Abstract
BACKGROUND
Allergic bronchopulmonary aspergillosis (ABPA) is an allergic reaction to Aspergillus species that aggravates bronchial asthma. Previous studies demonstrated the glucocorticoid-sparing effect of dupilumab in patients with ABPA. There is no report of complete withdrawal of glucocorticoids after dupilumab.
CASE SUMMARY
The patient was a 54-year-old woman with bronchial asthma treated with inhaled corticosteroids and a long-acting beta-2 agonist. She consulted our institution for productive cough and fever in March 2017. Chest computed tomography scan revealed mucoid impaction, and the bronchial lavage fluid culture was positive for Aspergillus fumigatus. The diagnosis was ABPA. The patient was treated with oral glucocorticoids from April 2017 to November 2017. In January 2019, she had bronchial asthma exacerbation, and a chest computed tomography scan showed recurrent mucoid impaction. She was treated with oral glucocorticoids and itraconazole. In February 2020, during tapering of oral glucocorticoid, she had the third episode of bronchial asthma exacerbation and a mucoid impaction. The patient was treated with dupilumab in addition to oral glucocorticoid and itraconazole. The clinical response improved, and oral glucocorticoid was discontinued in June 2020.
CONCLUSION
This is the first case of ABPA in which complete withdrawal of glucocorticoid was possible after treatment with dupilumab.
Keywords: Allergic bronchopulmonary aspergillosis, Dupilumab, Asthma, Interleukin-13, Interleukin-4, Case report
Core Tip: Allergic bronchopulmonary aspergillosis (ABPA) is an allergic reaction to antigen from Aspergillus species that causes exacerbation of bronchial asthma, eosinophilic pneumonia, and bronchiectasis. Conventional therapy includes the administration of oral glucocorticoids and other antiasthmatic therapy. However, there are intractable cases showing repeated clinical exacerbations of bronchial asthma despite therapy with oral glucocorticoids. Previous reports have shown that the addition of monoclonal antibodies against interleukin (IL)-4/IL-13 or dupilumab to the treatment is effective and allows the reduction in the dose of glucocorticoids in ABPA patients. However, there is no report of complete withdrawal of oral glucocorticoids after therapy with dupilumab in these patients. Here, we report the first case of ABPA in which complete withdrawal of oral glucocorticoid was possible after treatment with dupilumab.
INTRODUCTION
Allergic bronchopulmonary aspergillosis (ABPA) is an allergic reaction to Aspergillus species[1]. ABPA causes exacerbation of bronchial asthma, eosinophilic pneumonia, and bronchiectasis[1]. Treatment of ABPA is critical for the clinical control of bronchial asthma. The administration of oral glucocorticoid alone or in combination with antifungal drugs are effective therapeutic approaches[1]. However, ABPA is highly prone to relapse when the oral glucocorticoid dose is reduced or is completely discontinued. Patients with ABPA have also been reported to respond to the treatment with anti-immunoglobulin E (IgE) or anti-interleukin (IL)-5 antibody[2-4]. However, most cases of ABPA require therapy with oral glucocorticoids to control clinical exacerbations of bronchial asthma. The oral glucocorticoid-sparing effect of anti-IL-4/IL-13 antibody (dupilumab) has been previously reported[5]. However, there is no report on the complete withdrawal of glucocorticoids following dupilumab therapy. Here, we report a case of ABPA in which glucocorticoids were completely unnecessary to control bronchial asthma exacerbation after dupilumab therapy.
CASE PRESENTATION
Chief complaints
The patient was a 54-year-old woman that consulted the Mie Chuo Medical Center because of fever and productive cough.
