Abstract
Clinically significant separation anxiety [SA] has been identified as being common among patients who do not respond to psychiatric interventions, regardless of intervention type (pharmacological or psychotherapeutic), across anxiety and mood disorders. An attachment formation and maintenance domain has been proposed as contributing to anxiety disorders. We therefore directly determined prevalence of SA in a population of adult treatment non-responders suffering from primary anxiety. In these separation anxious nonresponders, we pilot-tested an SA-focused, attachment-based psychotherapy for anxiety, Panic-Focused Psychodynamic Psychotherapy-eXtended Range [PFPP-XR], and assessed whether hypothesized biomarkers of attachment were engaged.
We studied separation anxiety [SA] in 46 adults (ages 23–70 [mean 43.9 (14.9)]) with clinically significant anxiety symptoms (Hamilton Anxiety Rating Scale [HARS] ≥ 15), and reporting a history of past non-response to psychotherapy and/or medication treatments. Thirty-seven (80%) had clinically significant symptoms of separation anxiety (Structured Clinical Interview for Separation Anxiety Symptoms [SCI-SAS] score ≥8).
Five of these subjects completed an open clinical trial of Panic Focused Psychodynamic Psychotherapy eXtended Range [PFPP-XR], a 21–24 session, 12-week manualized attachment-focused anxiolytic psychodynamic psychotherapy for anxiety. Patients improved on “adult threshold” SCI-SAS (current separation anxiety) (p = .016), HARS (p = 0.002), and global severity, assessed by the Clinical Global Impression Scale (p = .0006), at treatment termination. Salivary oxytocin levels decreased 67% after treatment (p = .12). There was no significant change in high or low frequency HRV after treatment, but change in high frequency HRV inversely correlated with treatment change in oxytocin (p < .02), and change in low frequency HRV was positively associated with change in oxytocin (p < .02).
SA is surprisingly prevalent among non-responders to standard anti-anxiety treatments, and it may represent a novel transdiagnostic target for treatment intervention in this population. Anxiety and global function improved in a small trial of a brief, manualized, attachment-focused psychodynamic psychotherapy, potentially supporting the clinical relevance of attachment dysfunction in this sample. The large decrease in oxytocin levels with treatment, although not statistically significant in this very small sample, suggests the need for further study of oxytocin as a putative biomarker or mediator of SA response. These pilot data generate testable hypotheses supporting an attachment domain underlying treatment-resistant anxiety, and new treatment strategies.
1. Introduction
1.1. Separation anxiety and attachment
Recent research has demonstrated that separation anxiety [SA] and separation anxiety disorder [SAD] are common among adults; 43% of patients with SAD report adult onset in a recent WHO study [1–3]. SA occurs across the lifespan, triggered in affected individuals by actual or anticipated separation from someone to whom one feels attached. SA often precedes development of panic attacks [4–16]. Separation anxiety disorder (SAD) appears prevalent in adults across anxiety and mood disorders, with current rates of 12 and 20% in two clinical samples [17,18]. The National Comorbidity Survey replication study documented 6.6% lifetime community prevalence of adult SAD [19]. Separation anxiety (SA) is prevalent in patients with anxiety disorders and may lead to refractory course [20], although this has not yet been studied directly. Although SA negatively moderates prognosis in mood and anxiety treatment trials of medication and psychotherapy, no research has yet determined the prevalence of SA among treatment nonresponders.
Clinical data indicate that SA contributes to a refractory course [4,14,20–22]. Nonetheless, current treatments for anxiety do not address attachment dysregulation or SA [1,16,23,24]. SA might logically contribute to chronic, intractable anxiety, because patterns of pathological, highly anxiety-ridden, ambivalent attachments, as in SA, compromise the ability to experience and internalize positive relationships and to develop mental capacities for self-soothing, anxiety tolerance, affect modulation, and individuation [25,26]. These factors may render patients with high SA vulnerable to even minor disruptions in therapeutic relationships of all sorts, contributing to treatment non-response [14–20].
Panic Focused Psychodynamic Psychotherapy-eXtended Range (PFPP-XR) [27] is a trans-diagnostic version of PFPP [28], a brief, manualized psychodynamic psychotherapy with demonstrated efficacy for panic disorder [29]. PFPP-XR targets separation anxiety and attachment dysregulation, yet it has not yet been studied specifically in an SA sample, nor in anxiety nonresponders. No research has used SA to clinically probe the research domain [30] of attachment formation and maintenance, nor tested the utility of an attachment-focused psychotherapy for anxiety in this population. The best-established treatment approaches for anxiety have not explored SA and attachment dysregulation; yet as a novel, logical target for treatment interventions and augmentation, SA deserves consideration [1,20].
