Abstract
Background: Invasive procedures are a core aspect of pulmonary and critical care practice. Procedures performed in the intensive care unit can be divided into high-risk, low-volume (HRLV) procedures and low-risk, high-volume (LRHV) procedures. HRLV procedures include cricothyroidotomy, pericardiocentesis, Blakemore tube placement, and bronchial blocker placement. LRHV procedures include arterial line placement, central venous catheter placement, thoracentesis, and flexible bronchoscopy. Despite the frequency and importance of procedures in critical care medicine, little is known about the similarities and differences in procedural training between different Pulmonary and Critical Care Medicine (PCCM) and Critical Care Medicine (CCM) training programs. Furthermore, differences in procedural training practices for HRLV and LRHV procedures have not previously been described.
Objective: To assess procedural training practices in PCCM and CCM fellowship programs in the United States, and compare differences in training between HRLV and LRHV procedures.
Methods: A novel survey instrument was developed and disseminated to PCCM and CCM program directors and associate program directors at PCCM and CCM fellowship programs in the United States to assess procedural teaching practices for HRLV and LRHV procedures.
Results: The survey was sent to 221 fellowship programs, 168 PCCM and 34 CCM, with 70 unique respondents (31.7% response rate). Of the procedural educational strategies assessed, each strategy was used significantly more frequently for LRHV versus HRLV procedures. The majority of respondents (51.1%) report having no dedicated training for HRLV procedures versus 6.9% reporting no dedicated training for any LRHV procedure (P < 0.001). For HRLV procedures, 76.9% of respondents indicated that there was no set number of procedures required to determine competency, versus 25.3% for LRHV procedures (P < 0.001). For LRHV procedures, fellows were allowed to perform procedures independently without supervision 21.7% of the time versus 3.9% for HRLV procedures (P = 0.004). Program directors’ confidence in their ability to determine fellows’ competence in performing procedures was significantly lower for HRLV versus LRHV versus HRLV procedures (P < 0.001).
Conclusion: Significant differences exist in procedural training education for PCCM and CCM fellows for LRHV versus HRLV procedures, and awareness of this discrepancy presents an opportunity to address this educational gap in PCCM and CCM fellowship training.
Keywords: graduate medical education, critical care, teaching, risk evaluation and mitigation
Performing invasive procedures is a core aspect of pulmonary and critical care practice, and trainees learn foundational procedural skills during residency and fellowship training. Although most residency training programs provide instruction in some invasive procedures, such as central venous catheter (CVC) placement, this is no longer a requirement by the American Board of Internal Medicine (1). More advanced procedural teaching occurs during Pulmonary and Critical Care Medicine (PCCM) and Critical Care Medicine (CCM) fellowship training.
During PCCM and CCM fellowship training, trainees are expected to become competent in invasive procedures common to clinical practice. For certain procedures, the American College of Graduate Medicine Education has set a required minimum number to be completed during fellowship training to indicate experience and competence. For example, CCM and PCCM fellows must complete at least 50 and 100 bronchoscopies, respectively, during fellowship (2). For many other technical skills, the American College of Graduate Medicine Education, rather than mandating a minimum number of procedures, expects fellowship clinical competency committees to assess fellows’ procedural competence (3).
The variability in frequency and risk of certain procedures provides an additional challenge to procedural instruction and competency assessment in PCCM and CCM fellowship training. Procedures performed by fellows during PCCM or CCM training can be considered to be either low-risk, high-volume (LRHV) procedures or high-risk, low-volume (HRLV) procedures.
Examples of LRHV procedures include arterial line placement, CVC placement, flexible bronchoscopy, and thoracentesis. For these LRHV procedures, the risk of complications or adverse outcomes is decreased because of the increased frequency of procedural training, practice, and familiarity (4–6). Furthermore, there are more opportunities for longitudinal competency assessment in these procedures. Guidelines are lacking, however, regarding the nature and volume of training for other procedures that occur less frequently in clinical practice.
