Summary
Ambulatory blood pressure monitoring not only provides information on the blood pressure level, but on the diurnal changes in blood pressure as well. The present review summarizes the main fi ndings of the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcome (IDACO) with regard to risk stratifi cation based on short-term blood pressure variability. An exaggerated morning surge, exceeding the 90th percentile of the population, is an independent risk factor for mortality and cardiovascular and cardiac events. Conversely, a sleep-through or pre-awakening morning surge less than 20 mm Hg in systolic blood pressure is probably not associated with an increased risk of death or cardiovascular events. Blood pressure variability represented by the average of the daytime and nighttime SD weighted for the duration of the daytime and nighttime interval (SDdn) and by average real variability (ARV24) predicted outcome, but only improved the prediction of the composite cardiovascular events by 0.1%. Overall, results of analyses using the IDACO support the concept that short-term blood pressure variability adds to risk stratifi cation, but 24-hour ambulatory blood pressure level is the most valuable predictor for use in clinical practice.
Keywords: Blood pressure, blood pressure variability, morning surge, cardiovascular outcome
INTRODUCTION
Ambulatory monitoring provides a direct record of blood pressure throughout the whole day in patients engaged in their usual activities. Ambulatory blood pressure recordings have high reproducibility, are not subject to digit preference, and avoid the transient rise in blood pressure in response to a medical environment, the so-called white-coat effect1,2. We have built a shared new resource of prospective studies conducted in the general population with the objective of elucidating with great precision to what extent ambulatory blood pressure improves risk stratification compared to conventional blood pressure. We chose IDACO as the acronym for the new International Database of Ambulatory blood pressure in relation to Cardiovascular Outcome. All studies included in IDACO have been previously published in peer-reviewed journals3–11.
The morning surge in blood pressure
For the analysis of morning surge12, we selected studies in which the participants completed a diary during ambulatory blood pressure monitoring. The characteristics of these studies are available in references3–9.
For analysis of the morning surge in blood pressure, we determined the awake and asleep periods from the subjects’ diary cards. Subjects were asked to record the time when they got up in the morning and went to bed at night. The sleep-through morning surge was the difference between the morning pressure (the average blood pressure during the 2 hours after awakening) and the lowest nighttime blood pressure (the average of the lowest pressure and the two readings immediately preceding and following the lowest value)13. The pre-awakening morning surge was the difference between the morning blood pressure (the average blood pressure during the 2 hours after awakening) and the pre-awakening blood pressure (the average blood pressure during the 2 hours before awakening)13,14.
In all participants, the sleep-through and pre-awakening morning surge in systolic blood pressure averaged 20.7 ± 12.9 mm Hg and 13.1 ± 11.9 mm Hg, respectively. However, there were significant ethnic and sex differences in the morning blood pressure surge. The mean values of the sleep-through systolic morning surge in the top decile were smaller in women than in men among Europeans (40.9 vs 43.2 mm Hg; P = 0.003) and South Americans (38.8 vs 41.5 mm Hg; P = 0.041), where as the opposite was the case among Asians (52.4 vs 50.1 mm Hg; P = 0.064). For the pre-awakening systolic morning surge, the differences between women and men showed similar trends: 26.8 vs 29.2 mm Hg (P = 0.062), 22.5 vs 26.9 mm Hg (P = 0.059), and 30.6 vs 27.4 mm Hg (P = 0.13) in Europeans, South Americans and Asians, respectively. These differences explain why we applied ethnicity- and sex-specific deciles to study the predictive value of the morning blood pressure surge. This also ensured an equal distribution of ethnicities and women and men across the deciles. With adjustments applied for cohort, sex, age, body mass index, the 24-hour systolic blood pressure, current smoking, use of alcohol, serum cholesterol, the presence of diabetes mellitus, a history of cardiovascular disease, and antihypertensive treatment, the risk of non-cardiovascular mortality (P = 0.04) and of all fatal combined with non-fatal cardiac events (P = 0.03) was significantly higher in the top decile of the sleep-through morning surge compared to the average risk in the whole study population (table 1). When additionally adjusted for the night-to-day ratio of systolic blood pressure, the risk of all-cause mortality was 32% (P = 0.004) higher in the top decile of the sleep-through morning surge (≥ 37.0 mm Hg). For cardiovascular and non-cardiovascular death, these estimates were 18% (P = 0.30) and 42% (P = 0.005), and for all cardiovascular, cardiac, coronary, and cerebrovascular events, 30% (P = 0.01), 52% (P = 0.004), 45% (P = 0.03) and −5% (P = 0.74), respectively (table 1). Similar results were found when analysing the pre-awakening morning surge.
