 | (1.36–1.36) | 392 | 1.54 | (1.53–1.55) | 177 | 1.51 | (1.50–1.52) |
| Psychiatric disorders, including episodic mood disorders | 266 | 1.72 | (1.70–1.74) | 168 | 1.71 | (1.69–1.72) | 66 | 1.59 | (1.57–1.60) | 32 | 1.93 | (1.91–1.95) |
| Anxiety, dissociative, and somatoform disorders | 1244 | 1.44 | (1.44–1.45) | 762 | 1.39 | (1.38–1.39) | 345 | 1.64 | (1.64–1.65) | 137 | 1.37 | (1.37–1.38) |
| Nonorganic sleep disorder | 383 | 1.53 | (1.52–1.54) | 221 | 1.38 | (1.36–1.39) | 116 | 1.87 | (1.86–1.89) | 46 | 1.47 | (1.46–1.49) |
| Adjustment reaction | 83 | 1.48 | (1.45–1.51) | 54 | 1.53 | (1.50–1.56) | 16 | 1.13 | (1.11–1.16) | 13 | 2.11 | (2.07–2.14) |
| Depressive disorder | 167 | 1.60 | (1.58–1.63) | 106 | 1.61 | (1.58–1.63) | 43 | 1.70 | (1.68–1.72) | 18 | 1.52 | (1.50–1.54) |
| Attention-deficit/hyperactivity disorder | 272 | 1.11 | (1.09–1.14) | 194 | 0.96 | (0.93–0.98) | 55 | 1.67 | (1.64–1.70) | 23 | 2.18 | (2.14–2.21) |
CI, Confidence interval; SPR, standardized prevalence ratio.
The distributions of persistence were significantly different among the different severities of atopic dermatitis (Table I; P < .001). Patients with severe disease had a higher proportion than those whose atopic dermatitis persisted for more than 5 years. Furthermore, the prevalence of autoimmune disorders, atopic disorders, ocular disorders, chronic urticaria, metabolic disorders, and ischemic heart disorders was positively correlated to the persistence of atopic dermatitis (Table III).
Table III.
Prevalence of comorbidities among patients with different persistent periods of atopic dermatitis
| Total |
1 year |
2–5 years |
≥6 years |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 12,780) |
(N = 5039) |
(N = 6609) |
(N = 1078) |
|||||||||
| N | SPR | 95% CI | N | SPR | 95% CI | N | SPR | 95% CI | N | SPR | 95% CI | |
| Autoimmune disorders | ||||||||||||
| All | 203 | 1.59 | (1.57–1.61) | 69 | 1.39 | (1.37–1.41) | 104 | 1.66 | (1.64–1.68) | 30 | 2.21 | (2.19–2.23) |
| Rheumatoid arthritis | 92 | 1.46 | (1.43–1.49) | 35 | 1.44 | (1.41–1.46) | 45 | 1.36 | (1.33–1.39) | 12 | 2.17 | (2.13–2.20) |
| Systemic lupus erythematosus | 39 | 2.43 | (2.36–2.50) | 11 | 1.40 | (1.35–1.46) | 21 | 3.29 | (3.21–3.38) | 7 | 3.44 | (3.36–3.52) |
| Ankylosing spondylitis | 89 | 1.64 | (1.61–1.67) | 28 | 1.38 | (1.35–1.40) | 46 | 1.65 | (1.62–1.68) | 15 | 2.57 | (2.54–2.67) |
| Atopic disorders | ||||||||||||
| All | 5199 | 1.70 | (1.69–1.70) | 1647 | 1.43 | (1.43–1.44) | 2982 | 1.84 | (1.83–1.84) | 570 | 2.16 | (2.16–2.17) |
| Asthma | 2538 | 1.99 | (1.98–2.00) | 742 | 1.60 | (1.59–1.61) | 1502 | 2.17 | (2.16–2.18) | 294 | 2.91 | (2.90–2.93) |
