Abstract
Background: The impact of the coronavirus disease (COVID-19) pandemic extends beyond the realms of patient care and healthcare resource use to include medical education; however, the repercussions of COVID-19 on the quality of training and trainee perceptions have yet to be explored.
Objective: The purpose of this study was to determine the degree of interventional pulmonology (IP) fellows’ involvement in the care of COVID-19 and its impact on fellows’ clinical education, procedure skills, and postgraduation employment search.
Methods: An internet-based survey was validated and distributed among IP fellows in North American fellowship training programs.
Results: Of 40 eligible fellows, 38 (95%) completed the survey. A majority of fellows (76%) reported involvement in the care of patients with COVID-19. Fellows training in the Northeast United States reported involvement in the care of a higher number of patients with COVID-19 than in other regions (median, 30 [interquartile range, 20–50] vs. 10 [5–13], respectively; P < 0.01). Fifty-two percent of fellows reported redeployment outside IP during COVID-19, mostly into intensive care units. IP procedure volume decreased by 21% during COVID-19 compared with pre–COVID-19 volume. This decrease was mainly accounted for by a reduction in bronchoscopies. A majority of fellows (82%) reported retainment of outpatient clinics during COVID-19 with the transition from face-to-face to telehealth-predominant format. Continuation of academic and research activities during COVID-19 was reported by 86% and 82% of fellows, respectively. After graduation, all fellows reported having secured employment positions.
Conclusion: Although IP fellows were extensively involved in the care of patients with COVID-19, most IP programs retained educational activities through the COVID-19 outbreak. The impact of the decrease in procedure volume on trainee competency would be best addressed individually within each training program. These data may assist in focusing efforts regarding the education of medical trainees during the current and future healthcare crises.
Keywords: interventional pulmonology, training, COVID-19, survey
The coronavirus disease (COVID-19) pandemic marks the beginning of a new era in the practices of modern medicine (1), including medical education. As COVID-19 resulted in an abrupt change in the conduct of healthcare delivery, a new dilemma of how to accommodate continuing medical education and credentialing of medical trainees during times of crisis has materialized (2).
In the United States, the Accreditation Council for Graduate Medical Education acknowledged the challenges imposed on the medical education community by COVID-19 and provided guidance regarding the priorities in medical education and accreditation, personal protective equipment (PPE) shortages, and redeployment of medical residents and fellows (3). Nonetheless, data regarding the effect of COVID-19 on the quality of training and trainee perceptions are scarce. Interventional pulmonology (IP) is a subspecialty of pulmonary medicine, focused on interdisciplinary management of patients with malignant and nonmalignant thoracic diseases, using minimally invasive modalities (4, 5). IP fellowship entails 12 months of clinical training (6). Accreditation standards for IP training programs in North America have been established by a multisociety committee (7). A joint statement by the American Association for Bronchology and IP (AABIP) and Association of Interventional Pulmonology Program Directors (AIPPD) endorsed the Accreditation Council for Graduate Medical Education COVID-19 statement on trainee education (3) and issued guidance pertaining to IP training programs (8).
There exists a paucity of data pertaining to the effects of COVID-19 on trainees’ perceptions of the quality of clinical and academic training. Therefore, we performed a survey among in-training IP fellows in North American fellowship programs to explore the degree of fellow exposure to COVID-19, rates of redeployment outside standard training program, and pandemic effects on patient care, procedure volume, academic activities, and postgraduation employment search.
Methods
The study was approved by the Memorial Sloan Kettering Institutional Review Board (X20-025) and endorsed by the AABIP and the AIPPD. Physicians actively training in a North American accredited IP fellowship program for the academic year 2019–2020 were eligible for participation. Eligible IP fellows were contacted via e-mail and invited to complete the online survey. Participation in the survey was voluntary and responses were deidentified. Informed consent was not required as no protected health information data were collected. Up to three reminder emails in 5-day intervals were sent to fellows who failed to respond or complete the survey. Participation was defined as anonymous and confidential and responses were not disclosed to program directors or supervisors. All responses were anonymized on receipt.
