Abstract
The purpose of this study was to evaluate the impact of access to communication technology on caregiver quality of life, neurodevelopmental, and medical outcomes (eg, rehospitalization, emergency room visits, or surgeries) in preterm infants, and enrollment in public assistance programs. In this cross-sectional study, we surveyed families of preterm infants in a high-risk infant-follow-up clinic. We estimated associations of access to various modes of communication technology with outcomes, adjusting for sociodemographic and infant characteristics using linear and unconditional logistic regression. Access to email, text messaging, and smartphones was associated with higher quality of life scores on the Multicultural Quality of Life Index, and email and smartphone access was significantly associated with increased enrollment in early intervention. Evaluating smartphone and email access on neonatal intensive care unit discharge is important when considering enrollment in community programs and caregiver quality of life.
Keywords: follow-up, early intervention, SSI, prematurity, high-risk infant, post-discharge, outcomes, smartphone, texting, emailing
Introduction
Transitioning from the highly technological and closely monitored environment of the neonatal intensive care unit (NICU) to home can place a great deal of stress on families struggling to adjust to the new demands of taking care of a baby with potentially complex medical needs.1,2 The psychological and emotional stress that parents encounter while in the NICU is well documented,3,4 and this stress can continue to affect the family in different ways after their infant is discharged.5,6 Relationships within the family may become strained, the financial burden on the family may increase, and families may struggle to find adequate social support during this time.7 Issues with uncertainty of how to take care of the baby and understand their needs, lingering medical concerns and unanswered questions, and differing parental concerns and coping mechanisms all contribute to a higher level of stress than would be otherwise expected for new parents of a baby with no complex medical problems.7 All these stressors may be magnified in low-income and minority families, whose lower resource pool may make mitigation of these stressors more difficult.8,9
Information and communication technology, which may have a potentially significant, and largely unstudied, impact on parents and their feelings of stress at home, is a novel approach to supporting parents in the discharge process. Seventy-seven percent of Americans own a smartphone, and 90% of American adults use the Internet.10 Reliance on smartphones for Internet access has been found to be more prevalent among younger adults, non-whites, and lower income individuals.10 Parents today, in particular, parents of children with complex medical conditions, actively use communication technology such as smartphones, the Internet, email, and texting to access information regarding their child’s condition, reach out to their support network, and communicate with their primary pediatrician.11–13 Parents of infants who are admitted to or have been discharged from the NICU may benefit from this same type of access.
However, there is limited information as to whether access to technology can attenuate burdens for low-income families in particular. The majority of the studies in the literature pertaining to the use of communication technology and patients admitted to the NICU have focused on enhancing nursing communication and discharge teaching with parents, providing support to parents after discharge, and exploring what families are using technology for.12–16 No studies, to date, have investigated the impact that access to technology has on the quality of life of these patients’ caregivers following discharge. Information technology has an increasing presence in many aspects of medical care, but information technology ownership and its utility in increasing quality of life and accessing community services in low-income families has not been well established. Our study aimed to (1) describe access to various forms of technology for communication, identify whether certain forms of technology are associated with improved parent quality of life; (2) better infant medical and neurodevelopment outcomes; (3) increased enrollment in community-based programs such as early intervention; and (4) increase enrollment in income/food assistance programs at a safety net hospital, one which provides care to all patients regardless of ability to pay, including those that are undocumented, uninsured, and vulnerable.17
Methods
Study Design and Participants
This cross-sectional study involved administering a 120-item questionnaire/survey to participants. The survey contained validated components in English and Spanish and queried families about life after discharge from the NICU. The Spanish version of the questionnaire and an interpreter were used if English was not the parent’s primary language. We enrolled one parent (mother or father) of preterm (<37 weeks gestation) infants attending a high-risk infant-follow-up clinic at a quaternary urban children’s hospital between 2013 and 2015. This clinic provides multidisciplinary medical and neurodevelopmental follow-up for infants with gestational age <32 completed weeks or birth weight <1500 g. We included English- or Spanish-speaking parents of preterm infants who were up to 24 months corrected age (from term equivalent) with completed developmental assessments. If the infant was one of a multiple gestation, only one response was collected from the family. Consent was obtained when the parent agreed to complete the questionnaire, which was administered via laptop, in person, or by telephone. Participants were provided a small incentive (a $10 gift card) to complete the survey. The Children’s Hospital Los Angeles Human Subjects Protection Program approved the study protocol. Of the 199 eligible participants, 169 answered the questionnaire (85% response rate) and 89 completed the developmental assessments (64 presented at fewer than 6 months of age).
Measurements
The measurements of primary outcomes and parental access to various forms of communication technology are summarized below.
Questionnaire.
The survey assessed both access to and frequency of use of the following communication technology modalities: access to the Internet, email, and text and ownership of a smartphone. The survey also included a validated quality of life measure, the Multicultural Quality of Life Index (MCQLI).
Access to Forms of Communication Technology.
Parents were asked about both their access to and frequency of use of the following communication technology modalities following discharge from the NICU: access to the Internet, email, and text and ownership of a smartphone. Parents were permitted to select more than one modality.
Multicultural Quality of Life Index.
Parents completed the MCQLI as part of the survey. The MCQLI is a brief and culturally informed self-rated instrument consisting of 10 items that address key aspects of quality of life (eg, physical well-being and social emotional support).18 The survey was developed by paying particular attention to ethnic diversity and considers cultural background in its rating of quality of life. It has wide applicability across a variety of clinical conditions and has been translated and validated in multiple languages, including Spanish.19 Higher scores on the survey indicate higher quality of life as rated by the subject.
