Abstract
Background
There is a high prevalence of moderate-to-high levels of chronic stress among nurses, as well as an occurrence of musculoskeletal disorders.
Purpose
To evaluate the effectiveness of chair massage to reduce chronic stress and musculoskeletal pain in the Oncology Nursing team.
Setting
Two teaching cancer hospitals, one public and the other private, in São Paulo city, Brazil.
Participants
A total of 60 women from the Oncology Nursing team.
Research Design
A randomized controlled trial divided into two groups: chair massage and control without intervention.
Intervention
The massage group received two chair massage sessions lasting 15 minutes, twice a week, for three weeks.
Main Outcome Measure
Reduction of stress and pain measured by the List of Signs and Symptoms (LSS) and the Brief Pain Inventory (BPI), respectively.
Results
The average age was 32 (± 5.3) years. There was a reduction of stress measured by the LSS with a statistical difference in the group-time interaction (p < .001), with a Cohen’s d value of 1.21 between groups. The BPI analysis showed a statistically significant difference in the group-time interaction for general activity (p < .008), mood (p < .03), work (p < .000), and sleep (p = .03), with reduced pain interference in these components.
Conclusion
Chair massage reduced stress and pain interference in the team’s daily life activities, bringing a positive impact in the context of work stress and pain in Oncology nursing professionals.
Keywords: occupational stress, musculoskeletal pain, massage, nursing, team
INTRODUCTION
Nursing professionals work in a complex scenario due to the daily work fragilities and the work environment conditions, especially in Brazil(1–2) where self-perception of work as exhausting reaches at least 65.9% of the nursing staff. This evidences a correlation between working conditions, occupational health,(3) and patient safety.(1)
A high prevalence of chronic stress among nursing professionals is a frequent finding,(4–5) as well as the occurrence of musculoskeletal disorders.(6–8) Chronic job stress has been studied worldwide, with prevalence rates varying according to the care unit and hospital type.(9–12) A review study(13) on stress in nursing professionals in Latin American observed a frequency of moderate-to-high stress, ranging from 23% to 78%.
The stress experienced by the nursing team has been related to the high burden of responsibilities;(14) to inadequate resources and human working conditions, such as a lack of equipment and inappropriate staff sizing; conflicting relationships within the team; lack of support among colleagues;(15) feedback only given regarding unsatisfying performances;(16) few opportunities for continuous professional development; and verbal, psychological, and physical violence.(17)
There are stressing characteristics common to the nursing category in all patient care settings; however, the oncology unit, especially in the hospital setting, presents elements which favor psychological overload due to complex and conflicting situations, prolonged hospitalizations of patients, mutilating surgeries,(18) patient and family expectations, and the challenge of dealing with the constant terminality and threat to life,(19) in addition to the need for making decisions in ethically complex situations.(20)
The complexity of care and high work-load, whether physical or mental, predisposes these professionals to occupational illnesses and accidents, and to physical and mental wear,(21) thus increasing absenteeism rates and the number of sickness absences, bringing additional costs to the health institution.(20) In addition, chronic stress can compromise the quality of care and safety of patients, predisposing these professionals to make errors in preparing and administering medications.
With regard to physical wear, nursing also has high rates of musculoskeletal pain associated with the intrinsic characteristics of the care practice and common to the various care units, such as prolonged standing time; inadequate postures in performing the procedures; inadequate furniture/equipment; the handling of excessive weight, materials or patients; shift rotation; and night work.(22) The most affected body regions among hospital professionals are the lumbar, shoulder, and neck regions.(23) The prevalence of lumbar pain in nursing can range from 71.6% to 85.3% of the professionals;( 22–26) and neck pain for up to 46.8%. (22) There is evidence, albeit moderate, that perceived stress and life stressors contribute to developing chronic musculoskeletal disorders.(27)
Massage is a nonpharmacological integrative practice which can help in managing chronic stress and pain; good results have been obtained in reducing the stress perceived in health professionals,(28–30) and in managing their pain.(31) Chair massage (CHAIR-M) is used in the work environment, as it can be applied rapidly from a suitable chair without the need to remove clothes from the body of the recipient.(32) The chair, designed by D. Palmer, enables the person to receive a massage in a comfortable sitting position (height adjustment of the seat, angular supports for leg, chest, head, and arms).(33) It presents good results in reducing musculoskeletal pain, fibromyalgia, and anxiety; it also promotes relaxation and improves sleep quality.(29)
The massage is performed by acupressure, which is pressure on the points coming from acupuncture based on knowledge of meridians from Traditional Chinese Medicine,(34) with the therapists using their thumbs or index fingers. The anatomical spots commonly massaged are the neck, shoulders, back, arms, and hands. Studies using CHAIR-M in health workers used pre- and postintervention designs in volunteers who signed up to receive a massage.(32,35)
Given the negative impact of chronic stress and musculoskeletal pain on occupational health and the absence of controlled clinical trials using CHAIR-M in health workers, the objective of this study was to evaluate the effectiveness of the CHAIR-M to reduce chronic stress and musculoskeletal pain in an Oncology Nursing team. Thus, the question to answer is, “Can chair massage reduce chronic stress and musculoskeletal pain in an Oncology Nursing team?”
In addition, participants can benefit from the opportunity to receive a massage during the working day, and researchers can benefit from the possibility of validating a massage protocol with evidence of the effects of massage on stress and, consequently, on pain.
METHODS
Study Design
A randomized, two-arm clinical trial was conducted at teaching Cancer hospitals, one governmental and the other private, located in São Paulo city, Brazil. Data collection took place from November 2017 to August 2018.
Population
The population was composed of nursing professionals, all women. The sample size took the result of an intervention study with massage for stress relief(30) as a reference, with 15 points difference on the List of Stress Symptoms (LSS)(36) between the groups and 20 points of standard deviation (SD). Thus, in taking a test power of 80% and a 95% confidence level (CL), the estimated sample size was 28 nursing professionals in each group, rounded up to 30.