The survey was composed of a 99-item questionnaire in English and was conducted between March 22, 2020, and April 3, 2020. Research Electronic Data Capture (REDCap [Project REDCap]) tools hosted at Memorial Sloan Kettering were used to manage survey data (9). The preliminary survey was devised by three IP fellows (O.K.-D., A.J.S., and N.M.P.) based on the pillars of IP fellowship, as defined in the multisociety statement regarding the accreditation standards for IP training programs in North America: patient-centered clinical decision making, procedural skills, medical education, and academic activities (7). The survey was then reviewed and revised in a multistep process. The initial version was independently reviewed by the AABIP education committee and the AIPPD leadership. Iterative changes were made based on their guidance. Feedback was then sought from pilot testers, including three IP fellows and seven IP program directors. The final version was vetted by all investigators before survey distribution. Survey items included dichotomous questions, multiple-choice questions, Likert scale questions, continuous numerical value questions, and open-ended questions. Participants were asked to provide their age, sex, training background, country of training, and geographical area of training in the United States. Exposure to patients with COVID-19 was assessed, including participation in aerosol-generating procedures (AGPs), access to PPE, and stress management resources. Subsequently, participants were asked about redeployment outside standard IP practice. The next section explored the impact of COVID-19 on procedure volume and skills. Standard IP fellowship procedure types and volumes were derived from the multisociety IP Accreditation Committee report (7). Participants were asked to report procedure numbers from the beginning of fellowship through March 15, 2020, and the median number of monthly procedures was then calculated. Participants were asked to report numbers of the same procedures between March 16, 2020, and April 15, 2020, to allow for a quantitative comparison of procedure volumes before and during COVID-19. The time period between March 16, 2020, and April 15, 2020, was chosen as a representative 30-day period during the COVID-19 outbreak in North America. The survey then examined the effect of the COVID-19 pandemic on outpatient clinic, academic, and research activities during the fellowship. Finally, participants were asked to provide their perspectives on the effect of COVID-19 on their postgraduation employment search. Geographical variation of survey responses was assessed by comparing responses from fellows training in the Northeastern (NE) United States with those obtained from the remainder of the cohort. NE U.S. training programs were in Connecticut, Massachusetts, New Jersey, New York, and Pennsylvania (10). This comparison scheme is based on a Centers for Disease Control and Prevention report indicating the NE region was the epicenter of the U.S. COVID-19 outbreak during the survey period (11). The full survey can be found in the Appendix in the data supplement. The survey participants were again contacted in November 2020 via e-mail and social media tools to assess the status of postgraduation employment.
Descriptive statistics are presented as counts and percentages for categorical variables and mean and standard deviation or median and interquartile range (IQR) for continuous variables. The paired t test was used to compare the mean difference of procedure volume in all regions before and during the COVID-19 pandemic. The equal variance was assumed. For comparison of characteristics between the NE United States and other regions and between quarantining and nonquarantining fellows, the Student’s t test or nonparametric Wilcoxon test was used for continuous variable and the Chi-square or Fisher’s exact tests was used for categorical variables. All statistical tests were two-tailed, and a P < 0.05 was considered statistically significant. SAS software (version 9.4; SAS Institute Inc) was used for all analyses.
Results
At the time of the survey, the AIPPD registry included 40 fellows-in-training at 34 North American IP fellowship programs. Thirty-eight fellows (95%) completed the entire survey, and two fellows (5%) did not respond to the survey invitation. Background characteristics of survey participants are summarized in Table 1.
Table 1.
