Abstract
Context:
Choledochal cyst is a rare malformation that mainly affects girls.
Aims:
The aim of this work is to report the diagnostic, therapeutic and evolutionary aspects of bile duct cyst in children in Dakar.
Subjects and Methods:
we conducted a prospective monocentre descriptive study from 1 July, 2016, to 30 June, 2019, in the Pediatric Surgery Department of Albert Royer Children's Hospital in Dakar. The studied parameters featured clinical, biological, radiological, therapeutic and evolutionary data. Overall, ten patients, including eight girls and two boys, were selected.
Results:
Two patients presented the classic triple-syndrome complex featuring an abdominal pain, an abdominal mass and jaundice. Most of the patients presented a symptomatology associating abdominal pain and vomiting. Biological cholestasis syndrome was present in six cases and biological cytolysis syndrome in five cases. The abdominal ultrasound-computed tomography (CT) scan confirmed the diagnosis and helped to set the Todani classification with a predominance of Types 1 and 4. Surgical treatment by laparotomy consisted of total excision of the cyst followed by a Y-en-Roux hepatico-jejunal anastomosis in nine cases, whereas we performed a drainage of the cyst in one case. Two patients presented a morbidity of anastomotic suture release and evisceration and had a good outcome after surgical repair. There was no mortality.
Conclusions:
The diagnosis of choledochal cyst dilatation (CCD) can be suspected in the postnatal period on the basis of a gastro-intestinal symptomatology with or without associated to jaundice. The combination ultrasound-abdominal CT-scan helps set the diagnosis. The laparatomic approach always has its place for the management of CCD, especially in our context.
Keywords: Bile ducts, child, dilation, malformation, surgery
INTRODUCTION
Choledochal cyst dilatation (CCD) is an uncommon congenital abnormality. Its prevalence varies according to populations with a higher frequency in Asians.[1,2] It mainly occurs in females and constitutes the second cause of biliary duct congenital malformation after biliary atresia.[3] In developed countries, prenatal diagnosis allows an early management of this condition. In developing countries, the diagnosis is set after birth with sometimes a broad clinical spectrum. The aim of this paper is to outline the therapeutical and diagnostic aspects of choledochal cyst in children in Dakar.
SUBJECTS AND METHODS
We conducted a multicentre prospective and descriptive study ranging from 1 July 2016, to 30 June 2019. All children who had a CCD and who underwent a surgical treatment at the Pediatric Surgery Department of Albert Royer Children Hospital in Dakar were included.
The studied parameters comprised the clinical course, biological and radiological findings, Todani classification, surgical time limit, technical approach, surgical exploration data, procedures, morbidity and mortality. Our series accounted for eight girls and two boys, meaning a sex ratio of 0.25. The mean age of our patients during their admission was 85.3 months (7.1 years), with extremes ranging from 6 months to 15 years.
RESULTS
The clinical course mainly featured abdominal pain and vomiting that, respectively, occurred in nine and eight patients. Physical examination revealed a mass on the right hypochondrium and/or epigastrium on five patients and jaundice in four patients with two cholestatic patterns. The triple-syndrome complex comprising pain, jaundice and abdominal mass was present in two patients. Figure 1 shows the various clinical signs presented by the patients. The most commonly associated signs were abdominal pain and vomiting, as shown in Table 1.
Figure 1.
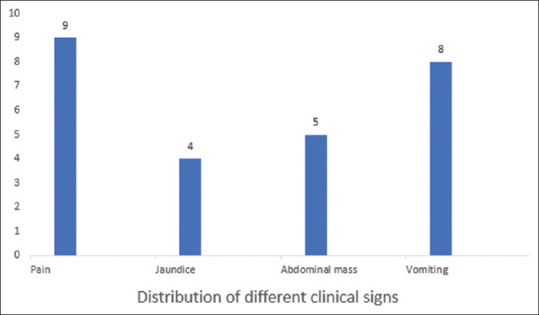
Distribution of clinical signs
Table 1.