The inclusion criteria were the following: women aged 20 to 45; working in the day-time shift (morning, afternoon, or 12-hour shift); LSS score ≥ 40; time working in the hospital of at least one year; and 30-day interval after returning from vacation or medical leave. The exclusion criteria were: smokers; hypertensive individuals; use of glucocorticoids, beta-blockers, psychoactive drugs in the last three months; pregnant or hysterectomized women; use of integrative practices (acupuncture, massage, herbal therapy, reiki, or floral therapy, among others) for at least two months.
Recruitment
The nonprobabilistic sample was recruited through disseminating the survey in hospitals through contact with the heads of the hospital sectors via institutional e-mail and in person. Researchers and the collection team also distributed the information in the hospital care units during shift change via numbered envelopes containing detailed information of the study, the Informed Consent Form, the LSS, and a questionnaire containing biosocio-demographic data needed to assess the eligibility of the volunteers. Two elastic folders were left in each care unit: one to deposit the envelopes with filled-in documentation, and another with envelopes for the professionals absent on the day of the disclosure.
Randomization
The volunteers who met the inclusion criteria were numbered for the two-group simple randomization (http://www.randomizer.org). After this, one of the researchers created a sequential numerical list: the first participant was randomly chosen and the rest were included in the list as they met the eligibility criteria and according to the groups of the randomized list. The study was blinded to researchers, participants, and statistician.
Intervention
The appointments were previously made with the lead researcher and shared with the therapists. The intervention involved two 15-minute chair massage sessions per week for three weeks performed after the work shift or at lunchtime, in a room especially designated for this purpose. The sessions were conducted by the therapist in a quiet setting, free from any other relaxing features such as music, essential oils, or environmental aromas. The team of therapists consisted of five auxiliary nurses, one nursing technician, and one nurse external to the study hospitals. The team was trained by the lead researcher, who has ten years of experience in massage techniques. Therapists received 5-hour training focused on the study protocol.
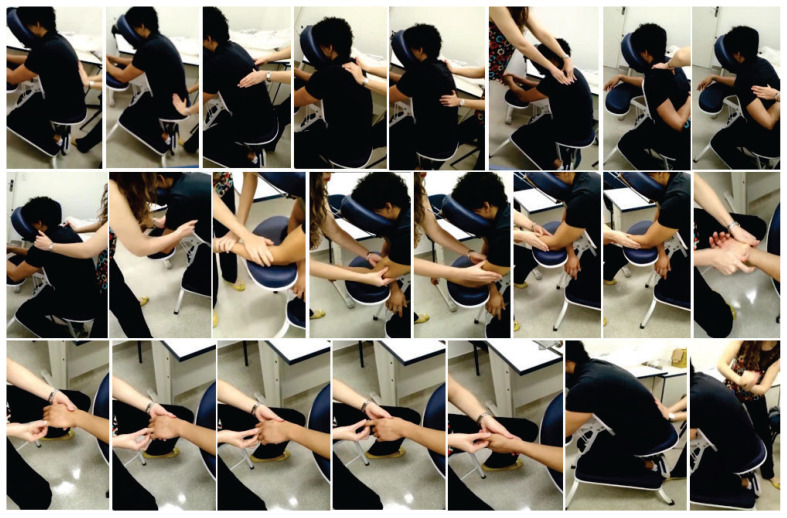
The CHAIR-M protocol (Figure 1) presented the following sequence: (1) superficial and deep sliding from proximal to distal, through the thoracic and lumbar paravertebral region; (2) pressure with the thumb on the paravertebral over the longest muscle of the back, from proximal to distal; (3) kneading the paravertebral region over the longest back muscle with the thumb, from proximal to distal; (4) kneading with the supracarpal region to the paravertebral region; (5) pressure with the thumb on the upper trapezius muscle; (6) kneading the upper trapezius muscle with the thumb; (7) kneading the minor rhomboid muscle with the thumb, from the medial to the lateral, leaving the fourth thoracic vertebra to the upper scapular angle; (8) kneading around the medial margins, lower angle and lateral margin of the scapula with the thumbs; (9) kneading on the infraspinatus muscle; (10) kneading on the interline of the glenohumeral joint; (11) kneading on the arm with fingers and the supracarpal; (12) kneading on fist extensor muscles with thumbs; (13) kneading the fist’s flexor muscles with the thumbs; (14) kneading the anterior and posterior regions of the upper limb with the supracarpal; (15) deep sliding on the palm of the hand with the supracarpal; (16) kneading the palm of the hand; (17) pressure and traction on fingers; (18) elbow extension and traction, vibration of the upper limb; (19) repeated procedures from 5 to 18 on the contralateral upper limb; (20) superficial and deep sliding on the paravertebral region; (21) percussion on the paravertebral musculature.
Figure 1.
Step-by-step of the chair massage protocol.
The control group received no treatment; they simply filled out the scales and questionnaires at the time defined in the study design.
Outcome Measures
Reduction of stress and pain were considered as outcomes. All participants in the CHAIR-M and Control groups answered the LSS and the Brief Pain Inventory (BPI) at the beginning of the study and after three weeks.
The LSS(36) is a list of 59 psychophysiological and psychosocial symptoms of stress in which the individual must check the intensity of symptoms on a Likert type scale. The score can vary from 0 to 177 points. Scores from 12 to 28 points characterize low stress; from 29 to 60 points, medium stress; from 61 to 120 points, high stress; and above 120 points, very high stress. The last validation of the LSS in a Brazilian population developed in 2001 showed a Cronbach alpha of 0.91, and a temporal stability assessed by the test-retest using Pearson’s correlation of 0.94.(37)
The BPI, validated for the Portuguese language, is a multidimensional scale which evaluates the severity of pain and the interference of pain in six situations: general activities, mood, walking ability, normal work, relations with others, sleep and enjoyment of life.(38) It has a range from 0 (no interference) to 10 (maximum interference). The internal consistency of the BPI Portuguese version was 0.91 for the pain severity dimension and 0.87 for the pain interference dimension; the construct validity determined by confirmatory factor analysis showed a good fit of the model.(38) The present study applied the pain interference dimension.
