Abstract
Aim
To explore resilience and associated factors in spousal caregivers of patients with cancer.
Design
An integrative review.
Methods
This review used the standardized critical appraisal instruments developed by the Joanna Briggs Institute and was conducted by researching the electronic databases of Cochrane, CINAHL, ProQuest, Science Direct, PubMed, Scopus, EBSCO and Google Scholar. The articles were published in English with full text from January 2010 to January 2020.
Results
According to data retrieval, 26 articles were finally selected. From this review, resilience was typically measured by using exact resilience scales (i.e. Connor‐Davidson or Wagnild Resilience Scales) or using other variables to indicate either more positive psychological outcomes or less negative psychological outcomes. For factors associated with resilience, these were classified as individual internal and external factors. Internal factors included caregiver burden, psychological distress, coping strategies and other factors, whereas social support, couple interaction, patient health status and other parameters were considered external factors.
Conclusions
Resilience plays an important role in promoting positive adaptation in spite of adversity among the spousal caregivers of patients with cancer. Due to the uniqueness of resilience among spousal caregivers, ways to assess resilience and identify its associated factors deserve more attention and careful consideration.
Keywords: cancer patients, caregivers, factors, nurses, nursing, resilience, spouse
1. INTRODUCTION
Cancer mortality is rapidly growing and is a major public health problem worldwide. There were an estimated 18.1 million new cases of cancer and 9.6 million deaths from cancer worldwide in 2018 (Ferlay et al., 2019). World Health Organization (WHO) (2020) estimated that the number of new cases of cancer would be projected to rise to 26 million globally in 2040 leading to an increase in the global cancer burden. Cancer marks a critical life event for the entire family that can cause distress and significant challenges for all involved (Engeli et al., 2016). Cancer has a tremendous effect on patients, and it also has a profound influence on patients' spouses and family, as many patients with cancer are reliant on the care provided by their family. Moreover, spouses or partners are most often the primary caregivers of people with cancer and they are at particular risk for caregiving burden. Previous studies have revealed that this burden of family caregivers can lead to role strain and stress, increasing caregivers’ own risk for morbidity and mortality (Gibbons et al., 2019). Large studies in caregivers of patients diagnosed with cancer have reported a high prevalence of depression reaching 72% (Lutfi & Al Lami, 2019) and spousal caregivers who resided with the patient appeared more vulnerable to suffer from or have psychological symptoms like depression and anxiety, finally diminishing the quality of life (QOL; Shaffer et al., 2017).
Transitioning from partners to being caregivers can lead to a decline in health, independence and freedom as a result of providing daily care for their love ones. Providing care for a patient with cancer has an impact on disease prognosis and is taken for granted as a responsibility by the public. Some studies have reported that the spouses of patients with cancer developed mental problems due to their caregiving experiences (Jia et al., 2015; Li et al., 2013). They found that partners reported more emotional distress than the patients with cancer. When spousal caregivers are highly distressed, the QOL of patients with cancer also declines over time (Northouse & McCorkle, 2010).
Previously, studies in spousal caregivers have often focused on the negative aspects, such as exploring risk factors and adverse consequences. The results have revealed that spousal caregivers of patients with cancer had poorer physical, psychological, social and even spiritual outcomes than those who were not the spousal caregivers or family members (Hlubocky et al., 2019; Kim et al., 2015); In addition, it has been estimated that spousal caregivers experienced higher levels of stress, poorer mental health, lower levels of general well‐being and poorer physical outcomes than non‐carers (Northouse & McCorkle, 2010). In spite of adversity, these spousal caregivers have experienced; some of them showed resilience. However, the studies regarding the positive aspects and protective factors closely associated with recovery and adaptation among spousal caregivers of patients with cancer are scarce.