Demographics and background of survey participants (n = 38)
| Variable | n (%) |
|---|---|
| Female sex | 6 (15) |
| Age, mean ± standard deviation, yr | 35 ± 3 |
| Training background | |
| Pulmonary medicine | 3 (8) |
| Pulmonary and critical care medicine | 34 (89.5) |
| Thoracic surgery | 1 (2.5) |
| Country of training | |
| United States | 35 (92) |
| Northeast | 12 (34.3) |
| South | 11 (31.4) |
| Midwest | 8 (22.8) |
| West | 4 (11.5) |
| Canada | 3 (8) |
COVID-19 Patient Care and COVID-19 Exposure
Seventy-six percent (29/38) of IP fellows reported involvement in the care of patients with COVID-19. Fellows reported involvement in the care of a median of 27 (IQR, 10–35) patients with COVID-19 during the representative 30 days of the COVID-19 outbreak period. Fellows training in NE U.S.–based programs reported involvement in the care of a higher median number of patients with COVID-19 than fellows from all other regions (30 [IQR, 20–50] vs. 10 [IQR, 5–13], respectively; P < 0.01). The work environments of IP fellows caring for a patient with COVID-19 are summarized in Table 2. Of fellows exposed to patients with COVID-19, 65% (19/29) and 58% (17/29) reported participation in tracheostomy and bronchoscopy procedures, respectively. Fellows reported performing a median of 5 (IQR, 2–15) bronchoscopies and 4 (IQR, 1–9) tracheostomies on patients with COVID-19 over the representative 30-day COVID-19 period. NE U.S.–based fellows reported a higher number of tracheostomies performed on patients with COVID-19 than their colleagues from other regions (5 [IQR, 4–15) vs. 1 [IQR, 1–4], respectively; P = 0.01).
Table 2.
Work environment of interventional pulmonology fellows involved in care for patients with COVID-19 (n = 29)
| Variable | n (%) |
|---|---|
| Clinical setting of COVID-19 patient care | |
| IP | 25 (86) |
| Non-IP | 18 (62) |
| Physical setting of COVID-19 patient care | |
| Bronchoscopy suite | 14 (48) |
| Operating room | 12 (41) |
| ICU, IMC, or stepdown unit | 26 (89) |
| Inpatient ward | 8 (27) |
| Emergency department | 3 (10) |
| Outpatient clinic | 2 (7) |
Definition of abbreviations: COVID-19 = coronavirus disease; ICU = intensive care unit; IMC = intermediate care unit; IP = interventional pulmonology; SACU = subacute care unit.
Ninety-seven percent (37/38) of fellows were satisfied with their access to PPE and 87% (33/38) reported access to stress management services. Nonetheless, 13% (5/38) reported self-quarantining and absence from work due to exposure to and/or infection with COVID-19.
Procedure Skills and Volumes
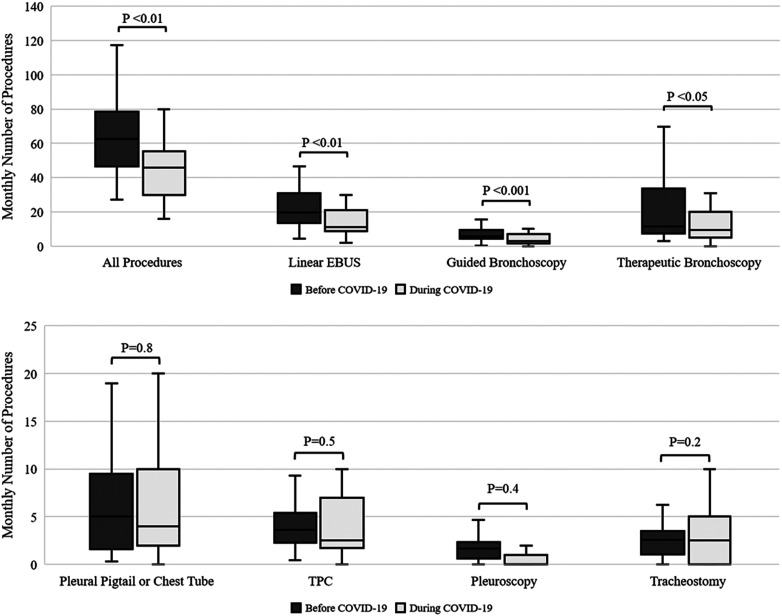
As illustrated in Figure 1, compared with pre–COVID-19 median monthly volume, overall procedure volume during COVID-19 decreased by 21% (P < 0.01). Procedure volumes of linear endobronchial ultrasound, guided bronchoscopies, and therapeutic bronchoscopies decreased by 27%, 39%, and 31%, respectively, when compared with pre–COVID-19 median monthly volumes for the same procedures (P ⩽ 0.01 for all comparisons). In contrast, differences in the volumes of pleural pigtail or chest tube placement, tunneled pleural catheter placement, and tracheostomy before and during COVID-19 did not reach statistical significance (Figure 1). Differences in the change in procedure volumes between the NE United States and other regions did not reach statistical significance (data not shown). In addition, differences in change in procedure volume between fellows who reported quarantining due to exposure or infection with COVID-19 and those who did not report quarantining did not reach statistical significance (data not shown).