History of present illness
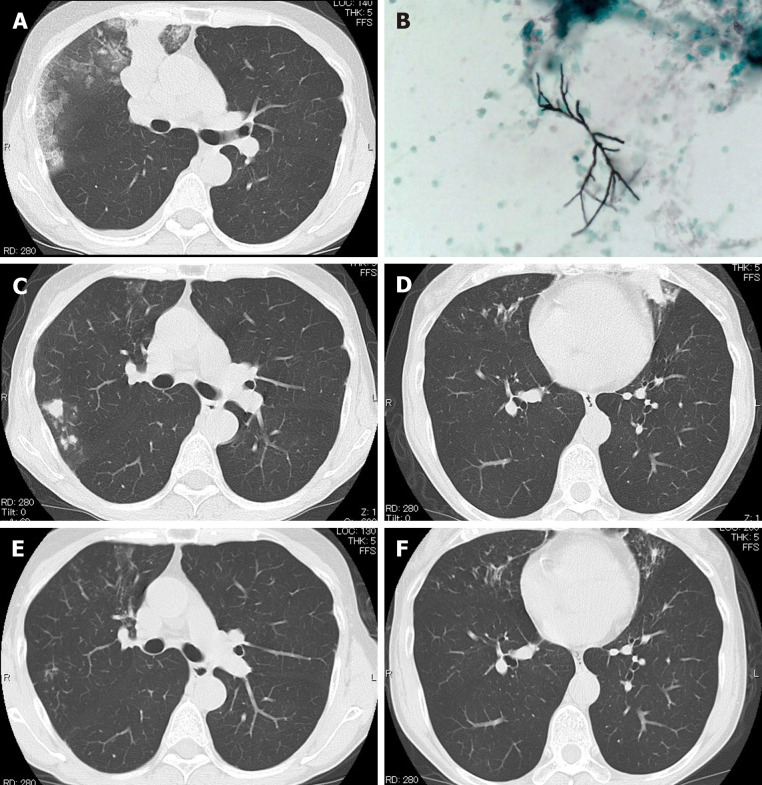
In April 2017, she presented at the outpatient clinic of Mie Chuo Medical Center for fever and productive cough. A chest computed tomography (CT) scan revealed consolidation, ground-glass opacity, and mucoid impaction of the right upper lung (Figure 1A). The culture of the bronchial lavage fluid was positive for Aspergillus fumigatus (A. fumigatus) (Figure 1B). The anti-aspergillus antibody was positive with a serum anti-aspergillus-specific IgE concentration of 28.9 UA/mL. The diagnosis was ABPA. Treatment with oral prednisolone at a dose of 0.5 mg/kg/d was started in April 2017. The clinical symptoms of the patient improved, and the oral glucocorticoid therapy was discontinued in November 2017.
Figure 1.
Chest computed tomography scan. A: At presentation, the computed tomography (CT) of the patient showed consolidation, ground-glass opacity, and mucoid impaction in the right upper lung; B: Grocott’s staining of the mucoid impaction tissue showed septate fungal hyphae, and Aspergillus fumigatus was confirmed by culture; C and D: Chest CT during the third recurrence of allergic bronchopulmonary aspergillosis showing mucoid impaction in the upper lobe of the right lung and lower lobe of the left lung; E and F: The CT findings in C and D disappeared 1 mo after dupilumab administration.
However, in January 2019, she presented again with fever and exacerbation of her bronchial asthma. The chest CT scan showed a recurrence of mucoid impaction. The CT finding improved after treating the patient with oral (0.5 mg/kg/d) glucocorticoid and oral itraconazole in January 2019. The dose of oral glucocorticoid was then gradually reduced.
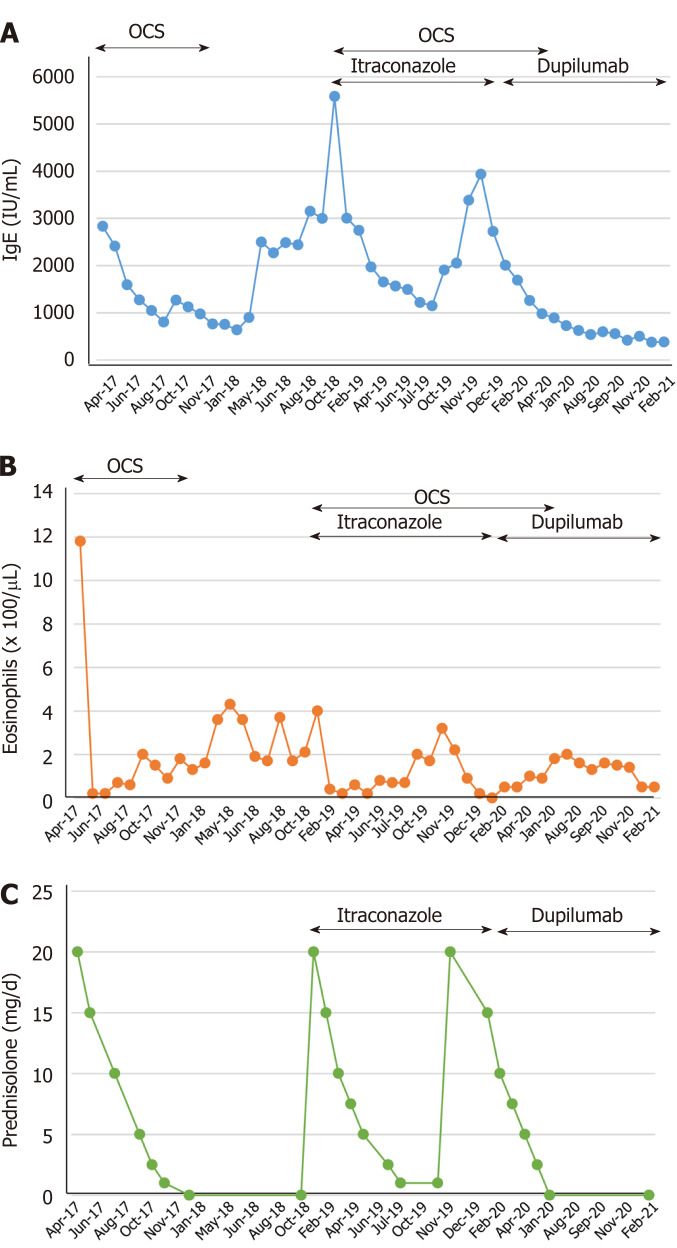
However, in November 2019, she had another episode of bronchial asthma exacerbation in association with increased serum total IgE, eosinophilia, and recurrent mucoid impaction by CT scan (Figure 1C and D). In February 2020, we started treating the patient with dupilumab (300 mg/2-wk) in addition to oral glucocorticoid (0.5 mg/kg/d) and itraconazole (100 mg/d). The mucoid impaction disappeared after the combined therapy of dupilumab and oral glucocorticoid (Figure 1E and F). We continued treating the patient with dupilumab, but discontinued the administration of oral glucocorticoid in June 2020. During follow-up, the patient showed no symptoms of bronchial asthma exacerbation or recurrence of mucoid impaction. IgE levels and the eosinophil count in peripheral blood were not increased after discontinuation of oral glucocorticoids and maintenance with dupilumab (Figure 2).