Procedures such as Sengstaken-Blakemore tube placement, bronchial blocker placement, cricothyroidotomy, or pericardiocentesis occur infrequently in PCCM and CCM training and practice but are potentially life-saving interventions and a component of critical care medicine (7, 8). In the absence of guidance from accrediting organizations or professional societies, it is unknown how PCCM and CCM fellowship programs teach fellows to perform HRLV procedures, or how best to assess competency in performing these procedures. Furthermore, although procedural training methods have been previously assessed in internal medical residency programs (9, 10) and in systematic reviews encompassing all trainees (11, 12), specific assessments of PCCM and CCM procedural training practices are lacking.
To better understand how specific HRLV and LRHV procedures are taught in PCCM and CCM fellowship programs, we performed a nationwide survey of fellowship program directors (PDs) and associate PDs (APDs).
Methods
Given the lack of existing instruments to assess the type and content of procedural teaching in PCCM fellowship training, we developed a novel survey tool to facilitate data collection. The authors’ background in medical education, as well as input from medical educators involved in both general fellowship education as well as procedural teaching, was used to develop the survey items and response options using established best practices in survey design (13, 14). The survey was iteratively reviewed by the authors until consensus regarding the content and organization of items was achieved. Subsequently, pretesting, using a think-out-loud approach, was performed with a cohort of representative respondents to assess for item clarity and understanding of the survey items and response options. Major modifications were incorporated into the survey instrument, and pretesting was repeated to reassess clarity and understanding (15). After the second round of pretesting, saturation was achieved, and the survey underwent pilot testing to assess technical issues related to the dissemination platform.
Qualtrics was used to distribute the survey. The survey was disseminated through the listserv of PDs and APDs maintained by the Association of PCCM PDs. The survey was sent to potential respondents with a subsequent follow-up reminder e-mail over a 4-week period. The potential risks and benefits of completing the survey were delineated in the invitation e-mail, and consent to participate was indicated by clicking the invitation link to access the survey.
The primary outcomes were the descriptive characteristics of the type and timing of procedural training for PCCM and CCM fellows. Specifically, the pedagogic methods for procedural training were assessed, as were methods by which fellowship programs determine fellows’ competency in performing procedures. The programs’ requirements for procedural supervision were also assessed.
For comparative analyses, individual procedures were categorized as either HRLV or LRHV procedures as determined by the consensus of the study authors. Given the absence of preexisting descriptions or categorization of HRLV or LRHV procedures, the authors identified and categorized procedures as HRLV or LRHV by consensus agreement based on collective clinical experience. HRLV procedures included bronchial blocker placement, cricothyroidotomy, Blakemore or Minnesota tube placement, and pericardiocentesis. LRHV procedures included arterial line placement, CVC placement, thoracentesis, and flexible bronchoscopy.
We compared differences in procedural education between HRLV and LRHV procedures. Specifically, PDs and APDs were asked whether fellows underwent procedural training before performing the procedure on a patient as compared with receiving training at some point during fellowship training independent of patient contact. To assess when fellows receive procedural training for LRHV and HRLV procedures, respondents indicated whether fellows were trained before and/or after actually performing the procedure on a patient (respondents could select either or both options). Respondents were also asked about the minimum number of procedures defined as necessary to demonstrate procedural competence. PDs’ and APDs’ confidence that their program accurately determines fellows’ competence in performing procedures was also assessed.
Statistical Analyses
After completion of data acquisition, results were exported to Microsoft Excel (Microsoft), organized, and visually inspected. Descriptive statistics were determined for clinical data with mean and standard deviation reported for continuous variables and number and percentages for categorical variables. For comparative analyses, the distribution of survey responses was determined to be nonparametric, and Fischer’s exact test was used to assess for differences between variables of interest. The survey data were exported to JMP Pro version 14.0 (SAS Institute) for comparative analyses. A P < 0.05 was considered to be significant for all comparative analyses.
Institutional review board evaluation was obtained through the National Institutes of Health, and the study was determined to be exempt.
Results
The survey was sent to 221 fellowship programs, 168 PCCM and 34 CCM, with 70 unique respondents (31.7% response rate). The majority of respondents (81.4%) were from PCCM only fellowship programs (see Table 1). The majority of respondents were PDs (64.3%), primarily from academic medical centers (82.9%), with a heterogeneous geographic distribution throughout the United States and a range of fellowship program sizes.
