Abstract
Purpose
In a clinical trial (NCT03406416) of a second-generation (44-channel) suprachoroidal retinal prosthesis implanted in subjects with late-stage retinitis pigmentosa (RP), we assessed performance in real-world functional visual tasks and emotional well-being.
Methods
The Functional Low-Vision Observer Rated Assessment (FLORA) and Impact of Vision Impairment–Very Low Vision (IVI-VLV) instruments were administered to four subjects before implantation and after device fitting. The FLORA contains 13 self-reported and 35 observer-reported items ranked for ease of conducting task (impossible-easy, central tendency given as mode). The IVI-VLV instrument quantified the impact of low vision on daily activities and emotional well-being.
Results
Three subjects completed the FLORA for two years after device fitting; the fourth subject ceased participation in the FLORA after fitting for reasons unrelated to the device. For all subjects at each post-fitting visit, the mode ease of task with device ON was better or equal to device OFF. Ease of task improved over the first six months with device ON, then remained stable. Subjects reported improvements in mobility, functional vision, and quality of life with device ON. The IVI-VLV suggested self-assessed vision-related quality of life was not impacted by device implantation or usage.
Conclusions
Subjects demonstrated sustained improved ease of task scores with device ON compared to OFF, indicating the device has a positive impact in the real-world setting.
Translational Relevance
Our suprachoroidal retinal prosthesis shows potential utility in everyday life, by enabling an increased environmental awareness and improving access to sensory information for people with end-stage RP.
Keywords: retinal prosthesis, functional vision, low vision, retinitis pigmentosa, orientation and mobility
Introduction
Developing retinal prostheses (“bionic eyes”) to provide functional vision to individuals with late-stage retinitis pigmentosa (RP) has been a goal for the last 30 years.1 RP is a genetically inherited disorder of the eye characterized by the progressive death and dysfunction of photoreceptor cells, inevitably resulting in vision loss and blindness.2 RP is linked to mutations in more than 300 genes,3 affects one in every 4000 people worldwide,2 and is mostly untreatable at this time.4,5 Retinal prostheses enable patients with late-stage RP to regain basic visual cues to assist with orientation and mobility (O&M) and activities of daily living.6,7 They work by stimulating the relatively intact secondary neurons in the retina with electrical current, to create artificial vision perceived as phosphenes (spots or arcs).8 The artificial vision is characterized as ultra-low vision, including localization of shapes/objects, perception of movement, and light sources.6,7
Retinal prostheses have been implanted in the epiretinal position, the subretinal position or the suprachoroidal (between choroid and sclera) position.6,7,9 The suprachoroidal surgical procedure is simpler than required for epiretinal and subretinal retinal prostheses, without the need for a vitrectomy.6,10 Our first-generation suprachoroidal prototype device, tested in a clinical trial in 2012 to 2014 (clinicaltrials.gov #NCT01603576), could not be taken home and was only tested in laboratory settings.11 Although use in the laboratory showed improvement in localization12–14 and navigational skills (Barnes NM et al., IOVS, 2015, 56, ARVO E-Abstract), use in the real-world environment was not assessed. The second-generation suprachoroidal prosthesis was fully implantable, with clinical trial subjects using the device at home and in their local environments. In addition, the number of stimulating channels was increased (from 24 to 44 channels) to obtain a wider extent of retina (∼38 × 28° visual field).15 The intraocular electrodes are connected via a helical lead wire to two stimulators implanted on the scalp behind the ear (Allen PJ et al., IOVS, 2019, 60, ARVO E-Abstract). The stimulators receive data from a body-worn video processor, which in turn receives visual information from a small camera mounted on a pair of glasses.
Functional vision in the real-world environment has been investigated with epiretinal16–21 and subretinal retinal prostheses,22,23 but not yet with suprachoroidal retinal prostheses. The Functional Low-Vision Observer Rated Assessment (FLORA) instrument was developed with input from the United States Food and Drug Administration as a response to the absence of accepted, standardized assessments of functional vision or quality of life that are targeted towards prosthetic vision in the real-world environment.17 The FLORA protocol adheres to the recommendations of the Harmonisation of Outcomes and Vision Endpoints in vision Restoration trials international taskforce and has been used in multiple studies to measure functional vision with the Argus II (Second Sight Medical Products, Sylmar, CA, USA) epiretinal prosthesis.17–21
The aim of this study was to investigate whether functional vision in the real-world setting improved in late-stage RP subjects using a second generation suprachoroidal retinal prosthesis over two years. A secondary aim was to assess the vision-related quality of life to determine if device usage had any impacts on overall wellbeing.
Methods
Study Design and Subjects
The study was approved by the Human Research Ethics Committee of the Royal Victorian Eye and Ear Hospital (Project ID 16/1266H) and was carried out according to the National Statement on Ethical Conduct in Human Research (2007) produced by the Australian National Health and Medical Research Council. Informed consent was obtained before enrollment, and procedures adhered to the tenets of the Declaration of Helsinki. This study complied with the recommendations of the HOVER International Task Force.24
Four subjects (see Table 1 for demographics) with late-stage RP were enrolled in an interventional prospective experimental clinical trial (clinicaltrials.gov NCT03406416) to test the safety, visual function, functional vision, real-world outcomes, and overall quality of life when using the second-generation suprachoroidal retinal prosthesis. Primary vision outcomes will be reported in another article, with the longitudinal assessment of functional vision in the real-world setting using the FLORA tool and the accompanying vision-related quality of life questionnaire (Impact of Vision Impairment–Very Low Vision [IVI-VLV]) reported herein.
Table 1.
Subject Demographics
| Subject 1 | Subject 2 | Subject 3 | Subject 4 | |
|---|---|---|---|---|
| Gender | Male | Male | Female | Male |
| Age at implantation (y) | 47 | 63 | 66 | 39 |
| Eye condition | Retinitis pigmentosa (rod cone dystrophy) | Retinitis pigmentosa (rod cone dystrophy) | Retinitis pigmentosa (cone rod dystrophy) | Retinitis pigmentosa (cone rod dystrophy) |
| Observed Nystagmus | Mild | Intermittent | None | Mild |
| Visual acuity before implantation in both eyes | Light perception | Light perception | Light perception | Light perception |
| Age when legally blind (y) | 20 | 34 | 41 | 13 |
| Approximate years of useful form vision | 34 | 43 | 56 | 19 |
| Primary mobility aid | Cane | Cane | Guide dog | Cane |
| Implanted eye | Left | Right | Right | Right |
Subjects underwent surgery and an eight-week recovery period before per-patient customization of the electrical stimulation parameters (referred to as device fitting) as shown in Figure 1. The surgical procedures were uncomplicated and postoperative recoveries uneventful (Allen et al., IOVS, 2020, 61, ARVO E-Abstract, no. 2200).