1.2. Underlying biology
Animal models, neuroimaging, and genetics studies [20,31] support the importance of attachment, separation distress, and SA in anxiety. Recent findings in the biology of attachment offer an opportunity to link psychological attachment theory with underlying biology. Extensive preclinical findings on the biology of attachment have not yet been translated to clinical treatments. Nor have rodent [32–34] and primate [35–37] studies of oxytocin [33,38–52] and other neurobiology underlying the attachment system [53] and its impact on anxiety development yet produced practical clinical treatments for symptoms related to attachment system dysregulation. The RDoC attachment domain recognizes this, but no studies have explored biological correlates of attachment based treatment yet. Conversely, PFPP [27], an attachment-focused psychotherapy with anxiolytic efficacy [29], has never before been evaluated through the lens of underlying attachment biology.
Potential biological correlates of insecure attachment include measures of parasympathetic and sympathetic nervous system activity and the neuropeptide oxytocin. High frequency heart rate variability (hfHRV), also known as respiratory sinus arrhythmia (RSA, 56,57) reflects respiratory influence on cardiac vagal tone and is associated more broadly with adaptive reactivity to stressors [56,57]. Low frequency heart rate variability (lfHRV) is also predominantly determined by cardiac parasympathetic afferents but reflects the influence of blood pressure control mechanisms, including some sympathetic-determined processes such as vasomotor tone [58]. Both high frequency and low frequency HRV decrease in response to acute mental stress, indicating vagal withdrawal. Because of difficulty in assessing parasympathetic activity elsewhere in the body, researchers often use cardiac vagal tone as a measure of overall corporal parasympathetic tone, but this assumption is not well supported [59]. Low RSA has been associated with depression, anxiety disorders, and insecure attachment in numerous studies, suggesting it does reflect impaired emotional control [56,57,60].
Oxytocin (OT) is a hypothalamic neuropeptide that suppresses endocrine and behavioral stress responses, relieves pain, and facilitates pro-social behaviors including maternal behavior and affiliative contact-seeking across mammalian species [45]. Attachment behavior has been linked to peripheral OT levels, and OT receptor polymorphisms also have been linked to attachment behaviors [61]. A growing literature suggests that higher OT levels enhance the perceived intensity of social experiences. Higher resting plasma OT levels are associated with empathy, closeness, and trust in close relationships [38,45–48] in non-clinical samples. In clinical populations of psychiatric patients, higher plasma OT levels correlate with greater anxiety, harm avoidance, aggression, guilt and suspicion [49,50], interpersonal difficulties [51,52], and romantic attachment anxiety and distress (greater reactivity in the context of relationships, as individuals with SA illustrate [40,63,64]). In social anxiety disorder, higher plasma OT levels correlate with higher anxiety and relationship dissatisfaction [64].
This study aimed to: 1. Assess prevalence of SA in a treatment refractory sample of anxiety patients, 2. Pilot-study PFPP-XR treatment in a sub-sample of these patients, and 3. Explore the relationship of RSA and OT to SA and its treatment response. This pilot study begins to assess the utility of biomarker changes with treatment, which can potentially illuminate biological processes in the treatment’s mechanism of action. Biomarker temporal change is likely to be more useful than cross-sectional assessment, as a repeated measures design can control for other factors affecting the biomarker measures such as exercise, genotype, child abuse, etc. We predicted a priori that increasing levels of separation anxiety would be correlated with decreased parasympathetic tone. This prevalence study and small pilot open clinical trial were designed to begin to identify and treat the large group of anxiety disorder nonresponders with attachment dysregulation.
2. Method
2.1. Prevalence study
Adults aged 18–70 with a primary complaint of anxiety and who by history had not responded to at least one empirically-proven treatment were recruited at the Weill Cornell Medical College Department of Psychiatry through word of mouth and advertising. All signed informed written consent; the WCMC IRB approved the study. Patients were included if they: (1) had prominent anxiety, (defined by Hamilton Anxiety Rating Scale [HARS] (67) score of ≥ 15) and (2) could provide evidence of nonresponse (clinically persistent anxiety) to at least one evidence-based anti-anxiety treatment, specifically: (a) at least 2 months of an adequately dosed SSRI or TCA equivalent (e.g., ≥ 20 mg fluoxetine equivalent, or imipramine ≥ 200 mg) taken as directed, or (b) ≥ 11 weeks of CBT with a CBT-trained therapist. Names of past clinicians and documentation of past non-response were obtained. Patients were excluded for psychosis, acute suicidality, bipolar disorder, and organic mental disorders. Forty-six nonresponders were recruited and evaluated for presence of clinically significant SA on the SCI-SAS [23], global severity on the CGI-S [66], and Heart Rate Variability [HRV] and salivary oxytocin [OT] measurements.