Table 1.
Multivariable-adjusted hazard ratios for the sleep-through and pre-awakening morning surge in systolic blood pressure
| Outcomes (number of events) | Sleep-through surge | Pre-awakening surge | ||
|---|---|---|---|---|
| Adjusted | Fully adjusted | Adjusted | Fully adjusted | |
| Mortality | ||||
| All causes (785) | 1.18 (0.99 – 1.42) | 1.32 (1.09 – 1.59)† | 1.11 (0.91 – 1.35) | 1.23 (1.00 – 1.51)* |
| Cardiovascular (287) | 1.06 (0.78 – 1.43) | 1.18 (0.87 – 1.61) | 1.08 (0.78 – 1.51) | 1.22 (0.87 – 1.71) |
| Non-cardiovascular (473) | 1.28 (1.01 – 1.61)* | 1.42 (1.11 – 1.80)† | 1.13 (0.87 – 1.46) | 1.23 (0.95 – 1.61) |
| Fatal and non-fatal events | ||||
| All cardiovascular (611) | 1.18 (0.97 – 1.44) | 1.30 (1.06 – 1.60)* | 1.31 (1.06 – 1.61)† | 1.45 (1.17 – 1.80)‡ |
| Cardiac (317) | 1.36 (1.04 – 1.78)* | 1.52 (1.15 – 2.00)† | 1.52 (1.14 – 2.01)† | 1.69 (1.26 – 2.27)‡ |
| Coronary (228) | 1.35 (0.98 – 1.85) | 1.45 (1.04 – 2.03)* | 1.50 (1.08 – 2.09)* | 1.64 (1.16 – 2.49)† |
| Cerebrovascular (281) | 0.89 (0.65 – 1.23) | 0.95 (0.68 – 1.32) | 1.04 (0.75 – 1.44) | 1.13 (0.81 – 1.58) |
| Infarction (140) | 0.79 (0.49 – 1.27) | 0.85 (0.52 – 1.39) | 1.26 (0.82 – 1.92) | 1.46 (0.93 – 2.30) |
| Haemorrhage (70) | 1.57 (0.90 – 2.73) | 1.46 (0.81 – 2.63) | 1.18 (0.64 – 2.18) | 1.11 (0.59 – 2.11) |
Hazard ratios (95% confidence intervals) express the risk in the top decile of the sleep-through or pre-awakening morning surge in systolic blood pressure compared to the overall risk in the whole study population. The 90th percentiles were determined after stratification for ethnicity and sex. The mean values of these cut-off points across ethnicities and sex weighted for the number of participants in each of the strata were 37 mm Hg for the sleep-through morning surge and 28 mm Hg for the pre-awakening morning surge. The Cox models included cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, diabetes mellitus, antihypertensive drug treatment, 24-hour systolic blood pressure and 9 design variables coding for the deciles. In fully adjusted models, the systolic night-to-day blood pressure ratio was additionally included in the Cox model. The cause of death was unknown in 25 cases. Significance of the hazard ratios: * P < 0.05, † P < 0.01, ‡ P < 0.001. Reproduced with permission from reference 12.
In an attempt to define in a more precise manner cut-off points for risk stratification in clinical practice, we explored the risk associated with all values of the sleep-through and pre-awakening morning surge in systolic blood pressure within the 5th to 95th percentile interval. The overall risk in the whole study population was used as reference (figure 1). For the sleep-through morning surge in systolic blood pressure, the lower boundary of the 95% confidence interval of the risk function crossed unity of the hazard ratio at 24.6 mm Hg and 20.9 mm Hg for total mortality and all cardiovascular events, respectively. For the pre-awakening morning surge in systolic blood pressure these crossings occurred at 22.7 mm Hg and 21.5 mm Hg, respectively. The results of these analyses suggest that for both measures of the morning surge in systolic blood pressure a value below 20 mm Hg is probably not associated with increased risk (figure 1).