Statistical Analysis
Central tendency and variability measures were calculated for the quantitative variables. Homogeneity across groups was verified by chi-squared test for the quality variables, except for medication for which the Fisher’s exact test was used, the Student’s t-test for age, and the Wilcoxon-Mann-Whitney for Body Mass Index (BMI). The mixed linear adjusted model for maximum restricted likelihood (REML) was used to determine statistical differences between the groups. The significance level was set at 5%. The effect size was analyzed by the Cohen’s d test(39) and interpreted as: insignificant (< 0.19), small (0.20–0.49), medium (0.50–0.79), large (0.80–1.29), and very large (> 1.30). The values to interpret the percentage of change were: huge reduction (> 75), very large reduction (50 ≤ r <75), large reduction (30 ≤ r <50), medium reduction (15 ≤ r < 30), small reduction (5 ≤ r < 15), and insignificant change (< 5). The minimal clinically important difference (MCID) based on distribution was calculated considering the medium effect size of Cohen’s d equal to 0.5.(40) Data were tabulated into Excel® and analyzed by the Statistical Package for the Social Sciences (SPSS® 22.0) and R® 4.0.4 software programs.
Ethical Aspects
The study was approved by the Research Ethics Committee of the University of São Paulo Nursing School (No. 2,087,446) and co-participating institutions (No. 2,535,386 and No. 2,348,294). Written informed consent was obtained from the eligible participants, and the Control group received the CHAIR-M for the same time as the intervention group after the study. The study was funded by the Research Support Foundation of São Paulo State (process No. 2017/19,645–2) and registered in the Brazilian Clinical Trial Registry No. RBR-3bjjf4.
RESULTS
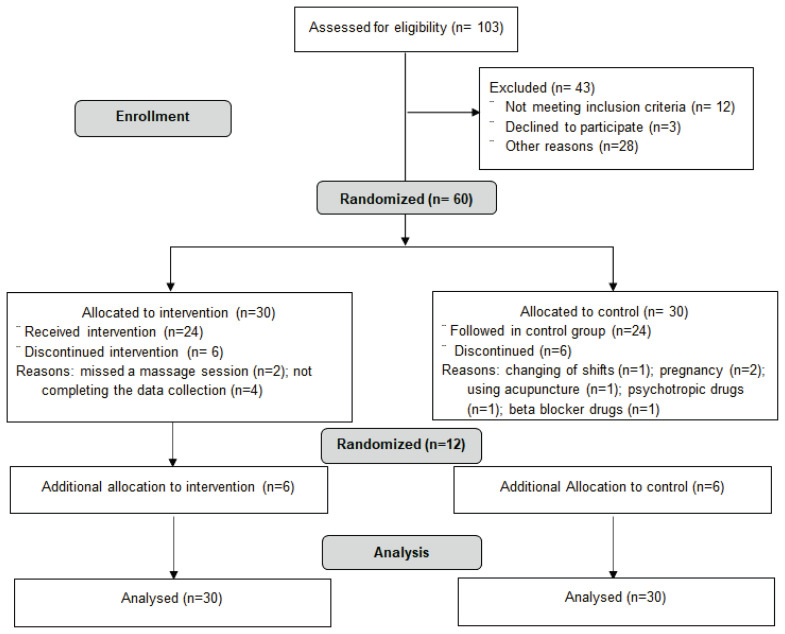
Recruiting and maintaining the nursing professionals throughout the study were difficult due to the loss of some participants, and it was necessary to recruit and randomize other ones. Figure 2 shows the allocation and conduct flowchart of the controlled and randomized study.
Figure 2.
Flowchart of the study design as recommended by CONSORT.
Participants’ Characteristics
The average age of the women was 34.2 (SD ± 5.3) years old, with a mean Body Mass Index (BMI) of 26.7 Kg/m2 (SD ± 5.0), presenting an overweight profile; 63.3% lived with a partner, 40% mentioned health problems (hypothyroidism, migraine, asthma, endometriosis, sleep disorders, dyslipidemia, and chronic pain), and 80% did not continuously use medication. The group consisted of 45% nurses, 33% nursing technicians, and 22% auxiliary nurses, 45% of whom have worked at the institution for four to six years. Given the diversity of care units, the participants were characterized according to the criticality of their work area. Thus, 68% worked in semicritical care units (inpatient, outpatient, bed management, radiology, or resonance), and the others (32%) in critical areas (surgical center, intensive care unit, emergency room, chemotherapy, endoscopy, hemodialysis, laboratory).
The groups were homogenous regarding the qualitative variables used to describe the population (Table 1)—age (p = .700), BMI (p = .825), LSS (0.132), and BPI—except for the pain interference component in enjoyment of life (p = .037).
Table 1.