2.2. Psychotherapy study
Patients from this prevalence study with clinically significant SA (defined as SCI-SAS ≥ 8) [23] (and without acute suicidality) were assessed for DSM-IV diagnosis using the Anxiety Disorders Interview Schedule for DSM IV–Lifetime version (ADIS-IV-L, 69) and treated in 21–24 sessions of PFPP-XR over 12 weeks. Patients on stable doses of medication for ≥ 2 months were continued on their stable doses, and all new medication trials and concurrent psychotherapies were prohibited. Trained clinical adherence raters monitored therapist adherence via videotaped sessions using the PFPP-XR adherence rating scale ICC = 0.92 [68]. A master's level independent evaluator performed clinical and biological assessments before and after treatment.
2.3. PFPP-XR
PFPP-XR uncovers unconscious psychological meanings of anxiety to achieve relief. The treatment focuses on anxious, dysregulated attachments that aggravate anxiety and bring about a sense of personal fragility and incompetence. Treatment explores circumstances and feelings surrounding anxiety onset, personal meanings of anxiety symptoms, and feelings and content of anxiety episodes and events to decode underlying significance. Core dynamic conflicts in anxiety include: difficulties with separation and autonomy; anger recognition/tolerance; and guilt/self-punishment through anxiety symptoms. Core conflicts, often identified through the transference, must be understood and altered. Strategies include addressing the transference and working through (demonstrating that conflicts emerge across situations). Patients' reaction to termination, often involving re-experiencing conflicts directly with the therapist, is actively addressed.
2.4. Therapists
Four therapists (3 female) participated, with an average of 7 years post-degree experience (SD = 4.1, range [2–25]), mean 7 years performing time-limited therapy (SD = 7.0, range [0–22]), and ≥ 1 year of clinical experience treating anxiety disorders.
2.5. Measures
The SCI-SAS, measuring SA in adults, displays excellent psychometric properties, and provides separate assessments of (retrospective) childhood and current adult separation anxiety [23]. As a change measure, we monitored the adult threshold measure of separation anxiety, as suggested [24], to focus on clinically significant symptoms. The Clinicians' Global Index of Severity [CGI-S [68]] assessed global severity. The Hamilton Anxiety Rating Scale (HARS, 67) assessed anxiety severity. Secondary measures included the Hamilton Rating Scale for Depression (HRSD, 71) to assess depression. We secondarily evaluated change in DSM Axis I diagnoses with the ADIS-IV-L before and after treatment [68]. On the ADIS, all subjects included in the psychotherapy study met criteria for social phobia, GAD and separation anxiety disorder. Two subjects additionally had panic disorder, 2 had MDD (neither as the primary diagnosis), and 2 had dysthymic disorder.
Biological measures were collected on one occasion for subjects not treated in psychotherapy, and for psychotherapy patients, before and after treatment. HRV: Subjects wore an ambulatory physiological monitor (Lifeshirt™, Vivometrics, San Diego, CA) collecting continuous ECG for 20 minutes at quiet rest. ECG RR intervals were edited to remove artifact and ectopy using CarioEdit software (Mind/Body Institute, U Ill Chicago). High and low frequency HRV were calculated using CardioBatch software (Mind/Body Institute, University of Illinois, Chicago) [71].
2.6. Oxytocin
Three resting saliva samples were collected at 45 minute intervals, and results for each session were averaged. We utilized salivary oxytocin measures rather than serum to facilitate collection of multiple samples to enhance reliability of the measure. Salivary oxytocin has shown very good correspondence with plasma oxytocin measures when plasma is extracted prior to assay (R = 0.59 (67)–0.89 (73) [64]). A commercial EIA kit (Abcam, Cambridge, MA) was used to measure oxytocin, without sample extraction or concentration. Eighteen percent of the 110 samples collected were below the assay detection limit. For calculation of mean oxytocin measurement, samples below the detection limit were assigned the detection limit of the assay (15 pg/ml). We did not restrict collection to one time of day or one menstrual cycle phase, as there is little evidence that circadian rhythm and menstrual cycle influence change in basal serum levels in humans [48,53,73]. Processing of all biomarkers was conducted blind to treatment response and other subject characteristics.
2.7. Data analysis
Prevalence of SA was defined as percentage of subjects who met SCI-SAS total score cutoff ≥ 8 for “case-ness”. Multiple regression analysis was used to examine the impact of high and low frequency HRV and OT on SCI-SAS score, and adult and child SCI-SAS subscales in the total sample. Age was a significant covariate with both HRV measures and SCI-SAS, hence included in the regression models. Clinical measures of psychotherapy outcome and change in biomarkers were analyzed by the paired t-test. Multiple regression was also used to examine the relationship of change in biomarkers to change in SCI-SAS score, and to examine the relationship between change in oxytocin levels and change in high and low frequency HRV. Test–retest (i.e., intra-rater) reliability, which measures the precision of repeated OT measurements, was assessed by the Pearson correlation coefficient or Spearman-rank correlation coefficient, as appropriate. All p-values are two-sided with statistical significance evaluated at the .05 alpha level. Test–re-test reliability is very strong since all the correlations are greater than 0.70. Ninety-five percent confidence intervals were calculated to assess the precision of the obtained estimates. All analyses were performed in SPSS Version 23.0 (SPSS Inc., Chicago, IL).