Figure 2.
Laboratory data and dose of oral prednisolone. Changes in the serum total immunoglobulin E (IgE) levels, peripheral blood eosinophil count and dose of oral corticosteroids (OCS).
History of past illness
She had no medical history of any disease.
Personal and family history
No history.
Physical examination
The patient's physical examination showed symptoms and signs of airway obstruction.
Laboratory examinations
During her first consultation, the culture of the bronchial lavage fluid was positive for A. fumigatus (Figure 1B), and the anti-aspergillus antibody was positive with a serum anti-aspergillus-specific IgE concentration of 28.9 UA/mL. The total serum levels of IgE (3387 IU/mL) were also increased during her second consultation.
Imaging examinations
A chest CT scan revealed consolidation, ground-glass opacity, and mucoid impaction of the right upper lung (Figure 1A). During her second and third consultations for clinical exacerbation of bronchial asthma, her chest CT scan findings were compatible with a recurrence of mucoid impaction.
FINAL DIAGNOSIS
The final diagnosis was ABPA with repeated clinical exacerbations of bronchial asthma.
TREATMENT
The patient was initially treated with oral prednisolone at a dose of 0.5 mg/kg/d in April 2017. The clinical symptoms of the patient improved, and the oral glucocorticoid therapy was discontinued in November 2017. The patient received treatment with oral (0.5 mg/kg/d) glucocorticoid and oral itraconazole (100 mg/d) in January 2019 during her second consultation for bronchial asthma exacerbation. The dose of oral glucocorticoid was then gradually reduced. During her third episode of bronchial asthma exacerbation, we treated the patient with dupilumab (300 mg/2-wk) in addition to oral glucocorticoid (0.5 mg/kg/d) and itraconazole (100 mg/d).
OUTCOME AND FOLLOW-UP
The mucoid impaction detected by the chest CT scan disappeared after the combined therapy of dupilumab and oral glucocorticoid (Figure 1E and F). We then continued treating the patient with dupilumab, but discontinued the administration of oral glucocorticoid in June 2020. Despite discontinuing her treatment with oral glucocorticoids, inhaled glucocorticoids, and a long-acting beta-2 agonist inhalation for 4 mo after starting therapy with dupilumab, she had no symptoms of bronchial asthma exacerbation or mucoid impaction by chest CT scan.
