Abstract
Introduction
Numerous population-based studies have focused on the global prevalence of atopic dermatitis (AD), but there are few studies on the global trends of the burden associated with AD.
Methods
We analyzed the global AD trends in 2017 in 195 countries worldwide using the Global Burden of Disease (GBD) Study database, including prevalence rates, age and sex patterns, and AD burden, using disability-adjusted life years (DALYs). Age-standardized DALYs were also compared to the sociodemographic index values of all the countries in 2017.
Results
The age-specific DALYs in 2017 showed a right-skewed distribution, with the highest DALYs between 1 and 5 years of age. Females had a higher burden of AD throughout all age groups and geographic regions. The GBD super region with the greatest burden of DALYs caused by AD was high income (178.63 DALYs per 100,000 males, 231.8 for females), and the country with the highest DALYs was Sweden (326.91). The GBD super region with the lowest age-standardized DALY burden caused by AD was south Asia (84.51 DALYs per 100,000 males, 100.54 for females).
Conclusion
There is a large GBD caused by AD. The observed burden is the greatest in resource-rich countries, females, and young children.
Key words: age-standardized prevalence rates, atopic dermatitis, burden, disability-adjusted life years (DALYs), Global Burden of Disease Study (GBD) database, global medicine, health care disparities, sociodemographic index (SDI)
Abbreviations used: AD, atopic dermatitis; DALY, disability-adjusted life year; GBD, global burden of disease; SDI, sociodemographic index
Capsule Summary.
-
•
Atopic dermatitis is the leading contributor to skin-related disability. This article demonstrates these trends on a global scale.
-
•
The burden of atopic dermatitis is the highest in children, women, and resource-rich countries. Redirection of resources may help reduce the global burden of this important disease.
Introduction
Atopic dermatitis (AD) is a common, chronically relapsing inflammatory skin disease that affects up to 2.4% of the population worldwide.1,2 The prevalence varies substantially among different countries.3 For example, the prevalence of adult AD was 4.9% in the United States and 2.1% in Japan.4 The prevalence of AD in children is as high as 20% in some countries, like Sweden.3 Although AD may sometimes be perceived as relatively benign, children with AD present with decreased quality of life, similar to other serious chronic disorders, such as cystic fibrosis and renal disease.5 AD can have serious detrimental effects on patients and families, impacting the social, academic, occupational, and financial aspects of their lives.6
One measure of AD disease morbidity is through disability-adjusted life years (DALYs), measured as the years of life lost due to premature mortality plus the years lost due to disability or its consequences.7 Additionally, sociodemographic index (SDI) is a measurement developed to identify where countries or other geographic areas are in their aspects of development. SDI is a composite average of income per capita, average educational attainment, and fertility rate, which is expressed on a scale of 0 to 1.8 Both DALYs and SDI have been referenced in the literature to aid in global health decision-making and bring increasing attention to various diseases worldwide.
Compared to other common dermatoses, AD ranked as the third most prevalent dermatologic condition (2.79%) but was the greatest contributor to the DALYs of skin dermatoses (0.36%) in 2017.9, 10, 11 Although the global prevalence actually decreased from 3.01% in 1990 to 2.79% in 2017, the global DALYs due to AD increased from 0.27% in 1990 to 0.36% in 2017.12 However, studies have shown increasing prevalence in certain countries, especially in developing countries, such as Chile, Kenya, and Algeria.3,13 In addition to the association with atopic conditions, like allergies and asthma, AD is related to other diseases, such as obesity, cardiovascular disease, and psychologic diseases, including anxiety and depression.14,15 This suggests that AD may be considered a chronic systemic disorder, with significant physical and psychosocial impairments.16,17
This observational study serves to show multiple global AD trends in 2017 in 195 countries worldwide using the global burden of disease (GBD) database.12 We assess AD age and sex patterns and disease burden using DALYs and compare the DALYs to SDI across all the countries measured by GBD. To our knowledge, a global analysis of AD has not yet been done using the GBD study database. We aim to contribute to the ongoing research required to adequately understand and address the global trends and prevalence of AD.