Review of Medical Records.
We obtained information from the patients’ medical records regarding delivery and complications during the neonatal hospitalization. We collected data regarding gestational age, birth weight, and diagnoses. We also reviewed the outpatient high-risk infant-follow-up clinic notes and recorded the Bayley scales and Vineland language scores at each visit.
Neurodevelopmental Assessment.
We assessed early development using the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III), which is the most widely used tool for assessing early development.20 The Bayley-III was administered as part of routine clinical care by doctoral-level psychologists (cognitive scale) and physical therapists (motor scale, comprising fine, and gross motor subtests). The primary objective of the Bayley-III is to “identify children with developmental delay and to provide information for intervention planning” through individually administered assessment of children aged 1 to 42 months. The Bayley-III has 5 distinct scales to better align with government guidelines regarding early childhood assessment: Cognitive (91 items), Language (97 items), and Motor scales (138 items), and caregiver ratings of Social-Emotional (35 items) and Adaptive Behavior (241 items). There is also a separation of assessment of cognitive, expressive language (48 items), and receptive language (49 items) skills, as well as the separation of fine (66 items) and gross (72 items) motor tasks, into subtests with explicit normative data.20,21 The Bayley-III has an age-corrected mean score of 100 with a standard deviation of 15; and higher scores indicate better development.
The Vineland Adaptive Behavior Scale II.
We assessed personal skills, social skills, and communication using the Vineland Adaptive Behavior Scales, Second Edition (VABS-II), in Spanish-speaking patients.22 Because adaptive behavior refers to an individual’s typical performance of the day-to-day activities required for personal and social sufficiency, these scales assess what a person actually does rather than what he or she is able to do. The VABS-II assesses adaptive behavior in 4 domains: Communication, Daily Living Skills, Socialization, and Motor Skills. It also provides a composite score that summarizes the individual’s performance across all 4 domains. The VABS-II has an age-corrected mean score of 100 and a standard deviation of 15; and higher scores indicate better function.22,23
Enrollment in Public Assistance Programs.
Participants were asked yes/no questions about the use of community-based developmental resources such as EI programs, use of social services such as food assistance programs (enrollment in the Supplemental Nutrition Assistance Program or Supplemental Nutrition Assistance Program for Women, Infants and Children), the Low Income Home Energy Assistance Program, Transitional Aid to Needy Families (TANF), and Supplemental Security Income (SSI) since discharge from the NICU. Self-report for enrollment in public assistance programs has been validated in other studies.24,25 These questions were adapted from HelpSteps, a survey designed to identify health-related social problems. The development of HelpSteps involved a literature review and key informant interviews with health and social services experts to produce an initial list of 25 social domains.26 Of these domains, the 5 most relevant were identified using a modified Delphi technique: (1) access to health care, (2) housing, (3) food security, (4) income security, and (5) intimate partner violence. Details about the HelpSteps survey appear in previous studies.26–30
Statistical Analysis
We described the characteristics of the study population using means and proportions. We compared the frequency of covariates (race/ethnicity, maternal education, language, income level, infant birth weight, neonatal comorbidities, post-discharge diagnoses, and medical technology) across various technological modalities (access to the Internet, email, text messaging, and owning a smartphone). P values were obtained from t tests for 2-category comparisons and analysis of variance if there were more than 2 categories. The Spearman correlation coefficient was used to test for correlations between the Bayley-III scores and continuous covariates.
Linear regression was used to evaluate the adjusted association between the use of technology and quality of life scores. Means (standard error) are presented, and adjusted differences in scores follow. Linear regression was also used to compare neurodevelopmental scores between groups. Unconditional multiple logistic regression was used to evaluate the association between technology use and medical outcomes and enrollment in public assistance programs after adjusting for confounders. Covariates that changed the β coefficients by 10% were retained in the multivariable models. Standard testing for collinearity (tolerance and variance inflation factor) revealed that collinearity in the multivariable model did not affect the standard error of the models. Beta coefficients (linear regression results) for neurodevelopmental scores and odds ratios (ORs) with 95% confidence intervals (CIs) and 2-sided P values for individual variable categories are reported.
To evaluate goodness of fit of the linear multivariable model, we evaluated the F test and R2 for the linear models. For the logistic regression model, we used the Hosmer and Lemeshow X2 goodness-of-fit test; we did not find any statistically significant departure from the fit. Standard procedures were used for both linear and logistic regression model diagnostics, and we found no substantial deviation from the goodness of fit. To identify whether income assistance or infant chronologic age was an effect modifier for food assistance (stratified analysis), we fit linear and unconditional logistic regression models containing a multiplicative interaction term.
All the statistical analyses were carried out using SAS, v 9.4 (SAS Institute, Cary, NC).
Results
Sixty-six percent of the survey participants were Hispanic, and 62% were non-English-speaking (Table 1). Seventy-five percent of the sample had an annual income less than $40 000. Thirty percent of the mothers had attained a high school level of education or less. Sixty-two percent of the infants were born earlier than 32 weeks, and 56% had a birth weight of less than 1500 g. The median (interquartile range) chronologic age was 14 months (8). Sixty-one percent had a neonatal comorbidity, defined as at least one diagnosis of fetal growth restriction, surfactant deficiency, necrotizing enterocolitis, intraventricular hemorrhage grade 3 or 4, patent ductus arteriosus, or retinopathy of prematurity. Seventy-three percent of infants had more than 2 clinic appointments per month; 29% required medical equipment such as supplemental oxygen or feeding tube on discharge; and 64% had a post-discharge diagnosis, defined as at least one diagnosis of autism, global developmental delay, or cerebral palsy.