Table 1.
Characteristics of survey respondents and fellowship programs
| Respondent or Fellowship Program Characteristic | Number (%) |
|---|---|
| Type of fellowship program | |
| PCCM | 57 (81.4) |
| CCM | 5 (7.1) |
| Both PCCM and CCM | 8 (11.4) |
| Role in a fellowship program | |
| PD | 45 (64.3) |
| APD | 25 (35.7) |
| Type of medical center | |
| Academic medical center | 58 (82.6) |
| Mixed or hybrid medical center (20) | 10 (14.3) |
| Community medical center | 2 (2.9) |
| Location of fellowship program | |
| Mid-Atlantic | 7 (10.0) |
| Midwest | 13 (18.6) |
| Mountain | 1 (1.4) |
| Northeast | 24 (34.3) |
| Northwest | 1 (1.4) |
| South | 9 (12.9) |
| Southeast | 10 (7.0) |
| Southwest | 1 (1.4) |
| West | 4 (5.7) |
| City size (population) in which fellowship program is located | |
| >500,000 | 45 (64.3) |
| 200,000–500,000 | 14 (20.0) |
| 100,000–200,000 | 10 (14.3) |
| Rural (<100,000) | 1 (1.4) |
| Size of fellowship program (number of fellows) | |
| 1–5 | 4 (5.7) |
| 6–10 | 20 (28.6) |
| 11–15 | 23 (32.9) |
| >15 | 23 (32.9) |
| Prefellowship residency training* | |
| Internal Medicine residency | 68 (97.1) |
| Other Internal Medicine subspecialty fellowship | 23 (32.9) |
| Emergency Medicine residency | 21 (30.0) |
| Other | 2 (2.9) |
Definition of abbreviations: APD = associate program director; CCM = critical care medicine; PCCM = pulmonary and CCM; PD = program director.
The percentage total for prefellowship residency training is greater than 100%, as respondents could select multiple options.
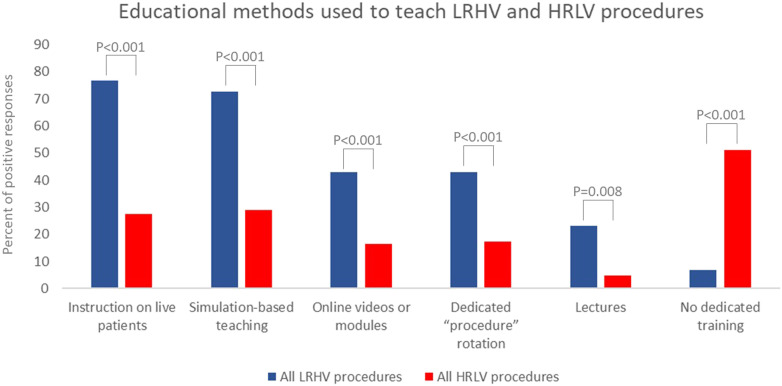
Significant variability existed between programs for type and timing of procedural training for fellows. As demonstrated in Table 2 and Figure 1, fellowship programs engage in a variety of educational interventions for procedural training, with significant differences in the frequency with which procedural teaching methods are used for LRHV procedures as compared with HRLV procedures. Every procedural educational strategy is used significantly more frequently for LRHV procedures, whereas the majority of respondents (51.1%) report having no dedicated training for HRLV procedures versus only 6.9% reporting no dedicated training for any LRHV procedure (P < 0.001).
Table 2.