Methods
Study design
We provide an ecologic analysis to compare DALYs to SDI across the globe using the 2017 GBD database.
Data source
Our data were obtained from the publicly available GBD datasets from 2017. The GBD datasets provide data to compare the impact of diseases, injuries, and risk factors across age groups, sexes, countries, and regions from 1990 to the present day for over 350 diseases in 195 countries.18 The GBD provides up-to-date data obtained through multiple sources, including, but not limited to, health facility data, censuses, surveys, clinical trials, demographic surveillance, disease registries, and publications.19 The GBD project is led by the Institute for Health Metrics and Evaluation at the University of Washington and collaborates with over 145 countries and 3600 researchers worldwide.18 An in-depth protocol is available from the Institute for Health Metrics and Evaluation on how the data are obtained, incorporated, calculated, and published in the GBD study.19
Statistical analysis
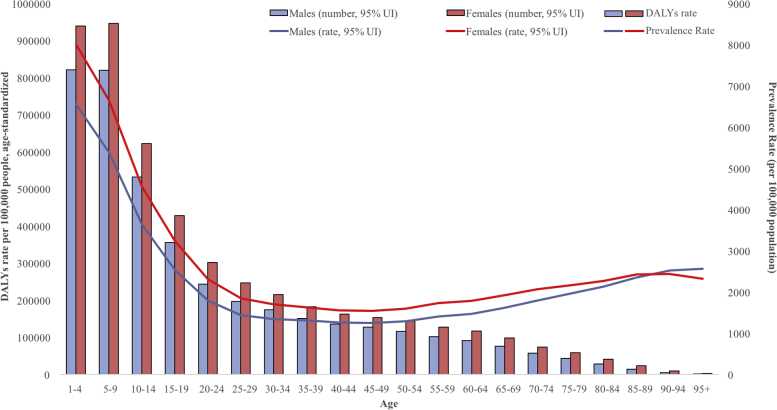
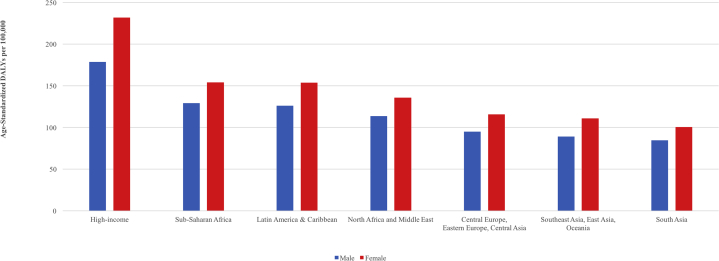
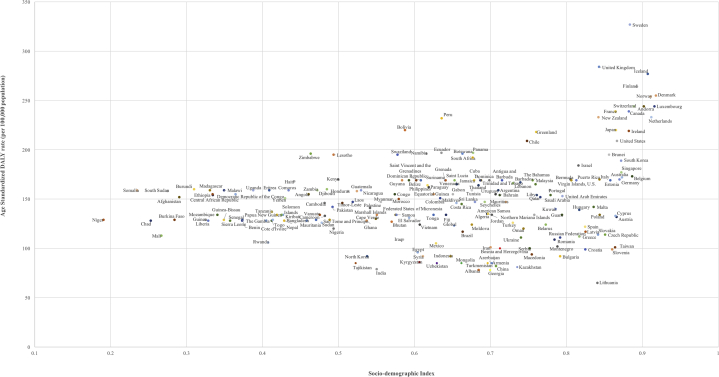
We provided age patterns by sex and the total number of DALYs caused by AD and age-specific DALY rates due to AD on a global level and by GBD super region in 2017 (Figs 1 and 2). Seven super regions were created by GBD based on geographic location and country gross domestic product. The age-standardized AD DALYs per 100,000 people were also compared to the absolute SDI values of all 195 GBD countries globally in 2017 (Fig 3).