Table 1.
Sociodemographics and Infant Characteristics With Use of Internet/Email and Mobile Technology (n = 169).
| Use of Internet, n (%) |
Use of Email, n (%) |
Use of Smartphone, n (%) |
Use of Texting, n (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Yes | No | P | Yes | No | P | Yes | No | P | Yes | No | P | |
|
| |||||||||||||
| Sociodemographics | |||||||||||||
| Person completing survey | |||||||||||||
| Mother | 156 | 118 (92.9) | 38 (95.0) | .99 | 107 (93.0) | 49 (94.2) | .77 | 120 (95.2) | 36 (87.8) | .10 | 135 (95.7) | 21 (80.8) | .02 |
| Father | 11 | 9 (7.1) | 2 (5.0) | 8 (7.0) | 3 (5.8) | 6 (4.8) | 5 (12.2) | 6 (4.3) | 5 (19.2) | ||||
| Race/ethnicity | |||||||||||||
| White non-Hispanic | 10 | 9 (7.7) | 1 (2.8) | .11 | 9 (8.3) | 1 (2.2) | .42 | 9 (7.8) | 1 (2.7) | .37 | 9 (6.9) | 1 (4.3) | .10 |
| Hispanic | 111 | 79 (67.5) | 32 (88.9) | 75 (69.4) | 36 (80.0) | 86 (74.1) | 25 (67.6) | 98 (75.4) | 13 (56.5) | ||||
| Black non-Hispanic | 16 | 14 (12.0) | 2 (5.6) | 11 (10.2) | 5 (11.1) | 10 (8.6) | 6 (16.2) | 12 (9.2) | 4 (17.4) | ||||
| Other | 16 | 15 (12.8) | 1 (2.8) | 13 (12.0) | 3 (6.7) | 11 (9.5) | 5 (13.5) | 11 (8.5) | 5 (21.7) | ||||
| Income ($/year) | |||||||||||||
| Less than $20 000 | 91 | 60 (50.0) | 31 (83.8) | .001 | 56 (50.9) | 32 (74.5) | .04 | 67 (56.3) | 24 (63.2) | .46 | 80 (60.2) | 11 (45.8) | .22 |
| $20 00l-$40 000 | 35 | 33 (27.5) | 2 (5.4) | 29 (26.4) | 6 (12.8) | 28 (23.5) | 7 (18.4) | 28 (21.0) | 7 (29.2) | ||||
| $40 00l-$60 000 | 14 | 13 (10.8) | 1 (2.7) | 11 (10.0) | 3 (6.4) | 10 (8.4) | 4 (10.5) | 11 (8.3) | 3 (12.5) | ||||
| $60 00l-$80 000 | 9 | 6 (5.0) | 3 (8.1) | 6 (5.5) | 3 (6.4) | 6 (5.0) | 3 (7.9) | 6 (4.5) | 3 (12.5) | ||||
| More than $80 000 | 8 | 8 (6.7) | 0 (0) | 8 (7.3) | 0 (0) | 8 (6.7) | 0 (0) | 8 (6.0) | 0 (0) | ||||
| Maternal education | |||||||||||||
| ≤High school | 50 | 40 (36.4) | 10 (35.7) | .95 | 33 (32.7) | 17 (46.0) | .15 | 40 (36.7) | 10 (34.5) | .82 | 44 (37.3) | 6 (30.0) | .53 |
| At least some college | 88 | 70 (63.6) | 18 (64.3) | 68 (67.3) | 20 (54.0) | 69 (63.3) | 19 (65.5) | 74 (62.7) | 14 (70.0) | ||||
| Language | |||||||||||||
| Non-English | 104 | 75 (63.6) | 29 (78.4) | .09 | 66 (60.6) | 38 (82.6) | .008 | 74 (62.7) | 30 (81.1) | .04 | 87 (65.9) | 17 (73.9) | .45 |
| English | 51 | 43 (36.4) | 8 (21.6) | 43 (39.4) | 8 (17.4) | 44 (37.3) | 7 (18.9) | 45 (34.1) | 6 (26.1) | ||||
| Infant characteristics | |||||||||||||
| Birthweight (g) | |||||||||||||
| Mean (SD) | 169 | 1111 (606) | 1197 (648) | .52 | 1070 (543) | 1337 (786) | 1124 (631) | 1165 (544) | .23 | 1135 (615) | 1090 (633) | .81 | |
| ≤1000 | 62 | 49 (55.1) | 13 (46.4) | .52 | 51 (56.7) | 11 (40.7) | .11 | 51 (53.1) | 11 (52.4) | .88 | 54 (50.9) | 8 (72.7) | .36 |
| ≥1000 to <1500 | 32 | 23 (25.8) | 9 (32.1) | 23 (25.6) | 9 (33.3) | 27 (28.1) | 5 (23.8) | 31 (29.2) | 1 (9.1) | ||||
| ≥ 1500 to <2500 | 16 | 13 (14.6) | 3 (10.7) | 13 (14.4) | 3 (11.1) | 12 (12.5) | 4 (19.1) | 15 (14.2) | 1 (9.1) | ||||
| ≥2500 | 7 | 4 (4.5) | 3 (10.7) | 3 (3.3) | 4 (14.8) | 6 (6.3) | 1 (4.8) | 6 (5.7) | 1 (9.1) | ||||
| Gestational age (weeks) | |||||||||||||
| Mean (SD) | 27.7 (3.2) | 28.9 (3.4) | .09 | 27.6 (3.3) | 29.4 (3.0) | .009 | 27.8 (3.3) | 28.8 (3.4) | .78 | 27.9 (3.3) | 28.7 (3.4) | .48 | |
| <28 | 56 | 44 (46.8) | 12 (38.7) | .10 | 46 (48.9) | 10 (32.3) | .35 | 42 (41.6) | 14 (58.3) | .05 | 48 (42.5) | 8 (66.7) | .04 |
| ≥28 to <32 | 48 | 36 (38.3) | 12 (38.7) | 34 (36.2) | 14 (45.1) | 44 (43.6) | 4 (16.7) | 47 (41.6) | 1 (8.3) | ||||