Figure 1.
Distribution of procedure volumes before and during coronavirus disease (COVID-19). The distribution of the median monthly number of overall and individual interventional pulmonology procedures before COVID-19 compared with the number of overall and individual interventional pulmonology procedures during a representative 30-day period during the COVID-19 outbreak. The box-and-whisker plots describe the distribution of the median of each procedure. The bold line inside each box represents the median; the boxes surrounding them represent the interquartile range; the lower whisker extends from the 5th to the 25th percentile; the upper whisker extends from the 75th to the 95th percentile. EBUS = endobronchial ultrasound; TPC = tunneled pleural catheter.
Fellow perspectives on the potential negative impact of COVID-19 on the adequacy of training in specific procedures are summarized in Table 3. No statistically significant differences in these perspectives were noted on comparison of responses from NE U.S.–based versus non–NE U.S.–based fellows.
Table 3.
Fellows reporting a negative impact of COVID-19 on procedure skills (n = 38)
| Area of Negative Impact | n (%)* |
|---|---|
| Diagnostic bronchoscopy | 7 (18) |
| Navigation bronchoscopy† | 6 (85) |
| Radial EBUS | 5 (71) |
| Linear EBUS | 3 (43) |
| Therapeutic bronchoscopy | 23 (60) |
| Airway stenting | 16 (69) |
| Endobronchial valve placement | 16 (69) |
| Rigid intubation | 15 (65) |
| APC | 13 (56) |
| Electrocautery | 13 (56) |
| Cryoablation | 12 (52) |
| Laser | 10 (43) |
| Bronchial thermoplasty | 10 (43) |
| Pleural procedures | 13 (34) |
| Pleuroscopy | 12 (92) |
| Pigtail catheter/chest tube placement | 2 (15) |
| Tunneled pleural catheter placement | 2 (15) |
| Additional procedures | 4 (10) |
| Tracheostomy | 4 (100) |
| PEG | 1 (25) |
Definition of abbreviations: APC = argon plasma coagulation; COVID-19 = coronavirus disease; EBUS = endobronchial ultrasound; PEG = percutaneous endoscopic gastrostomy.
Number and proportion of fellows reporting the potential negative impact of COVID-19 on procedure skill acquisition.
Including radial-probe EBUS, ultrathin bronchoscopy, electromagnetic navigation, and/or robotic-assisted navigation bronchoscopy.