Figure 1.
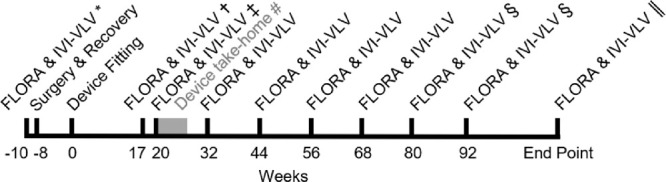
Timeline of key events relative to device fitting (week 0). *Presurgical baseline FLORA measured with no device. ✝Post-device fitting baseline FLORA at week 17. ‡Subject 4 ceased FLORA measurements at week 20 for reasons unrelated to the device. §Only subject 3 had FLORA and IVI-VLV performed at weeks 80 and 92 because of the impacts of the COVID-19 pandemic in 2020. ||Endpoint is defined as the last time point in the study where FLORA and IVI-VLV were performed for subjects 1, 2, and 3, which were at 110, 109, and 136 weeks (approximately two years) post-device fitting, respectively. The timing of the endpoint for subject 3 was extended because of the COVID-19 pandemic in 2020. #The gray zone marks the time range where subjects began using the device unsupervised at home (subject 1 = week 21.0, subject 2 = week 20.3, subject 3 = week 23.3, subject 4 = week 27.6).
After device fitting/switch-on (week 0), initial psychophysics testing produced a reliable phosphene map and list of required stimulation parameters for each subject. This configuration was maintained for the trial duration to accommodate familiarization with the phosphenes. Subjects then attended the laboratory for visual rehabilitation with the research team (weeks 1–16) receiving training on phosphene interpretation,8 effective head-scanning,25 and using the camera in laboratory-based tasks.13,26 Head-scanning skills and eye-head-camera position awareness were developed by discussing the purpose and position of the camera, explaining how to perform environment scanning methodically, and practicing interacting with high-contrast objects and obstacles.25 The post-fitting baseline FLORA assessments at week 17 were conducted after initial training was complete but before any O&M training. All FLORA assessments were performed with a backpack visual processing system so that video footage could be obtained. After training on use of a small portable vision processing unit (PVP), subjects were approved by the principal investigator (P.J.A.) for unsupervised device usage at home (“device take-home,” range 20–27 weeks, Fig. 1) and advised to use the device with the PVP as an adjunct to their existing low-vision mobility aids. Subjects were also encouraged to seek feedback from family members while exploring surroundings with the device and provided with a focused beam torch for head tracking practice. The research team and O&M specialist next discussed orientation and mobility goals with each subject and together visited their home and environs for training in specific strategies of device usage in adjunct to their existing aids. This O&M training was done in between the 12-weekly outcome visits and generally took about three to four hours per session with adequate breaks.
Subjects served as their own controls, with comparisons made between pre-surgery baseline (no device) and at time points of generally every three months from the post-device fitting baseline (week 17) with the device ON and OFF (Fig. 1). All four subjects completed FLORA assessments before surgery, and at 17 and 20 weeks after device fitting and were authorized to use the device unsupervised at home (Fig. 1). Subject 4 was issued a take-home device but did not complete FLORA assessments after week 20 because of a change in personal circumstances, unrelated to the device, and is thus excluded from analyses. Subjects 1, 2, and 3 further completed assessments at 32, 44, 56, and 68 weeks after device fitting. Subject 3 completed additional assessments at 80, 92, and 136 weeks after device fitting, whereas subjects 1 and 2 completed additional assessments at 110 and 109 weeks after device fitting, respectively. Interruption to the trial, and, hence, the difference in time points assessed between subject 3 and subjects 1 and 2 was a consequence of the COVID-19 pandemic in 2020. All data were collected between February 2018 and December 2020.
FLORA
Subjects were assessed for functional visual abilities in and around their residential setting and interviewed in their own home using the FLORA.17,18 The FLORA contains 13 self-report questions (Part 1), 35 observer-rated functional visual tasks (Part 2) for subjects to complete under observation organized into four distinct domains (“Visual Orientation,” “Visual Mobility,” “Daily Life,” and “Interaction With Others”) and a four-part case-report narrative that summarizes the assessor's evaluation of the effect of the retinal prosthesis on each subject's life (Part 3). In the Phase I developmental trial, the list of questions in Part 1 and tasks in Part 2 of the FLORA were confirmed to be sensitive to changes in functional vision in the ultra-low vision range and the rating scale did not suffer from floor or ceiling effects.17
Assessments were made by an independent qualified O&M low-vision rehabilitation specialist who had been trained on the study protocol and the FLORA. The same O&M specialist provided the goal-specific O&M training and performed the FLORA assessments. The ease with which subjects completed each functional vision task was assessed with the device ON and OFF with a four-point scale: impossible, difficult, moderate, and easy. It was our habit to start each session with device ON so that familiarity with the task would favor device OFF since the same task was first completed with the device ON. The final FLORA rating score (positive, mild positive, prior positive, neutral, negative effects) was used to assess the overall impact on the patient's life and was scored by an independent clinician using the assessments performed by the O&M specialist.
All FLORA evaluations occurred at the subjects’ residence and within their local area to measure outcomes directly relevant to their real-world environment. No effort was made to control lighting or other environmental factors to ensure assessment was reflective of a real-world experience. Because of the subjects’ individual environment and physical state (fatigue), it was not always possible to perform all 35 tasks for all subjects at specific time points.
IVI-VLV Questionnaire
Vision-related quality of life was quantified using the IVI-VLV27 questionnaire, containing 28 items with four response options using Likert scaling, ranging from “not at all” to “a lot of the time.” Items 1 to 10 have an additional response that states the subject did not do a task for other reasons. Items form two specific subscales: “activities of daily living, mobility, and safety” (16 items) and “emotional well-being” (12 items). The IVI-VLV data was collected at equivalent time points to the FLORA data (Fig. 1). Although subject 4 did not perform the FLORA after week 20, they were able to complete the IVI-VLV questionnaire sporadically.
Statistical Analysis
Stata Version 16.1/SE (StataCorp LLC, College Station, TX, USA) was used for computations. The change in ease of each task over time was investigated graphically using cumulative (stacked) bar charts, in a similar way to the real-world outcomes for the Alpha AMS device results.23 Because of the small number of subjects and the nominal ranking of task difficulty, the central tendency of subject-level ease of task was summarized separately for each visit and device status via mode. If multiple modes were present, the higher mode was taken. For each task in Part 2 at endpoint, ease was compared between device ON and OFF using Wilcoxon's matched-pairs signed-rank test as per previous results with the Argus II device,18,19 noting that because of sample size in a primary safety study, it was underpowered for this purpose. Not all tasks were completed by subjects at all time points because of subject and environmental factors.