Distribution of the Nursing Professionals by Bio-socio-demographic and Professional Qualitative Variables
| Variable | Categories | CHAIR-M | Control | P value | ||
|---|---|---|---|---|---|---|
|
| ||||||
| N | % | N | % | |||
| Marital status | Married | 18 | 60.0 | 13 | 43.3 | 0.296 |
| Divorced | 4 | 13.3 | 2 | 6.7 | ||
| Lives with someone | 2 | 6.7 | 5 | 16.7 | ||
| Single | 6 | 20.0 | 10 | 33.3 | ||
| Base diseasea | No | 18 | 60.0 | 19 | 63.3 | 0.792 |
| Yes | 12 | 40.0 | 11 | 36.7 | ||
| Medicationb | Yes | 9 | 30.0 | 6 | 20.0 | 0.542 |
| No | 21 | 70.0 | 24 | 80.0 | ||
| Position | Nurse | 17 | 56.7 | 10 | 33.3 | 0.144 |
| Auxiliary/Technician | 13 | 43.3 | 20 | 66.7 | ||
| Hospital | Public | 21 | 60.0 | 10 | 33.3 | 0.624 |
| Private | 9 | 30.0 | 20 | 66.7 | ||
| Work shift | Daytime | 15 | 53.6 | 13 | 46.4 | 0.201 |
| Morning | 14 | 53.8 | 12 | 46.2 | ||
| Afternoon | 1 | 16.7 | 5 | 83.3 | ||
| Working time at the institution | Up to 3 years | 5 | 16.7 | 12 | 40.0 | 0.079 |
| 4 to 6 years | 14 | 46.7 | 13 | 43.3 | ||
| Over 6 years | 11 | 36.7 | 5 | 16.7 | ||
| Care units | Semicriticalc | 20 | 49.1 | 21 | 50.9 | 1.000 |
| Criticald | 10 | 57.1 | 9 | 42.9 | ||
Hypothyroidism, asthma, endometriosis, migraine, sleep disorders, dyslipidemia, chronic pain
Oral contraceptives, injectable contraceptives, intrauterine device, polycystic ovarian medication
Semicritical: Hospitalization Unit, Ambulatory, Bed Management, Laboratory, Radiology, Resonance
Critical: Surgical Center, Intensive Care Unit, Emergency Room, Chemotherapy, Endoscopy, Hemodialysis
Effect of Intervention on Stress
The stress analysis by the LSS showed that 6.7% (n=4) had a very high stress score, 65.0% (n=39) had a high level, and 28.3% (n=17) had medium level. The mean score from the LSS in each group showed a decrease of the stress score in the CHAIR-M group and maintenance of the same pattern in the control group (Table 2), with a significant difference between the groups (p < .0001), and also observed through the 95% CI.
Table 2.
Descriptive Measures of LSS Scores and Study Groups’ Comparative Analysis
| Group | Time | N | Mean | SD | Median | Range | P value a | 95% IC |
|---|---|---|---|---|---|---|---|---|
| CHAIR-M | Pre | 30 | 81.7 | 24.7 | 79.5 | 40–133 | <0.0001 | [72.90, 90.50] |
| Post | 30 | 46.1 | 18.3 | 44 | 5–92 | [39.60, 52.60] | ||
| Control | Pre | 30 | 72.1 | 23.9 | 68 | 40–132 | [63.50, 80.60] | |
| Post | 30 | 72.4 | 25.5 | 67 | 36–130 | [63.30, 81.50] |
Mixed linear adjusted model – interaction time:group
Effect size by Cohen’s d between groups was 1.21, with a 36% reduction in the stress score in CHAIR-M. The intragroup effect size was 1.66 in CHAIR-M group with a 44% reduction in stress score and zero in the Control group. Both comparisons showed a reduction superior to the MCID = 12.3 in the CHAIR-M group.
A stress reduction occurred in both hospitals by stratifying the CHAIR-M and control groups by locus (p < .001). There was a reduction regarding the phase of the menstrual, follicular or luteal cycle (p < .001), but the effect was not significant in women who did not menstruate. There was a reduction regarding the working time in the hospital for the categories up to one year and more than six years (p < .001).
Effect of Intervention on Pain
More than half of the participants (60%) reported pain. In the CHAIR-M group, 56.7% (n=17) reported pain, and the mean time of perceived pain was 10 months. Continuous pain was reported by 52.9% (n=9) of the group, and 47.1% (n=8) mentioned intermittent pain with an average daily frequency of twice. Regarding pain and etiology type, 47.1% (n=8) reported somatic pain, 23.5% (4.0) neuropathic, 11.8% (n=2) visceral pain, and 5.9% (n=1) each with bone pain, visceral and idiopathic pain junction. Cervical, thoracic, and lumbar were the main pain sites among the several mentioned. Movement contributed to the onset of pain in 64.7% (n=11) of the participants who reported pain. The CHAIR-M group used analgesic and rest (32.3%; n=6), analgesic (23.5%; n=4), and rest (17.6%; n=3) among the strategies for pain relief, as well as others mentioned alone such as stretching and massage.
In the Control group, 63.3% (n=19) had pain complaints, and the mean time of perceived pain was five months. Among those with pain, 36.8% (n=7) reported continuous pain, and 63.2% (n=12) intermittent pain with an average daily frequency of twice. Regarding the type of pain, 42.1% (n=8) reported somatic pain, 21.0% (n=4) neuropathic, 15.8% (n=3), visceral and idiopathic, and 5.3% (n=1) for visceral, idiopathic, somatic, and visceral pain each. The most cited pain regions were the head, back (cervical to lumbar), and legs. Movement contributed to the onset of pain in 63.2% (n=12) of those who reported pain, followed by mental stress (21.0%; n=4). This group used rest (42.1%; n=8), analgesic and rest (26.3%; n=3), and analgesic (26.3%; n=3) among the strategies for pain reduction, as well as others mentioned alone such as acupuncture and massage.
Perceived pain changed in the groups in the final assessment, as did the pain regions. The percentage of pain in the CHAIR-M group decreased from 56.7% to 40%, and the pain regions changed with relief in back, lumbar, and cervical pain. The pain percentage in the control group decreased from 63.3% to 50%. There was a reduction in headaches, back, and lumbar pain.
There was a statistically significant reduction of pain interference across groups on daily activity (p = .008), mood (p = .027), normal work (p = .001), and sleep (p = .031) (Table 3). A significant intragroup reduction was observed in the CHAIR-M group for the following BPI components: general activity, mood, walking ability, normal work, relations with others, sleep, and enjoyment of life (p < .05), but only observed in general activities and normal work via the 95% CI. As shown in Table 3, the difference pre/postintervention was superior to the MCID value in the CHAIR-M group, except for walking ability (MCDI=1.5), and not observed in the Control group. The difference between CHAIR-M and Control groups was also superior to the MCID for each item of the pain interference dimension.
Table 3.