DISCUSSION
The pathogenesis of ABPA is not completely clear. Deficient fungal clearance from the airways and excessive activation of CD4+ T helper 2 (Th2) cells play important roles[1]. A predominant activation of Th2 cells in ABPA leads to increased inflammatory cytokines, including IL-4, IL-5, IL-13, CCL-17, and IL-9[6]. Failure to eradicate the fungus leads to a sustained immune response in the airways of patients with ABPA[7]. This excessive immune response induces an inflammatory response characterized by elevated serum levels of IgE, increased mast cell degranulation, enhanced activation of eosinophils and neutrophils that ultimately causes mucoid impaction, eosinophilic pneumonia, or bronchiectasis[8].
The therapeutic efficacy of monoclonal antibodies against Th2 mediators including IgE (omalizumab), IL-5 (mepolizumab), IL-5R (benralizumab), and anti-IL-4/IL-13 (dupilumab) has been reported in patients with ABPA[2-4]. The administration of dupilumab decreases the peripheral blood count of eosinophils and the serum levels of IgE in patients with severe bronchial asthma[9]. Several reports have also demonstrated the efficacy of dupilumab in ABPA (Table 1)[5,9-11]. For example, Mümmler et al[5] reported a case of bronchial asthma associated with ABPA in which the administration of omalizumab or dupilumab reduced the dose of oral glucocorticoids. Also, Mikura et al[9] and Ramonell et al[10] reported cases of ABPA in which the administration of dupilumab, but not that of mepolizumab, made possible a reduction in the dose of oral glucocorticoids. Mepolizumab and benralizumab suppress eosinophil activation, but they are unable to inhibit IgE pro-inflammatory activity. However, dupilumab inhibits the upstream of the Th2-mediated immune response, and thus it is effective in ABPA patients with elevated serum total IgE. Omalizumab is also effective in ABPA, but its indication is restricted to cases showing serum IgE levels less than 1500 IU/mL[1,3]. These observations support the therapeutic efficacy and the oral glucocorticoid-sparing effect of monoclonal antibodies against Th2 mediators in ABPA patients. Unlike previous cases in the present study, we report the first case of ABPA in which the therapy with dupilumab was so effective that oral glucocorticoids, inhaled glucocorticoids, and long-acting beta-2 agonists became completely unnecessary to control recurrence of clinical exacerbations and improve radiological abnormalities in bronchial asthma. Phase III clinical trials should be undertaken in the future to confirm these beneficial effects of dupilumab in ABPA patients.
Table 1.
Reported cases of allergic bronchopulmonary aspergillosis treated with dupilumab
|
Ref.
|
Age, yr
|
Sex
|
Timing of dupilumab therapy
|
Treatment in combination with dupilumab
|
Baseline IgE (IU/mL)
|
Baseline eosinophil count (/µL)
|
Chest CT findings
|
| Ramonell et al[10], 2020 | 60 | Female | Disease recurrence | OCS | 561 | 90 | Cylindrical bronchiectasis |
| Ramonell et al[10], 2020 | 51 | Female | Disease recurrence | OCS | > 2000 | 90 | Bilateral central bronchiectasis |
| Ramonell et al[10], 2020 | 33 | Male | Disease diagnosis | Voriconazole | 11290 | 1750 | Mild diffuse bronchiectasis |
| Mümmler et al[5], 2020 | 49 | Female | Disease recurrence | OCS | 7000 | 950 | Pulmonary infiltrates, diffuse pulmonary bronchiectasis and bronchial wall thickening |
| Tashiro et al[11], 2021 | 72 | Female | Disease diagnosis | None | 2525 | 5637 | Centrilobular nodules, infiltrations, and high-attenuation mucus in the bronchi with central dilatation |
| Mikura et al[9], 2021 | 45 | Male | Disease recurrence | OCS, itraconazole | 2306 | 1914 | High-attenuation mucus and ground glass opacity |
| Present case | 54 | Female | Disease recurrence | OCS, itraconazole | 2833 | 1180 | Consolidation, ground-glass opacity, and high-attenuation mucus |
IgE: Immunoglobulin E; CT: Computed tomography; OCS: Oral corticosteroids.
CONCLUSION
This is the first report of a case of ABPA in which reduction in the dose and, subsequently, complete withdrawal of glucocorticoids was possible after treatment with dupilumab.
Footnotes
Informed consent statement: Informed consent was obtained from the subject involved in the study.