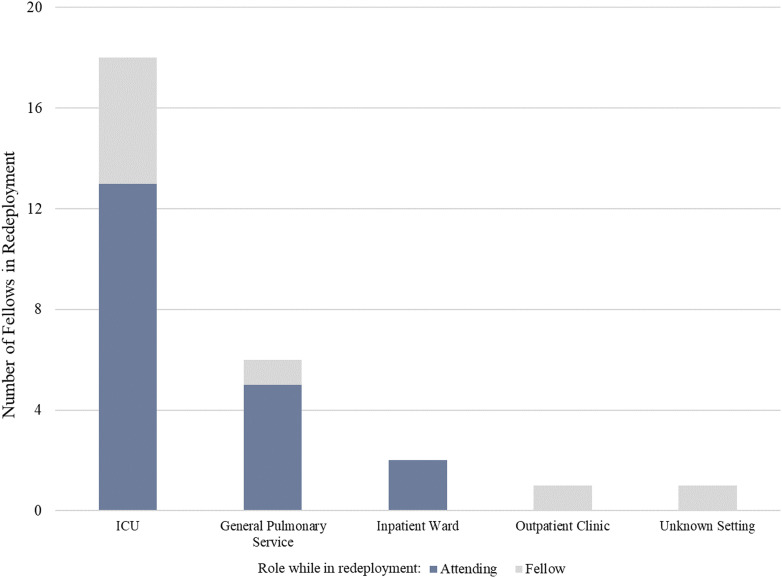
Redeployment
Redeployment outside of IP practice was planned or pursued for 52% (20/38) of theConception and design fellows; of these, 30% (6/20) were already redeployed at the time of the survey and reported spending a median of 60 (IQR, 40–96) weekday hours and 10 (IQR, 0–24) weekend hours practicing in their redeployment field during the representative 30-day COVID-19 period. Redeployment was defined as voluntary and mandatory in 45 (9/20) and 55% (11/20) of cases, respectively. The distribution of redeployment frameworks and physician status are illustrated in Figure 2.
Figure 2.
Interventional pulmonology fellow work environment and physician status during noninterventional pulmonology redeployment (n = 20). ICU = intensive care unit.
Outpatient Clinics
Ninety-two percent (35/38) of fellows reported management of outpatients in a clinic as part of their training. Of these, 82% reported continued outpatient clinic activity during COVID-19. Compared with the pre–COVID-19 period, outpatient clinic activity during COVID-19 was reported as decreased by 77% (27/35) of fellows and 17% (6/35) of fellows reported that their clinics were canceled because of COVID-19. The proportion of fellows reporting face-to-face encounters as the main clinic format decreased from 97% (37/38) before COVID-19 to 17% (6/38) during COVID-19 (P < 0.01). The proportion of fellows involved in telemedicine clinics increased from 3% (1/38) before COVID-19 to 66% (25/38) during COVID-19 (P < 0.01).
Academic Activity
Seventy-nine percent (30/38) of fellows reported their program incorporated a curriculum of IP lectures into their training. Eighty-six percent (26/30) of fellows reported the continuation of educational activities during COVID-19. Compared with the pre–COVID-19 period, educational activities during COVID-19 were reported as unchanged or increased by 53% (16/30) and as decreased or canceled by 47% (14/30) of fellows. The predominant format of lectures before COVID-19 was face-to-face in 76% (23/30) of fellow responses and decreased to 10% (3/30) during COVID-19 (P < 0.01), whereas teleconferencing was reported by 20% (6/30) of fellows before COVID-19 and increased to 86% (26/30) during COVID-19 (P < 0.01).
Twenty-nine percent (11/38) of fellows reported the incorporation of dedicated research time into their fellowship program. Of those, 82% (9/11) reported their research time was unchanged or increased and 18% (2/11) reported their research time was decreased during COVID-19.
Postgraduation Employment
Seventy-six percent of fellows (29/38) reported having secured a postgraduation position at the time of the survey. Of these, 69% (20/29) had no concern or were indifferent, whereas 31% (9/29) were concerned over the likelihood of starting work in their new position after graduation. Of the fellows who were yet to secure a position at the time of the survey, 78% (7/9) reported that their job search was delayed or stopped owing to COVID-19 and expressed concern over their ability to secure employment after graduation, whereas 22% (2/9) reported that their search continued uninterrupted. As of November of 2020, 97% (37/38) of the survey participants confirmed they were able to secure a postgraduation job. The remaining survey participant secured a fellowship position for an additional year of advanced training.
Discussion
The COVID-19 pandemic has dramatically affected patient care and allocation of healthcare resources (12); however, its implications on medical education have not been well studied. The impact on IP fellowship training may be unique compared with other programs given the previous training background of most IP fellows in critical care medicine, which is a skill set in high demand during the COVID-19 pandemic.