Fig 1.
Global 2017 AD age-standardized DALYs per 100,000 people in males and females. The bars indicate DALYs rate, and the lines indicate prevalence rate. AD, Atopic dermatitis; DALYs, disability-adjusted life years.
Fig 2.
Age-standardized DALYs of AD by sex and geographic GBD super regions in 2017. AD, Atopic dermatitis; DALYs, disability-adjusted life years; GBD, global burden of disease.
Fig 3.
Age-standardized DALYs rates from AD by SDI for 195 countries and territories in 2017. AD, Atopic dermatitis; DALYs, disability-adjusted life years; SDI, sociodemographic index.
Results
The GBD 2017 global prevalence of AD in both sexes was 2689.85 per 100,000 people (95% confidence interval 2535.20-2860.85).12 The global age-standardized DALYs per 100,000 people due to AD was 123.31 (95% confidence interval 66.79-205.17) for both sexes, 110.72 (59.85-184.36) for men, and 136.43 (74.03-227.23) for women.
In 2017, the age-specific DALYs and prevalence rates showed a right-skewed distribution, with a peak between 1 and 5 years of age (Fig 1). Females showed higher DALYs due to AD throughout all age groups. As the patients aged, AD DALYs decreased in both females and males. The prevalence rate of AD also initially decreased with age until the mid50s, in which it began increasing in both the sexes. The global age-standardized DALYs due to AD in 2017 varied by geographic region but were consistently higher in females than in males in all regions (Fig 2). The GBD super region with the greatest age-standardized DALY burden caused by AD was high income (178.63 DALYs per 100,000 for males and 231.8 for females). The GBD super region with the lowest age-standardized DALY burden caused by AD was south Asia (84.51 DALYs per 100,000 for males and 100.54 for females).
The age-standardized DALY rates due to AD in 2017 were also compared with the SDI of all 195 countries measured by GBD (Fig 3). Of the 195 countries analyzed, the 10 countries with the highest age-standardized AD DALY burdens per 100,000 people were Sweden (326.91), United Kingdom (284.15), Iceland (276.98), Finland (263.57), Denmark (254.63), Norway (254.06), Andorra (243.84), Switzerland (243.75), Luxembourg (243.52), and Canada (239.03). Nine of these 10 countries were in the highest top 10th percentile of SDI.
Discussion
It is well known that the prevalence of AD is higher in younger age groups, and our data show that AD burden is the highest in patients aged 1 to 5 years. This could be explained by examining how DALYs are calculated. As mentioned previously, DALY is the sum of years of life lost due to premature death and years lived with disability (product of prevalent cases and disability weights).20 The peak prevalence of AD in this age range multiplied by increasing disability weights for mild, moderate, and severe AD produces a high DALY rate.12 The high AD burden in younger age groups could also be due to the immense strain on a child during their critical stages of psychosocial development. Embarrassment and bullying because of their skin condition could result in social isolation, which can lead to depression.21 Functioning at school and work may also be impacted by impaired concentration compounded by sleep loss caused by chronic itching.21,22 The negative impact on children's behavior and sleep has been correlated to decreases in intelligence quotient, verbal comprehension, processing speed, and working memory, which may hinder future earning potential.23 Furthermore, the burden of AD extends to the family of the child suffering from the chronic skin disease as caretakers may lose time off work to care for their child.24 Strained parent-child relationships have also been previously reported due to the stressful task of managing the child's skin care.25 In addition, although AD is generally considered a childhood disease that develops during the first few years of life, recent studies have shown that adults can have a chronic and relapsing disease course, which may explain the plateau and eventual rise of the disease prevalence rate.26,27
A sex disparity in the burden of DALYs due to AD was also shown in our data. Previous studies have reported several female-specific trends in AD, including a higher prevalence than that in males, increased likelihood of persistence of AD beyond puberty, and recurrence of AD.4,28 Our data suggest an additional sex-specific predictor of the course of AD, in that, females have a higher burden of disease due to AD throughout all age groups. The reason for this is not yet entirely understood, but possible explanations could include the higher overall prevalence in females, severity of the disease, secondary complications, and impact on the quality of life. The impact of AD on individual and family quality of life has been shown to be more severe in females than in males.29, 30, 31 It is speculated that females have a culturally determined, higher ideal of physical appearance than males, which may explain this quality of life disparity between the sexes and could lead to a greater psychosocial burden of disease in AD.32 These sex-specific differences in AD burden should be kept in mind while developing programs to address the burden of AD.