Fig. 1.
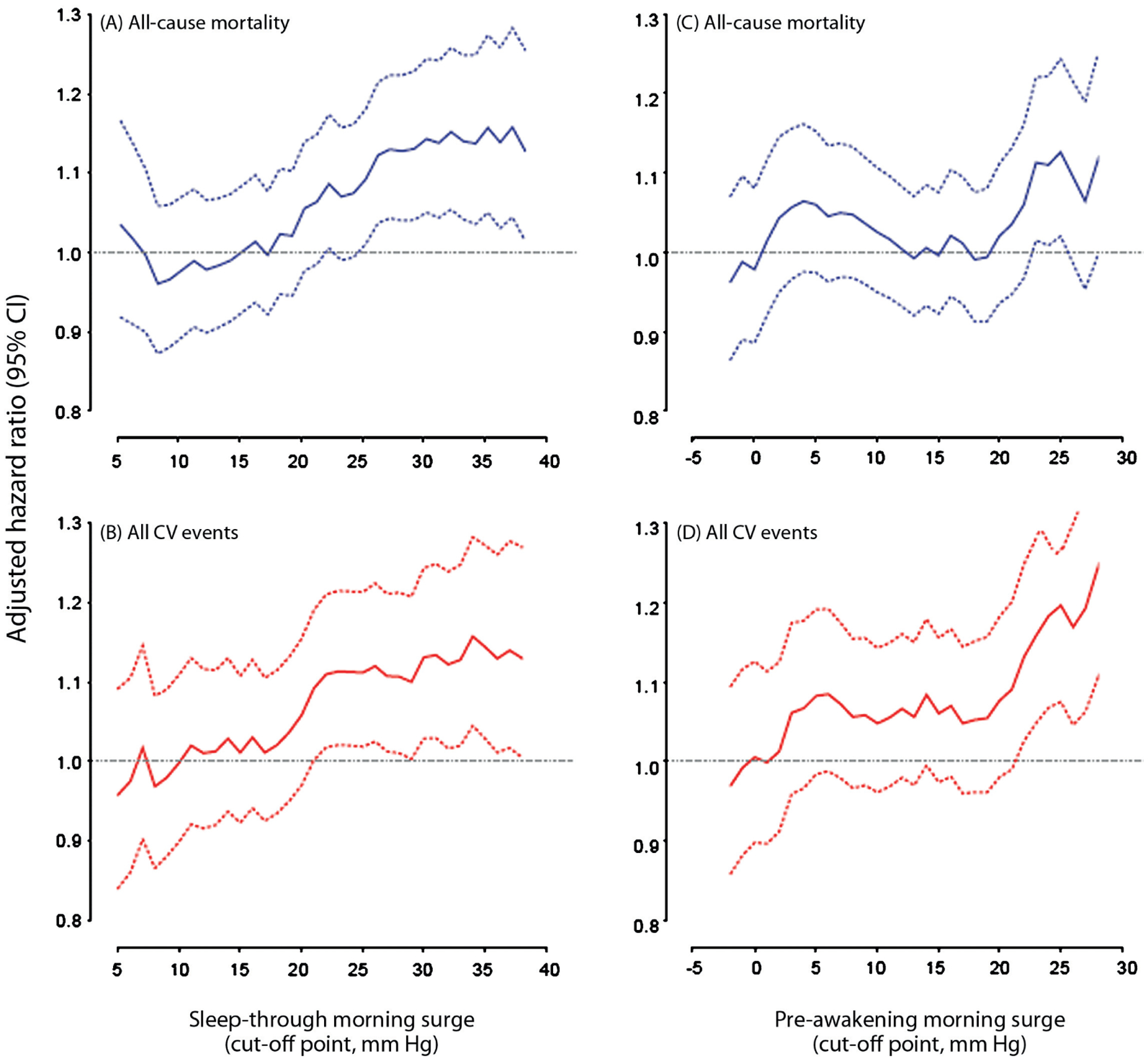
Multivariable-adjusted hazard ratios (solid lines) and their 95% confidence intervals (dashed lines) for all-cause mortality (A and C) and for all fatal combined with non-fatal cardiovascular (CV) events (B and D) by cut-off points ranging from the 5th to 95th percentile for the sleep-through (A and B) and pre-awakening (C and D) morning surge in systolic blood pressure in 5645 subjects. The hazard ratios express the risk in subjects whose morning surge exceeds the cut-off point compared to the average risk in the whole study population and were adjusted for cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, diabetes mellitus, antihypertensive drug treatment, 24-hour systolic blood pressure, and the systolic night-to-day blood pressure ratio. Reproduced with permission from reference 12.