Results
Subjects all perceived phosphene vision after device switch-on and achieved ultra-low vision outcomes during laboratory-based training for object localization, motion discrimination and orientation and mobility with device ON.
FLORA–Ease of Task Scores
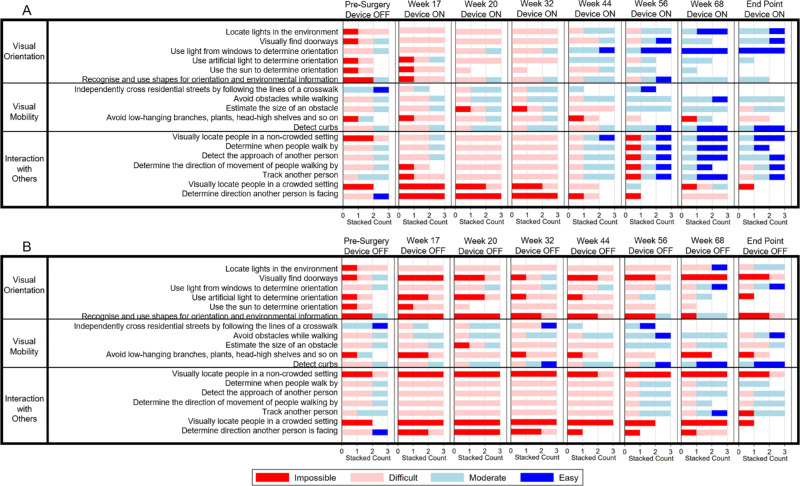
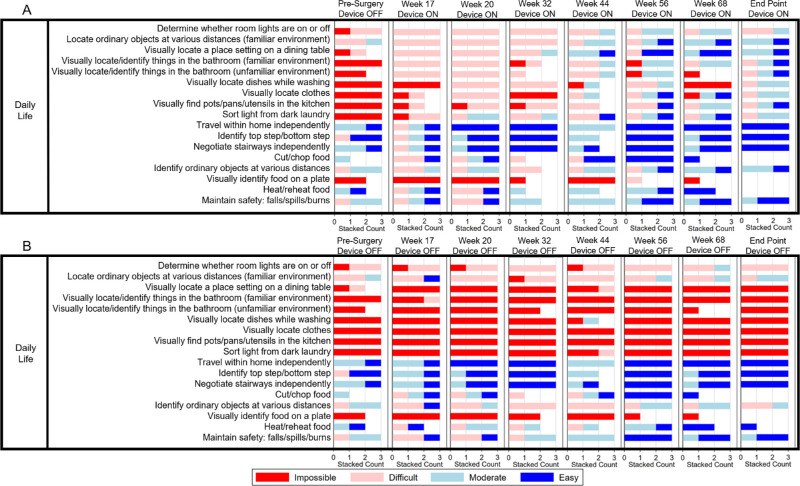
The ease of task scores are presented as cumulative (stacked) counts for the “Visual Orientation,” “Visual Mobility,” and “Interaction with Others” domains in Figure 2 and for the “Daily Life” domain in Figure 3. The X axis goes up to a maximum of three because there are three subjects. The “Daily Life” domain is shown separately for ease of viewing as it has a much larger number of tasks (17 tasks; Fig. 3) than the other domains (five to seven tasks each; Fig. 2). Generally, functional vision tasks became easier to complete over time with the device ON (Figs. 2A, 3A), trending toward “moderate” and “easy” compared to “difficult” at the presurgical baseline. In comparison, tasks were generally “impossible” or “difficult” to complete with device OFF at all time points (Figs. 2B, 3B). Figures 2 and 3 show an initial improvement in ease of task at the post-fitting baseline (week 17) with device ON compared to presurgical baseline, but the most striking improvement is seen with device ON in the first six months from the post-fitting baseline (week 17 to week 44) indicating a learning effect from visual rehabilitation and training. From week 44 to the study endpoint at two years, there is minimal further improvement in ease of task scores across all domains.
Figure 2.
Ease of task scores for functional vision tasks in the “Visual Orientation,” “Visual Mobility” and “Interaction with Others” domains with the device ON (A) and OFF (B) at each visit presented as cumulative (stacked) counts. Gaps indicate that a task was not able to be completed by all 3 subjects at that time point. Presurgery Device OFF results are duplicated in A for ease of reference.
Figure 3.
Ease of task scores of subjects for functional vision tasks in the “Daily Life” domain with the device ON (A) and OFF (B) at each visit presented as cumulative (stacked) counts. Gaps indicate that a task was not able to be completed by all three subjects at that time point. Presurgery Device OFF results are duplicated in A for ease of reference.
Tasks that involved a greater reliance on vision to complete (i.e., tasks 2, 14–20; finding doorways, visually locating a place setting on a dining table, things in the bathroom [familiar and unfamiliar], dishes while washing, clothes, pots/pans/utensils in the kitchen, people in a noncrowded setting, and sorting light from dark laundry) showed the greatest improvement from before surgery to the study endpoint than any other group of tasks. Many of these tasks went from “impossible” to complete before surgery to “moderate” or even “easy” to complete by the endpoint. In comparison, tasks 21 to 23 (travel within home independently, identify top step/bottom step, negotiate stairways independently) were rated as mostly “easy” to complete with device ON and OFF, indicating that success did not rely on extra visual information from the device. Alternatively, a few tasks, such as task 26 (visually identify food on a plate), were rated as ‘impossible’ to complete throughout the study with the device ON and OFF, indicating that the visual information provided by the device was not adequate to perform this task. Task 10 (locating low-hanging branches etc.), was generally rated as “difficult” to “impossible” with device ON and OFF, although anecdotally subjects report the device can assist with identifying higher objects such as traffic lights. This may be due to expectations within a familiar environment, as well as the size and contrast of high objects, with some overhanging tree branches being very thin relative to larger, high-contrast traffic lights. Task 7 (independently cross residential streets by following the lines of a crosswalk) was not performed routinely because crosswalks (with zebra markings) are not often available in Australia and the outdoor exploration area varied at each time point.
For all subjects at the post-fitting baseline (week 17), the ease of task score for the majority of tasks with the device switched ON was higher or equal to when it was switched OFF (Fig. 4). For subjects 1 and 2 the results are stable over time, with most tasks “impossible” to perform with device OFF and “moderate” to “easy” to perform with device ON after week 44. For subject 3, there is more variation in performance with the device OFF. Tasks are generally “impossible” to “difficult” with device OFF and generally “moderate” to perform with device ON. It was noted at week 56 that subject 3 appeared tired and distractible throughout the session (device ON and OFF), which impacted performance at that time point.