Our results also demonstrate a higher AD burden in high-income regions. This is supported by previous prevalence studies, which have reported an association between a higher socioeconomic status and AD prevalence and morbidity.33,34 Individuals living in metropolitan areas with higher educational attainment have been associated with a higher prevalence of AD.35, 36, 37 Many metropolitan-related environment factors may account for this phenomenon. An increased prevalence of AD was associated with motor vehicle particle air pollution and increased use of modern fuels, like kerosene, in homes.38,39 Additionally, the “hygiene hypothesis” has been proposed to explain the high prevalence of atopic diseases in more developed countries.40 The hypothesis suggests that improved living conditions, antibiotic use, and childhood vaccinations result in the reduction of infections. The lack of microbial burden thus redirects the typical T-helper type 1 immune response toward a T-helper type 2 response, predisposing individuals to the diverse range of atopic diseases.40
There is a large economic burden associated with AD. Although current and comprehensive information on the financial burden of AD is not available, the most recent study conducted estimated the financial costs associated with AD in the United States in 2004 as $4.3 billion.41 These costs included direct medical costs, such as medical visits and medication use, and indirect costs, including lost productivity of patients and caregivers and restricted activity days.41 The current cost of AD likely exceeds the 2004 estimate because of increasing costs of medications and prevalence.42 Furthermore, more than one-fourth of health care costs for patients with AD may be attributed to treating AD and its comorbid conditions, such as allergic rhinitis and asthma.43 The cost of illness varies considerably among countries, but the total expense for each health care system is significant.44,45 For example, the total cost of AD in Canada was estimated to be $1.4 billion in 2002.45 A positive relationship between AD severity and cost has been previously reported.45, 46, 47 Despite wealthier countries having higher DALYs, the global economic burden due to AD is likely to remain significant. Given the high financial impact of AD, it is important to develop better directed population-based interventions and initiatives.
Limitations of GBD studies have been previously described, and there are additional important considerations in the context of the global burden of AD.42 Studies measuring the prevalence and incidence of AD often differ in focus based on target populations, sex categories, and age groups, making data difficult to compare due to different study methodologies. Further limitations include the descriptions of case definitions (eg, self-reported, physician's, or dermatologist's diagnosis) or how prevalence is defined (eg, point prevalence, period prevalence, and lifetime prevalence). Available studies for comparisons among different GBD regions may also be limited by geographic coverage, where certain populations have a relative over- or under-representation of total studies in comparison to their total population. Furthermore, the social stigmatization associated with AD may also lead to underestimation of global cases due to under-reporting by patients.42
AD continues to be a significant public health concern globally, particularly in high-income countries and among women and young children. The personal impact on patients and their families as well as the financial implications on economies are huge and should not be underappreciated. As a worldwide epidemiological assessment, GBD 2017 provides broad and frequently updated control measures for AD burden. This extracted data analysis might help guide AD research protocols, health policies, and prioritization efforts to reduce the global burden of this important and impactful skin disease.
Footnotes
Funding sources: The GBD was partially funded by the Bill & Melinda Gates Foundation.