Conflict-of-interest statement: None of the authors declared no conflict of interest concerning this case report.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: April 25, 2021
First decision: June 6, 2021
Article in press: June 22, 2021
Specialty type: Allergy
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Panaitescu C, Zhuo ZQ S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Zhang YL
Contributor Information
Tadashi Nishimura, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Tomohito Okano, Department of Pulmonary and Critical Care Medicine, Mie University, Tsu 514-8507, Mie, Japan.
Masahiro Naito, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Chikashi Tsuji, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Soichi Iwanaka, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Yasumasa Sakakura, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Taro Yasuma, Department of Immunology, Mie University School of Medicine, Mie University, Tsu 514-8507, Mie, Japan.
Hajime Fujimoto, Department of Pulmonary and Critical Care Medicine, Mie University, Tsu 514-8507, Mie, Japan.
Corina N D'Alessandro-Gabazza, Department of Immunology, Mie University School of Medicine, Mie University, Tsu 514-8507, Mie, Japan.
Yasuhiro Oomoto, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
Tetsu Kobayashi, Department of Pulmonary and Critical Care Medicine, Graduate School of Medicine Mie, Mie University, Tsu 514-8507, Mie, Japan.
Esteban C Gabazza, Department of Immunology, Mie University School of Medicine, Mie University, Tsu 514-8507, Mie, Japan. gabazza@doc.medic.mie-u.ac.jp.
Hidenori Ibata, Department of Pulmonary Medicine, Mie Chuo Medical Center, Tsu 514-1101, Mie, Japan.
References
- 1.Agarwal R, Sehgal IS, Dhooria S, Muthu V, Prasad KT, Bal A, Aggarwal AN, Chakrabarti A. Allergic bronchopulmonary aspergillosis. Indian J Med Res. 2020;151:529–549. doi: 10.4103/ijmr.IJMR_1187_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altman MC, Lenington J, Bronson S, Ayars AG. Combination omalizumab and mepolizumab therapy for refractory allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol Pract. 2017;5:1137–1139. doi: 10.1016/j.jaip.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Li JX, Fan LC, Li MH, Cao WJ, Xu JF. Beneficial effects of Omalizumab therapy in allergic bronchopulmonary aspergillosis: A synthesis review of published literature. Respir Med. 2017;122:33–42. doi: 10.1016/j.rmed.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Soeda S, Kono Y, Tsuzuki R, Yamawaki S, Katsube O, To M, To Y. Allergic bronchopulmonary aspergillosis successfully treated with benralizumab. J Allergy Clin Immunol Pract. 2019;7:1633–1635. doi: 10.1016/j.jaip.2018.11.024. [DOI] [PubMed] [Google Scholar]
- 5.Mümmler C, Kemmerich B, Behr J, Kneidinger N, Milger K. Differential response to biologics in a patient with severe asthma and ABPA: a role for dupilumab? Allergy Asthma Clin Immunol. 2020;16:55. doi: 10.1186/s13223-020-00454-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schuyler M. The Th1/Th2 paradigm in allergic bronchopulmonary aspergillosis. J Lab Clin Med. 1998;131:194–196. doi: 10.1016/s0022-2143(98)90089-0. [DOI] [PubMed] [Google Scholar]
- 7.Romani L. Immunity to fungal infections. Nat Rev Immunol. 2011;11:275–288. doi: 10.1038/nri2939. [DOI] [PubMed] [Google Scholar]
- 8.Knutsen AP, Slavin RG. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin Dev Immunol. 2011;2011:843763. doi: 10.1155/2011/843763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mikura S, Saraya T, Yoshida Y, Oda M, Ishida M, Honda K, Nakamoto K, Tamura M, Takata S, Shimoyamada H, Fujiwara M, Ishii H. Successful Treatment of Mepolizumab- and Prednisolone-resistant Allergic Bronchopulmonary Aspergillosis with Dupilumab. Intern Med. 2021 doi: 10.2169/internalmedicine.6679-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramonell RP, Lee FE, Swenson C, Kuruvilla M. Dupilumab treatment for allergic bronchopulmonary aspergillosis: A case series. J Allergy Clin Immunol Pract. 2020;8:742–743. doi: 10.1016/j.jaip.2019.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tashiro H, Takahashi K, Kurihara Y, Sadamatsu H, Kimura S, Sueoka-Aragane N. Efficacy of dupilumab and biomarkers for systemic corticosteroid naïve allergic bronchopulmonary mycosis. Allergol Int. 2021;70:145–147. doi: 10.1016/j.alit.2020.08.006. [DOI] [PubMed] [Google Scholar]