Educational methods used to teach procedures during the fellowship
| Procedure | Instruction on Live Patients [n (%)] | Simulation-based Teaching [n (%)] | Online Videos or Modules [n (%)] | Dedicated “Procedure” Rotation [n (%)] | Lectures [n (%)] | No Dedicated Training [n (%)] |
|---|---|---|---|---|---|---|
| Arterial line placement | 40 (70.0) | 24 (41.4) | 18 (31.0) | 9 (15.5) | 8 (13.8) | 12 (20.7) |
| CVC placement | 43 (71.2) | 51 (85.0) | 28 (46.7) | 27 (45.0) | 11 (18.3) | 3 (5.0) |
| Flexible bronchoscopy | 49 (83.1) | 56 (94.9) | 30 (50.8) | 40 (67.8) | 20 (33.9) | 0 |
| Thoracentesis | 48 (82.8) | 40 (69.0) | 25 (43.1) | 25 (43.1) | 15 (25.9) | 1 (1.7) |
| All LRHV procedures | 45.0 (76.8) | 42.8 (72.6) | 25.3 (42.9) | 25.3 (42.9) | 13.5 (23.0) | 4.0 (6.85) |
| Blakemore or Minnesota tube placement | 15 (25.9) | 7 (12.1) | 6 (10.3) | 5 (8.6) | 0 (0) | 38 (65.5) |
| Bronchial blocker placement | 21 (35.6) | 16 (27.1) | 7 (11.9) | 8 (13.6) | 5 (8.5) | 27 (45.8) |
| Cricothyroidotomy | 23 (39.7) | 33 (56.9) | 15 (25.9) | 21 (36.2) | 6 (10.3) | 14 (24.1) |
| Pericardiocentesis | 5 (8.6) | 11 (19.0) | 10 (17.2) | 6 (10.3) | 0 (0) | 40 (69.0) |
| All HRLV procedures | 16.0 (27.5) | 16.8 (28.8) | 9.5 (16.3) | 10.0 (17.2) | 2.8 (4.7) | 29.8 (51.1) |
| P value for comparison between all LRHV and HRLV procedures | <0.001 | <0.001 | <0.001 | <0.001 | 0.008 | <0.001 |
Definition of abbreviations: CVC = central venous catheter; HRLV = high-risk, low-volume; LRHV = low-risk, high-volume.
Figure 1.
Educational methods used to teach HRLV procedures versus LRHV procedures. HRLV = high-risk, low-volume; LRHV = low-risk, high-volume.
Fellowship programs use a variety of methods for assessing fellows’ competency in performing procedures. The most common method for assessing competency for LRHV was direct observation (87.8%), whereas only 14.3% of HRLV procedures were assessed in this manner (P < 0.001). Simulation-based assessments were infrequent for all procedures, although more common for LRHV procedures (23.8%) than for HRLV procedures (8.2%, P = 0.002). HRLV procedures were significantly more likely to have no formal mechanism for assessing fellows’ procedural competency, as compared with LRHV procedures (70.1% vs. 5.5%, P < 0.001).
The difference in supervision between HRLV and LRHV procedures was significant. For LRHV procedures, fellows were allowed to perform procedures independently without supervision 21.7% of the time versus 3.9% for HRLV procedures (P = 0.004). With regard to specific LRHV procedures, no fellows (0%) were allowed to perform flexible bronchoscopy independently as compared with 28.9% for the other LRHV procedures (see Table E1 in the data supplement). Fellows are never allowed to independently perform LRHV procedures only 21.6% of the time versus never being allowed to perform HRLV procedures 68.4% of the time (P < 0.001).
The majority of respondents (76.9%) indicated that there was no set number of HRLV procedures required to determine competency, as compared with 25.3% of respondents regarding LRHV procedures (P < 0.001). There was wide variability, however, among the number of procedures needed to determine competency for individual LRHV procedures (Table 3). The majority of respondents indicated there was no set number of required procedures for an arterial line placement (35.8%) as compared with 1–10 procedures for CVC placement (38.9%) and thoracentesis (35.8%), whereas more than 50 procedures were required for flexible bronchoscopy (85.2%).
Table 3.