Conflicts of interest: This research has been conducted as part of the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD), coordinated by the Institute for Health Metrics and Evaluation. Katelyn Urban is a collaborator with the GBD. This article was not developed with consultation or support with the Global Burden of Disease research team. Authors Chu and Nedley and Drs Giesey, Mehrmal, Uppal, and Delost have no conflicts of interest to declare.
IRB approval status: Not applicable.
References
- 1.Leung D.Y. Pathogenesis of atopic dermatitis. J Allergy Clin Immunol. 1999;104(3):S99–S108. doi: 10.1016/s0091-6749(99)70051-5. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Collaborative Network . 2017. Global Burden of Disease Study 2016 (GBD 2016) results.http://ghdx.healthdata.org/gbd-2016 Accessed May 1, 2020. Available at: [Google Scholar]
- 3.Asher M.I., Montefort S., Bjorksten B. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368(9537):733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 4.Barbarot S., Auziere S., Gadkari A. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy. 2018;73(6):1284–1293. doi: 10.1111/all.13401. [DOI] [PubMed] [Google Scholar]
- 5.Beattie P.E., Lewis-Jones M.S. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol. 2006;155(1):145–151. doi: 10.1111/j.1365-2133.2006.07185.x. [DOI] [PubMed] [Google Scholar]
- 6.Drucker A.M., Wang A.R., Li W.Q., Sevetson E., Block J.K., Qureshi A.A. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137(1):26–30. doi: 10.1016/j.jid.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organizaation Health statistics and information systems. Glob Health Estimates. 2014;13:2014. [Google Scholar]
- 8.GBD 2016 Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehrmal S., Uppal P., Giesey R.L., Delost G.R. Identifying the prevalence and disability-adjusted life years of the most common dermatoses worldwide. J Am Acad Dermatol. 2020;82(1):258–259. doi: 10.1016/j.jaad.2019.09.066. [DOI] [PubMed] [Google Scholar]
- 10.Hay R.J., Johns N.E., Williams H.C. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 11.Karimkhani C., Dellavalle R.P., Coffeng L.E. Global skin disease morbidity and mortality: an update from the Global Burden of Disease Study 2013. JAMA Dermatol. 2017;153(5):406–412. doi: 10.1001/jamadermatol.2016.5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute for Health Metrics and Evaluation (IHME) IHME; 2018. Findings from the Global Burden of Disease Study 2017.http://www.healthdata.org/policy-report/findings-global-burden-disease-study-2017 Accessed May 1, 2020. Available at: [Google Scholar]
- 13.Williams H., Stewart A., von Mutius E., Cookson W., Anderson H.R. International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Group. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121(4):947–954. doi: 10.1016/j.jaci.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Brunner P.M., Silverberg J.I., Guttman-Yassky E. Increasing comorbidities suggest that atopic dermatitis is a systemic disorder. J Invest Dermatol. 2017;137(1):18–25. doi: 10.1016/j.jid.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 15.Yaghmaie P., Koudelka C.W., Simpson E.L. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol. 2013;131(2):428–433. doi: 10.1016/j.jaci.2012.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slattery M.J., Essex M.J., Paletz E.M. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J Allergy Clin Immunol. 2011;128(3):668–671. doi: 10.1016/j.jaci.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiebert G., Sorensen S.V., Revicki D. Atopic dermatitis is associated with a decrement in health-related quality of life. Int J Dermatol. 2002;41(3):151–158. doi: 10.1046/j.1365-4362.2002.01436.x. [DOI] [PubMed] [Google Scholar]