Figure 4.
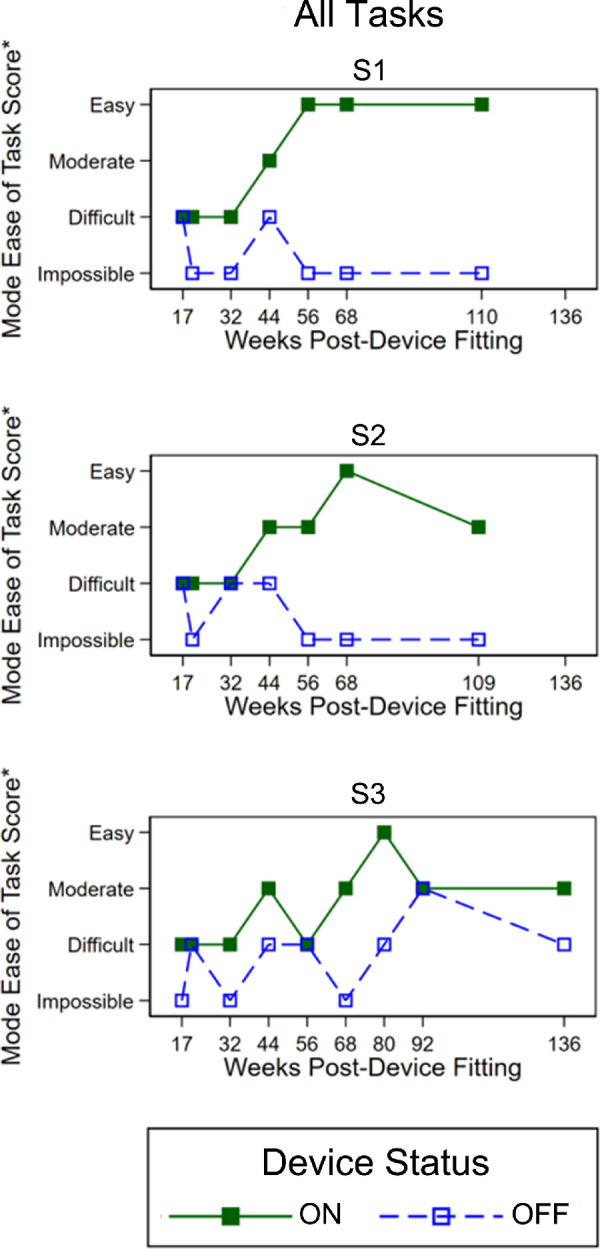
Mode ease of task scores for all tasks for subjects 1, 2, and 3 with the device switched ON and OFF up to two years (109–136 weeks) post-device fitting. *If bi-modal, higher mode presented.
The ease of task FLORA results with statistical inferences are shown in Table 2. A positive mean difference (Device ON/OFF) indicates that the task was easier with the device ON; a zero mean difference indicates the ease of task was equivalent with the device ON and OFF. There were no tasks with worse performance when the device was ON. The data show weak evidence of improvement with the device ON for most tasks; however, this trial with a primary endpoint of safety was not powered to detect a difference statistically. The assumption with this statistical analysis is that the difference between each task difficulty level (e.g., impossible to difficult) is equivalent.
Table 2.
FLORA Ease of Task Results: Mean Difference (Device On - Off) at Endpoint
| End Point | |||||||
|---|---|---|---|---|---|---|---|
| Task Number | Domain | Task | Subjects | Range Device Off | Range Device On | Mean Difference | P Value* |
| 1 | Visual orientation | Locate lights in the environment | 3 | [2,3] | [3,4] | 0.7 | 0.157 |
| 2 | Visual orientation | Visually find doorways | 3 | [1,2] | [3,4] | 2.0 | 0.083 |
| 3 | Visual orientation | Use light from windows to determine orientation | 3 | [2,4] | [4,4] | 1.0 | 0.166 |
| 4 | Visual orientation | Use artificial light to determine orientation | 1 | [1,1] | [3,3] | 2.0 | 0.317 |
| 5 | Visual orientation | Use the sun to determine orientation | 0 | ||||
| 6 | Visual orientation | Recognize and use shapes for orientation and environmental information | 2 | [1,2] | [3,3] | 1.7 | 0.180 |
| 7 | Visual Mobility | Independently cross residential streets by following the lines of a crosswalk | 0 | ||||
| 8 | Visual Mobility | Avoid obstacles while walking | 3 | [2,4] | [3,3] | 0.0 | 1.000 |
| 9 | Visual Mobility | Estimate the size of an obstacle | 3 | [2,3] | [2,3] | 0.3 | 0.564 |
| 10 | Visual Mobility | Avoid low-hanging branches, plants, head-high shelves, etc. | 2 | [1,2] | [2,2] | 0.5 | 0.317 |
| 11 | Visual Mobility | Detect curbs | 3 | [3,4] | [3,4] | 0.0 | 1.000 |
| 12 | Daily life | Determine whether room lights are on or off | 3 | [2,2] | [2,3] | 0.3 | 0.317 |
| 13 | Daily life | Locate ordinary objects at various distances (familiar environment) | 3 | [2,3] | [3,4] | 0.7 | 0.317 |
| 14 | Daily life | Visually locate a place setting on a dining table | 3 | [1,1] | [3,4] | 2.3 | 0.102 |
| 15 | Daily life | Visually locate/identify things in the bathroom (familiar environment) | 3 | [1,1] | [2,4] | 2.0 | 0.109 |
| 16 | Daily life | Visually locate/identify things in the bathroom (unfamiliar environment) | 3 | [1,1] | [2,4] | 2.0 | 0.109 |
| 17 | Daily life | Visually locate dishes while washing | 3 | [1,1] | [2,3] | 1.7 | 0.102 |
| 18 | Daily life | Visually locate clothes | 3 | [1,1] | [2,3] | 1.7 | 0.102 |
| 19 | Daily life | Visually find pots/pans/utensils in the kitchen | 3 | [1,1] | [2,4] | 2.0 | 0.109 |
| 20 | Daily life | Sort light from dark laundry | 3 | [1,1] | [2,3] | 1.7 | 0.102 |
| 21 | Daily life | Travel within home independently | 3 | [4,4] | [4,4] | 0.0 | 1.000 |
| 22 | Daily life | Identify top step/bottom step | 3 | [4,4] | [4,4] | 0.0 | 1.000 |
| 23 | Daily life | Negotiate stairways independently | 3 | [4,4] | [4,4] | 0.0 | 1.000 |
| 24 | Daily life | Cut/chop food | 0 | ||||
| 25 | Daily life | Identify ordinary objects at various distances | 3 | [2,3] | [3,4] | 1.0 | 0.166 |
| 26 | Daily life | Visually identify food on a plate | 0 | ||||
| 27 | Daily life | Heat/reheat food | 0 | ||||
| 28 | Daily life | Maintain safety: falls/spills/burns | 3 | [3,4] | [3,4] | 0.0 | 1.000 |
| 29 | Interaction with others | Visually locate people in a non-crowded setting | 3 | [1,2] | [3,4] | 2.3 | 0.102 |
| 30 | Interaction with others | Determine when people walk by | 2 | [3,3] | [3,4] | 0.5 | 0.317 |
| 31 | Interaction with others | Detect the approach of another person | 3 | [2,3] | [3,4] | 0.7 | 0.157 |
| 32 | Interaction with others | Determine the direction of movement of people walking by | 3 | [2,3] | [2,4] | 0.3 | 0.317 |
| 33 | Interaction with others | Track another person | 3 | [1,3] | [2,4] | 0.7 | 0.157 |
| 34 | Interaction with others | Visually locate people in a crowded setting | 1 | [1,1] | [1,1] | 0.0 | 1.000 |
| 35 | Interaction with others | Determine direction another person is facing | 0 | ||||
Impossible = 1, Difficult = 2, Moderate = 3, Easy = 4. The difference between Mean ON and OFF score is provided, with a positive score representing an improvement in function.