According to Yoon et al. (2019), the term “resilience” was defined in a variety of manners in the previous studies and the consistent explanation across the studies pertained to the function of resilience in motivating caregivers to remain mentally healthy to help them cope with the anxiety and depression caused by their adverse life events (Palacio et al., 2018). Moreover, many studies that have examined the role of resilience in caregivers of patients with dementia had series of achievements (Joling et al., 2016; Teahan et al., 2018). Resilience of spousal caregivers represents the process of psychological adaptation in a particular time of caring (Mulud & McCarthy, 2017; O’Rourke et al., 2010) and the factors of resilience across the caregiving stages requires further exploration.
Therefore, it is significant to focus on resilience of the spouses who are primary caregivers of patients with cancer and review factors associated with their resilience. The purpose of this review is to identify the measurement used to assess resilience and to review and synthesize related factors of resilience in spousal caregivers of patients with cancer.
2. METHODS
2.1. Selection strategy
This review of studies was related to factors of resilience in the field of spousal caregivers of patients with cancer in compliance with the PRISMA statement. A literature search was conducted using the following internet databases: Cochrane, CINAHL, Science Direct, PubMed, Scopus, EBSCO and Google Scholar, to identify relevant studies published from January 2010 to January 2020 published in English. To search academic articles across several disciplines including nursing, psychology, sociology and medicine, an expert librarian was consulted for the selected databases. The initial search terms used the following Medical Subject Heading (MeSH) terms and text words (Table 1). Snowball searches were used to screen the literatures databases gradually.
TABLE 1.
English search terms
| String 1 | resilience or resiliency or resilient |
| String2 | “spousal caregiver” or “family caregiver” or “carer” or “spouses” or “partner” or “partners” |
| String 3 | cancer or malignancy or malignant tumor or malignant or oncology |
| Final search | (resilience or resiliency or resilient) AND (“spousal caregiver” or “family caregiver” or “carer” or “spouses” or “partner” or “partners”) AND (cancer or malignancy or malignant tumor or malignant or oncology) |
2.2. Inclusion and exclusion criteria
The articles retrieved by the search were assessed by the first author and were considered if they met the following eligibility: (a) resilience in spousal caregivers for patients with cancer who were alive; (b) resilience by using resilience scales or measure resilience by using related variables that reflected resilience that were clearly mentioned in the articles; (c) spousal caregivers’ age greater than 18‐year‐old; (d) quantitative, qualitative and mixed‐method research; and (e) articles that met the above eligible criteria were included in this review if it was possible to extract the findings.
2.3. Data extraction
The data were extracted using standardized data extraction criteria adapted from the PRISMA flow diagram (Figure 1). Initially, a total of 2,348 articles were identified. After removing duplicates, 246 articles remained to be screened. The titles and abstracts of these articles were screened following the JBI Critical Appraisal Checklist (Joanna Briggs Institute, 2014). A total of 94 articles that did not meet the inclusion criteria were excluded. Next, 152 articles remained and they were full text screened. Finally, 26 articles were included that met the inclusion criteria for this systematic review. Summary tables (Table 2) were used to show the factors related to resilience included in the review. In addition, more details including design, participants, measurement, results and quality are listed in the supplementary materials (Table S1).
FIGURE 1.
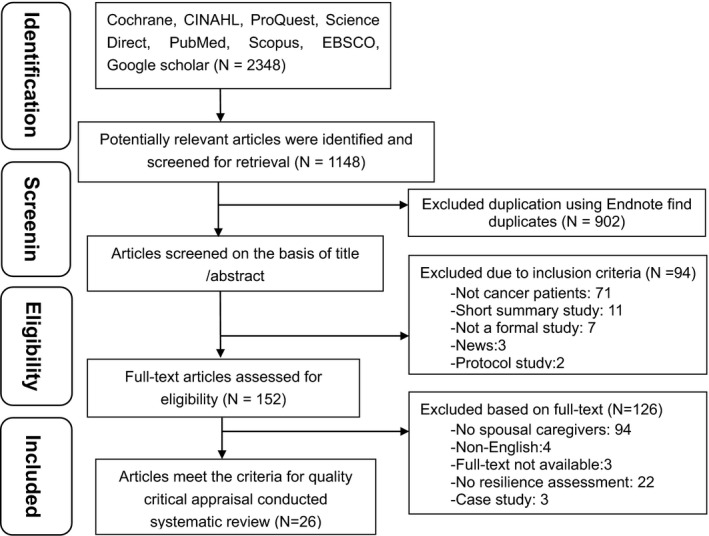
Four steps of flow diagram
TABLE 2.