- 18.Frequently asked questions: IHME. Accessed May 1, 2020. Available at: http://www.healthdata.org/gbd/faq
- 19.Protocol for the global burden of diseases, injuries, and risk factors study (GBD) Institute for Health Metrics and Evaluation; 2018. http://www.healthdata.org/gbd/about/protocol Accessed May 1, 2020. Available at: [Google Scholar]
- 20.Lajoie J. National Collaborating Centre for Infectious Diseases; 2014. Understanding the measurement of global burden of disease.https://nccid.ca/publications/understanding-the-measurement-of-global-burden-of-disease/ Accessed May 1, 2020. Available at: [Google Scholar]
- 21.Lewis-Jones S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema. Int J Clin Pract. 2006;60(8):984–992. doi: 10.1111/j.1742-1241.2006.01047.x. [DOI] [PubMed] [Google Scholar]
- 22.Zuberbier T., Orlow S.J., Paller A.S. Patient perspectives on the management of atopic dermatitis. J Allergy Clin Immunol. 2006;118(1):226–232. doi: 10.1016/j.jaci.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 23.Camfferman D., Kennedy J.D., Gold M., Simpson C., Lushington K. Sleep and neurocognitive functioning in children with eczema. Int J Psychophysiol. 2013;89(2):265–272. doi: 10.1016/j.ijpsycho.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Carroll C.L., Balkrishnan R., Feldman S.R., Fleischer A.B., Jr., Manuel J.C. The burden of atopic dermatitis: impact on the patient, family, and society. Pediatr Dermatol. 2005;22(3):192–199. doi: 10.1111/j.1525-1470.2005.22303.x. [DOI] [PubMed] [Google Scholar]
- 25.Arndt J., Smith N., Tausk F. Stress and atopic dermatitis. Curr Allergy Asthma Rep. 2008;8(4):312–317. doi: 10.1007/s11882-008-0050-6. [DOI] [PubMed] [Google Scholar]
- 26.Vinding G.R., Zarchi K., Ibler K.S., Miller I.M., Ellervik C., Jemec G.B. Is adult atopic eczema more common than we think? - a population-based study in Danish adults. Acta Derm Venereol. 2014;94(4):480–482. doi: 10.2340/00015555-1761. [DOI] [PubMed] [Google Scholar]
- 27.Mortz C.G., Andersen K.E., Dellgren C., Barington T., Bindslev-Jensen C. Atopic dermatitis from adolescence to adulthood in the TOACS cohort: prevalence, persistence and comorbidities. Allergy. 2015;70(7):836–845. doi: 10.1111/all.12619. [DOI] [PubMed] [Google Scholar]
- 28.Peters A.S., Kellberger J., Vogelberg C. Prediction of the incidence, recurrence, and persistence of atopic dermatitis in adolescence: a prospective cohort study. J Allergy Clin Immunol. 2010;126(3):590–595. doi: 10.1016/j.jaci.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 29.Hon K.L., Leung T.F., Wong K.Y., Chow C.M., Chuh A., Ng P.C. Does age or gender influence quality of life in children with atopic dermatitis? Clin Exp Dermatol. 2008;33(6):705–709. doi: 10.1111/j.1365-2230.2008.02853.x. [DOI] [PubMed] [Google Scholar]
- 30.Chernyshov P.V. Gender differences in health-related and family quality of life in young children with atopic dermatitis. Int J Dermatol. 2012;51(3):290–294. doi: 10.1111/j.1365-4632.2011.04997.x. [DOI] [PubMed] [Google Scholar]
- 31.Girolomoni G., Abeni D., Masini C. The epidemiology of atopic dermatitis in Italian schoolchildren. Allergy. 2003;58(5):420–425. doi: 10.1034/j.1398-9995.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- 32.Holm E.A., Esmann S., Jemec G.B. Does visible atopic dermatitis affect quality of life more in women than in men? Gend Med. 2004;1(2):125–130. doi: 10.1016/s1550-8579(04)80017-2. [DOI] [PubMed] [Google Scholar]