P value from Wilcoxon's matched-pairs signed-rank test.
FLORA—Anecdotal Experiences
Subjects reported their anecdotal experiences with the device over the two years of the trial. All subjects were able to use the device to localize the presence of light and detect whether a lightbulb was on or off. Table 3 tabulates these anecdotal experiences, which were responses from the self-report questions in Part 2 of the FLORA. Identifying real-life objects in the local environment, increased motivation, and engaging in social interactions were common themes.
Table 3.
Subjects’ Responses to Self-Report Questions
| Subject | Weeks After Device Fitting | Activities Performed, Objects Seen, and Comments Made |
|---|---|---|
| S1 | 17 | More energetic, happy, and positive |
| Increased motivation | ||
| Not bumping into things like trees* (Week 32) | ||
| 20 | Increased confidence | |
| 32 | Identifying traffic lights, cars, people, trees, and poles on the street | |
| Increased independence | ||
| 44 | Identifying wood and machines in woodwork class | |
| Identifying car on driveway | ||
| Does not need assistance to travel to the supermarket | ||
| Identifying people in woodwork class* (Week 56) | ||
| 56 | “Like another cane” | |
| Lining up with pole on road crossing | ||
| Identifying hammer in woodwork class | ||
| 68 | Less help/assistance when going on walks in the park | |
| Explore shopping center/hardware store | ||
| Flashes of objects are better when it is sunny | ||
| Finding traffic lights/trees/poles/cars | ||
| 110 | Identifying rubbish bin | |
| Identifying trees and poles on street | ||
| Finding letterbox outside | ||
| S2 | 17 | Doors in train show up brighter |
| Less need for shore-lining with cane in shopping centers | ||
| 20 | Identifying doorways at train station | |
| Confusion with shadows | ||
| Able to see some shop fronts and seats | ||
| 32 | Identify trees, poles, lamp posts | |
| ‘Flashes’ when nothing is there | ||
| Can locate things on tables in cafes | ||
| Navigating past photocopier, cash register, and café at work* (week 44, week 56) | ||
| 44 | Used it to supplement information in the theatre (foyer and scanning the crowd) | |
| Located bins, parked cars* (week 68) | ||
| Increased awareness of the space | ||
| Increased confidence | ||
| 56 | Confirming information in familiar environments | |
| Uses device inside to locate items on table | ||
| Uses at theatre to get a feel for surrounding space | ||
| 68 | Identify people moving in the foyer | |
| Filling in gaps with familiar information | ||
| 109 | Adds to information provided by cane | |
| Uses cane to confirm what the “flashes” are | ||
| Device more effective on tabletop | ||
| S3 | 17 | Avoiding contact with clothesline in backyard |
| Finding clothesline pegs | ||
| Finding bus stop | ||
| 20 | Different to usual trying to find phosphenes | |
| 32 | Identifying face in mirror | |
| Locating spouse in café | ||
| Avoiding walking into doorways at home* (week 44) | ||
| Walking around the house more confidently – not swerving and more confident in movement* (week 68) | ||
| Increased tendency to explore new environments* (week 56) | ||
| Confidence improved* (week 80) | ||
| 44 | Identified clutter at friend's place | |
| 56 | More confidence | |
| Identifying when someone leaves a chair from a sitting position | ||
| 68 | Identifying letterbox | |
| Using device concurrently with tactile sensation inside | ||
| Awareness of trees outside | ||
| Less asking around to know where they are in an unfamiliar environment | ||
| Increased shadow detection | ||
| 80 | Making eye contact with students in classroom | |
| Getting an idea of classroom size | ||
| Able to do beachfront walk | ||
| Familiarity overrides device | ||
| Device enhances current knowledge | ||
| 92 | Identifying people walking across train station | |
| Locate car in driveway at home inside | ||
| 136 | Identified and picked up a card on the floor of home | |
| S4 | 17 | Increased motivation |
| 20 | Detecting poles and signage on the street | |
| Differentiate nature strip (verge) from the park inside | ||
| Identifying door/light objects/desk items |
Indicates comments made at multiple time points. Later time points are indicated in parentheses.
FLORA—Impact on Life and Well-Being
The independent examiner categorized the narrative provided by the O&M assessor in Part 3 of the FLORA for each subject, confirming an overall “positive effect” of the retinal prosthesis on daily life for all subjects at all time points, with the sole exception of one “neutral effect” recorded for one subject (subject 3) at week 20. A “positive effect” score indicated a self-report of an improvement in well-being or functional vision that the independent O&M specialist was able to confirm during observation. The single neutral experience occurred during early visual rehabilitation when the subject was still adapting to using the device as an adjunct to their usual navigation strategies.
IVI-VLV
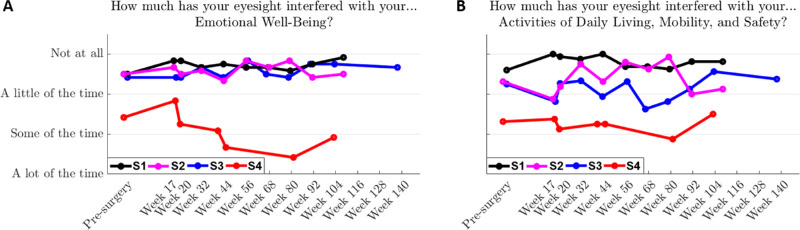
For the emotional well-being component of the IVI-VLV, scores for subjects 1, 2, and 3 were stable over the two years and did not differ from before surgery, whereas there was a decrease for subject 4 (Fig. 5). An independent psychologist worked with this subject to address psychosocial stressors that were not study related. Scores for subjects 1, 2, and 3 suggested they were well adjusted to their vision loss, with the impact of vision loss on activities of daily living, mobility, and safety essentially ranging from “a little of the time” to “not at all” (Fig. 5).