| ≥32 to <34 | 13 | 11 (11.7) | 2 (6.5) | 9 (9.6) | 4 (12.9) | 10 (9.9) | 3 (12.5) | 12 (10.6) | 1 (8.3) | ||||
| ≥34 to <37 | 8 | 3 (3.2) | 5 (16.1) | 5 (5.3) | 3 (9.7) | 5 (4.9) | 3 (12.5) | 6 (5.3) | 2 (16.7) | ||||
| Infant chronologic age | 12.0 (6.7) | 11.9 (7.4) | .97 | 11.8 (6.7) | 12.2 (7.6) | .80 | 11.9 (6.4) | 12.1 (8.6) | .88 | 11.9 (6.7) | 12.4 (8.7) | .80 | |
| Mean (SD) | |||||||||||||
| Neonatal comorbiditiesa | |||||||||||||
| Yes | 103 | 79 (61.2) | 24 (60.0) | .89 | 79 (67.5) | 24 (46.2) | .009 | 83 (64.8) | 20 (48.8) | .07 | 93 (65.0) | 10 (38.5) | .01 |
| No | 66 | 50 (38.8) | 16 (40.0) | 38 (32.5) | 28 (53.9) | 45 (35.2) | 21 (51.2) | 50 (35.0) | 16 (61.5) | ||||
| ≥2 clinic appointments/month | |||||||||||||
| Yes | 124 | 95 (74.2) | 29 (74.4) | .99 | 88 (75.2) | 36 (72.0) | .66 | 94 (73.4) | 30 (76.9) | .66 | 104 (73.2) | 20 (80.0) | .62 |
| No | 43 | 33 (25.8) | 10 (25.6) | 29 (24.8) | 14 (28.0) | 34 (26.6) | 9 (23.1) | 38 (26.8) | 5 (20.0) | ||||
| Use of medical equipmentb | |||||||||||||
| Yes | 49 | 37 (28.7) | 12 (30.0) | .87 | 33 (28.2) | 16 (30.8) | .73 | 39 (30.5) | 10 (24.4) | .46 | 40 (28.0) | 9 (34.6) | .49 |
| No | 120 | 92 (71.3) | 28 (70.0) | 84 (71.8) | 36 (69.2) | 89 (69.5) | 31 (75.6) | 103 (72.0) | 17 (65.4) | ||||
| Post-discharge diagnosesc | |||||||||||||
| Yes | 108 | 81 (86.2) | 27 (87.1) | .99 | 83 (88.3) | 25 (80.7) | .28 | 88 (87.1) | 20 (83.3) | .74 | 98 (86.7) | 10 (83.3) | .67 |
| No | 17 | 13 (13.8) | 4 (12.9) | 11 (11.7) | 6 (19.3) | 13 (12.9) | 4 (16.7) | 15 (13.3) | 2 (16.7) | ||||
Neonatal comorbidities include at least one diagnosis of fetal growth restriction, surfactant deficiency, necrotizing enterocolitis, intraventricular hemorrhage grade 3 or 4, patent ductus arteriosus, and retinopathy of prematurity.
Use of medical equipment includes oxygen, tracheostomy, wheelchair, adaptive stroller, and feeding tube.
Post-discharge diagnoses include at least one diagnosis of autism, global developmental delay, and cerebral palsy.
Email, text messaging, and owning a smartphone were associated with higher quality of life scores on the MCQLI scale, as were adjusted differences between groups (Table 2). There was no significant change in the Bayley-III or Vineland neurodevelopmental scale scores between parents with and without access to the Internet, email, mobile technology, and texting after adjusting for race, maternal education, language spoken at home, annual income, age, birth weight, post-discharge diagnosis, comorbidities, use of medical equipment, and enrollment in EI (Table 3). There was also no significant difference between access to communication technology and medical outcomes such as readmission, emergency room visits, or need for surgery after adjusting for the variables mentioned above (Table 4).
Table 2.
Association of Parent Quality of Life and Access to Technology Among Parents of High-Risk Infants (n = 169).
| Mean (SE) | Mean (SE) | Adjusted Difference Between Groupsa | P | |
|---|---|---|---|---|
|
| ||||
| Characteristic | Internet | No Internet | ||
| MCQLI score | 80.5 (18.2) | 78.1 (25.1) | −0.09 (−7.03, 7.21) | .98 |
| MCQLI score | Email 83.0 (14.7) | No email 72.3 (27.7) | 8.74 (2.24, 15.23) | .009 |
| MCQLI score | Texting 83.4 (15.4) | No texting 58.1 (29.4) | 16.96 (9.10, 4.81) | <.001 |
| MCQLI score | Smartphone 83.2 (15.6) | No smartphone 68.6 (27.8) | 12.01 (5.07, 18.96) | <.001 |
Abbreviations: SE, standard error; MCQLI, Multicultural Quality of Life Index.