Summary of factors related to resilience included in the review
| Category | Sub category | Details | Number of literatures | Average score |
|---|---|---|---|---|
| Internal factors | Positive factors | Coping strategy |
7 (Elliott et al., 2015; Engeli et al., 2016; Gibbons et al., 2019; Luo et al., 2019; McDonald et al., 2018; Opsomer et al., 2019; Street et al., 2010) |
1.64 |
| Spirituality |
3 (Greeff & Thiel, 2012; McDonald et al., 2018; Palacio & Limonero, 2019) |
1.74 | ||
| Positive personality characteristics |
5 (Cassidy, 2013; Hwang et al., 2018; Jones et al., 2015; Lim et al., 2014; Tang et al., 2013) |
1.86 | ||
| Post‐traumatic growth |
2 |
1.87 | ||
| Negative factors | Caregiver burden |
8 (Cassidy, 2013; Hwang et al., 2018; Jones et al., 2015; Li et al., 2018, 2019; Liu et al., 2018; Palacio et al., 2018; Tang et al., 2013) |
1.86 | |
| Psychological distress |
6 (Cassidy, 2013; Hwang et al., 2018; Lim et al., 2014; Palacio & Limonero, 2019; Senneseth et al., 2017; Simpson et al., 2015) |
1.80 | ||
| Caregivers physical health status |
3 (Hwang et al., 2018; Karatzias et al., 2017; Senneseth et al., 2017) |
1.78 | ||
| External factors | Positive factors | Family and social support |
9 (Cassidy, 2013; Greeff & Thiel, 2012; Hwang et al., 2018; Lim et al., 2014; Luo et al., 2019; McDonald et al., 2018; Opsomer et al., 2019; Senneseth et al., 2017; Tang et al., 2013) |
1.78 |
| Dyadic interaction |
6 (Elliott et al., 2015; Gibbons et al., 2019; Lillie et al., 2018; Lim et al., 2014; McDonald et al., 2018; Roen et al., 2018) |
1.67 | ||
| Positive aspects of caring |
2 |
1.87 | ||
| Negative factors | Patients’ health status |
7 (Bookwala, 2014; Hwang et al., 2018; Li et al., 2018, 2019; Liu et al., 2018; Opsomer et al., 2019; Saria et al., 2017) |
1.81 | |
| Adverse life events |
2 |
1.72 |
2.4. Data synthesis and assessment
The research results were presented as a narrative summary. Each paper was rated for quality using the “standard quality assessment criteria for evaluating primary research papers from a variety of fields” (Kmet et al., 2004). There are 14 criteria that were used to evaluate quantitative studies, including study design rationality, method and outcome validity, and results and conclusions. in the checklist. They are 10 criteria for qualitative studies, including study design evidence, theoretical framework and context clarity, data collection and analysis systematic, procedure credibility and reflexivity, and other factors, on the assessment checklist. When dealing with the mix‐method studies, both qualitative and quantitative assessment criteria were used to obtain an average score. The maximum possible average quality score is 2.0, and the minimum score is zero. In the evaluation process, for this study, an article that scored below 1.5 was regarded as low quality and was not be included the review (Tables S2 and S3).