Minimum number of procedures the fellowship program requires fellows to perform on real patients in clinical practice to demonstrate procedural competence
| Procedure | No Set Number | 1–10 | 11–20 | 21–50 | >50 |
|---|---|---|---|---|---|
| Arterial line placement | 19 (35.8) | 17 (32.1) | 14 (26.4) | 1 (1.9) | 2 (3.8) |
| CVC placement | 14 (25.9) | 21 (38.9) | 10 (18.5) | 7 (13.0) | 2 (3.7) |
| Flexible bronchoscopy | 6 (11.1) | 0 (0) | 1 (1.9) | 1 (1.9) | 46 (85.2) |
| Thoracentesis | 15 (28.3) | 19 (35.8) | 13 (24.5) | 5 (9.4) | 1 (1.9) |
| All LRHV procedures | 13.5 (25.3) | 14.3 (26.7) | 9.5 (17.8) | 3.5 (6.6) | 12.8 (23.6) |
| Blakemore or Minnesota tube placement | 40 (75.5) | 11 (21.0) | 2 (3.8) | 0 (0) | 0 (0) |
| Bronchial blocker placement | 43 (81.1) | 4 (7.5) | 5 (9.4) | 1 (1.9) | 0 (0) |
| Cricothyroidotomy | 38 (71.7) | 7 (13.2) | 7 (13.2) | 1 (1.9) | 0 (0) |
| Pericardiocentesis | 42 (79.2) | 7 (13.2) | 3 (5.7) | 1 (1.9) | 0 (0) |
| All HRLV procedures | 40.8 (76.9) | 7.3 (13.7) | 4.3 (8.0) | 0.8 (1.4) | 0 (0) |
| P value for comparison between all LRHV and HRLV procedures | <0.001 | 0.10 | 0.09 | 0.18 | <0.001 |
For definition of abbreviations, see Table 2.
For LRHV procedures, there was no difference in whether fellows underwent procedural training before performing the procedure on a patient (73.5%), as compared with receiving training at some point during fellowship training independent of patient contact (52.3%, P = 0.296). There was a significant difference between prepatient contact training (21.2%) versus training at any point during fellowship (40.0%, P = 0.023) for HRLV procedures (Table 4).
Table 4.
Proportion of programs with a process for procedural training or education before performing the procedure on a patient as compared to at some point during the fellowship
| Procedure | Training or Education
before Performing a Procedure on a Patient |
Training or Education at
Some Point during Fellowship |
P Value |
|---|---|---|---|
| [n (%)] | [n (%)] | ||
| Arterial line placement | 28 (43.1) | 39 (60.0) | 0.05 |
| CVC placement | 56 (86.2) | 57 (87.7) | 0.80 |
| Flexible bronchoscopy | 58 (89.2) | 61 (93.8) | 0.35 |
| Thoracentesis | 49 (75.4) | 56 (86.1) | 0.12 |
| All LRHV procedures | 47.7 (73.5) | 53.3 (81.9) | 0.296 |
| Blakemore or Minnesota tube placement | 6 (9.2) | 15 (23.1) | 0.03 |
| Bronchial blocker placement | 11 (16.9) | 29 (44.6) | <0.001 |
| Cricothyroidotomy | 30 (46.2) | 42 (64.6) | 0.03 |
| Pericardiocentesis | 8 (12.3) | 18 (27.7) | 0.03 |
| All HRLV procedures | 13.8 (21.2) | 26.0 (40.0) | 0.023 |
For definition of abbreviations, see Table 2.
PDs’ confidence that the program accurately determines fellows’ competence in performing procedures differed for LRHV versus HRLV procedures. On a five-point Likert scale, with 1 indicating high confidence and 5 indicating a significant lack of confidence, the mean score for LRHV procedures was 1.31 ± 0.79 versus 3.52 ± 1.20 for HRLV procedures (P < 0.001) (Table 5).
Table 5.
Confidence that the program accurately determines fellows’ competence in performing procedures
| Procedure | Mean Likert Score* |
|---|---|
| Arterial line placement | 1.40 ± 0.93 |
| CVC placement | 1.32 ± 0.73 |
| Flexible bronchoscopy | 1.25 ± 0.65 |
| Thoracentesis | 1.27 ± 0.84 |
| All LRHV procedures | 1.31 ± 0.79 |
| Bronchial blocker placement | 3.31 ± 1.18 |
| Blakemore or Minnesota tube placement | 3.56 ± 1.13 |
| Cricothyroidotomy | 3.46 ± 1.34 |
| Pericardiocentesis | 3.77 ± 1.13 |
| All HRLV procedures | 3.52 ± 1.20 |
| P value for comparison between all LRHV and HRLV procedures | <0.001 |
For definition of abbreviations, see Table 2.