Clinical sign associations
| Symptoms | n (%) |
|---|---|
| Abdominal pain + vomiting | 4 (40) |
| Abdominal pain + jaundice + abdominal mass | 2 (20) |
| Abdominal pain + abdominal mass + vomiting | 2 (20) |
| Abdominal pain + vomiting + jaundice | 1 (10) |
| Jaundice + vomiting + abdominal mass | 1 (10) |
Biological cholestatic syndrome was present in six cases, with total bilirubin levels ranging from 2 to 29 times the normal rate, direct bilirubin levels from 2 to 55 times the normal rate and alcaline phosphates from 2 to five times the normal levels. Biological cytolysis syndrome was noted in five cases, with transaminases levels reaching 38 times the normal rate.
The ultrasound, performed in all patients, allowed to evoke the diagnosis in all cases. Once an ultrasonographic diagnosis of choledochal cyst was provided, abdominal computed tomography CT-scan was performed and showeda choledochal cyst Type 1 in six cases, Type 4 in three cases and Type 3 in one case, according to Todani classification. Figures 2 and 3 show the most common types.
Figure 2.
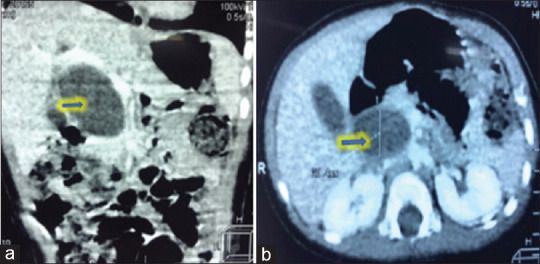
Choledochal cyst Todani type 1 (arrow) (a): Sagittal section. (b): Transverse section
Figure 3.
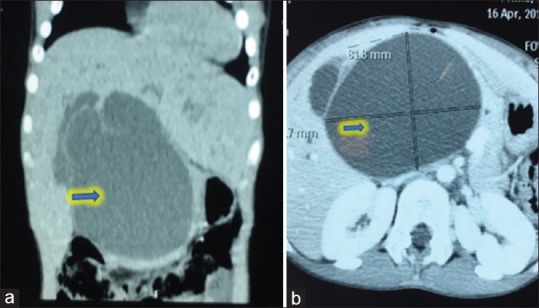
Choledochal cyst Todani type 4 (arrow) (a): Sagittal section. (b): Transverse section
The mean surgical time limit was 3 months and 4 days, with extremes ranging from 1 day to 11 months and 19 days. Open surgery was realised for all patients. Right sub-costal approach was performed in eight cases, whereas the median sub-umbilical approach was performed in two cases. Surgical exploration revealed a macroscopic healthy liver in eight cases, a macroscopic cholestatic liver in one patient and a macroscopic cirrhotic liver associated with ascites in one patient, and helped confirm the types according to Todani. Figures 2 and 3, respectively, show Types 1 and 4 that represent the most common patterns.
Nine patients underwent a total cyst excision with Roux-en-Y hepatico-jejunal transmesocolic anastomosis [Figures 4 and 5]. A patient had an external derivation of the cyst.
Figure 4.
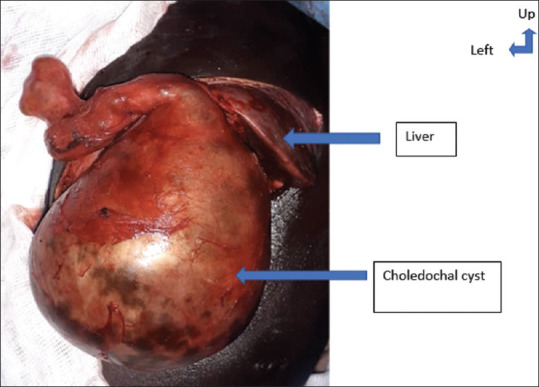
Pre-operative picture of choledochal cyst type 1
Figure 5.