Figure 5.
IVI-VLV results relating to emotional well-being (A) and activities of daily living (B). Data shows that emotional well-being and activities of daily living scores remain stable over the two-year clinical trial for subjects 1, 2, and 3. For subject 4, emotional well-being decreased over time because of psychosocial stressors unrelated to the study.
Discussion
The principal finding was that subjects with late-stage RP implanted with the second-generation suprachoroidal retinal prosthesis demonstrated improved ease of task scores in the FLORA instrument over the 2 years of the study with the device ON relative to device OFF, and relative to pre-surgical baseline and post-fitting baseline (week 17). Furthermore, an overall “positive effect” of the device on daily life in all three subjects with complete longitudinal data was found at all time-points with only one exception (overall “neutral effect” in subject 3 at week 20). The combined quantitative and qualitative data suggests the suprachoroidal device provides real-world benefit. The positive impacts of the device in activities of daily living are similar to those reported in studies with the FLORA instrument in Argus II patients18,19 and with the Modified Turano Independent Mobility Questionnaire in Alpha AMS patients.23 Hence, our real-world assessment of the suprachoroidal retinal prosthesis with the FLORA tool supports our interim laboratory-based orientation and mobility results showing that device ON performs better than the device OFF in high-contrast indoor conditions (Kolic M. et al., IOVS, 2021, 62, ARVO E-Abstract).
Improvement of ease of task scores over time with the device ON, primarily occurred between week 17 (post-fitting baseline) and week 44 (i.e., a period of 27 weeks or six months; Figs. 2A and 3A) and was accompanied by minimal changes with device OFF suggesting a positive effect of visual rehabilitation. The subjects became increasingly proficient at using and interpreting the phosphenes produced by the device in this time, with the learning effect because of ongoing visual rehabilitation training and practice at home. In Argus II users, the post-approval study measured FLORA at baseline, 1 year, and 2 years. They hypothesized that the improvement in FLORA between baseline and one year was due to visual rehabilitation but were unable to determine the learning effect timeframe. Other measurements of visual outcomes with the Argus II, though, have indicated a critical learning period of a few months, after which performance plateaus.28,29 For the Alpha AMS device, the Modified Turano Independent Mobility Questionnaire results showed a significant improvement in activities of daily living at two months after implantation, compared to preimplantation baseline.23 They did not have longitudinal data to comment on the time period of the visual rehabilitation learning effect.
Our study found greatest improvement in the “Daily Life” domain (Fig. 3), and selective improvement in the “Visual Orientation,” “Visual Mobility,” and “Interaction with Others” domains (Fig. 2). In comparison, the Argus II longitudinal FLORA findings19 found similar levels of improvement between the “Visual Orientation,” “Visual Mobility,” and “Daily Life” domains (67%, 80%, 58% improvement from baseline, respectively), and minimal improvement in the “Interaction with Others” domain (14%). The Alpha AMS device cannot be directly compared, as the tool to measure activities of daily living was different. However, they did report improvements in ease of task scores across a broad range of activities after two months of implantation.23
It was not expected that the “Daily Life” domain would show the greatest improvement with device ON relative to OFF, as many tasks in the “Daily Life” domain were familiar and commonly performed. For instance, in task 13, location of ordinary objects such as windows and tables at various distances relies heavily on memory. These tasks could have been completed with residual vision (light perception), because the suprachoroidal device does not obstruct incidental light, and the retinal prosthesis was implanted in the “worse-seeing” eye, so the “better” eye may assist. Nonetheless, the data clearly showed a benefit with the device ON, making common and simple tasks even easier to complete, and aligning with the Argus II findings for task 13.19 The overall finding for the “Daily Life” domain suggests that the addition of extra visual information to other senses such as touch and proprioception made completing functional vision tasks in the real world easier.
Although visually locating objects within a familiar environment (their house) was greatly improved with the device ON (tasks 13–19), traveling independently within the home (task 21) was generally easy both with the device ON and OFF. However, anecdotal data did provide further information, with a family member of one subject remarking they were walking around the house more confidently and unwaveringly with the device ON. Two further tasks in the “Daily Life” domain (Task 22, identify top step/bottom step, and Task 23, negotiate stairways independently) were also already “easy” with the device OFF and had no additional benefit with the device ON. This agrees with the Argus II studies,18,19 where two of these three tasks were actually found to be easier with device OFF (travel within home independently, identify top step/bottom step) in the initial study. Notably, for the Alpha AMS data, the activity of daily living that was most positively affected by the implant was reported to be “walking in familiar areas.”23 However, it is hard to make a direct comparison of navigation outcomes in familiar environments using different testing tools.
Within the “Daily Life” domain, tasks with a greater reliance on vision than other senses (i.e., Tasks 14–20, including visually locating a place setting on a dining table, locating objects in the house, sorting laundry, identifying people in a non-crowded setting) showed the greatest overall improvement at study end point (Figs. 2 and 3). There was a dramatic improvement in Task 20 (sorting light from dark laundry) with the device ON after week 44, that was also found with the Argus II device.18,19
Interestingly, unlike the Argus II studies,18,19 tasks in the “Visual Mobility” domain centering on the subjects’ ability to use vision to detect obstacles showed minimal increase in performance with the device ON. This may be because, even with device OFF, three of five tasks (independently cross residential streets by following the lines of a crosswalk, avoid obstacles while walking, detect curbs) are “moderate” to “easy” to perform with usual O&M strategies. It may also be due to the subjects’ difficulty in differentiating between shadows and actual objects with the current visual processing system, especially outside where ambient light levels vary. A separate study in the same cohort demonstrated improved performance in a high-contract obstacle avoidance task using the device without traditional navigation aids (Kolic M. et al., IOVS, 2021, 62, ARVO E-Abstract). The research team is currently working on development in the vision processing algorithms to improve object discrimination and remove background clutter such as shadows (Walker JG et al., IOVS, 2020, 61, ARVO E-Abstract).