| Allergic rhinitis | 4498 | 1.72 | (1.71–1.73) | 1374 | 1.43 | (1.42–1.43) | 2611 | 1.88 | (1.87–1.88) | 513 | 2.24 | (2.23–2.25) |
| Ocular disorders | ||||||||||||
| All | 4218 | 1.37 | (1.37–1.37) | 1340 | 1.19 | (1.18–1.19) | 2371 | 1.47 | (1.46–1.47) | 507 | 1.67 | (1.67–1.68) |
| Conjunctivitis | 4071 | 1.39 | (1.38–1.39) | 1287 | 1.19 | (1.19–1.20) | 2288 | 1.49 | (1.48–1.49) | 496 | 1.73 | (1.72–1.73) |
| Cataracts | 857 | 1.27 | (1.26–1.27) | 262 | 1.13 | (1.12–1.14) | 495 | 1.36 | (1.36–1.37) | 100 | 1.25 | (1.24–1.26) |
| Glaucoma | 238 | 1.69 | (1.67–1.71) | 75 | 1.46 | (1.44–1.48) | 133 | 1.80 | (1.78–1.82) | 30 | 1.92 | (1.90–1.95) |
| Chronic urticaria | 1751 | 3.14 | (3.12–3.15) | 539 | 2.51 | (2.49–2.52) | 936 | 3.32 | (3.30–3.33) | 276 | 4.82 | (4.80–4.84) |
| Metabolic disorders | ||||||||||||
| All | 1634 | 1.34 | (1.33–1.34) | 578 | 1.28 | (1.28–1.29) | 847 | 1.36 | (1.36–1.37) | 209 | 1.50 | (1.50–1.51) |
| Diabetes mellitus | 942 | 1.46 | (1.45–1.47) | 324 | 1.38 | (1.37–1.39) | 491 | 1.48 | (1.47–1.49) | 127 | 1.71 | (1.70–1.72) |
| Lipid disorders | 1289 | 1.29 | (1.28–1.30) | 464 | 1.24 | (1.23–1.25) | 662 | 1.30 | (1.29–1.31) | 163 | 1.42 | (1.42–1.43) |
| Hypertensive disorders | ||||||||||||
| All | 1821 | 1.16 | (1.16–1.17) | 617 | 1.11 | (1.10–1.11) | 987 | 1.21 | (1.20–1.21) | 217 | 1.19 | (1.19–1.20) |
| Essential hypertension | 1695 | 1.17 | (1.17–1.18) | 571 | 1.11 | (1.10–1.11) | 929 | 1.24 | (1.23–1.25) | 195 | 1.15 | (1.15–1.16) |
| Hypertensive heart disease | 761 | 1.24 | (1.23–1.25) | 248 | 1.15 | (1.15–1.16) | 420 | 1.27 | (1.26–1.28) | 93 | 1.37 | (1.36–1.38) |
| Ischemic heart diseases | ||||||||||||
| All | 774 | 1.24 | (1.23–1.25) | 244 | 1.11 | (1.10–1.12) | 427 | 1.29 | (1.29–1.30) | 103 | 1.44 | (1.44–1.45) |
| Acute myocardial infarction | 123 | 1.33 | (1.31–1.35) | 41 | 1.32 | (1.30–1.35) | 65 | 1.23 | (1.21–1.26) | 17 | 1.45 | (1.43–1.48) |
| Angina pectoris | 246 | 1.28 | (1.26–1.30) | 80 | 1.19 | (1.17–1.20) | 131 | 1.25 | (1.23–1.26) | 35 | 1.75 | (1.73–1.76) |
| Other forms of chronic ischemic heart disease | 612 | 1.25 | (1.24–1.26) | 183 | 1.05 | (1.05–1.06) | 349 | 1.37 | (1.36–1.38) | 80 | 1.42 | (1.41–1.43) |
| Cerebrovascular disorders | ||||||||||||
| All | 354 | 1.17 | (1.16–1.18) | 121 | 1.26 | (1.24–1.27) | 182 | 2.02 | (2.00–2.04) | 36 | 1.82 | (1.80–1.84) |
| Occlusion of cerebral arteries | 286 | 1.09 | (1.07–1.10) | 105 | 1.18 | (1.17–1.19) | 150 | 1.08 | (1.07–1.10) | 31 | 1.03 | (1.01–1.04) |
| Occlusion and stenosis of precerebral arteries | 104 | 1.82 | (1.78–1.85) | 38 | 2.09 | (2.05–2.13) | 53 | 1.73 | (1.70–1.77) | 13 | 1.61 | (1.58–1.65) |
| Psychiatric disorders | ||||||||||||