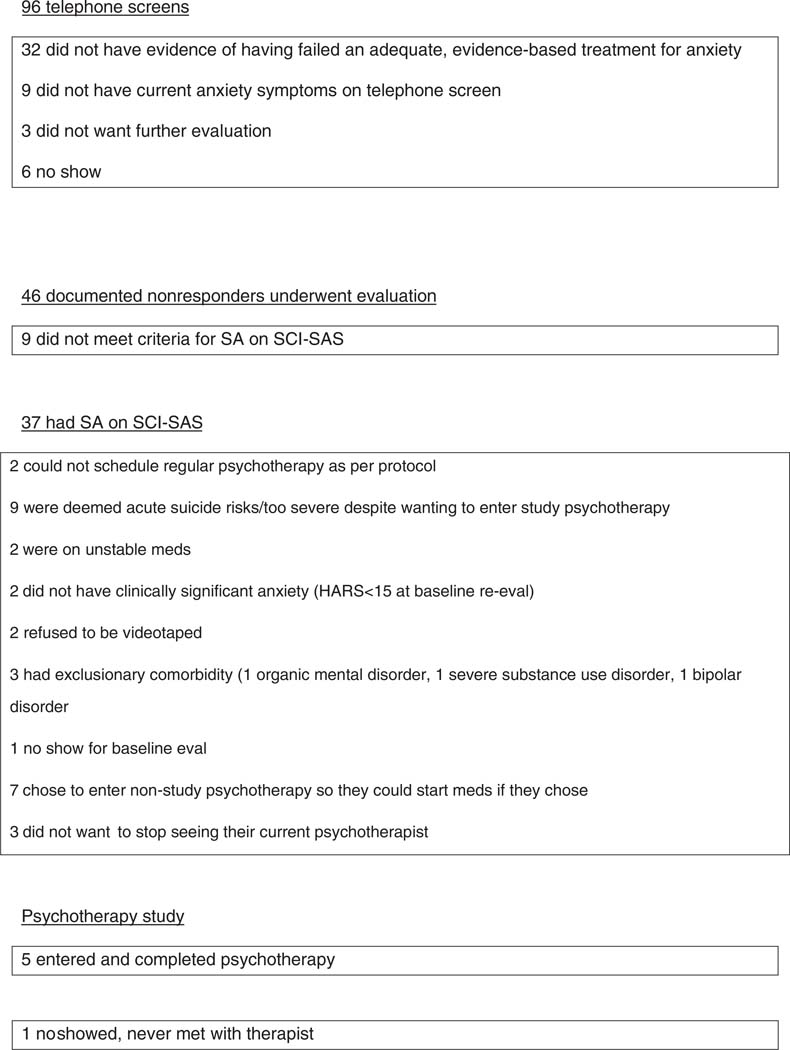
3. Results (Fig. 1)
Fig. 1.
Consort diagram: SA in anxiety nonresponders study.
3.1. Prevalence of SA in nonresponders study
Patients had a mean age of 43.9 years (14.9). 59% were female. 27% of the sample was Hispanic; 34% were African American, 62% Caucasian, 4% Asian. 45% were single, 25% married, 12% divorced, 6% separated, 5% widowed, and 7% cohabiting. Mean HDRS was 20.2 (6.2), mean HARS 15.7 (5.9), and mean CGI-S 4.6 (0.9). Of 46 patients with a primary complaint of anxiety, HARS ≥ 15, and documented nonresponse to an adequate medication or CBT trial, 37 (80%) had clinically significant separation anxiety as assessed by SCI-SAS total score. SA+ patients did not differ demographically or in clinical severities from the entire sample of non-responders. The child subscale of the SCI-SAS, but not the adult subscale, was inversely associated with subject age (p < .02).
3.2. Heart rate variability
As hypothesized, SA severity on the SCI-SAS was inversely associated with low frequency HRV at trend significance (p = .07). High frequency HRV also was inversely, but more weakly associated with SCI-SAS, p = .16. Gender and antidepressant use were not associated with any heart rate measures.
3.2.1. Oxytocin
SA severity was non-significantly associated with the SCI-SAS total score, (p = .14). OT was more closely associated with the child subscale of the SCI-SAS (p = .01) than the adult subscale (p = 0.6).
3.3. PFPP-XR pilot study
Six patients entered this study. One, who dropped out after session 1 because of scheduling conflicts was not included in treatment analyses. The mean age of the sample was 50.5 years (15.7). Three subjects were married, and two were single; three were white non-Hispanic, and two were Hispanic of mixed race. Three were employed, two had stopped working due to chronic anxiety. Significant, clinically meaningful improvement occurred with treatment (Table 1).
Table 1.