- 33.Ofenloch R.F., Schuttelaar M.L., Svensson A. Socioeconomic status and the prevalence of skin and atopic diseases in five European countries. Acta Derm Venereol. 2019;99(3):309–314. doi: 10.2340/00015555-3082. [DOI] [PubMed] [Google Scholar]
- 34.Mercer M.J., Joubert G., Ehrlich R.I. Socioeconomic status and prevalence of allergic rhinitis and atopic eczema symptoms in young adolescents. Pediatr Allergy Immunol. 2004;15(3):234–241. doi: 10.1111/j.1399-3038.2004.00125.x. [DOI] [PubMed] [Google Scholar]
- 35.Shaw T.E., Currie G.P., Koudelka C.W., Simpson E.L. Eczema prevalence in the United States: data from the 2003 National Survey of Children's Health. J Invest Dermatol. 2011;131(1):67–73. doi: 10.1038/jid.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu F., Yan S., Li F. Prevalence of childhood atopic dermatitis: an urban and rural community-based study in Shanghai, China. PLoS One. 2012;7(5):e36174. doi: 10.1371/journal.pone.0036174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yemaneberhan H., Flohr C., Lewis S.A. Prevalence and associated factors of atopic dermatitis symptoms in rural and urban Ethiopia. Clin Exp Allergy. 2004;34(5):779–785. doi: 10.1111/j.1365-2222.2004.1946.x. [DOI] [PubMed] [Google Scholar]
- 38.Diaz-Sanchez D., Proietti L., Polosa R. Diesel fumes and the rising prevalence of atopy: an urban legend? Curr Allergy Asthma Rep. 2003;3(2):146–152. doi: 10.1007/s11882-003-0027-4. [DOI] [PubMed] [Google Scholar]
- 39.Venn A.J., Yemaneberhan H., Bekele Z., Lewis S.A., Parry E., Britton J. Increased risk of allergy associated with the use of kerosene fuel in the home. Am J Respir Crit Care Med. 2001;164(9):1660–1664. doi: 10.1164/ajrccm.164.9.2103101. [DOI] [PubMed] [Google Scholar]
- 40.Okada H., Kuhn C., Feillet H., Bach J.F. The 'hygiene hypothesis' for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1–9. doi: 10.1111/j.1365-2249.2010.04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bickers D.R., Lim H.W., Margolis D. The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55(3):490–500. doi: 10.1016/j.jaad.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 42.Drucker A.M., Wang A.R., Qureshi A.A. Research gaps in quality of life and economic burden of atopic dermatitis: the National Eczema Association Burden of Disease Audit. JAMA Dermatol. 2016;152(8):873–874. doi: 10.1001/jamadermatol.2016.1978. [DOI] [PubMed] [Google Scholar]
- 43.Ellis C.N., Drake L.A., Prendergast M.M. Cost of atopic dermatitis and eczema in the United States. J Am Acad Dermatol. 2002;46(3):361–370. doi: 10.1067/mjd.2002.120528. [DOI] [PubMed] [Google Scholar]
- 44.Verboom P., Hakkaart-Van L., Sturkenboom M., De Zeeuw R., Menke H., Rutten F. The cost of atopic dermatitis in the Netherlands: an international comparison. Br J Dermatol. 2002;147(4):716–724. doi: 10.1046/j.1365-2133.2002.04964.x. [DOI] [PubMed] [Google Scholar]
- 45.Barbeau M., Bpharm H.L. Burden of atopic dermatitis in Canada. Int J Dermatol. 2006;45(1):31–36. doi: 10.1111/j.1365-4632.2004.02345.x. [DOI] [PubMed] [Google Scholar]
- 46.Kemp A.S. Atopic eczema: its social and financial costs. J Paediatr Child Health. 1999;35(3):229–231. doi: 10.1046/j.1440-1754.1999.00343.x. [DOI] [PubMed] [Google Scholar]
- 47.Su J.C., Kemp A.S., Varigos G.A., Nolan T.M. Atopic eczema: its impact on the family and financial cost. Arch Dis Child. 1997;76(2):159–162. doi: 10.1136/adc.76.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]