Model adjusted for race, maternal education, infant post-discharge diagnoses, use of medical equipment, and enrollment in early intervention.
Table 3.
Adjusted Association of Use of Internet/Mobile Technology and Neurodevelopmental Scores (n = 89)a.
| Change in Bayley-III Composite Cognitive Score (β Coefficient) | 95% CI | P | Change in Bayley-III Composite Motor Score (β Coefficient) | 95% CI | P | Change in Vineland Adaptive Behavior II Score (β Coefficient) | 95% CI | P | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Use of Internet | 3.79 | −5.39, 12.97 | .41 | 1.70 | −7.74, 11.13 | .72 | −4.09 | −11.40, 3.22 | .27 |
| Use of email | −0.25 | −9.89, 9.39 | .96 | 1.98 | −7.86, 11.81 | .69 | −0.68 | −8.41,7.06 | .86 |
| Use of mobile technology (smartphone) | −9.11 | −20.35, 2.12 | .11 | −8.65 | −20.15, 2.86 | .14 | −5.32 | −14.44, 3.81 | .25 |
| Use of text | −4.06 | −17.66, 9.53 | .84 | −3.90 | −17.76, 9.97 | .58 | −0.23 | −10.78, 10.32 | .97 |
Abbreviation: Bayley-III, Bayley Scales of Infant and Toddler Development, Third Edition; CI, confidence interval.
Adjusted for race, maternal education, age, birth weight, post-discharge diagnosis, use of medical equipment, and early intervention.
Table 4.
Adjusted Association of Internet/Mobile Technology and Medical Outcomes (Rehospitalization or Emergency Room Visit; n = 169)a.
| OR | 95% CI | P | |
|---|---|---|---|
|
| |||
| Use of Internet | 0.97 | 0.35–2.66 | .94 |
| Use of email | 0.74 | 0.26–2.06 | .56 |
| Use of mobile technology (smartphone) | 0.42 | 0.13–1.29 | .13 |
| Use of text | 0.80 | 0.18–3.66 | .78 |
Abbreviations: OR, odds ratio; CI, confidence interval.
Adjusted for race, maternal education, age, birth weight, post-discharge diagnosis, use of medical equipment, and early intervention.
As seen in Figure 1, after adjusting for the same factors as above, we found that email and smartphone access was significantly associated with increased enrollment in EI, with an adjusted OR (aOR) of 3.08 and 3.21 (95% CI = 1.31–7.49 and 1.23–8.36, respectively), and having a smartphone was associated with enrollment in SSI or TANF with an adjusted OR (aOR) of 3.35 (95% CI = 1.23–9.23). There was no significant association between use of the Internet or texting and higher MCQLI score or enrollment in public assistance programs (Supplemental Table).
Figure 1.
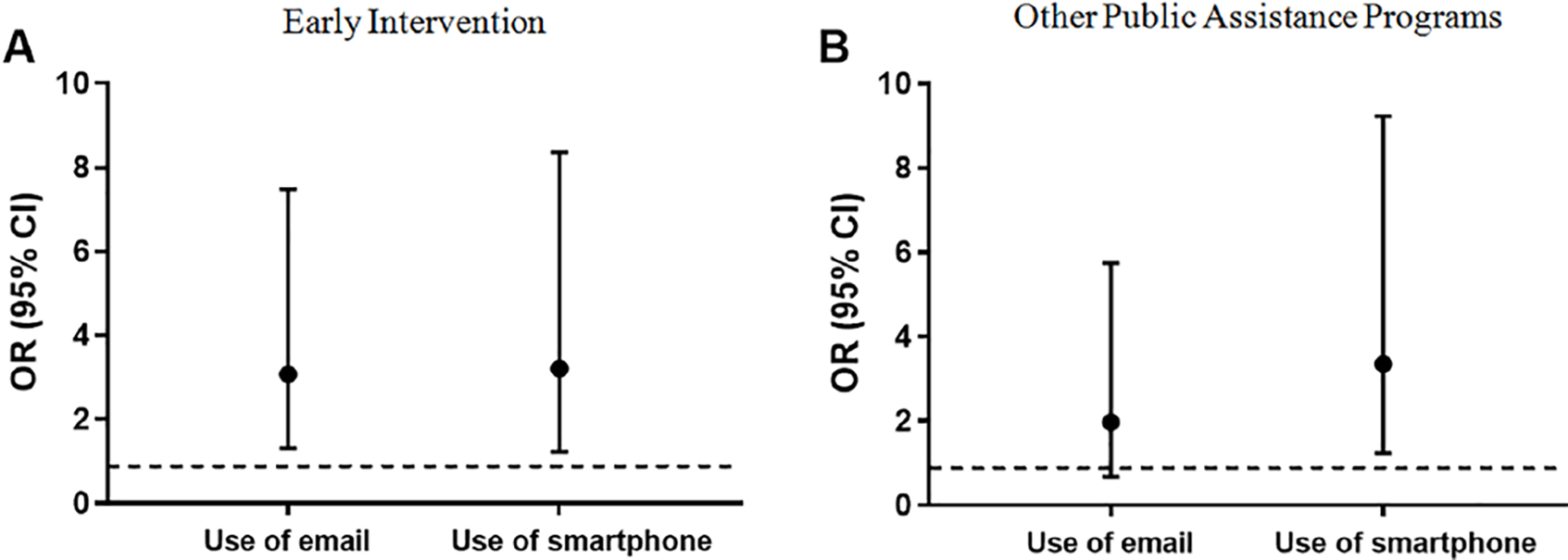
Adjusted association of mobile technology and enrollment in public assistance programs (n = 169). (A) Adjusted association of use of mobile technology and enrollment in early intervention and (B) adjusted association use of mobile technology and enrollment in Supplemental Security Income or Transitional Aid for Needy Families (TANF). Models adjusted for race, maternal education, chronologic age in months, post-discharge diagnosis, use of medical equipment, and early intervention in panel B.