Descriptive Measures of the Pain Interference BPI Scores, MCID Value, and Study Groups’ Comparative Analysis
| IBD/Group | Time | N a | Mean (SD) | Range | Difference Pre/Post | MCID | P value b | 95% IC |
|---|---|---|---|---|---|---|---|---|
| General Activity | 1.2 | 0.008 | ||||||
| CHAIR-M | Pre | 17 | 5.9 (2.0) | 1–9 | [4.74, 7.06] | |||
| Post | 12 | 3.2 (1.6) | 0–5 | 2.7 | [1.63, 4.37] | |||
| Control | Pre | 19 | 5.7 (2.8) | 0–10 | [4.87, 7.33] | |||
| Post | 15 | 6.1 (2.2) | 2–8 | −0.4 | [4.61, 6.79] | |||
| Mood | 1.3 | 0.027 | ||||||
| CHAIR-M | Pre | 17 | 5.4(2.5) | 0–10 | [4.14, 6.66] | |||
| Post | 12 | 2.9 (2.2) | 0–6 | 2.5 | [1.40, 4.40] | |||
| Control | Pre | 19 | 6.0 (2.8) | 1–10 | [4.81, 7.19] | |||
| Post | 15 | 5.8 (2.5) | 2–10 | 0.2 | [4.46, 7.14] | |||
| Walking Ability | 1.5 | 0.082 | ||||||
| CHAIR-M | Pre | 17 | 4.7 (2.8) | 0–9 | [3.30, 6.10] | |||
| Post | 12 | 3.2 (1.7) | 0–5 | 1.5 | [1.54, 4.86] | |||
| Control | Pre | 19 | 5.1 (3.1) | 0–5 | [3.78, 6.42] | |||
| Post | 15 | 5.1 (2.8) | 0–5 | 0 | [3.61, 6.59] | |||
| Normal Work | 1.2 | 0.001 | ||||||
| CHAIR-M | Pre | 17 | 6.5 (2.0) | 3–10 | [5.34, 7.66] | |||
| Post | 12 | 3.3 (1.5) | 0–5 | 3.2 | [1.92, 4.68] | |||
| Control | Pre | 19 | 5.6 (2.8) | 0–10 | [4.50, 6.70] | |||
| Post | 15 | 6.3 (1.9) | 3–9 | −0.7 | [3.87, 6.33] | |||
| Relations With Others | 1.5 | 0.087 | ||||||
| CHAIR-M | Pre | 17 | 5.1 (2.5) | 0–9 | [3.66, 6.54] | |||
| Post | 12 | 3.0 (2.7) | 0–9 | 2.1 | [1.29, 4.71] | |||
| Control | Pre | 19 | 5.2 (2.8) | 0–10 | [3.84, 6.56] | |||
| Post | 15 | 5.1 (2.5) | 0–9 | 0.1 | [3.57, 6.63] | |||
| Sleep | 1.3 | 0.031 | ||||||
| CHAIR-M | Pre | 17 | 5.8 (2.9) | 0–10 | [4.55, 7.05] | |||
| Post | 12 | 3.3 (2.9) | 0–10 | 2.5 | [1.82, 4.78] | |||
| Control | Pre | 19 | 5.2 (3.2) | 0–10 | [4.02, 6.38] | |||
| Post | 15 | 5.5 (3.0) | 0–10 | −0.3 | [4.17, 6.83] | |||
| Enjoyment of Life | 1.4 | 0.053 | ||||||
| CHAIR-M | Pre | 17 | 4.9 (2.2) | 0–9 | [3.55, 6.55] | |||
| Post | 12 | 3.3 (1.9) | 1–9 | 1.6 | [1.69, 4.91] | |||
| Control | Pre | 19 | 4.7 (3.4) | 0–10 | [3.42, 5.98] | |||
| Post | 15 | 5.1 (2.7) | 0–9 | −0.4 | [3.66, 6.54] | |||
Some participants did not answer the Brief Pain Inventory in post assessment
Mixed linear adjusted model – interaction time:group
The analysis of the effect size by Cohen’s d between groups showed a huge effect on general activity (d = 1.53) and on normal work (1.79), as well as a very large effect on mood (1.28). Although some BPI components showed a large effect seen in the walking ability (0.87), relations with others (0.84), sleep (0.81), and enjoyment of life (0.79) components, there was no significant statistical difference between the study groups over time.
No adverse event was observed or mentioned by the participants.
DISCUSSION
The chair massage proved to be effective in reducing the chronic stress of the Oncology Nursing team, and in reducing pain interference mainly in daily activity and normal work. The nursing team experiences situations related to the care process, the working relationships, and the hierarchical structure, which exposes them to high rates of stress(9–13,20) and pain,(22–26,41) and complementary practices can be beneficial to relieve these symptoms.
Stress and Pain in the Nursing Team
The experience of stress over a long period of time favors developing health problems such as metabolic syndrome,(42) mental disorders,(9,42) sleep disorders, memory problems,(43) and Burnout Syndrome, which may impact patient safety with low-quality care and risk of adverse events.(44) A meta-analysis(20) involving almost 10,000 Oncology nurses identified the presence of 30% of emotional exhaustion assessed by the Burnout Scale, evidencing the emotional involvement of the team with the problems experienced by the patient and family members, as well as the work environment.