Clinical outcome of nonresponders with anxiety disorders and high SA in PFPP-XR.
| Measure | Threshold adult SCI-SAS | HARS | HDRS | CGI-Severity | ADIS severity primary dx |
|---|---|---|---|---|---|
| Pre n = 5 | 3.8 (.8) | 18.6 (4.1) | 23.4 (3.7) | 4.6 (.55) | 6.3a |
| Post n = 5 | 1.4 (1.1) | 8.8 (2.2) | 13.8 (3.3) | 2.2 (0.45) | 3.3 |
| t | − 4.0 | 9.8 | 6.6 | 9.8 | |
| P | .016 | .002 | .007 | .0006 |
Values are means (SD).
Mean severity of primary diagnosis on ADIS/threshold for DSM “caseness” = 4; all lost primary diagnosis at termination. 5 = “impaired” 6 = significantly impaired. 3 = subthreshold.
3.4. Biomarker changes pre–post treatment
Biomarker data pre- and post-treatment show no statistically significant changes. There was, however, a 66% decrease in salivary OT (171 ± 31 to 57 ± 22 pg/ml, t = −1.9; p = .12) in this very small sample. There was no consistent change with treatment in high or low frequency HRV (hfHRV 5.12 vs. 4.95, t = −.9, p = 0.4; lfHRV 5.33 vs. 5.26, t = .74, p = 0.7)) and no significant relationship of change in any of the three biomarkers with change in SCI-SAS score. However, in a regression model, change in oxytocin was inversely associated with change in high frequency HRV (p < .02) and positively associated with change in low frequency HRV (p < .02). Improvements in vagal tone correlated with OT normalization (decreases) and decreases in low frequency HRV correlated with OT decreases over the span of the treatment.
4. Discussion
The prevalence finding of this study demonstrates for the first time that clinically significant separation anxiety is widespread among patients who report having not responded to standard treatments for clinically significant anxiety. This is an important clinical observation, suggesting SA is often a part of this syndrome, and should become a target for treatment interventions. The study was cross sectional, and not designed to address the etiological relationship of separation anxiety, or attachment dysregulation, to development and persistence of other anxiety disorders [20]. Other studies have made some of these links [3,6,32], yet the degree to which early attachment dysregulation and insecurity are causal factors in persistent anxiety apparently refractory to current treatments remains unclear.
Results from the pilot psychotherapy trial demonstrate feasibility of a manualized psychodynamic psychotherapy in this treatment-refractory sample. The findings of significant improvement with treatment are intriguing, yet the very small sample size and uncontrolled design preclude drawing any conclusions about efficacy without confirmation in randomized controlled trials. Given that treatment nonresponders have a diminished likelihood of responding to additional treatments, the measurable improvement in a brief separation anxiety focused manualized psychodynamic psychotherapy is heartening.
The finding of a trend for HRV, a measure of cardiac parasympathetic tone, to be inversely associated with SA severity is consistent with findings in other anxiety disorders [57,58]. The large decrease in oxytocin lev\els with treatment, although not statistically significant in this very small sample, suggests the need for further study of oxytocin as a putative biomarker or mediator of SA response. The significant associations between change in OT and change in HRV with treatment, although preliminary, are intriguing and suggest that autonomic and OT regulation may be linked. The longitudinal design of this study could enhance the sensitivity to detect these relationships. These pilot data generate testable hypotheses that can lend support to an attachment domain underlying treatment-resistant anxiety, and new strategies for treatment.
Limitations of this small pilot study include retrospective reports of treatment failure by patients, accompanied by documentation of unsuccessful treatments by treating clinicians in most but not all cases, and the very small sample size, failure to concentrate the OT samples, multiple comparisons, and uncontrolled design of the psychotherapy trial.
Acknowledgments
Funding support for this project comes from the Brain and Behavior Research Foundation, a Fund in the New York Community Trust established by DeWitt Wallace, and NIMH R01 MH70918-01 A2. Dr. Milrod receives book royalties from Taylor & Francis. In the past 3 years, Dr. Schneier has received research support from Forest Laboratories and royalties from Cambridge University Press and UpToDate.
Dr. Paul Christos and oxytocin assays were partially supported by the Clinical and Translational Science Center at Weill Cornell Medical College (UL1-TR000457-06).