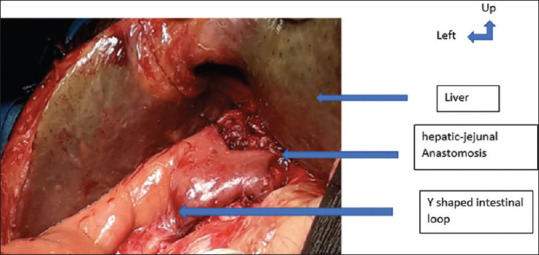
Image after cyst excision and hepatic-jejunal anastomosis
Two patients went through a morbidity, indicating a surgical repair, for an anastomotic suture release and evisceration. They both had a good outcome after surgical reintervention. We did not record mortality.
DISCUSSION
In general, in CCD condition, the triple-syndrome complex features abdominal pain, jaundice and abdominal mass. Nevertheless, it is not steady in children.[4,5,6] In fact, out of our ten patients, only two had a complete triad. The most common clinical courses included abdominal pain and vomiting.
The ultrasound-abdominal CT-scan combination allowed to set both the diagnosis and Todani classification. However, besides the exploration of large cysts, the combination of ultrasound and magnetic resonance imaging is a rational strategy and helps reduce radiations.[7] Most of the authors recommend early management during the 1st months of life to avoid complications because hepatic cirrhosis can occur precociously.[8] A case of liver failure was reported in an 5-month-old toddler.[9,10] Our data suggest a management delay for our patients compared to that of the literature.[2,9] This could be explained by the absence of prenatal diagnosis in our context, late admission and lack of knowledge of this condition by some practitioners.
The treatment of CCD is surgical.[11,12] The approach may be through laparotomy or laparoscopy with similar results.[11] In fact, Cherqaoui et al.[13] reported in a series of 19 patients that a laparoscopic approach of CC is possible and safe, even on toddler who had a prenatal diagnosis, with a low morbidity and identical operative suites to laparotomy. In our series, laparatomic surgical exploration was performed for all patients. It allowed to confirm the predominance of Type 1 of Todani classification, in consonance with that of the literature data.[4,6,11]
Several surgical treatments have been proposed for the management of choledochal cyst. Historically, Types 1, 2 and 4 underwent a cysto-enterostomy, resulting in a high incidence of recurrent cholangitis and stenosis.[14] Furthermore, this procedure does not withdraw the cyst mucosa which can lead to biliary duct carcinomas.[14]
Currently, the most admitted surgical approach is total excision of the enlarged portion of the biliary duct followed by a hepatico-duodenal or hepatico-jejunal anastomosis.[15,16,17] For many authors, the technique of choice remains the anastomosis of the biliary duct with the jejunum through a Y-shaped loop.
Our complication rate is similar to the data from the literature, witnessed by the series provided by Khmekhem et al.[11] and Cherqaoui et al.,[13] who, respectively, reported a complication rate of 37.5% and 5.2%.
The mortality varies in the literature but has essentially decreased these last years and has almost become zero in a recent series.[13,18,19] After a follow-up of 24 months, no deaths were recorded.