Performance in the “Interaction with Others” domain was improved with the device ON for a number of tasks. Task 29 (Visually locate people in a noncrowded setting) was noticeably improved with the device ON, as also seen in the previous Argus II studies.18,19 Our quantitative data is supported by anecdotal reports such as “locating spouse in a café,” “identifying people leaving from a sitting position,” and “identifying people in woodwork class” (Table 3). Only modest benefits were found with the device ON compared to OFF for Tasks 30 through 33 (determine when people walk by, determine the direction of movement of people walking by, detect the approach of another person, track another person) because these tasks can be performed with auditory skills. Nevertheless, this modest improvement may be due to the device, because a previous study with the Argus II prosthesis showed that subjects were able to identify the direction of person walking in their field of view, despite every effort to remove auditory cues.16
Improvement in the “Visual Orientation” domain was also limited to select tasks. The most dramatic improvements were seen in Task 2 and Task 6, where subjects were required to “visually find doorways” and “recognize and use shapes for orientation and environmental information,” respectively. With respect to the improvement in Task 6, subject anecdotes (Table 3) such as “Navigating past photocopier, cash register, and café at work” and “locating bins and parked cars” corroborate this.
There were three tasks where performance was better with Device OFF at pre-surgery baseline than at the week 17 post-fitting baseline; “determine direction another person is facing,” “track another person,” and “independently cross residential streets at a crosswalk” (Fig. 2). One reason is that there was likely a small learning effect in how the independent O&M examiner assessed the FLORA, given that the FLORA grading scheme is not used in clinical practice. This effect was minimized by training and preparation and seems resolved by week 20. Another reason is that the subjects were able to use nonvisual cues including auditory and tactile inputs; however, environmental conditions and, hence, performance can vary over time. For example, the ease of “tracking another person” or determining the “direction another person is facing” with Device OFF depends on how evident the auditory cues were on a given day. Furthermore, because of differences in road crossing markings and distances and that different crossings were used over time, the O&M techniques for road crossing with device OFF are likely to vary.
Self-reported vision-related quality of life was monitored using the IVI-VLV instrument, designed specifically for use in people with very low vision.27 The results cannot be compared directly to the Argus II study, because improvements in quality of life for Argus II recipients were assessed using the Vision and Quality of Life Index.30 However, both the Argus II device recipients assessed with the Vision and Quality of Life Index 31 and the suprachoroidal device recipients assessed with the IVI-VLV in the current study found that device implantation or usage did not impact on general emotional well-being.
A main limitation of this study was the low number of subjects, being primarily a safety study. Furthermore, there was an inability to complete certain tasks at all time points because of various factors (inappropriate environment to complete the task, timing constraints or subject fatigue). Another limitation was the inability to mask either the subject or the O&M assessor as to the status of the device (ON or OFF). Although it is possible to provide “scrambled” visual input to prosthesis recipients while completing seated tasks,24 to mask them to the correct “device ON” trials, this is not ethical in mobility trials for safety reasons. However, we did endeavor to routinely test device ON first, so that any bias in the data because of task familiarity would be toward device OFF, as described in the Argus II post-approval study.19 Inability to mask phosphene perception may also result in bias within the anecdotal data. There may also be learning effects in device OFF data because of use of the same tasks repeatedly over time, which may explain the mild Improvement in the “Interaction with Others” domain after week 56, or otherwise Improvement in base O&M skills. The same O&M specialist trained the subjects in adjunct use of the device in their home environs in addition to FLORA assessments, which may have encouraged confirmation bias. Another limitation is the use of a single O&M specialist with no interobserver agreement determined. Furthermore, the FLORA is currently a non-standardized assessment, although the creators have indicated they would like to standardize the task list for direct cross-comparison between different treatment trials. Despite study limitations, the subjects were all implanted monocularly in the “worse-seeing” eye, and testing was performed with both eyes open and with usual aids, so Improvement with the device ON is indicative of the real-world effects of the system.
When compared to laboratory-based tests,24 the FLORA has the advantage that it is directly assessing functional vision in the subjects’ own unique home and environment. The testing is performed using real items and local navigational routes. Subjects were able to practice localization, identification, and navigation with their device ON between FLORA assessments and get feedback from family members, an important part of visual rehabilitation. However, the weakness of FLORA assessment is the higher degree of variability because of lack of standardization of the lighting, contrast, amount of “clutter” in the environment, and size of objects/items, compared to well-controlled laboratory-based tasks. Because of local variations, the tasks performed by each subject may have different inherent difficulty. No standardized items were used (except for the laundry task); however, often subjects had high-contrast objects in the home already. For example, all subjects had a dark bench/table with light-colored mugs, bowls, plates, and chopping boards. For the laundry task, we provided each subject with a matching set of white and black laundry (socks and singlets) to minimize intrusion. The subjects did not move house during the trial and used the same household items over time; hence, object contrast was maintained indoors. However, the navigational routes outside differed over time, because of fatigue, time and weather conditions. However, on a given day the same route was taken so the comparison within each subject for device ON and OFF was standardized.
The quantitative results and anecdotal report in this study support the use of the suprachoroidal retinal prosthesis for end-stage RP patients in real-world settings. It is clear that even a small increment to the visual sense improves day-to-day O&M outcomes and has a positive effect on daily life. Use of the device in conjunction with current mobility aids provides extra information about surroundings that subjects report as useful. Further development of advanced vision processing software to differentiate between objects and backgrounds in low contrast settings could improve mobility, particularly in outdoor settings where shadows can interfere with object detection. Future research should focus on testing a larger number of subjects to gain statistically significant results. It will also be of interest to determine real-world outcomes with the device in patients who have higher baseline visual function than simple light perception, such as those with hand-motion vision.
Acknowledgments
The authors thank Second Sight Medical Products for providing and allowing academic use of the FLORA instrument.
Supported by Australian National Health and Medical Research grant no. 1082358 to P.J. Allen, L.N. Ayton, and M.A. Petoe. Additional funding support from Bionic Vision Technologies. The Bionics Institute and the Centre for Eye Research Australia acknowledge the support of the Victorian Government through its Operational Infrastructure Support Program.
Disclosure: L. Karapanos, None; C.J. Abbott, BVT (F), BVT (R); L.N. Ayton, None; M. Kolic, BVT (F), BVT (R); M.B. McGuinness, None; E.K. Baglin, BVT (F), BVT (R); S.A. Titchener, BVT (F); J. Kvansakul, None; D. Johnson, None; W.G. Kentler, None; N. Barnes, Data61 (P), BVT (F); D.A.X. Nayagam, Bionics Institute (P), BVT (F); P.J. Allen, CERA (P), BVT (F); M.A. Petoe, Bionics Institute (P), BVT (F), BVT (R)
References
- 1.Humayun MS, de Juan E Jr., Dagnelie G. The Bionic Eye: A Quarter Century of Retinal Prosthesis Research and Development. Ophthalmology .2016; 123: S89–S97. [DOI] [PubMed] [Google Scholar]
- 2.Hartong DT, Berson EL, Dryja TP.. Retinitis pigmentosa. Lancet. 2006; 368: 1795–1809. [DOI] [PubMed] [Google Scholar]
- 3. RetNet: Genes and Mapped Loci Causing Retinal Diseases. Available at: https://sph.uth.edu/retnet/disease.htm . Accessed January 24, 2021.