1 = very confident, 5 = very unconfident.
Discussion
In PCCM and CCM fellowship programs, significant differences exist in procedural training and competency assessments for LRHV procedures as compared with HRLV procedures. This study demonstrated significant heterogeneity among the types of educational interventions used for LRHV procedures, with multiple different pedagogic strategies employed to teach fellows how to perform arterial and CVC placement, flexible bronchoscopy, and thoracentesis. Significantly fewer educational opportunities were identified for HRLV procedures across the surveyed fellowship programs, with the majority of programs indicating that they offered no dedicated training for these procedures.
Similarly, assessments of procedural competency varied significantly between LRHV and HRLV procedures, with regard to both the assessment modalities used and the number of procedures required for fellows to demonstrate competency. Supervision for LRHV procedures varied significantly, with most programs allowing fellows to perform arterial line insertion, CVC insertion, and thoracentesis independently at some point during fellowship training. Flexible bronchoscopy, however, was considered differently by respondents, as the majority indicated that fellows were never allowed to perform this procedure independently outside of emergency settings. Fellows were significantly less likely to be allowed to perform HRLV procedures than any LRHV procedure, and fellowship PDs were significantly less confident in fellows’ ability to perform HRLV procedures after graduation.
The discrepancies in teaching and assessment approaches to LRHV and HRLV procedures may reflect practical considerations by PDs. There is limited time during the fellowship, such that maximizing opportunities to sufficiently train fellows on procedures they will perform frequently in their careers is a high-yield use of time and resources. Clinical demands on fellows and limited resources for teaching fellows to perform infrequent procedures may further contribute to the training differences observed between LRHV and HRLV procedural training. A possibility for this might be that faculty in PCCM and CCM fellowship programs may also be unfamiliar with HRLV procedures and uncomfortable training fellows to perform these procedures. Limited resources, such as HRLV simulators, may also be less common and less available, further impacting the lack of exposure fellows have to learning and practicing HRLV procedures. Finally, fellows in other Internal Medicine subspecialties may also need experience in performing HRLV procedures (e.g., Cardiology fellows need to learn to perform pericardiocentesis and Gastroenterology fellows need to learn to place Blakemore tubes), limiting the already rare opportunities for PCCM fellows to learn and perform these procedures in clinical practice.
In addition, the HRLV procedures we evaluated can generally be performed by physicians in other specialties, including interventional pulmonologists for bronchial blocker placement, gastroenterologists for Blakemore tube placement, cardiologists for pericardiocentesis, and surgeons for cricothyroidotomy. This distribution of different subspecialists being able to perform HRLV procedures may further affect PCCM and CCM faculty’s confidence in performing and teaching these procedures, as well as impact PDs' decisions to allocate time and resources to teaching these procedures during fellowship training.
It is notable, however, that the clinical consequences of not being able to perform HRLV procedures such as bronchial blocker placement, Blakemore tube insertion, cricothyroidotomy, and pericardiocentesis may be catastrophic. Inability to perform these emergency procedures can result in significant morbidity and even mortality. For example, for a patient who cannot be intubated and cannot be bag-mask ventilated, cricothyroidotomy is a life-saving procedure. Furthermore, graduates of PCCM and CCM fellowship programs may end up practicing in settings where other subspecialists are not immediately available to perform these HRLV procedures for them.
It is unclear why there is a stark differentiation in supervision between flexible bronchoscopy and the other LRHV procedures, as our study did not investigate respondents’ motivations for differences in training practices. Potential explanations for the difference between the requirement for supervision for bronchoscopy as opposed to other LRHV procedures could include financial incentives, a specialty-based proprietary view of bronchoscopy as compared with other LRHV procedures, or other motivations not assessed in this study. In addition, for patients who are not intubated, bronchoscopy is frequently performed with moderate sedation, which may require the direct supervision of an attending physician.