CONCLUSIONS
The diagnosis of CCD can be suspected in the postnatal period on the basis of a gastro-intestinal symptomatology featuring abdominal pain and vomiting with or without associated to jaundice. Ultrasound-abdominal CT-scan combination helps set the diagnosis. Laparatomic approach always has its place for the management of CCD especially in our context. Bilio-digestive derivation through Roux-en-Y performed after total excision of cyst yields good outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bhavsar MS, Vora HB, Giriyappa VH. Choledochal cysts: A review of literature. Saudi J Gastroenterol. 2012;18:230–6. doi: 10.4103/1319-3767.98425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim MJ, Han SJ, Yoon CS, Kim JH, Oh JT, Chung KS, et al. Using MR cholangiopancreatography to reveal anomalous pancreaticobiliary ductal union in infants and children with choledochal cysts. AJR Am J Roentgenol. 2002;179:209–14. doi: 10.2214/ajr.179.1.1790209. [DOI] [PubMed] [Google Scholar]
- 3.Le L, Pham AV, Dessanti A. Congenital dilatation of extrahepatic bile ducts in children. Experience in the central hospital of Hue, Vietnam. Eur J Pediatr Surg. 2006;16:24–7. doi: 10.1055/s-2005-873071. [DOI] [PubMed] [Google Scholar]
- 4.Tan KC, Howard ER. Choledochal cyst: A 14-year surgical experience with 36 patients. Br J Surg. 1988;75:892–5. doi: 10.1002/bjs.1800750921. [DOI] [PubMed] [Google Scholar]
- 5.Onufer EJ, Shakhsheer B, Vrecenak JD. Spontaneous perforation of a choledochal cyst after prolonged gastroenteritis. J Pediatr Surg. 2018;35:7–10. [Google Scholar]
- 6.Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts: Lessons from a 20 year experience. Arch Dis Child. 1995;73:528–31. doi: 10.1136/adc.73.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamidi S, Livingston MH, Alnaqi A, Yousef Y, Walton JM. Management of a massive choledochal cyst in a 12 year-old girl: Which imaging modalities should be performed preoperatively? J Ped Surg Case Reports. 2016;10:42–6. [Google Scholar]
- 8.Hung MH, Lin LH, Chen DF, Huang CS. Choledochal cysts in infants and children: Experiences over a 20-year period at a single institution. Eur J Pediatr. 2011;170:1179–85. doi: 10.1007/s00431-011-1429-2. [DOI] [PubMed] [Google Scholar]
- 9.Diao M, Li L, Cheng W. Timing of surgery for prenatally diagnosed asymptomatic choledochal cysts: A prospective randomized study. J Pediatr Surg. 2012;47:506–12. doi: 10.1016/j.jpedsurg.2011.09.056. [DOI] [PubMed] [Google Scholar]
- 10.Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: Part 2 of 3: Diagnosis. Can J Surg. 2009;52:506–11. [PMC free article] [PubMed] [Google Scholar]
- 11.Khmekhem R, Zitouni H, Ben Ahmed Y, Jlidi S, Nouira F, Charieg A, et al. Surgery of cystic dilatation of the bile duct in children, results of 16 observations. J Pédiatr Puér. 2012;25:199–205. [Google Scholar]
- 12.Saikusa N, Naito S, Iinuma Y, Ohtani T, Yokoyama N, Nitta K. Invasive cholangiocarcinoma identified in congenital biliary dilatation in a 3-year-old boy. J Pediatr Surg. 2009;44:2202–5. doi: 10.1016/j.jpedsurg.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 13.Cherqaoui A, Peycelon M, Blanc M, Guys JM, Bonnard A, Lagausie PD. Intérêt de la laparoscopie et du diagnostic anténatal en cas de kyste du Cholédoque. Arch Pédiatr. 2010;17:18. [Google Scholar]
- 14.Dhupar R, Gulack B, Geller DA, Marsh JW, Gamblin TC. The changing presentation of choledochal cyst disease: An incidental diagnosis. HPB Surg 2009. 2009:103739. doi: 10.1155/2009/103739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jordan PH, Goss JA, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg. 2004;187:790–5. doi: 10.1016/j.amjsurg.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Santore MT, Behar BJ, Blinman TA, Doolin EJ, Hedrick HL, Mattei P, et al. Hepaticoduodenostomy vs hepaticojejunostomy for reconstruction after resection of choledochal cyst. J Pediatr Surg. 2011;46:209–13. doi: 10.1016/j.jpedsurg.2010.09.092. [DOI] [PubMed] [Google Scholar]
- 17.Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: A systematic review and meta-analysis. J Pediatr Surg. 2013;48:2336–42. doi: 10.1016/j.jpedsurg.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 18.Liu SL, Lia L, Hou WY, Zhangb J, Huanga LM, Lib X et al. Laparoscopic excision of choledochal cyst and Roux-en-Y hepaticojejunostomy in symptomatic neonates. J Pediatr Surg. 2009;44:508–11. doi: 10.1016/j.jpedsurg.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Diao M, Li L. Using laparoscopic double hemicircumferential running single-layer suture in hepaticojejunostomy for choledochal cysts in children. J Pediatr Surg. 2018;53:199–202. [Google Scholar]