3. FINDINGS
3.1. Description of the studies
For the purpose of reporting, the characteristics of the 26 articles were summarized (Table S1). With regard to the methodologies, 17 articles were quantitative studies and these included 14 cross‐sectional and 3 longitudinal studies. The statistics used in quantitative studies included Student's t test, Pearson and Spearman correlations, and linear and logistic regression analysis. These were used to evaluate the factors associated with resilience among spousal caregivers. In addition, nine articles were qualitative studies that included three mixed‐method researches. The qualitative studies used semi‐structured interviews as a strategy for gathering information and their analyses were based on thematic, content, phenomenological and grounded analysis methods. Regarding the study populations, 17 articles included not only spousal caregivers and nine articles reported only on spousal caregivers. Furthermore, 24 articles reported the outcomes of cancer caregivers and 2 articles reported on the outcomes of cancer caregivers, as well as caregivers of other types of diseases. With regard to countries, there were five studies conducted in the USA, China and Australia, respectively. There were two articles each from the UK and Norway, and the remaining seven articles were from Switzerland, South Africa, Canada, Spanish, Taiwan, South Korea and Hong Kong. For the relationship between spousal caregivers and patients, most of the studies included women, especially more wives, with mean ages in the middle‐age and elderly range.
3.2. Methodological quality
The results of the methodological quality assessment for the 26 articles are summarized. All of the 26 articles met the criteria of sufficient quality, with strong to good levels (Kmet et al., 2004). However, there were no high‐quality level articles like RCT, or a meta‐analysis.
3.3. Characteristics of spousal caregivers
The first demographic characteristic was sex. Two articles reported sex was related to resilience (Bookwala, 2014; Street et al., 2010). Street et al. (2010) stated that a high level of resilience was displayed by most wife caregivers. However, there were conflicting results from Bookwala (2014) who identified that the female resilience scores were lower than those of men. One study found that sex and resilience had no significant relationship (Simpson et al., 2015). The second characteristic was age. Four articles found that resilience was age‐related (Jones et al., 2015; Opsomer et al., 2019; Simpson et al., 2015; Tang et al., 2013;). Three studies indicated that a higher resilience was correlated with increasing age (p < .05) (Opsomer et al., 2019; Simpson et al., 2015; Tang et al., 2013). However, Jones et al. (2015) found elderly spousal caregivers had lower resilience than general adult population (p < .01). The third characteristic examined was educational level. Only one article found caregivers who had higher educational levels had resilience (p < .05, 95% CI = 1.03, 2.76) (Tang et al., 2013). But there was one article that showed no significant association between resilience and educational level (Simpson et al., 2015). The fourth characteristic was relationship with patients. This review focuses on spousal caregiver resilience, and it was further verified from previous evidence that spousal caregivers showed higher resilience than other family caregivers in four articles (Cassidy, 2013; Jia et al., 2015; Jones et al., 2015; Tang et al., 2013). Only Simpson et al. (2015) found that there was no difference between spousal and other caregivers on resilience scores. The last characteristic was child‐rearing while facing spousal cancer. Only one article (Senneseth et al., 2017) showed that spousal caregivers had low resilience (z = 2.31, p = .02) because parenting children may increase the life stress and this demanded more energy to deal with the caregiving challenge.
In summary, resilience in spousal caregivers of patients with cancer was found to be higher in those of the female sex, younger age, better education and with no child‐rearing burden. However, other demographic characteristics, such as ethnicity, occupation and work status, were not found to be associated with resilience in this review.
3.4. Measurement used to indicate resilience
3.4.1. Using exact resilience scales to assess resilience
The first exact resilience scale used was the Connor‐Davidson Resilience Scale (CD‐RISC; Connor & Davidson, 2003). Five articles using this scale were found, which was the most widely used scale in this review (Hwang et al., 2018; Jia et al., 2015; Karatzias et al., 2017; Li et al., 2018; Luo et al., 2019;). The original scale had 25 items (CD‐RISC‐25) on the self‐reporting scale and was widely used in the following groups: community samples, primary care outpatients, general psychiatric outpatients, clinical trial of generalized anxiety disorder and two clinical trials of post‐traumatic stress disorder. There existed a brief version called the 10‐item Connor‐Davidson resilience scale (CD‐RISC‐10) that was also used to assess resilience (Campbell‐Sills & Stein, 2007). The CD‐RISC measures several components of resilience, including the ability to adapt to change, deal with what comes along, cope with stress, stay focused and think clearly, not get discouraged in the face of failure and handle unpleasant feelings, such as anger, pain or sadness. In this review, these scales had been translated into Chinese (Yu & Zhang, 2007), South Korean (Yang et al., 2013), Spanish (Notario‐Pacheco et al., 2011), South African (Jorgensen & Seedat, 2008) and a Japanese version (Nishi et al., 2013).