The IDACO findings established the prognostic value of the morning surge in blood pressure in general populations. An exaggerated morning surge, exceeding the 90th percentile of the population, is an independent risk factor for mortality and cardiovascular and cardiac events. Conversely, a sleep-through or pre-awakening morning surge in systolic blood pressure below 20 mm Hg is probably not associated with an increased risk of death or cardiovascular events.
Short-term blood pressure variability
The characteristics of the studies included in the analysis of short-term reading-to-reading blood pressure variability are available in references3–11.
As measures of short-term reading-to-reading blood pressure variability, we used15 the SD over 24 hours weighted for the time interval between consecutive readings (SD24), the average of the daytime and nighttime SDs weighted for the duration of the daytime and nighttime interval (SDdn)16, and the average real variability weighted for the time interval between consecutive readings (ARV24)17. The SDdn is the mean of day and night SD values corrected for the number of hours included in each of these 2 periods, according to the formula16: SDdn = ((day SD × hours included in the daytime) + (night SD × hours included in the nighttime))/(hours included in daytime plus nighttime). This method removes the influence of the day-night blood pressure difference from the estimate of blood pressure variability. The ARV24 averages the absolute differences of consecutive measurements and accounts in this manner for the order in which the blood pressure measurements are obtained. It is calculated by the following formula:
where k ranges from 1 to N-1 and w is the time interval between BPk and BPk+1. N is the number of blood pressure readings. The ARV24, SD24 and SDdn were highly correlated with one another; the correlation coefficients ranged from 0.75–0.81 (P ≤ 0.001) for systolic blood pressure, and 0.71–0.79 (P ≤ 0.001) for diastolic blood pressure.
In adjusted models not including 24-hour blood pressure level, systolic blood pressure variability predicted both total and cardiovascular mortality (table 2; P ≤ 0.04), with the exception of SD24 in relation to total mortality (P = 0.17). We obtained similar results after additional adjustment for the 24-hour systolic blood pressure, with the exception of SD24 and SDdn, which no longer predicted cardiovascular mortality (P ≥ 0.71). Diastolic blood pressure variability predicted total and cardiovascular mortality both in adjusted and fully adjusted models (table 2; P ≤ 0.002).
Table 2.
Multivariable-adjusted standardized hazard ratios relating outcome to blood pressure variability
| Systolic blood pressure | Diastolic blood pressure | |||||
|---|---|---|---|---|---|---|
| Outcome (number of events) | SD24 | SDdn | ARV24 | SD24 | SDdn | ARV24 |
| SD, mm Hg | 15.6 | 12.2 | 11.2 | 11.8 | 9.1 | 8.5 |
| Mortality | ||||||
| Total (n = 1242) | 1.00 (0.94 – 1.07) | 1.08 (1.01 – 1.15)† | 1.11 (1.04 – 1.18)§ | 1.09 (1.03 – 1.16)‡ | 1.16 (1.09 – 1.23)§ | 1.13 (1.07 – 1.19)§ |
| Cardiovascular (n = 487) | 1.03 (0.93 – 1.13) | 1.05 (0.95 – 1.17) | 1.17 (1.07 – 1.28)† | 1.15 (1.05 – 1.26)‡ | 1.18 (1.08 – 1.29)§ | 1.21 (1.12 – 1.31)§ |
| Fatal and non-fatal events | ||||||
| Cardiovascular (n = 1049) | 1.02 (0.96 – 1.09) | 1.04 (0.97 – 1.11) | 1.07 (1.00 – 1.14)† | 1.05 (0.99 – 1.12) | 1.07 (1.01 – 1.14)† | 1.07 (1.01 – 1.13)† |
| Cardiac (n = 577) | 1.03 (0.94 – 1.12) | 1.01 (0.92 – 1.11) | 1.03 (0.94 – 1.13) | 1.02 (0.94 – 1.11) | 1.03 (0.95 – 1.12) | 1.02 (0.94 – 1.11) |
| Coronary (n = 421) | 1.07 (0.96 – 1.18) | 1.04 (0.93 – 1.16) | 1.03 (0.93 – 1.14) | 1.02 (0.93 – 1.13) | 1.02 (0.92 – 1.12) | 1.02 (0.92 – 1.12) |
| Stroke (n = 457) | 0.98 (0.88 – 1.09) | 1.03 (0.92 – 1.14) | 1.10 (1.00 – 1.21)† | 1.08 (0.99 – 1.19) | 1.09 (0.99 – 1.20) | 1.14 (1.05 – 1.23)† |
Values are standardized hazard ratios (95% confidence intervals), which express the risk per SD increase in the predictor variables. All hazard ratios were computed by Cox regression stratified for cohort and adjusted for sex, age, 24-hour blood pressure and heart rate, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, diabetes mellitus, and treatment with antihypertensive drugs. Significance of the hazard ratios: † P < 0.05, ‡ P < 0.01, and § P < 0.001. Reproduced with permission from reference 15.