References
- [1].Milrod B. An epidemiological contribution to clinical understanding of anxiety. Am J Psychiatry 2015;172(7):601–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cyranowski J, Milrod B. In: & Gabbard G, editor. Separation anxiety disorder in the American psychiatric association's textbook of treatments for psychiatric disorders. Washington, DC: American Psychiatric Press; 2014. [Google Scholar]
- [3].Silove D, Ionso J, Bromet E, Gruber M, Sampson N, Scott K, et al. Pediatric-onset and adult-onset separation anxiety disorder across countries in the World Mental Health Survey. Am J Psychiatry 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Miniati M, Calugi S, Rucci P, Shear MK, Benvenuti A, Santoro D, et al. Predictors of response among patients with panic disorder treated with medications in a naturalistic follow-up: the role of adult separation anxiety. J Affect Disord 2012;136(3):675–9 [Epub 2011 Nov 30]. [DOI] [PubMed] [Google Scholar]
- [5].Preter M, Lee SH, Petkova E, Vannucci M, Kim S, Klein DF. controlled cross-over study in normal subjects of naloxone-preceding-lactate infusions; respiratory and subjective responses: relationship to endogenous opioid system, suffocation false alarm theory and childhood parental loss psychological medicine; 2010, 10.1017/S0033291710000838. [DOI] [PMC free article] [PubMed]
- [6].Kossowsky J, Pfaltz MC, Schneider S, Taeymans J, Locher C, Gaab J. The separation anxiety hypothesis of panic disorder revisited: a meta-analysis. Am J Psychiatry 2013, 10.1176/appi.ajp.2012.12070893. [DOI] [PubMed] [Google Scholar]
- [7].Shear MK. Factors in the etiology and pathogenesis of panic disorder: revisiting the attachment-separation paradigm. Am J Psychiatry 1996;153(Suppl 7):125–36. [DOI] [PubMed] [Google Scholar]
- [8].Fonagy P, Target M. Attachment and reflective function: their role in self-organization. Dev Psychopathol 1997;9:679–700. [DOI] [PubMed] [Google Scholar]
- [9].Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593–602 [Published erratum appears in Arch Gen Psychiatry 2005, 62:768.]. [DOI] [PubMed] [Google Scholar]
- [10].Roberson-Nay R, Eaves RJ, Hettema JM, Kendler KS, Silberg JL. Childhood separation anxiety disorder and adult onset panic attacks share a common genetic diathesis. Depress Anxiety 2012;29:320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cassano GB, Michelini S, Shear MK, Coli E, Maser JD, Frank E. The panic–agoraphobic spectrum: a descriptive approach to the assessment and treatment of subtle symptoms. Am J Psychiatry 1997;154:27–38. [DOI] [PubMed] [Google Scholar]
- [12].Rucci P, Miniati M, Oppo A, Mula M, Calugi S, Frank E, et al. The structure of lifetime panic-agoraphobic spectrum. J Psychiatr Res 2009;43:366–79. [DOI] [PubMed] [Google Scholar]
- [13].Frank E, Shear MK, Rucci P, Cyranowski JM, Endicott J, Fagiolini A, et al. Influence of panic-agoraphobic spectrum symptoms on treatment response in patients with recurrent major depression. Am J Psychiatry 2000;157(7):1101–7. [DOI] [PubMed] [Google Scholar]
- [14].Antonella Benvenutia, Paola Ruccib, Simona Calugia c,, Cassanoa Giovanni B, Mario miniatia, Ellen frank. MDD nonresponse linked to panic spectrum Relationship of residual mood and panic–agoraphobic spectrum phenomenology to quality of life and functional impairment in patients with major depression. Int Clin Psychopharmacol 2010;25:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Frank E, Cyranowski JM, Rucci P, Shear MK, Fagiolini A, Thase ME, et al. Clinical significance of lifetime panic spectrum symptoms in the treatment of patients with bipolar I disorder. Arch Gen Psychiatry 2002;59(10):905–11. [DOI] [PubMed] [Google Scholar]
- [16].Coryell W, Fiedorowicz JG, Solomon D, Leon AC, Rice JP, Keller MB. Effects of anxiety on the long-term course of depressive disorders. Br J Psychiatry 2012;200:210–5, 10.1192/bjp.bp.110.081992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Silove D, Marnane C, Wagner R, Manicavasagar V. Brief report–associations of personality disorder with early separation anxiety in patients with adult separation anxiety disorder. J Personal Disord 2011;25(1):128–33. [DOI] [PubMed] [Google Scholar]
- [18].Pini S, Abelli M, Shear KM, et al. Frequency and clinical correlates of adult separation anxiety in a sample of 508 outpatients with mood and anxiety disorders. Acta Psychiatr Scand 2009. 13 (epub ahead of print). One of the largest clinical samples researching ASAD, this study shows delineation between onset ages for those with CSAD only and those who had CSAD and ASAD. [DOI] [PubMed] [Google Scholar]