Discussion
In our population of low-income families surveyed after NICU discharge, we found that email and smartphone use was significantly associated with increased scores on the MCQLI scale, indicating that parents with access to these modes of communication technology perceived that they had increased quality of life compared with parents without access. In addition, we found that email access and smartphone ownership was significantly associated with increased enrollment in EI services and that email access was significantly associated with increased enrollment in SSI or TANF. However, there was no difference detected in neurodevelopment as measured by the Bayley Scales or in readmission, emergency room visits, or surgeries between infants whose parents had access to communication technology and those who did not.
Scores on the MCQLI in our population revealed a significant association between email access, smartphone ownership, and texting capability and higher quality of life. The survey is comprehensive in the scope of its questions with regard to various aspects of quality of life. The Pew Research Center, in its analysis of smartphone use in 2015, found that most owners of smartphones view their devices as freeing, connecting, and helpful,10 all of which can contribute to an overall feeling of better quality of life. A review of the literature related to information and communication technology use by adults with chronic medical conditions conducted by Wildevuur and Simonse found that an increase in quality of life and health-related quality of life, possibly by empowering patients and caregivers to take an active role in managing their diseases.31 Furthermore, low-income smartphone owners (with annual household incomes less than $30 000) are more likely to be dependent on the technology compared with owners earning more than $75 000 per year.10 Connections to a support system, social media, and health websites and applications, which may provide respite, reassurance, or information, may also enhance this feeling of better quality of life despite the burden of caring for a medically complex premature infant at home.
No previously published studies to date have investigated any association between neurodevelopmental outcomes and access to various modes of communication technology. Since we did not assess how parents used their technology (eg, searching the Internet for information or calling or texting family members or other caregivers), it is possible that we did not see an impact on neurodevelopmental scores or medical outcomes because of how the technology was used. There are many types of health-related applications that can be accessed via smartphone or the Internet but few that are specific to the NICU population. Text4baby, for example, is a prominent, widely used mobile health application aimed specifically at underserved populations that uses smartphones to communicate important health information and reminders to pregnant women and mothers with infants less than 1 year of age.32–34 The information content is aimed at maintaining a healthy pregnancy, and the application has been associated with increased health behaviors such as flu vaccination.35 However, such applications may not have been of benefit to our patient population.12 While many parents in other studies have reported using the Internet to search for health information related to their child’s diagnosis,16,36,37 it appears that in our population access to this resource did not have an effect on decreasing rates of readmission or emergency room visits. Having access to communication technology may not influence or decrease the quality of time that infants spend with caregivers in activities that stimulate neurodevelopment. Our study is the first to demonstrate that access to technology does not appear to inhibit or enhance an infant’s neurodevelopment. Perhaps, the large range of ages might inhibit findings and the differences may not be apparent in the first 2 years of life.
We also found that there was no association between access to any mode of communication technology and medical outcomes, such as readmission. Readmission rates to the NICU may be more influenced by factors that mobile technology ownership cannot mitigate. For example, previous studies have shown that readmission rates may be a function of the length of stay38 and presence of a system in place to prepare parents with a solid foundation for discharge home.39 It appears that access to communication technology may not be able to replace adequate preparation for discharge and the transition to home.
In our study, email and smartphone use was associated with increased enrollment in community-based EI programs. Children from lower socioeconomic status families are at increased risk for developmental delays. Therefore, engaging with this vulnerable population and ensuring their enrollment in EI programs is of particular importance for neurodevelopmental outcomes.40,41 Previous studies have analyzed predictors of EI enrollment, but none so far have assessed or identified any form of access to communication technology specifically as facilitating or hindering enrollment.42,43 The association we found may be due to increased awareness of the EI program via social media and parent groups and the enhanced ability to research more about the EI program and its benefits. Parents, mothers in particular, turn to the Internet for health and parenting advice for their children, including information about caring for their infants post discharge.44 Ways to enhance and encourage child development may be a popular topic of discussion on social media platforms and online parent resources, and increased access to this topic may motivate parents to seek out programs to help their child. Awareness of these community programs may also be enhanced by communicating, via text or email, with family or friends who are familiar with the programs. Barriers to enrollment such as time away from work, transportation challenges, or being overwhelmed by the stresses of daily life40 with a medically complex infant may be overcome by the convenience of smartphone access and texting or emailing with the parent’s support system.