In adjusted analyses not including the 24-hour blood pressure level, systolic blood pressure variability predicted all of the fatal combined with non-fatal outcomes (P ≤ 0.03) with the exception of coronary events (P ≥ 0.07). However, in fully adjusted analyses, systolic blood pressure variability lost its predictive value with the exception of ARV24 in relation to all cardiovascular events combined and stroke (table 2). Diastolic blood pressure variability was predictive of all combined end points (P ≤ 0.03) with the exception of coronary events (P ≥ 0.15). In fully adjusted models, diastolic blood pressure variability only predicted all cardiovascular events combined (ARV24 and SDdn) and fatal plus non-fatal stroke (ARV24) (table 2).
Figure 2 shows the absolute risk of a combined cardiovascular event in relation to 24-hour blood pressure at different levels of systolic and diastolic ARV24 (panels A and B). The analyses were standardized to the distributions (mean or ratio) of cohort, sex, age, 24-hour heart rate, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, diabetes mellitus, and treatment with antihypertensive drugs. Absolute risk increased with both the 24-hour blood pressure (P < 0.001) and ARV24 (P ≤ 0.04). However, with the 24-hour blood pressure in the model, ARV24 added only 0.1% to the explained risk of a composite cardiovascular event15.
Fig. 2.
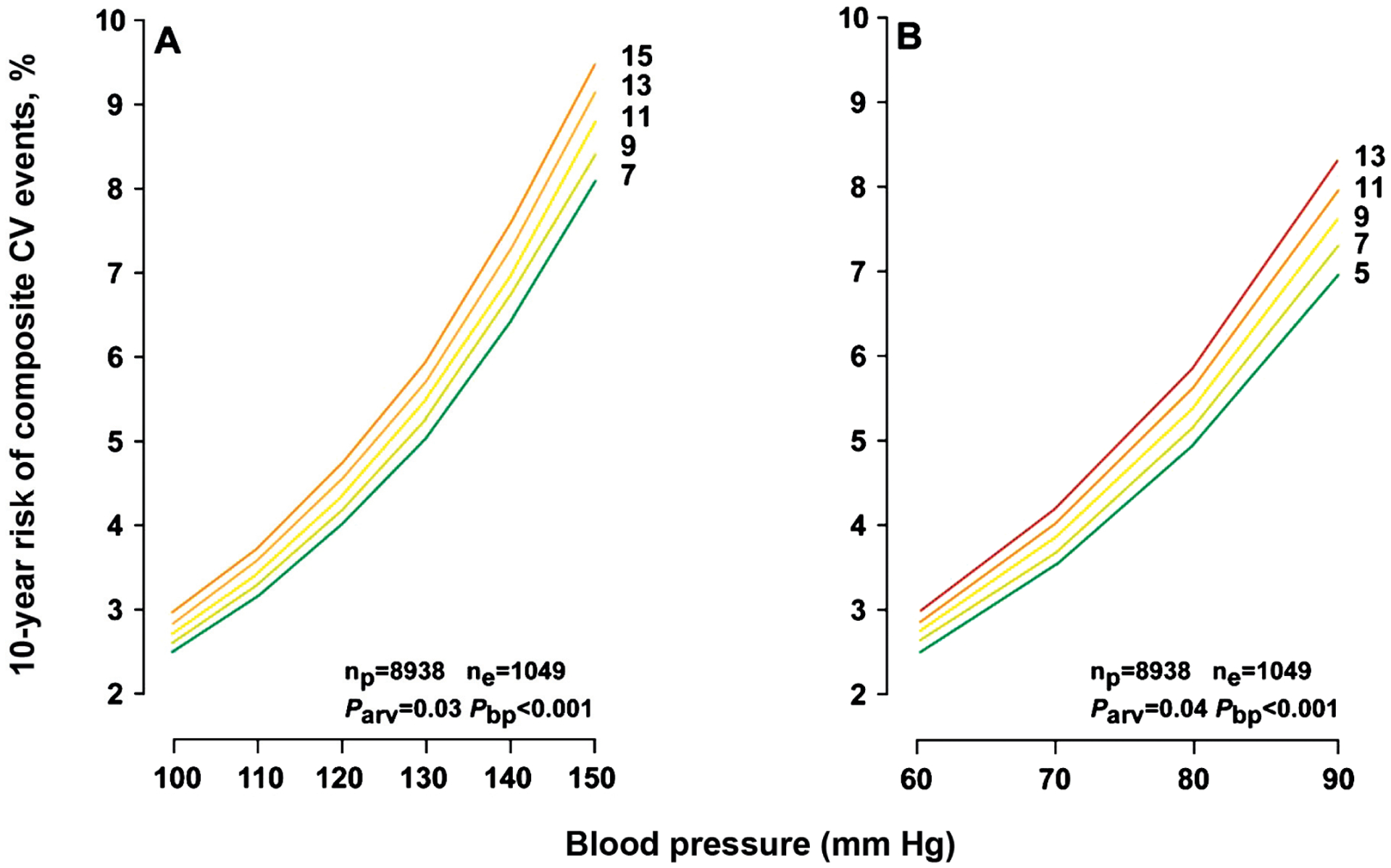
Ten-year absolute risk of combined cardiovascular events in relation to 24-hour blood pressure (A and B) at different levels of systolic and diastolic average real variability over 24 hours (ARV24). The analyses were standardized to the distributions (mean or ratio) of cohort, sex, age, 24-hour heart rate, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, diabetes mellitus, and treatment with antihypertensive drugs. Plotted values of 24-hour blood pressure span the 5th to 95th percentile interval. The continuous risk functions correspond with the 5th, 25th, 50th, 75th and 95th percentile of ARV. P-values are for the independent effect of ARV (Parv) and 24-hour blood pressure (Pbp). np and ne indicate the number of participants at risk and the number of cardiovascular events. Reproduced with permission from reference 15.