The musculoskeletal pain analyzed herein corroborates a study conducted in Pernambuco (Brazil), in which 53.8% of the hospital nursing team presented musculoskeletal pain, with emphasis on the lumbar region and on the knees.(45) A survey-type study conducted with nurses in 12 hospitals from five regions in China identified that more than half of the nurses presented wrist and/or cervical pain, followed by other anatomical regions such as shoulders, back, and knees.(7) The differences observed herein occur according to the body constitution of the patients assisted and of the professionals, as well as the working environment. A study with Portuguese nurses found a prevalence of low-back pain around 60% in the year, and the most related activities were the following: leaning the trunk, lifting and moving loads over 20 kg, and working in a standing position. Furthermore, the risk factors identified were the following: age under 40 years old, less time in the profession, and tall persons; rest and the use of analgesics were the most used interventions by nurses for pain management.(46) Analgesics and muscle-relaxing drugs are the most used classes of medications in the practice of self-medication in Brazil.(47)
Effect of Chair Massage on Pain and Stress
This study showed that chair massage is an integrative practice with beneficial results in stress reduction and pain. Bed-side nurses of an urban hospital enrolled in a randomized controlled study showed significant and beneficial results using CAHIR-M on perceived stress, when compared to a 10-minute coffee break.(32) A single-arm clinical trial with nurses from the psychiatric unit and the pain rehabilitation clinic applied 10 sessions of CHAIR-M for 15 minutes, once a week, for 10 weeks during rest time or coffee breaks, and found a significant decrease in stress and anxiety symptoms after the intervention, mainly in nurses of the 12-hour shift between the fifth and sixth week.(35) Another single- arm study which delivered CHAIR-M to ambulatory Oncology nurses, found that they used around four sessions of 15-minute CHAIR-M with a significant decrease in perceived stress, but no difference in systolic and diastolic blood pressure or heart rate.(48)
Studies with CHAIR-M applied to nursing professionals have focused on stress, but it is possible to find CHAIR-M delivered to other workers. A preliminary randomized and controlled study with office workers in Poland applied eight sessions of CHAIR-M twice a week for 15 minutes, and observed a significant reduction of pain in the lower and upper spine and the right arm, and a slightly smaller improvement in the left shoulder and left forearm.(33) Another Polish study(49) with white-collar workers compared three groups, namely CHAIRM, music therapy, and control groups, to evaluate the effect of chair massage and music therapy on relaxation, tension, and heart rate by algometry. The results showed statistically significant increases in relaxation and a decrease in tension for the two interventions, with better results for the CHAIR-M group which was applied for 15 minutes twice a week for four weeks. The effect of CHAIR-M was also applied for prophylaxis of musculoskeletal pain in student musicians compared to control and exercise groups, with two sessions a week of 15 minutes for two weeks. The results showed that both exercises and CHAIR-M increased the pain threshold between 20% and 28%.(50)
A meta-analysis carried out on the efficacy of the massage therapy for pain management showed that it should be strongly recommended compared to no treatment, and it was weakly recommended compared to placebo or an active comparator (i.e., physical therapy and acupuncture).(31)
The action mechanism of the massage is not completely clear. In the Gate Control Theory, the pressure stimulus from the massage reaches the brain more quickly than the pain stimulus, “closing the gate”, thus blocking the pain stimulus. Another theory postulates that the massage induces deep sleep, reducing the Substance P, which is responsible for pain transmission. The massage increases the serotonin levels, causing a decrease in Substance P, and favors reducing cortisol, in turn reducing stress. Cortisol reduction would be associated with moderate pressure and with the mechanoreceptors triggered by the massage. There is an increase in vagal activity, and a signal is emitted to the limbic system and hypothalamic structures, reducing cortisol secretion.(29)
Strengths and Limitations
There was no change in the profile of the patients assisted, staff sizing, financial recognition, or in the establishment of career plans in the participating institutions during the care period. The strength of this study is its randomized and controlled design, the training of the persons to deliver the massage sessions, and the CHAIR-M protocol. The limitations of this study were: new recruitment to complete the sample size; a small number of participants who reported pain; no follow-up of the participants to assess the beneficial CHAIR-M duration; changing in the setting where the massage was applied in some sessions due to the room being unavailable; not excluding participants using analgesics.
The outcomes evidenced that this practice can be implemented in health services to improve workers’ health to relieve stress and musculoskeletal pain. Future research can show the impact of CHAIR-M on absenteeism reduction and quality of care.
CONCLUSION
The CHAIR-M was effective in reducing chronic stress in the Oncology Nursing team as measured by the LSS. Its effectiveness on pain was observed in interference of musculoskeletal pain mainly in general activity and normal work, according to the BPI, but also showed good results in mood and sleep. The proposed protocol and six sessions of intervention time of 15 minutes proved adequate to relieve signs and symptoms of stress and partially of musculoskeletal pain in the nursing team.
ACKNOWLEDGMENTS
Special thanks to the nursing team that participated in this research.
Footnotes
CONFLICT OF INTEREST NOTIFICATION