At the University of Washington in Seattle, pulmonary and critical care medicine program leaders promptly responded to the disruption in fellows’ training by providing fellows with well-being support, prioritizing patient care responsibilities, and early engagement of fellows-in-training–related decision-making processes (13). Our survey confirms that COVID-19 resulted in the interruption of IP fellows’ clinical training. Nonetheless, the degree of interruption did not seem to affect the overall educational goals and values of IP training, as defined by a multisociety statement (7). Our survey revealed that IP fellows were extensively involved in the care of patients with COVID-19, both within the practice of IP and outside of it. Redeployment was primarily directed toward intensive care units. This is intrinsically reasonable as 89.5% of IP fellows who completed the survey are critical care medicine trained (Table 1). Moreover, care of patients with COVID-19 encompassed the participation of fellows in AGPs, most notably bronchoscopies and tracheostomies (14–16). Furthermore, 13% of fellows reported absence from work due to self-quarantining; however, the potential relationship between participation in AGPs and absence due to self-quarantining is not addressed by the current survey. Importantly, fellows were overall content with access to PPE. These results reflect an overall satisfactory balance between protection of medical trainees, reallocation of healthcare resources, and continuation of medical education during times of crisis (2).
As expected, IP procedure volumes decreased during COVID-19, when compared with pre–COVID-19 numbers. This mainly pertained to bronchoscopies and can potentially be explained by several factors: 1) minimization of AGPs as a policy (15); 2) diversion of resources from outpatient to inpatient care, resulting in delay and cancellation of outpatient bronchoscopies; 3) population practice of social distancing (17) resulting in patient avoidance of visits into healthcare facilities; and 4) decrease in outpatient activities resulting in reduced referrals. The volumes of pleural procedures remained stable. This may be because these procedures are often unavoidable as patients with pleural disease tend to be symptomatic. In addition, pleural procedures are not considered AGP and are hence less restricted by COVID-19. Lastly, despite being significantly aerosol-generating, tracheostomy numbers remained stable during COVID-19. This can be attributed to the high proportion of patients with COVID-19 requiring long-term mechanical ventilation (18).
From a programmatic standpoint, maintaining a minimum number of procedures performed within the institution is crucial for program accreditation to demonstrate that adequate facilities, expertise, and clinical volume are provided by which trainees can develop competency over the course of the training period. Fellows expressed concern over the negative impact of COVID-19 on procedural training, primarily therapeutic bronchoscopy. Individual trainee completion of minimum numbers of procedures, however, does not indicate competency and is therefore not an accreditation requirement (6). It is therefore the responsibility of program directors to individually assess graduating fellows for competency and promptly address areas in which lack of competency is evident. Despite a decrease in bronchoscopies, a review of the median monthly number of major procedures at the time of the survey revealed that volumes of linear endobronchial ultrasound, guided, and therapeutic bronchoscopy were above the recommended numbers designated by the multisociety committee for accreditation of IP training programs (7). This indicates that by the end of the 2019–2020 academic year, overall procedural volumes are likely to remain aligned with program accreditation standards.
Our survey indicates a transition of fellow outpatient activities from face-to-face to telemedicine format, with most programs retaining outpatient clinic activities. These findings are in alignment with a worldwide trend of transition to telehealth (19). Of programs that incorporate IP core curriculum lectures, as mandated by accreditation standards of IP programs (7), 70% have maintained the curricular activities, although many transitioned to a teleconference format. This model has been previously shown to promote medical student safety (20). Online learning resources may represent an additional solution to the cessation of face-to-face educational activities during the crisis (21). In addition, most programs were able to protect fellows’ dedicated research time with a significant number of fellows reporting an increase in research time. This likely reflects the decrease in clinical workload, primarily in procedure and outpatient clinic volumes. Collectively, these data support the argument that IP clinical and academic activities were not significantly attenuated by COVID-19.
At the time of the survey, 76% of fellows had secured postgraduation employment, whereas 24% did not have a secured position. In retrospect, all survey responders were able to secure a postgraduation employment position. Nevertheless, this finding highlights a potentially negative financial impact of the pandemic. It is therefore imperative to promote a system that will identify job opportunities for graduating physicians during times of crisis and allow for the continuation of interviews when travel is limited; teleconference interviews represent one solution together with the establishment of a central repository for institutions seeking IP specialists.