- [19].Shear K, Jin R, Ruscio AM, et al. Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the national comorbidity survey replication. Am J Psychiatry 2006;163:1074–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Milrod B, Markowitz JC, Gerber A, et al. Childhood separation anxiety and the pathogenesis and treatment of adult anxiety. Am J Psychiatry 2014;171:34–43. [DOI] [PubMed] [Google Scholar]
- [21].Laor N, Wolmer L, Mayes LC, Golomb A, Silverberg DS, Weizman R, et al. Israeli Preschoolers under scud missile attacks. A developmental perspective on risk-modifying factors. Arch Gen Psychiatry 1996;53(5):416–23. [DOI] [PubMed] [Google Scholar]
- [22].Dell'Osso L, Carmassi C, Corsi M, Pergentini I, Socci C, Maremmani AG, et al. Adult separation anxiety in patients with complicated grief versus healthy control subjects: relationships with lifetime depressive and hypomanic symptoms. Ann Gen Psychiatry 2011;10:29, 10.1186/1744-859X-10-29 [Published online 2011 October 27]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Saxe GN, Stoddard F, Hall E, Chawla N, Lopez C, Sheridan R, et al. Pathways to PTSD, part I: children with burns. Am J Psychiatry 2005;162(7):1299–304. [DOI] [PubMed] [Google Scholar]
- [24].Cyranowski JM, Shear MK, Rucci P, Fagiolini A, Frank E, Grochocinski VJ, et al. Adult separation anxiety: psychometric properties of a new structured clinical interview. J Psychiatr Res 2002;36:77–86. [DOI] [PubMed] [Google Scholar]
- [25].Manicavasagar V, Marnane C, Pini S, Abelli M, Rees S, Eapen V, et al. Adult separation anxiety disorder: a disorder comes of age. Curr Psychiatry Rep 2010. Aug;12(4):290–7. [DOI] [PubMed] [Google Scholar]
- [26].Bowlby J. A secure base: parent–child attachment and healthy human development. Tavistock professional book. London: Routledge; 1988. [Google Scholar]
- [27].Bowlby J. Attachment and loss. New York: Basic Books; 1973. [Google Scholar]
- [28].Busch F, Milrod B, Singer M, Aronson A. Panic focused psychodynamic psychotherapy: eXtended range: psychodynamic psychotherapy for anxiety disorders: a transdiagnostic treatment manual Taylor & Francis. LLC; 2012. [Google Scholar]
- [29].Milrod B, Busch F, Cooper A, Shapiro T. Manual of panic-focused psychodynamic psychotherapy. Washington, D.C.: APA Press; 1997 [Google Scholar]
- [30].Milrod B, Leon AC, Busch FN, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. Am J Psychiatry 2007;164:265–72. [DOI] [PubMed] [Google Scholar]
- [31]. http://www.nimh.nih.gov/research-priorities/rdoc/rdoc-constructs.shtml#attachment_formation.
- [32].Eley TC, McAdams TA, Rijsdijk FV, Lichtenstein P, Narusyte J, Reiss D, et al. The intergenerational transmission of anxiety: a children-of-twins study. Am J Psychiatry 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Brunelli SA, Zimmerberg B, Hofer MA, hood KE, tucker Halpern C. Developmental effects of selective breeding for an infant trait. In: Greenberg G, & Lerner RM, editors. developmental science behavior and genetics. Wiley Blackwell; 2010. [Google Scholar]
- [34].Insel T. The challenge of translation in social neuroscience: a reivew of oxytocin, vasopressin, and affiliative behavior. Neuron 2010;65:768–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hofer MA, Lewis-Fernandez. In: Simpson HB, Neria Y, & Schneier F, editors. New concepts in the evolution and development of anxiety In Anxiety disorders. Cambridge University Press; 2010. [Google Scholar]
- [36].Coplan JD, Mathew SJ, Abdallah CG, Mao X, Kral JG, Smith EL, et al. Early-life stress and neurometabolites of the hippocampus. Brain Res 2010;1358:191–9 [Epub 2010 Aug 14]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Jackowski A, Perera TD, Abdallah CG, Garrido G, Tang CY, Martinez J, et al. Early-life stress, corpus callosum development, hippocampal volumetrics, and anxious behavior in male nonhuman primates. Psychiatry Res 2011;192(1):37–44 [Epub 2011 Mar 5]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Winslow J, Noble P, Lyons C, Sterk S, Insel T. Rearing effects on cerebrospinal fluid oxytocin concentration and social buffering in rhesus monkeys. Neuropsychopharmacology 2003;28:910–8. [DOI] [PubMed] [Google Scholar]
- [39].Bartz J, Zaki J, Ochsner K, Bolger N, Kolevzon A, Ludwig N, et al. Oxytocin sectively improves empathic accuracy. Psychol Sci 2010;21:1426–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Marazziti D, Dell'Osso B, Baroni S, Mungai F, Catena M, Rucci P, et al. A relationship between oxytocin and anxiety of romantic attachment. Clin Pract Epidemiol Ment Health 2006;2:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Rockliff H, Karl A, McEwan K, Gilber J, Matos M, Gilbert P. Effects of intranasal oxytocin on 'compassion focused imagery'. Emotion 2011;11:1388–96. [DOI] [PubMed] [Google Scholar]