Our study is one of the first to investigate the association between access to communication technology in low-income families and infant neurodevelopmental outcomes and quality of life. There is growing interest in examining the implementation of communication technology in patient care, and data are lacking about the NICU discharge population. This population is at risk for adverse neurodevelopmental outcomes and creating increased family stress. One strength of this study is that we used a quality of life measure that has been validated in Spanish-speaking populations. Our results are reproducible and generalizable to similar urban low-income populations. Furthermore, the findings from our quality of life measures are consistent with one another, increasing the validity of our findings. Limitations of this study include its potential for suffering from selection bias, specifically self-selection or volunteer bias. However, on examination of the source population (eligible patients from the high-risk infant-follow-up clinic), we found the patient variables were very comparable to our analytic population, which increased the internal validity of our results. Because this study was a cross-sectional investigation, we cannot infer causality. For parents who identified themselves as Hispanic, we did not ask for details about their ancestral background and did not examine for differences in outcome based on native language, although this would be helpful for future studies. Last, our survey did not query parents about how they were using their various forms of communication technology (eg, primarily for social media, communicating with family or other caregivers, or researching health or parenting topics). Future directions for this research would include assessing whether allocating smartphone resources that have been validated in Spanish result in a similar increased quality of life that we observed here and increased enrollment in public assistance programs.
Conclusion
More than 500 000 infants are born prematurely in the United States every year, and 90% of these preterm infants survive to discharge. This situation places a considerable emotional and financial burden on the infants’ caregivers. Lower income families are particularly vulnerable to the effects of this burden. This situation, which can affect the caregivers’ quality of life, may be mitigated by access to communication technology, in particular, smartphone ownership and texting capability. This study supports access to technology as a potential resource for these families to stay connected with their support system or health care providers. Assessing parents’ access to technology prior to the infants being discharged home and possibly providing financial assistance to secure access to technology may be an additional way for providers to ensure families’ well-being and preparedness for the transition home.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was sponsored and supported by the Lucile Packard Foundation for Children’s Health Young Investigator Award for Children with Special Health Care Needs, the Saban Research Career Development Award, and the Confidence Foundation. Dr Lakshmanan is supported by Grant KL2TR001854 from the National Center for Advancing Translational Science (NCATS) of the US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–1126. [DOI] [PubMed] [Google Scholar]
- 2.Turner M, Winefield H, Chur-Hansen A. The emotional experiences and supports for parents with babies in a neonatal nursery. Adv Neonatal Care. 2013;13: 438–446. [DOI] [PubMed] [Google Scholar]
- 3.Purdy IB, Craig JW, Zeanah P. NICU discharge planning and beyond: recommendations for parent psychosocial support. J Perinatol. 2015;35(suppl 1):S24–S28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hynan MT, Mounts KO, Vanderbilt DL. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol. 2013;33: 748–753. [DOI] [PubMed] [Google Scholar]
- 5.Aagaard H, Uhrenfeldt L, Spliid M, Fegran L. Parents’ experiences of transition when their infants are discharged from the neonatal intensive care unit: a systematic review protocol. JBI Database System Rev Implement Rep. 2015;13: 123–132. [DOI] [PubMed] [Google Scholar]
- 6.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281:799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garfield CF, Lee Y, Kim HN. Paternal and maternal concerns for their very low-birth-weight infants transitioning from the NICU to home. J Perinat Neonatal Nurs. 2014;28:305–312. [DOI] [PubMed] [Google Scholar]
- 8.Cronin CM, Shapiro CR, Casiro OG, Cheang MS. The impact of very low-birth-weight infants on the family is long lasting. A matched control study. Arch Pediatr Adolesc Med. 1995;149:151–158. [DOI] [PubMed] [Google Scholar]
- 9.Enlow E, Faherty LJ, Wallace-Keeshen S, Martin AE, Shea JA, Lorch SA. Perspectives of low socioeconomic status mothers of premature infants. Pediatrics. 2017;139:e20161310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith A. US Smartphone Use in 2015. Washington, DC: Pew Research Center; 2015. [Google Scholar]
- 11.Dhillon AS, Albersheim SG, Alsaad S, Pargass NS, Zupancic JA. Internet use and perceptions of information reliability by parents in a neonatal intensive care unit. J Perinatol. 2003;23:420–424. [DOI] [PubMed] [Google Scholar]
- 12.Gabbert TI, Metze B, Bührer C, Garten L. Use of social networking sites by parents of very low birth weight infants: experiences and the potential of a dedicated site. Eur J Pediatr. 2013;172:1671–1677. [DOI] [PubMed] [Google Scholar]
- 13.De Rouck S, Leys M. Illness trajectory and Internet as a health information and communication channel used by parents of infants admitted to a neonatal intensive care unit. J Adv Nurs. 2013;69:1489–1499. [DOI] [PubMed] [Google Scholar]
- 14.Thoren EM, Metze B, Buhrer C, Garten L. Online support for parents of preterm infants: a qualitative and content analysis of Facebook “preemie” groups. Arch Dis Child Fetal Neonatal Ed. 2013;98:F534–F538. [DOI] [PubMed] [Google Scholar]
- 15.Gund A, Sjoqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inform Decis Mak. 2013;13:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plantin L, Daneback K. Parenthood, information and support on the Internet. A literature review of research on parents and professionals online. BMC Fam Pract. 2009;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dobson A, DaVanzo J, Haught R. The financial impact of the American Health Care Act’s Medicaid provisions on safety-net hospitals. https://www.commonwealth-fund.org/publications/fund-reports/2017/jun/financial-impact-american-health-care-acts-medicaid-provisions. Published June 28, 2017. Accessed April 25, 2019.