The authors declare no conflicts of interest, personally or related to funding. The study was funded by the Research Support Foundation of the state of São Paulo (process No. 2017/19,645-2).
REFERENCES
- 1.Magalhães AM, Costa DG, Riboldi CO, Mergen T, Barbosa AS, Moura GM. Association between workload of the nursing staff and patient safety outcomes. Rev Esc Enferm USP. 2017;51:e03255. doi: 10.1590/s1980-220x2016021203255. [DOI] [PubMed] [Google Scholar]
- 2.Loro MM, Zeitoune RCG. Collective strategy for facing occupational risks of a nursing team. Rev Esc Enferm USP. 2017;51:e03205. doi: 10.1590/s1980-220x2015027403205. [DOI] [PubMed] [Google Scholar]
- 3.Machado MH, Santos de Oliveira E, Lemos WR, Wermelinger MW, Vieira M, dos Santos MR, et al. Pesquisa Perfil da Enfermagem no Brasil: Relatório Final. Rio de Janeiro, Brazil: Nerhus-Daps-Ensp/Fiocruz; 2017. [Accessed 2021 Jun 20]. Available from: http://www.cofen.gov.br/perfilenfermagem/pdfs/relatoriofinal.pdf. [Google Scholar]
- 4.Ribeiro RP, Marziale MH, Martins JT, Galdino MJ, Ribeiro PHV. Occupational stress among health workers of a university hospital. Rev Gaúcha Enferm. 2018;39:e65127. doi: 10.1590/1983-1447.2018.65127. [DOI] [PubMed] [Google Scholar]
- 5.Silva-Júnior JS. Preventing occupational stress in healthcare workers. Sao Paulo Med J. 2016;134(1):92. doi: 10.1590/1516-3180.20161341T1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haeffner R, Kalinke LP, Felli VEA, Mantovani MF, Consonni D, Sarquis LM. Absenteeism due to musculoskeletal disorders in Brazilian workers: thousands of days missed at work. Rev Bras Epidemiol. 2018;21:e180003. doi: 10.1590/1980-549720180003. [DOI] [PubMed] [Google Scholar]
- 7.Yan P, Yang Y, Zhang L, Li F, Huang A, Wang Y, et al. Correlation analysis between work-related musculoskeletal disorders and the nursing practice environment, quality of life, and social support in the nursing professionals. Medicine. 2018;97(9):e0026. doi: 10.1097/MD.0000000000010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cargnin ZA, Schneider DG, Vargas MAO, Machado RR. Non-specific low back pain and its relation to the nursing work process. Rev Latinoam Enferm. 2019;27:e3172. doi: 10.1590/1518-8345.2915.3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Public Health. 2019;16(1):61. doi: 10.3390/ijerph16010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vahedian-Azimi A, Hajiesmaeili M, Kangasniemi M, Fornes-Vives J, Hunsucker RL, Rahimibashar F, et al. Effects of stress on critical care nurses: a national cross-sectional study. J Intensive Care Med. 2019;34(4):311–322. doi: 10.1177/0885066617696853. [DOI] [PubMed] [Google Scholar]
- 11.Sharma N, Takkar P, Purkayastha A, Jaiswal P, Taneja S, Lohia N, et al. Occupational stress in the Indian Army oncology nursing workforce: a cross-sectional study. Asia Pac J Oncol Nurs. 2018;5(2):237–243. doi: 10.4103/apjon.apjon_61_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ko W, Kiser-Larson N.Stress levels on nurses in oncology outpatients units Clin J Oncol Nurs 2016; 202158–164. 10.1188/16.CJON.158-164 [DOI] [PubMed] [Google Scholar]
- 13.Ratochinski CM, Powlowytsch PW, Grzelczak MT, Souza WC, Mascarenhas LP, Gomes LP. Stress in nursing professionals: a systematic review. Rev Bras Ciên Saúde. 2016;20(4):341–346. [Google Scholar]
- 14.Kowalczuk K, Krajewska-Kułak E, Sobolewski M. Factors determining work arduousness levels among nurses: using the example of surgical, medical treatment, and emergency wards. Biomed Res Int. 2019;2019:6303474. doi: 10.1155/2019/6303474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pozzebon D, Piccin CF, Da Silva AM, Corrêa EC. Relationship among perceived stress, anxiety, depression and craniocervical pain in nursing professionals under stress at work. Fisioter Mov. 2016;29(2):377–385. doi: 10.1590/0103-5150.029.002.AO17. [DOI] [Google Scholar]
- 16.Kaburi BB, Bio FY, Kubio C, Ameme DK, Kenu E, Sackey SO, et al. Psychological working conditions and predictors of occupational stress among nurses, Salaga Government Hospital, Ghana, 2016. Pan Afr Med J. 2019;33:320. doi: 10.11604/pamj.2019.33.320.16147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bordignon M, Monteio MI. Violence in the work-place in nursing: consequences overview [in Portuguese] Rev Bras Enferm. 2016;69(5):939–942. doi: 10.1590/0034-7167-2015-0133. [DOI] [PubMed] [Google Scholar]
- 18.Morais BX, Pedro CM, Dalmolin GL, Silva AM. Professional satisfaction of nursing workers from a service of hematology-oncology [in Portuguese] Rev Rene. 2018;19:e3165. doi: 10.15253/2175-6783.2018193165. [DOI] [Google Scholar]
- 19.Bastos RA, Quintana AM, Carnevale F. Psychological distress experienced by nurses who work with patients in death process: a clinical-qualitative study. Trends Psychol. 2018;26(2):795–805. [Google Scholar]
- 20.Cañadas-De la Fuente GA, Gómez-Urquiza JL, Ortega-Campos EM, Cañadas GR, Albendín-García L, De la Fuente-Solana EI. Prevalence of burnout syndrome in oncology nursing: a meta-analytic study. Psychooncology. 2018;27(5):1426–1433. doi: 10.1002/pon.4632. [DOI] [PubMed] [Google Scholar]
- 21.Carvalho DP, Rocha LP, Barlem JG, Specht J, Dias JS, Schallenberger CD. Workloads and nursing workers’ health: integrative review. Cogitare Enferm. 2017;22(1):1–10. [Google Scholar]
- 22.Santos HE, Marziale MH, Felli VE. Presenteeism and musculoskeletal symptoms among nursing professionals. Rev Lat Am Enferm. 2018;26:e3006. doi: 10.1590/1518-8345.2185.3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee SJ, Lee JH, Gershon RR. Musculoskeletal symptoms in nurses in the early implementation phase of California’s Safe Patient Handling Legislation. Res Nurs Health. 2015;38(3):183–193. doi: 10.1002/nur.21657. [DOI] [PubMed] [Google Scholar]
- 24.Borges TP, Kurebayashi LF, Silva MJ. [Lombalgia ocupacional em trabalhadores de enfermagem: massagem versus dor]. Rev Esc Enferm USP. 2014;48(4):699–675. doi: 10.1590/S0080-623420140000400014. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim ME, Cheval B, Cullati S, Mongin D, Lauper K, Pihl-Thingvad J, et al. Back pain occurrence and treatment-seeking behavior among nurses: the role of work-related emotional burden. Qual Life Res. 2020;29(5):1301–1310. doi: 10.1007/s11136-019-02405-4. [DOI] [PubMed] [Google Scholar]