| All | 1476 | 1.40 | (1.40–1.41) | 623 | 1.31 | (1.30–1.31) | 910 | 1.49 | (1.49–1.50) | 179 | 1.40 | (1.39–1.41) |
| Psychiatric disorders, including episodic mood disorders | 266 | 1.72 | (1.70–1.74) | 101 | 1.51 | (1.50–1.53) | 138 | 1.90 | (1.88–1.92) | 27 | 1.63 | (1.62–1.65) |
| Anxiety, dissociative and somatoform disorders | 1244 | 1.44 | (1.44–1.45) | 471 | 1.37 | (1.36–138) | 642 | 1.52 | (1.51–1.53) | 131 | 1.41 | (1.41–1.42) |
| Nonorganic sleep disorder | 383 | 1.53 | (1.52–1.54) | 139 | 1.35 | (1.34–1.36) | 211 | 1.78 | (1.77–1.79) | 33 | 1.14 | (1.12–1.15) |
| Adjustment reaction | 83 | 1.48 | (1.45–1.51) | 29 | 1.34 | (1.31–1.36) | 46 | 1.61 | (1.58–1.64) | 8 | 1.35 | (1.32–1.37) |
| Depressive disorder | 167 | 1.60 | (1.58–1.63) | 57 | 1.34 | (1.32–1.36) | 90 | 1.80 | (1.77–1.82) | 20 | 1.87 | (1.85–1.90) |
| Attention-deficit/hyperactivity disorder | 272 | 1.11 | (1.09–1.14) | 77 | 0.83 | (0.81–0.85) | 170 | 1.27 | (1.25–1.30) | 25 | 1.49 | (1.46–1.52) |
CI, Confidence interval; SPR, standardized prevalence ratio.
Discussion
In the present study, we used the National Health Insurance Research Database of Taiwan to demonstrate that the prevalence of atopic dermatitis and the proportions of patients with different severities of the disease were consistent. However, the prevalence of atopic dermatitis reported in this study may represent only patients with active diseases who sought medical treatment in certain years.
Many previous studies have focused on the comorbidities of patients with atopic dermatitis. Associations between atopic dermatitis and certain comorbidities, such as autoimmune disorders,5, 6, 7, 8,10 atopic disorders,5, 6, 7, 8 and ocular disorders,11,12 have been consistently demonstrated, whereas the associations between atopic dermatitis and certain other comorbidities, such as hypertension, metabolic disorders, cardiovascular disorders, and stroke, are still controversial.5, 6, 7, 8 Consistent with our results, Silverberg et al13 showed in a recent, cross-sectional, US, population-based study that atopic dermatitis patients had higher odds of having asthma, anxiety and depression, autoimmune disease, diabetes, high blood pressure, and heart disease than healthy controls. Silverberg14 also found that adult atopic dermatitis was associated with cardiovascular disease and stroke in 3 population-based studies. However, Egeberg et al15 reported no increased risks of diabetes mellitus and myocardial infarction in Danish adult atopic dermatitis patients compared with healthy controls. They also found that an increased risk of hypertension was observed only in patients with severe atopic dermatitis.