Limitations
Some limitations of our study deserve attention. Although the response rate among IP was 95%, the absolute number of participating fellows is small. This number, however, is proportional to the number of accredited IP programs across North America. The timing of the survey may also represent a limitation. For comparison purposes, we chose a representative 30-day period during COVID-19 in North America. Although the effect of COVID-19 extends beyond that 30-day period, evaluation of this impact is beyond the scope of our current survey but may be the focus of future surveys. Furthermore, as the effects of COVID-19 vary temporally and spatially between different geographic regions, survey responses would vary between regions according to the regional burden of the pandemic at the time of the survey. This limitation was addressed by exploring regional variation and comparing the NE United States—the epicenter of COVID-19 at the time of the survey—with other regions. Future surveys encompassing longer time periods may allow for better assessment of interregional variability. A small minority of IP programs include more than one fellow. Responses from fellows training in the same institution have the potential to amplify the effect of COVID-19 on that institution. Deidentification of survey respondents prevented stratification of the data by the number of fellows per program. Nevertheless, as this pertains to a minority of IP programs, it can be assumed that the impact of multifellow programs is minimal and the overall impact of COVID-19 on IP training remains adequately depicted. Although results of the survey pertaining to the specifics of IP training may not necessarily be generalizable to other fields of medical training, many other aspects of this survey, such as the effect of COVID-19 on academics and fellows’ perspectives on employment do relate to other fields of medical training. Finally, inherent to all surveys, recall, demand characteristics, desirability, and extreme responding biases need to be considered. Given the high response rate within the IP fellow community and the voluntary nature of our survey, we believe the risk for sampling, nonresponse, and acquiescence biases is likely low.
Conclusions
To the best of our knowledge, this is the first survey to address trainee exposure, quality of training, and perspectives with regard to training amid the COVID-19 pandemic. Our results are encouraging because of the perceived overall small negative impact of COVID-19 on the training experience of fellows; however, they highlight aspects of medical training during a time of crisis that may require attention from policymakers. The effect of COVID-19 on IP training may have been diminished as it impacted the final third of the training period; however, its effect on fellows training during the 2020–2021 academic year may be different depending on the dynamics, time-course, and characteristics of the pandemic. Together with other challenges presented by the COVID-19 pandemic, this aspect of medical education will likely require adaptation to a more systematic approach. Maintaining adequate clinical exposure in both inpatient and outpatient settings, minimizing the potential negative impact of redeployment, retaining academic and research activities, and providing support in postgraduation employment are all critical aspects of training that require attention by national organizations, professional societies, and training programs. This survey also establishes an infrastructure for future, larger surveys of trainees as well as a reference period from the early COVID-19 pandemic experience to track changes in the IP fellowship training experience as the pandemic continues to evolve.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank all interventional pulmonology fellows for their inspiring dedication, solidarity, and sacrifices with patient care during the pandemic as well as collegial support and donation of their precious time in participation in this survey.
Footnotes
Supported by the Memorial Sloan Kettering Cancer Center Support grant/Core grant P30 CA008748.
Author Contributions: Conception and design: O.K.-D., A.J.S., N.M.P., J.A.B., B.C.H., M.C., A.S., J.A.A., A.I.M., A.C.A., H.J.L., J.J.M., N.R.D., D.W.H., and R.P.L. Collection and assembly of data: O.K.-D., A.J.S., and N.M.P. Data analysis: O.K.-D., A.J.S., N.M.P., I.-H.L., M.C., and R.P.L. Manuscript writing: O.K.-D., A.J.S., N.M.P., I.-H.L., M.C., and R.P.L. Final approval of the manuscript: all authors.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosuresare available with the text of this article atwww.atsjournals.org.