- 18.Mezzich JE, Cohen NL, Ruiperez MA, Banzato CE, Zapata-Vega MI. The Multicultural Quality of Life Index: presentation and validation. J Eval Clin Pract. 2011;17: 357–364. [DOI] [PubMed] [Google Scholar]
- 19.Zapata-Vega MI, Rivera J, Tarlin N, Bijan I, Maurer M. Using a brief 10-item generic measure of quality of life in English and Spanish speaking diabetic patients. Int J Psychiatry Med. 2010;40:399–411. [DOI] [PubMed] [Google Scholar]
- 20.Anderson PJ, Burnett A. Assessing developmental delay in early childhood—concerns with the Bayley-III scales. Clin Neuropsychol. 2017;31:371–381. [DOI] [PubMed] [Google Scholar]
- 21.Belfort MB, Santo E, McCormick MC. Using parent questionnaires to assess neurodevelopment in former preterm infants: a validation study. Paediatr Perinat Epidemiol. 2013;27:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sparrow SS, Cicchetti DV, Balla DA, Doll EA. Vineland Adaptive Behavior Scales: Survey Forms Manual. 2nd ed. Minneapolis MN: Pearson Assessment; 2005. [Google Scholar]
- 23.Meert K, Slomine BS, Christensen JR, et al. Burden of caregiving after a child’s in-hospital cardiac arrest. Resuscitation. 2018;127:44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rose-Jacobs R, Fiore JG, de Cuba SE, et al. Children with special health care needs, supplemental security income, and food insecurity. J Dev Behav Pediatr. 2016;37:140–147. [DOI] [PubMed] [Google Scholar]
- 25.Black MM, Quigg AM, Cook J, et al. WIC participation and attenuation of stress-related child health risks of household food insecurity and caregiver depressive symptoms. Arch Pediatr Adolesc Med. 2012;166: 444–451. [DOI] [PubMed] [Google Scholar]
- 26.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. 2007;119:e1332–e1341. [DOI] [PubMed] [Google Scholar]
- 27.Lakshmanan A, Agni M, Lieu T, et al. The impact of preterm birth <37 weeks on parents and families: a cross-sectional study in the 2 years after discharge from the neonatal intensive care unit. Health Qual Life Outcomes. 2017;15:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hassan A, Blood E, Pikcilingis A, et al. Improving social determinants of health: effectiveness of a web-based intervention Am J Prev Med. 2015;49:822–831. [DOI] [PubMed] [Google Scholar]
- 29.Hassan A, Blood EA, Pikcilingis A, et al. Youths’ health-related social problems: concerns often overlooked during the medical visit. J Adolesc Health. 2013;53:265–271. [DOI] [PubMed] [Google Scholar]
- 30.Wylie SA, Hassan A, Krull EG, et al. Assessing and referring adolescents’ health-related social problems: qualitative evaluation of a novel web-based approach. J Telemed Telecare. 2012;18:392–398. [DOI] [PubMed] [Google Scholar]
- 31.Wildevuur SE, Simonse LW. Information and communication technology-enabled person-centered care for the “big five” chronic conditions: scoping review. J Med Internet Res. 2015;17:e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bushar JA, Fishman J, Garfinkel D, Pirretti A. Enrolling underserved women in mHealth programs: results from Text4baby outreach campaigns. Health Promot Pract. 2019;20(2):292–299. doi: 10.1177/1524839918763589 [DOI] [PubMed] [Google Scholar]
- 33.Evans WD, Wallace JL, Snider J. Pilot evaluation of the Text4baby mobile health program. BMC Public Health. 2012;12:1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whittaker R, Matoff-Stepp S, Meehan J, et al. Text4baby: development and implementation of a national text messaging health information service. Am J Public Health. 2012;102:2207–2213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bushar JA, Kendrick JS, Ding H, Black CL, Greby SM. Text4baby influenza messaging and influenza vaccination among pregnant women. Am J Prev Med. 2017;53:845–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roche MI, Skinner D. How parents search, interpret, and evaluate genetic information obtained from the Internet. J Genet Couns. 2009;18:119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Allen K, Rainie L. Parents Online. Washington, DC: Pew Research Center; 2002. [Google Scholar]
- 38.Bapat R, McClead R, Shepherd E, Ryshen G, Bartman T. Challenges, successes and opportunities for reducing readmissions in a referral-based children’s hospital NICU. J Neonatal Perinatal Med. 2016;9:433–440. [DOI] [PubMed] [Google Scholar]
- 39.Welch CD, Check J, O’Shea TM. Improving care collaboration for NICU patients to decrease length of stay and readmission rate. BMJ Open Qual. 2017;6:e000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clements KM, Barfield WD, Kotelchuck M, Wilber N. Maternal socio-economic and race/ethnic characteristics associated with early intervention participation. Matern Child Health J. 2008;12:708–717. [DOI] [PubMed] [Google Scholar]
- 41.Miller JE. Developmental screening scores among preschool-aged children: the roles of poverty and child health. J Urban Health. 1998;75:135–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shapiro-Mendoza C, Kotelchuck M, Barfield W, et al. Enrollment in early intervention programs among infants born late preterm, early term, and term. Pediatrics. 2013;132: e61–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Little AA, Kamholz K, Corwin BK, Barrero-Castillero A, Wang CJ. Understanding barriers to early intervention services for preterm infants: lessons from two states. Acad Pediatr. 2015;15:430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dol J, Delahunty-Pike A, Siani SA, Campbell-Yeo M. eHealth interventions for parents in neonatal intensive care units: a systematic review. JBI Database System Rev Implement Rep. 2017;15:2981–3005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