The ability to perform HRLV procedures has significant clinical consequences, and our data suggest that procedural training in HRLV is an opportunity for improvement in PCCM and CCM training programs. Potential solutions to the significant differences in training and assessment between LRHV and HRLV procedures could include increased awareness of the significant training gap that exists in PCCM and CCM fellowship training. Although awareness of the training gap is necessary to addressing these issues, it is not sufficient, and conscious efforts by fellowship leadership to devote time and resources to training fellows in HRLV procedures could increase PDs’ and fellows’ confidence in their ability to perform these procedures if needed (12, 16). Similar to the literature regarding rare or never events in clinical practice (17, 18), awareness of and training for HRLV procedures in PCCM and CCM fellowship training could mitigate procedural risk and potentially optimize patient outcomes. Our study demonstrated that fellowship educators are using a multimodal array of educational strategies to teach LRHV procedures; dedicating those resources to teaching HRLV procedures could help to bridge the gap in training. In addition, there may be a role for national professional organizations such as the American Thoracic Society to develop and provide educational resources and opportunities for learning HRLV procedures, given that these procedures occur rarely and creating local resources for teaching and learning HRLV procedures may not be feasible for an individual program.
Limitations
This study has several limitations. The relatively low response rate increases the risk of nonresponder bias affecting the results and threatens the generalizability of the findings. However, the response rate in this study is similar to other nationwide survey studies (19). The presence of an Interventional Pulmonology program could affect participants’ responses and introduce variability into the training and practice patterns. Variability between urban and rural or regional academic medical centers could affect training and practice patterns, and our respondents were primarily from larger urban centers (Table 1). As such, our results may not be generalizable to rural, regional fellowship programs. Finally, our study did not assess respondents’ justifications for their answers, such that nuances or local curricular or resource considerations specific to a given program or institution were not assessed or included in the study.
Conclusions
Significant differences exist in procedural training education for PCCM and CCM fellows for LRHV versus HRLV procedures. Assessment of procedural competencies and expectations regarding supervision for fellows performing procedures also varied significantly. These differences manifested in a significant difference in PDs’ and APDs’ determination of their confidence in fellows’ ability to perform procedures after graduation, with high confidence in graduates’ abilities for LRHV procedures and a significant lack of confidence for HRLV procedures. Increased awareness of this disparity and focused educational interventions in fellowship procedural education may help to bridge the gap in procedural training and competency between LRHV and HRLV procedures.
Supplementary Material
Footnotes
Author Contributions: N.G.S., N.S., and J.B.R. conceived of and designed the research project. All authors contributed to survey design. J.B.R performed data analyses and wrote the manuscript, all authors edited the the manuscript. All authors reviewed and approved the final manuscript.
This article has a data supplement, which is accessible from this issue’s table of contents at http://www.atsjournals.org
Author disclosuresare available with the text of this article atwww.atsjournals.org.
References
- 1.American Board of Internal Medicine. Philadelphia, PA: American Board of Internal Medicine; 2020. Internal medicine certification policies. [accessed 2020 Jul 20]. Available from: https://www.abim.org/certification/policies/internal-medicine-subspecialty-policies/internal-medicine.aspx. [Google Scholar]
- 2. Accreditation Council for Graduate Medical Education, Common Program Requirements for Pulmonary and Critical Care Medicine Fellowship Programs. [accessed 2020 May 22]. Available from: https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements.