- [42].Shamay-Tsoory S, Fischer M, Dvash J, Harari H, Perach-Bloom N, Levkovitz Y. Intranasal administration of oxytocin increases envy and schadenfreude (gloating). Biol Psychiatry 2009;66:864–70. [DOI] [PubMed] [Google Scholar]
- [43].Kubansky L, Mendes W, Appleton A, Block J, Adler G. A heartfelt response: oxytocin effects on response to social stress in men and women. Biol Psychol 2012;90:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Bartz J, Zaki J, Oshsner K, Bolger N, Kolvezon A, Ludwig N, et al. Efects of oxytocin on recollections of maternal care and closeness. Proc Natl Acad Sci U S A 2010;107:21371–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Bartz J, Simeon D, Hamilton H, Kim S, Crystal S, Braun A, et al. Oxytocin can hinder trust and cooperation in borderline personality disorder. SCAN 2011;6:556–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Grewen K, Davenport R, Light K. An investigation of plasma and salivary oxytocin responses in breast- and formula-feeding mothers of infants. Psychophysiology 2010;47:625–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Radke S, deBruijn E. The other side of the coin: oxytocin decreases the adherence to fairness norrms. Front Hum Neurosci 2012;6:Article193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Amico J, Tenicela R, Johnston J, Robinson A. A time-dependent peak of oxytocin exists in cerebrospinal fluid but not plasma of humans. J Clin Endocrinol Metab 1983;57:947–51. [DOI] [PubMed] [Google Scholar]
- [49].Feldman R, Weller A, Zagoory-Sharon O, Levine A. Evidence for a neurosendocrinological foundation of human affiliation. Psychol Sci 2007;18:965–70. [DOI] [PubMed] [Google Scholar]
- [50].Gordon I, Zagoor-SHaron O, Leckman J, Feldman R. Prolactin, oxytocin and the development of paternal behavior across the first six months of fatherhood. Horm Behav 2010;58:513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Uvnas-Moberg K, Arn I, Theorell T, Jonsson C. Personality traits in a group of individuals with functional disorders of the gastrointestinal tract and their correlation with gastrin, cholecystokinin, somatostatin and oxytocin levels. J Psychosom Res 1991;35:515–23. [DOI] [PubMed] [Google Scholar]
- [52].Turner R, Altemus M, Yip D, Kupferman E, Fletcher D, Bostrom A, et al. Effects of oxytocin, prolactin and ACTH in women. Stress 2002;5:269–76. [DOI] [PubMed] [Google Scholar]
- [53].Chalinor S, Winters S, Amico J. Patterns of oxytocin concentrations of healthy women and men: effects of the menstrual cycle and short-term fasting. Endocr Res 1994;20:117–25. [DOI] [PubMed] [Google Scholar]
- [54].Friedman BH, Thayer JF. Autonomic balance revisited: panic anxiety and heart rate variability. J Psychosom Res 1998;44:133–51. [DOI] [PubMed] [Google Scholar]
- [55].Sack M, Hopper J, Lamprecht F. Low respiratory sinus arrythmia and prologned psychophyiological arousal in posttraumatic stress disorder: heart rate dynamics and individual differences in arousal regulation. Biol Psychiatry 2004;55:284–90. [DOI] [PubMed] [Google Scholar]
- [56].Friedman B. An automatic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol 2007;74:185–99. [DOI] [PubMed] [Google Scholar]
- [57].G A, Reyes Del Paso GA, Langewitz W, Mulder LJM, Van Roon A, Duschek S. Psychophysiology 2013;50:477–87. [DOI] [PubMed] [Google Scholar]
- [58].Ritz T. Studying noninvasive indices of vagal control: the need for respiratory control and the problem of target specificity. Biol Psychol 2009;80:158–68. [DOI] [PubMed] [Google Scholar]
- [59].Bornstein MH, Seuss PE. Child and mother cardiac vagal tone: continuity, stability, and concordance across the first 5 years. Dev Psychobiol 2000;36:54–65. [PubMed] [Google Scholar]
- [60].Declerck H, Boone C, Kiyonari T. Oxytocin and cooperation under conditions of uncertainty: the modulating role of incentive and social information. Horm Behav 2010;57:368–74. [DOI] [PubMed] [Google Scholar]
- [61].Holt-Lundstad J, Birmingham W, Light K. Influence of a “warm touch” support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase and cortisol. Psychosom Med 2008;70:976–85. [DOI] [PubMed] [Google Scholar]
- [62].Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50–5. [DOI] [PubMed] [Google Scholar]
- [63].DiNardo PA, Brown TA, Barlow DH. Anxiety disorders interview schedule for DSM-IV: Current Version, (ADIS-IV). New York: Graywinds Publications; 1995. [Google Scholar]
- [64].Byrne E, Fleg J, Vaitkevicius P, Wright J, Porges S. Role of aerobic capacity and body mass index in the age-associated decline in heart rate variability. J Appl Physiol 1996;81:743–50. [DOI] [PubMed] [Google Scholar]
- [65].Marazziti D, Dell'Osso B, Baroni S, et al. A relationship between oxytocin and anxiety of romantic attachment. Clin Pract Epidemiol Ment Health 2006;2:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]