- 4.Wang AL, Knight DK, Vu T-TT, et al.. Retinitis Pigmentosa: Review of Current Treatment. Int Ophthalmol Clin .2019; 59: 263–280. [DOI] [PubMed] [Google Scholar]
- 5.Dias MF, Joo K, Kemp JA, et al.. Molecular genetics and emerging therapies for retinitis pigmentosa: basic research and clinical perspectives. Prog Retin Eye Res .2018; 63: 107–131. [DOI] [PubMed] [Google Scholar]
- 6.Ayton LN, Barnes N, Dagnelie G, et al.. An update on retinal prostheses. Clin Neurophysiol .2019; 131: 1383–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bloch E, Luo Y, da Cruz L.. Advances in retinal prosthesis systems. Ther Adv Ophthalmol .2019; 11: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinclair NC, Shivdasani MN, Perera T, et al.. The appearance of phosphenes elicited using a suprachoroidal retinal prosthesis. Invest Ophthalmol Vis Sci .2016; 57: 4948–4961. [DOI] [PubMed] [Google Scholar]
- 9.Cheng DL, Greenberg PB, Borton DA.. Advances in retinal prosthetic research: A systematic review of engineering and clinical characteristics of current prosthetic initiatives. Curr Eye Res .2017; 42: 334–347. [DOI] [PubMed] [Google Scholar]
- 10.Saunders AL, Williams CE, Heriot W, et al.. Development of a surgical procedure for implantation of a prototype suprachoroidal retinal prosthesis. Clin Exp Ophthalmol .2014; 42: 665–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ayton LN, Blamey PJ, Guymer RH, et al.. First-in-human trial of a novel suprachoroidal retinal prosthesis. PLoS One .2014; 9: e115239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes N, Scott AF, Lieby P, et al.. Vision function testing for a suprachoroidal retinal prosthesis: effects of image filtering. J Neural Eng .2016; 13: 036013. [DOI] [PubMed] [Google Scholar]
- 13.Petoe MA, McCarthy CD, Shivdasani MN, et al.. Determining the contribution of retinotopic discrimination to localization performance with a suprachoroidal retinal prosthesis. Invest Ophthalmol Vis Sci .2017; 58: 3231–3239. [DOI] [PubMed] [Google Scholar]
- 14.Shivdasani MN, Sinclair NC, Gillespie LN, et al.. Identification of characters and localization of images using direct multiple-electrode stimulation with a suprachoroidal retinal prosthesis. Invest Ophthalmol Vis Sci .2017; 58: 3962–3974. [DOI] [PubMed] [Google Scholar]
- 15.Abbott CJ, Nayagam DA, Luu CD, et al.. Safety studies for a 44-channel suprachoroidal retinal prosthesis: a chronic passive study. Invest Ophthalmol Vis Sci .2018; 59: 1410–1424. [DOI] [PubMed] [Google Scholar]
- 16.Dagnelie G, Christopher P, Arditi A, et al.. Performance of real-world functional vision tasks by blind subjects improves after implantation with the Argus II retinal prosthesis system. Clin Exp Ophthalmol .2017; 45: 152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geruschat DR, Flax M, Tanna N, et al.. FLORA: Phase I development of a functional vision assessment for prosthetic vision users. Clin Exp Optom .2015; 98: 342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geruschat DR, Richards TP, Arditi A, et al.. An analysis of observer-rated functional vision in patients implanted with the Argus II Retinal Prosthesis System at three years. Clin Exp Optom .2016; 99: 227–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delyfer MN, Gaucher D, Mohand-Saïd S, et al.. Improved performance and safety from Argus II retinal prosthesis post-approval study in France [published online ahead of print December 23, 2020]. Acta Ophthalmol , 10.1111/aos.14728. [DOI] [PubMed] [Google Scholar]
- 20.Yoon YH, Humayun M, Kim YJ.. One-year anatomical and functional outcomes of the Argus II implantation in Korean patients with late-stage retinitis pigmentosa: a prospective case series study [published online ahead of print December 4, 2020]. Ophthalmologica , 10.1159/000513585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho AC, Humayun MS, Dorn JD, et al.. Long-term results from an epiretinal prosthesis to restore sight to the blind. Ophthalmology .2015; 122: 1547–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stingl K, Bartz-Schmidt KU, Besch D, et al.. Subretinal Visual Implant Alpha IMS—clinical trial interim report. Vision Res .2015; 111: 149–160. [DOI] [PubMed] [Google Scholar]
- 23.Edwards TL, Cottriall CL, Xue K, et al.. Assessment of the electronic retinal implant alpha AMS in restoring vision to blind patients with end-stage retinitis pigmentosa. Ophthalmology .2018; 125: 432–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayton LN, Rizzo JF, Bailey IL, et al.. Harmonization of outcomes and vision endpoints in vision restoration trials: recommendations from the international HOVER taskforce. Transl Vis Sci Technol .2020; 9: 25–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brady-Simmons C, Van Der Biest R, Bozeman L.. Miami Lighthouse for the Blind and Visually Impaired Case Study: vision rehabilitation for the first Florida resident to receive the Argus II “Bionic Eye.” J Vis Impair Blind .2016; 110: 177–181. [Google Scholar]
- 26.Titchener SA, Kvansakul J, Shivdasani MN, et al.. Oculomotor responses to dynamic stimuli in a 44-channel suprachoroidal retinal prosthesis. Transl Vis Sci Technol .2020; 9: 31–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finger RP, Tellis B, Crewe J, et al.. Developing the impact of Vision Impairment-Very Low Vision (IVI-VLV) questionnaire as part of the LoVADA protocol. Invest Ophthalmol Vis Sci .2014; 55: 6150–6158. [DOI] [PubMed] [Google Scholar]
- 28.da Cruz L, Coley BF, Dorn J, et al.. The Argus II epiretinal prosthesis system allows letter and word reading and long-term function in patients with profound vision loss. Br J Ophthalmol .2013; 97: 632–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghodasra DH, Chen A, Arevalo JF, et al.. Worldwide Argus II implantation: recommendations to optimize patient outcomes. BMC Ophthalmol .2016; 16: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Misajon R, Hawthorne G, Richardson J, et al.. Vision and quality of life: the development of a utility measure. Invest Ophthalmol Vis Sci .2005; 46: 4007–4015. [DOI] [PubMed] [Google Scholar]
- 31.Duncan JL, Richards TP, Arditi A, et al.. Improvements in vision-related quality of life in blind patients implanted with the Argus II Epiretinal Prosthesis. Clin Exp Optom .2017; 100: 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]