- 3. Fessler HE, Addrizzo-Harris D, Beck JM, Buckley JD, Pastores SM, Piquette CA, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014;146:813–834. doi: 10.1378/chest.14-0710. [DOI] [PubMed] [Google Scholar]
- 4. Rothschild JM, Landrigan CP, Cronin JW, Kaushal R, Lockley SW, Burdick E, et al. The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694–1700. doi: 10.1097/01.ccm.0000171609.91035.bd. [DOI] [PubMed] [Google Scholar]
- 5. Nilsson L, Pihl A, Tågsjö M, Ericsson E. Adverse events are common on the intensive care unit: results from a structured record review. Acta Anaesthesiol Scand. 2012;56:959–965. doi: 10.1111/j.1399-6576.2012.02711.x. [DOI] [PubMed] [Google Scholar]
- 6. Ayas NT, Norena M, Wong H, Chittock D, Dodek PM. Pneumothorax after insertion of central venous catheters in the intensive care unit: association with month of year and week of month. Qual Saf Health Care. 2007;16:252–255. doi: 10.1136/qshc.2006.021162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hobolth L, Krag A, Malchow-Møller A, Gancho V, Jensen S, Møller S, et al. Adherence to guidelines in bleeding oesophageal varices and effects on outcome: comparison between a specialized unit and a community hospital. Eur J Gastroenterol Hepatol. 2010;22:1221–1227. doi: 10.1097/meg.0b013e32833aa15f. [DOI] [PubMed] [Google Scholar]
- 8. Babic Z, Nikolic-Heitzler V, Bulj N, Pintaric H, Planinc D, Mihatov S. Hemodynamically unstable pericardial effusion in the Intensive Cardiac Unit: prospective study. Acta Med Austriaca. 2003;30:76–79. [PubMed] [Google Scholar]
- 9. Ricotta DN, Smith CC, McSparron JI, Chaudhry SI, McDonald FS, Huang GC. When old habits train a new generation: findings from a national survey of internal medicine program directors on procedural training. Am J Med Qual. 2018;33:383–390. doi: 10.1177/1062860617743786. [DOI] [PubMed] [Google Scholar]
- 10. Smith CC, Gordon CE, Feller-Kopman D, Huang GC, Weingart SN, Davis RB, et al. Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency. J Gen Intern Med. 2004;19:510–513. doi: 10.1111/j.1525-1497.2004.30161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huang GC, McSparron JI, Balk EM, Richards JB, Smith CC, Whelan JS, et al. Procedural instruction in invasive bedside procedures: a systematic review and meta-analysis of effective teaching approaches. BMJ Qual Saf. 2016;25:281–294. doi: 10.1136/bmjqs-2014-003518. [DOI] [PubMed] [Google Scholar]
- 12. Cook DA, Brydges R, Zendejas B, Hamstra SJ, Hatala R. Mastery learning for health professionals using technology-enhanced simulation: a systematic review and meta-analysis. Acad Med. 2013;88:1178–1186. doi: 10.1097/ACM.0b013e31829a365d. [DOI] [PubMed] [Google Scholar]
- 13. Artino AR, Jr, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36:463–474. doi: 10.3109/0142159X.2014.889814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cook DA, Beckman TJ. Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med. 2006;119:166.e7–166, e16. doi: 10.1016/j.amjmed.2005.10.036. [DOI] [PubMed] [Google Scholar]
- 15. Willis GB, Artino AR., Jr What do our respondents think we’re asking? Using cognitive interviewing to improve medical education surveys. J Grad Med Educ. 2013;5:353–356. doi: 10.4300/JGME-D-13-00154.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg SB. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35:e1511–e1530. doi: 10.3109/0142159X.2013.818632. [DOI] [PubMed] [Google Scholar]
- 17. Sankaranarayanan G, Wooley L, Hogg D, Dorozhkin D, Olasky J, Chauhan S, et al. Immersive virtual reality-based training improves response in a simulated operating room fire scenario. Surg Endosc. 2018;32:3439–3449. doi: 10.1007/s00464-018-6063-x. [DOI] [PubMed] [Google Scholar]
- 18. Keane J, Pawlowski J. Using simulation for OR team training on fire safety. AORN J. 2019;109:374–378. doi: 10.1002/aorn.12630. [DOI] [PubMed] [Google Scholar]
- 19. Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:32. doi: 10.1186/s12874-015-0016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenthal E, Schwartzberg L, Trump DL, Yeatman TJ, Zinner MJ. Chandler, AZ: Antibody-Drug Conjugates Review; 2017. The Nature and Nurturing of Hybrid Academic-Community Cancer Centers. . [accessed 2020 Jul 4]. Available from: https://www.adcreview.com/articles/nature-nurturing-hybrid-academic-community-cancer-centers/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.