The IDACO report established that short-term reading-to-reading blood pressure variability is an independent risk factor, but moreover it also highlighted that the level of the 24-hour blood pressure remains the primary blood pressure-related risk factor to account for in clinical practice. For research making use of intermittent techniques of ambulatory blood pressure monitoring, our current findings suggest that both SDdn and ARV24 might be useful measures, but not the SD computed over the whole day, which also includes the day-night blood pressure difference. One possible limitation of the current analyses is that there is no published information on the number of readings required to assess blood pressure variability in a reliable or reproducible manner.
CONCLUSIONS
The level of the 24-hour blood pressure remains the primary blood pressure-related risk factor to account for in clinical practice. Notwithstanding the new insights generated by the IDACO, several research questions about the prognostic value of short-term blood pressure variability remain to be answered in the future. First, the morning surge above the 90th percentile significantly and independently predicted cardiovascular outcome and might contribute to risk stratification by ambulatory blood pressure monitoring. However, randomized clinical trials are needed to answer the question whether restoring the diurnal blood pressure profile might be beneficial in terms of the prevention of cardiovascular morbidity and mortality. Secondly, the prognostic value of blood pressure variability seems limited in comparison with the 24-hour blood pressure level. However, in the setting of clinical research, studies of blood pressure variability will continue to generate meaningful information.