The second scale used in these reviewed studies was the Wagnild Resilience Scale (RS; Wagnild & Young, 1993). In the 17 quantitative articles, two articles measured resilience using this scale (Saria et al., 2017; Simpson et al., 2015). This scale can be used to assess the ability to successfully deal with life adversities. This is a psychometrically sound measure with higher scores showing higher resiliency. The 25‐item RS (RS‐25) has two subscales, a 17‐item personal competence and an 8‐item acceptance of self and life (Wagnild, 2009). The 14‐item short form of RS (RS‐14) is an offshoot of the 25 items and measures similar psychological concepts. The RS‐14 as constructed by Wagnild comprised of five essential characteristics of a meaningful life, perseverance, self‐reliance, equanimity and existential aloneness. The Wagnild Resilience Scale has been used with a variety of individuals of different ages, socio‐economic and educational backgrounds, and it is a reliable and valid tool to measure resilience (Wagnild, 2009).
The third scale used was the Brief Resilience Scale (BRS) (Smith et al., 2008). There were two articles that used this scale (Cassidy, 2013; Lim et al., 2014). It is a six‐item self‐report instrument that employs the positive psychology toolkit which measures the ability to bounce back from stress on a Likert scale with higher scores indicating higher resilience. It is predictably related to personal characteristics, social relations, coping and health. Unlike the previous measures that assess protective factors or resources, it is used to measure resilience in terms of how an individual adapts to stress, bounces back, resists illness and thrives in the face of adversity.
The fourth scale used was the Brief Resilience Coping Scale (BRCS) (Sinclair & Wallston, 2004). Of the 17 quantitative articles, this scale was used in two articles (Palacio et al., 2018; Palacio & Limonero, 2019). It is a four‐item measure designed to capture tendencies to cope with stress in a highly adaptive manner. The BRCS has adequate internal consistency (r = 0.76) and test–retest reliability (r = 0.71). Its convergent validity is demonstrated by predictable correlations with measures of personal coping resources, pain coping behaviours and psychological well‐being. This scale had also been translated into many language versions (Fung, 2020; López‐Pina et al., 2016).
The last scales used were the Dispositional Resilience Scale (DRS; Bartone et al., 1989) and Family Resilience Assessment Scale (FRAS; Sixbey, 2005). In the selected articles, only one article used the DRS (Senneseth et al., 2017). It is comprised of 45 items with responses recorded along a four‐point Likert‐type scale. The DRS was developed as a measure of hardiness or psychological resilience comprised of three interrelated factors or subscales: perceived control; commitment; and challenge. In addition, there were two studies that used the Chinese version of the Family Resilience Assessment Scale (FRAS‐C; Li et al., 2016). The Chinese version scale has 32 items and comprised of three subscales: family communication and problem‐solving, use of social resources and maintenance of a positive outlook.