The discrepancies among such past studies might have resulted from the different designs of the studies and the ethnic differences in their study populations. One recent meta-analysis focusing on atopic dermatitis and major cardiovascular outcomes showed that the results from cross-sectional studies were heterogeneous, whereas those from cohort studies were more consistent.16 The authors demonstrated that in cohort studies, atopic dermatitis was associated with increased risks of myocardial infarction, stroke, angina, and heart failure, whereas in cross-sectional studies these associations were absent. This indicates that study designs can indeed influence the outcome measurements. Because comorbidities and atopic dermatitis may not develop simultaneously, a cohort study might be more accurate in investigating the associations between various comorbidities and atopic dermatitis. In addition, ethnic differences may also influence the results of different studies. Consistent with our results, for example, Su et al17 and Sung et al18 independently reported an increased risk of stroke in patients with atopic dermatitis in Taiwan. However, this association was insignificant in a German population.19
One important aspect of this study was that we used 2 characteristics—namely, treatment pattern–based severity stratification and the persistence of the disease—to assess the association of atopic dermatitis severity with the development of comorbidities. Because the disease severity of atopic dermatitis may fluctuate over time, we believed that using these 2 characteristics would more accurately reflect the real situation of the association between atopic dermatitis severity and the development of comorbidities. The prevalence of autoimmune disorders, atopic disorders, chronic urticaria, ocular disorders, and ischemic heart disorders showed consistently positive correlations with atopic dermatitis severity according to both characteristics. Meanwhile, the prevalence of cerebrovascular disorders and metabolic disorders showed positive correlations with treatment-determined severity and persistence, respectively. On the other hand, the prevalence of other disorders did not change significantly when being assessed according to either of the 2 characteristics. These results indicate that the underlying mechanisms of the associations between these comorbidities and atopic dermatitis might be different. Autoimmune disorders, atopic disorders, and chronic urticaria may have shared or similar immune dysregulation with atopic dermatitis because this could account for the observed positive correlations and higher values of standardized prevalence ratios. However, ocular disorders may show immune dysregulation similar to that of atopic dermatitis or may result from the adverse effects of atopic dermatitis treatment because either of these alternatives could account for the positive correlations. However, the development of metabolic disorders, hypertensive disorders, ischemic heart disorders, and cerebrovascular disorders may be related either to chronic systemic inflammation resulting from atopic dermatitis or other inflammatory diseases, or to lifestyle factors observed in atopic dermatitis patients.20 The influencing factors involved in the development of these comorbidities may be complex and are related to the aforementioned factors. Therefore, the effect of atopic dermatitis severity or persistence on the prevalence of these comorbidities, with the exception of ischemic heart disorders, may not be so obvious. Although the prevalence of ischemic heart disorders showed positive correlations in terms of both of the above-mentioned characteristics, the differences among the groups were not as large as those observed for autoimmune disorders, atopic disorders, and chronic urticaria. As such, the results still indicate a possibly different relationship with atopic dermatitis between ischemic heart disorders and those 3 disorders. The exact mechanisms underlying the associations between various comorbidities and atopic dermatitis require further investigation.
The major limitation of this study consists in the potential risks of miscoding and misclassification, which are inherent weaknesses of database research. To reduce these risks, we used more stringent criteria to define patients with atopic dermatitis and comorbidities. As a result, the number of atopic dermatitis patients identified in this study might be an underestimation of the true number of such patients in the investigated population. Only patients with more active disease requiring medical treatment were recruited. This limitation means that this study mainly focused on the data of patients with active disease.
In conclusion, we found that the prevalence of various comorbidities was higher among atopic dermatitis patients than among the general population, and that the severity and persistence of atopic dermatitis may be associated with the prevalence of certain comorbidities.
Footnotes
Drs Tang and Chu contributed equally to this article.
Funding sources: Supported by Sanofi Taiwan Co Ltd.
Conflicts of interest: Dr Cho has received lecture fees from Sanofi Taiwan Co Ltd. Dr Chu is an advisory board member of Sanofi Taiwan Co Ltd and has received honoraria from it. Drs Chan and Tang and Author Hsieh have no conflicts of interest to declare.
The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
This clinical trial was approved by the National Taiwan University Hospital Research Ethics Committee (201802007RINA).
Contributor Information
Chao-Hsiun Tang, Email: chtang@tmu.edu.tw.
Chia-Yu Chu, Email: chiayu@ntu.edu.tw.