References
- 1.World Health Organization. Geneva, Switzerland: World Health Organization; 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020. [accessed 2020 May 24]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. [Google Scholar]
- 2. Harrington RA, Elkind MSV, Benjamin IJ. Protecting medical trainees on the COVID-19 frontlines saves us all. Circulation. 2020;141:e775–e777. doi: 10.1161/CIRCULATIONAHA.120.047454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. Chicago, IL: ACGME; 2020. ACGME announces policy to enforce compliance with COVID-19 prevailing requirements. [accessed 2020 Apr 8]. Available from: https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10256/ACGME-Announces-Policy-to-Enforce-Compliance-with-COVID-19-Prevailing-Requirements. [Google Scholar]
- 4. Bolliger CT, Mathur PN, Beamis JF, Becker HD, Cavaliere S, Colt H, et al. European Respiratory Society/American Thoracic Society. ERS/ATS statement on interventional pulmonology. Eur Respir J. 2002;19:356–373. doi: 10.1183/09031936.02.00204602. [DOI] [PubMed] [Google Scholar]
- 5. Shafiq M, Lee H, Yarmus L, Feller-Kopman D. Recent advances in interventional pulmonology. Ann Am Thorac Soc. 2019;16:786–796. doi: 10.1513/AnnalsATS.201901-044CME. [DOI] [PubMed] [Google Scholar]
- 6. Colt HG, Williamson JP. Training in interventional pulmonology: what we have learned and a way forward. Respirology. 2020;25:997–1007. doi: 10.1111/resp.13846. [DOI] [PubMed] [Google Scholar]
- 7. Mullon JJ, Burkart KM, Silvestri G, Hogarth DK, Almeida F, Berkowitz D, et al. Interventional pulmonology fellowship accreditation standards: executive summary of the multisociety interventional pulmonology fellowship accreditation committee. Chest. 2017;151:1114–1121. doi: 10.1016/j.chest.2017.01.024. [DOI] [PubMed] [Google Scholar]
- 8.The American Association for Bronchology and Interventional Pulmonology and the Association of Interventional Pulmonology Program Directors. St. Paul, MN: The American Association for Bronchology and Interventional Pulmonary; 2020. SARS-CoV-2 (COVID-19) interventional pulmonology fellowship guidance. [accessed 2020 Jun 6]. Available from: https://aabronchology.org/2020/04/21/covidresponse/ [Google Scholar]
- 9. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United Sates Census Bureau. Washington, DC: United States Census Bureau; 2010. 2010 census regions and divisions of the United States. [accessed 2020 Nov 20]. Available from: https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Atlanta, GA: CDC; 2020. A weekly surveillance summary of US COVID-19 activity. [accessed 2020 May 16]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-05–08–2020.pdf. [Google Scholar]
- 12. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 13. Çoruh B. Flattening the curve: minimizing the impact of COVID-19 on a pulmonary and critical care medicine fellowship training program. ATS Scholar. 2020;1:110–118. doi: 10.34197/ats-scholar.2020-0047PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wahidi MM, Shojaee S, Lamb CR, Ost D, Maldonado F, Eapen G, et al. The use of bronchoscopy during the Coronavirus Disease 2019 pandemic: CHEST/AABIP guideline and expert panel report. Chest. 2020;158:1268–1261. doi: 10.1016/j.chest.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Atlanta, GA: CDC; 2020. Social distancing: keep your distance to slow the spread. [accessed 2020 May 16]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html. [Google Scholar]
- 18. Angel L, Kon ZN, Chang SH, Rafeq S, Palasamudram Shekar S, Mitzman B, et al. Novel percutaneous tracheostomy for critically ill patients with COVID-19. Ann Thorac Surg. 2020;110:1006–1011. doi: 10.1016/j.athoracsur.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27:1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Park SW, Jang HW, Choe YH, Lee KS, Ahn YC, Chung MJ, et al. Avoiding student infection during a Middle East respiratory syndrome (MERS) outbreak: a single medical school experience. Korean J Med Educ. 2016;28:209–217. doi: 10.3946/kjme.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keegan DA, Chan MK, Chan T. Helping medical educators worldwide to pivot curricula online: Med Educ. 2020;54:766–767. doi: 10.1111/medu.14220. PivotMedEd.com [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.