ACKNOWLEDGEMENTS
The European Union (grants IC15-CT98-0329-EPOGH, LSHM-CT-2006-037093, and HEALTH-F4-2007-201550), the Fonds voor Wetenschappelijk Onderzoek Vlaanderen (Ministry of the Flemish Community, Brussels, Belgium; grants G.0575.06 and G.0734.09), and the Katholieke Universiteit Leuven (grants OT/00/25 and OT/05/49) gave support to the Studies Coordinating Centre in Leuven. The European Union (grants LSHM-CT-2006-037093 and HEALTH-F4-2007-201550) also supported the research groups in Kraków and Shanghai. The authors gratefully acknowledge the secretarial assistance of Ms Sandra Covens and Ms Ya Zhu (Studies Coordinating Centre, University of Leuven, Leuven, Belgium).
Footnotes
CONFLICT OF INTEREST: none declared.
REFERENCES
- 1.O’Brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P, on behalf of the European Society of Hypertension Working Group on Blood Pressure Monitoring. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005; 23: 697–701. [DOI] [PubMed] [Google Scholar]
- 2.Staessen JA, Wang J, Bianchi G, Birkenhäger WH. Essential hypertension. Lancet 2003; 361: 1629–41. [DOI] [PubMed] [Google Scholar]
- 3.Hansen TW, Jeppesen J, Rasmussen F, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and mortality: a population-based study. Hypertension 2005; 45: 499–504. [DOI] [PubMed] [Google Scholar]
- 4.Staessen JA, Bieniaszewski L, O’Brien ET, Imai Y, Fagard R. An epidemiological approach to ambulatory blood pressure monitoring: the Belgian population study. Blood Press Monit 1996; 1: 13–26. [PubMed] [Google Scholar]
- 5.Kuznetsova T, Malyutina S, Pello E, Thijs L, Nikitin Y, Staessen JA. Ambulatory blood pressure of adults in Novosibirsk, Russia: interim report on a population study. Blood Press Monit 2000; 5: 291–6. [DOI] [PubMed] [Google Scholar]
- 6.Kuznetsova T, Staessen JA, Kawecka-Jaszcz K, Babeanu S, Casiglia E, Filipovský J, Nachev C, Nikitin Y, Peleská J, O’Brien E, on behalf of the EPOGH Investigators. Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit 2002; 7: 215–24. [DOI] [PubMed] [Google Scholar]
- 7.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 2002; 20: 2183–9. [DOI] [PubMed] [Google Scholar]
- 8.Li Y, Wang JG, Gao HF, Nawrot T, Wang GL, Qian YS, Staessen JA, Zhu DL. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit 2005; 10: 125–34. [DOI] [PubMed] [Google Scholar]
- 9.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H, Hypertension Working Group: Ambulatory blood pressure. Normality and comparison with other measurements. Hypertension 1999; 34(part 2): 818–25. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens 1991; 9: 355–60. [DOI] [PubMed] [Google Scholar]
- 11.Ingelsson E, Björklund K, Lind L, Ärnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA 2006; 295: 2859–66. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Hansen TW, Kikuya M, Boggia J, Richart T, Metoki H, Ohkubo T, Torp-Pedersen C, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Sandoya E, Kawecka-Jaszcz K, Ibsen H, Imai Y, Wang JG, Staessen JA, on behalf of the International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) investigators. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension 2010; 55: 1040–8. [DOI] [PubMed] [Google Scholar]
- 13.Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as predictor of silent and clinical cerebrovascular disease in elderly hypertensives. A prospective study. Circulation 2003; 107: 1401–6. [DOI] [PubMed] [Google Scholar]
- 14.Metoki H, Ohkubo T, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai K. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension 2006; 47: 149–54. [DOI] [PubMed] [Google Scholar]
- 15.Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 2010; 55: 1049–57. [DOI] [PubMed] [Google Scholar]
- 16.Bilo G, Giglio A, Styczkiewicz K, Caldara G, Maronati A, Kawecka-Jaszcz K, Mancia G, Parati G. A new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fall. J Hypertens 2007; 25: 2058–66. [DOI] [PubMed] [Google Scholar]
- 17.Mena L, Pintos S, Queipo NV, Aizpúrua JA, Maestre G, Sulbarán T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens 2003; 23: 505–11. [DOI] [PubMed] [Google Scholar]