- 26.Fujii T, Oka H, Takano K, Asada F, Nomura T, Kawamata K, et al. Association between high fear-avoidance beliefs about physical activity and chronic disabling low back pain in nurses in Japan. BMC Musculosketet Disord. 2019;20(1):572. doi: 10.1186/s12891-019-2965-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buscemi V, Chang W, Liston MB, McAuley JH, Schabrun SM. The role of perceived stress and life stressors in the development of chronic musculoskeletal pain disorders: a systematic review. J Pain. 2019;20(10):1127–1139. doi: 10.1016/j.jpain.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 28.Mahdizadeh M, Jaberi AA, Bonabi TN. Massage therapy in management of occupational stress in emergency medical services staffs: a randomized controlled trial. Int J Ther Massage Bodywork. 2019;12(1):16–34. [PMC free article] [PubMed] [Google Scholar]
- 29.Field T. Massage therapy research review. Complement Ther Clin Pract. 2016;24:19–31. doi: 10.1016/j.ctcp.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurebayashi LF, Turrini RN, Souza TP, Takiguchi RS, Kuba G, Nagumo MT. Massage and Reiki used to reduce stress and anxiety: randomized clinical trial [in Portuguese] Rev Lat Am Enferm. 2016;24:e2834. doi: 10.1590/1518-8345.1614.2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crawford C, Boyd C, Paat CF, Price A, Xenakis L, Yang E, et al. The impact of massage therapy on function in pain populations: a systematic review and meta-analysis of randomized controlled trials: Part I, Patients experiencing pain in the general population. Pain Med. 2016;17(7):1353–1375. doi: 10.1093/pm/pnw099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brennan MK, De Bate RD. The effect of chair massage on stress perception of hospital bedside nurses. J Bodyw Mov Ther. 2006;10(4):335–342. doi: 10.1016/j.jbmt.2005.11.003. [DOI] [Google Scholar]
- 33.Cabak A, Kotynia P, Banasinski M, Obminski Z, Tomaszewski W. The concept of “chair massage” in the workplace as prevention of musculoskeletical overload and pain. Ortop Traumatol Rehab. 2016;18(3):279–288. doi: 10.5604/15093492.1212997. [DOI] [PubMed] [Google Scholar]
- 34.Ondrejkovicova A, Petrovics G, Svitkova K, Bajtekova B, Bangha O. Why acupuncture in pain treatment? NeuroEndocrinol Lett. 2016;37(3):163–168. [PubMed] [Google Scholar]
- 35.Engen DJ, Wahner-Roedler DL, Vincent A, Chon TY, Cha SS, Luedtke CA, et al. Feasibility and effect of chair massage offered to nurses during work hours on stress-related symptoms: a pilot study. Complement Ther Clin Pract. 2012;18(4):212–215. doi: 10.1016/j.ctcp.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 36.Ferreira EAG, Vasconcellos EG, Marques AP. Assessment of pain and stress in fibromyalgia patients. Rev Bras Reumatol. 2002;42(2):104–110. [Google Scholar]
- 37.Rio OFL. dissertação. São Paulo: Pontifícia Universidade Católica de São Paulo; 2006. p. 96. [Google Scholar]
- 38.Ferreira KA, Teixeira MJ, Mendonza TR, Cleeland CS. Validation of brief pain inventory to Brazilian patients with pain. Support Care Cancer. 2011;19(4):505–511. doi: 10.1007/s00520-010-0844-7. [DOI] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 40.Sedaghat AR. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. 2019;161(4):551–560. doi: 10.1177/0194599819852604. [DOI] [PubMed] [Google Scholar]
- 41.Prado JM, Kurebayashi LF, Silva MJ. Experimental and placebo auriculotherapy for stressed nurses: randomized controlled trial [in Spanish] Rev Esc Enferm USP. 2018;52:e03334. doi: 10.1590/S1980-220X2017030403334. [DOI] [PubMed] [Google Scholar]
- 42.Ribeiro RP, Marziale MH, Martins JT, Ribeiro PH, Robazzi ML, Dalmas JC. Prevalence of Metabolic Syndrome among nursing personnel and its association with occupational stress, anxiety and depression. Rev Lat Am Enferm. 2015;23(3):435–440. doi: 10.1590/0104-1169.0383.2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li M, Shu Q, Huang H, Bo W, Wang L, Wu H. Associations of occupational stress, workplace violence and organizational support on chronic fatigue symptoms among nurses. J Adv Nurs. 2020;76(5):1151–1161. doi: 10.1111/jan.14312. [DOI] [PubMed] [Google Scholar]
- 44.Rodrigues CC, Santos VEP, Sousa P. Patient safety and nursing: interface with stress and Burnout Syndrome. Rev Bras Enferm. 2017;70(5):1083–1088. doi: 10.1590/0034-7167-2016-0194. [DOI] [PubMed] [Google Scholar]
- 45.Maciel EG, Júnior, Trombini-Souza F, Maduro PA, Mesquita FOS, Silva TF. Self-reported musculoskeletal disorders by the nursing team in a university hospital. BrJP. 2019;2(2):155–158. [Google Scholar]
- 46.Santos PM, Martins R, Serranheira F. Low back pain prevalence in nurses in hospital context [in Portuguese] Gestão Desenv. 2016;24:161–171. doi: 10.7559/gestaoedesenvolvimento.2016.289. [DOI] [Google Scholar]
- 47.Arrais PS, Fernandes ME, Pizzol TS, Ramos LR, Mengue SS, Luiza VL, et al. Prevalência de medicação no Brasil e fatores associados. Rev Saúde Pública. 2016;50(supl2):13s. doi: 10.1590/S1518-8787.2016050006117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hand ME, Margolis J, Staffileno BA. Massage chair sessions: favorable effects on ambulatory cancer center nurses’ perceived level of stress, blood pressure, and heart rate. Clin J Oncol Nurs. 2019;23(4):375–381. doi: 10.1188/19.CJON.375-381. [DOI] [PubMed] [Google Scholar]
- 49.Cabak A, Mikicin M, Lyp M, Stanislawska I, Kaczor R, Tomaszewski W. Preventive chair massage with algometry to maintain psychosomatic balance in white-collar workers. Adv Exp Med Biol. 2017;1022:77–84. doi: 10.1007/5584_2017_45. [DOI] [PubMed] [Google Scholar]
- 50.Cygánska A, Truszczynska-Baszak A, Tomaszewski P. Impact of exercises and chair massage on musculoskeletal pain of young musicians. Int J Environ Res Public Health. 2020;17(14):5128. doi: 10.3390/ijerph17145128. [DOI] [PMC free article] [PubMed] [Google Scholar]