References
- 1.Cho Y.T., Chu C.Y. Advances in systemic treatment for adults with moderate-to-severe atopic dermatitis. Dermatol Sin. 2019;37:3–11. [Google Scholar]
- 2.Weidinger S., Novak N. Atopic dermatitis. Lancet. 2016;387:1109–1122. doi: 10.1016/S0140-6736(15)00149-X. [DOI] [PubMed] [Google Scholar]
- 3.Simpson E.L., Guttman-Yassky E., Margolis D.J. Association of inadequately controlled disease and disease severity with patient-reported disease burden in adults with atopic dermatitis. JAMA Dermatol. 2018;154:903–912. doi: 10.1001/jamadermatol.2018.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silverwood R.J., Forbes H.J., Abuabara K. Severe and predominantly active atopic eczema in adulthood and long term risk of cardiovascular disease: population based cohort study. BMJ. 2018;361:k1786. doi: 10.1136/bmj.k1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paller A.S., Jaworski J.C., Simpson E.L. Major comorbidities of atopic dermatitis: beyond allergic disorders. Am J Clin Dermatol. 2018;19:821–838. doi: 10.1007/s40257-018-0383-4. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira C., Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29:250–258. doi: 10.1684/ejd.2019.3557. [DOI] [PubMed] [Google Scholar]
- 7.Silverberg J.I. Comorbidities and the impact of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;123(2):144–151. doi: 10.1016/j.anai.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 8.Brunner P.M., Silverberg J.I., Guttman-Yassky E. Increasing comorbidities suggest that atopic dermatitis is a systemic disorder. J Invest Dermatol. 2017;137:18–25. doi: 10.1016/j.jid.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 9.Chu C.Y., Lee C.H., Shih I.H. Taiwanese Dermatological Association consensus for the management of atopic dermatitis. Dermatol Sin. 2015;33:220–230. doi: 10.1016/j.jfma.2020.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Narla S., Silverberg J.I. Association between atopic dermatitis and autoimmune disorders in US adults and children: a cross-sectional study. J Am Acad Dermatol. 2019;80:382–389. doi: 10.1016/j.jaad.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Thyssen J.P., Toft P.B., Halling-Overgaard A., Gislason G.H., Skov L., Egebergg A. Incidence, prevalence, and risk of selected ocular disease in adults with atopic dermatitis. J Am Acad Dermatol. 2017;77:280–286. doi: 10.1016/j.jaad.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Govind K., Whang K., Khanna R., Scott A.W., Kwatra S.G. Atopic dermatitis is associated with increased prevalence of multiple ocular comorbidities. J Allergy Clin Immunol Pract. 2019;7:298–299. doi: 10.1016/j.jaip.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Silverberg J.I., Gelfand J.M., Margolis D.J. Association of atopic dermatitis with allergic, autoimmune, and cardiovascular comorbidities in US adults. Ann Allergy Asthma Immunol. 2018;121:604–612. doi: 10.1016/j.anai.2018.07.042. [DOI] [PubMed] [Google Scholar]
- 14.Silverberg J.I. Association between adult atopic dermatitis, cardiovascular disease, and increased heart attacks in three population-based studies. Allergy. 2015;70:1300–1308. doi: 10.1111/all.12685. [DOI] [PubMed] [Google Scholar]
- 15.Egeberg A., Andersen Y.M.F., Gislason G.H., Skov L., Thyssen J.P. Prevalence of comorbidities and associated risk factors in adults with atopic dermatitis. Allergy. 2017;72:783–791. doi: 10.1111/all.13085. [DOI] [PubMed] [Google Scholar]
- 16.Ascott A., Mulick A., Yu A.M. Atopic dermatitis and major cardiovascular outcomes: a systematic review and meta-analysis of population-based studies. J Allergy Clin Immunol. 2019;143:1821–1829. doi: 10.1016/j.jaci.2018.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su V.Y., Chen T.J., Yeh C.M. Atopic dermatitis and risk of ischemic stroke: a nationwide population-based study. Ann Med. 2014;46:84–89. doi: 10.3109/07853890.2013.870018. [DOI] [PubMed] [Google Scholar]
- 18.Sung Y.F., Lin C.C., Yin J.H. Increased risk of stroke in patients with atopic dermatitis: a population-based, longitudinal study in Taiwan. J Med Sci. 2017;37:12–18. [Google Scholar]
- 19.Standl M., Tesch F., Baurecht H. Association of atopic dermatitis with cardiovascular risk factors and diseases. J Invest Dermatol. 2017;137(5):1074–1081. doi: 10.1016/j.jid.2016.11.031. [DOI] [PubMed] [Google Scholar]
- 20.Andersen Y.M.F., Egeberg A., Gislason G.H., Hansen P.R., Skov L., Thyssen J.P. Risk of myocardial infarction, ischemic stroke, and cardiovascular death in patients with atopic dermatitis. J Allergy Clin Immunol. 2016;138:310–312. doi: 10.1016/j.jaci.2016.01.015. [DOI] [PubMed] [Google Scholar]