3.4.2. Using psychological outcome variables to indicate resilience
According to this review, some studies identified resilience based on the use of positive or negative psychological outcome variables to reflect resilience. The resilience of spousal caregivers was described as either having more positive psychological outcomes like good adaptation, well‐being and positive coping, or less negative psychological outcomes like depression and stress. There were three articles that evaluated resilience by using positive psychological outcomes. One study (Gibbons et al., 2019) used a well‐being scale, and Jones et al. (2015) used some psychological variables to reflect resilience such as coping styles and traits of mindfulness. They used six standardized questionnaires to measure resilience in caregivers of elderly cancer survivors. Additionally, Bookwala (2014) measured resilience using mastery and self‐esteem to explore resilience. In addition, there was one article that appraised resilience by using negative psychological outcome by examining depression (Tang et al., 2013). Jones et al. (2015) used resilience‐related factors to evaluate resilience comprehensively, including severity of distress symptoms, coping strategies, caregiver's QOL, caregiver burden and mindfulness. Greeff and Thiel (2012) used the Resiliency Model of Stress, Adjustment and Adaptation to assess family adaptation and aspects of family functioning in spouses of prostate cancer, which was a technique to employ life course theory and the stress‐coping process as the guiding theoretical frameworks to assess resilience.
In summary, there were several different resilience measurements used in the reviewed studies that varied in terms of purpose, focus and method of analyses. Two types of measurements in resilience were explored across 26 studies. A total of 15 articles identified resilience by using resilience scales, and other articles used positive outcomes as the measurement to indicate resilience, including positive outcomes like coping skills, adaptation, mindfulness, self‐efficacy and negative outcomes such as depression, stress and caregiver burden. They are not directly comparable for evaluating resilience. Nevertheless, there was considerable overlap in dimensions of resilience and indicators used to some extent.
3.5. Classification of factors associated with resilience
By virtue of the resilience pattern of individual internal and external resources in coping with adversity (Garcia‐Dia et al., 2013), this study classified related factors of resilience into internal and external factors. Internal factors referred to any factors within the caregivers themselves and under the control of caregivers no matter whether they were tangible or intangible including both positive and negative aspects, such as personality psychological traits, physical quality and self‐help skills. In contrast, external factors were those that affected elements outside and under no control of caregivers like family, community and socio‐economic resources. Additionally, the factors were divided into either having positive or negative effects on resilience.
3.5.1. Internal factors
Internal factors that had positive effects on resilience
Seven studies investigated positive coping strategies factors to promote resilience (Elliott et al., 2015; Engeli et al., 2016; Gibbons et al., 2019; Luo et al., 2019; McDonald et al., 2018; Opsomer et al., 2019; Street et al., 2010). In all the review studies, coping strategies included problem‐solving or decision‐making abilities according to cancer variant of the situation. These included many coping skills such as distraction, manageability, role adjustment, individual competences, maintaining normality and creating a new normality. For instance, positive coping skills appeared to have a protective effect on resilience in spousal caregivers (r = 0.34; p < .05; Luo et al., 2019). Hence, positive coping strategies as adaption processes had a protective role on resilience for spousal caregivers.
Five articles proposed that resilience was associated with positive personality characteristics, which refers to individual's difference in patterns of thinking, feelings and behaviours, such as self‐efficacy, self‐confidence and self‐esteem (Cassidy, 2013; Hwang et al., 2018; Jones et al., 2015; Lim et al., 2014; Tang et al., 2013). First, mindfulness and optimism were considered to be positive thoughts (Cassidy, 2013; Jones et al., 2015; Lim et al., 2014). For instance, mindfulness as a coping ability in dealing with acutely distressed caregivers may be critical for lower levels of depression and anxiety (r = −0.26 to −0.37, p < .5; Jones et al., 2015). In addition, self‐efficacy (r = 0.15, p < .01; Cassidy, 2013), self‐esteem (OR = 1.82, 95% CI = 1.12, 2.94, p = .016; Hwang et al., 2018) and self‐confidence (OR = 0.26, 95% CI = 10.65, p < .05; Tang et al., 2013) were associated with resilience which was mentioned in one study. Therefore, it appears logical that positive personality characteristics would enhance caregiver resilience, while there was not enough evidence to estimate resilience as an outcome using these factors.
Three studies found that spiritual and religious faith played an important role in caregiver resilience (Greeff & Thiel, 2012; McDonald et al., 2018; Palacio & Limonero, 2019). In a correlation analysis, there was a positive correlation between resilience and spirituality (r = 0.220, p < .05; Palacio & Limonero, 2019). Spiritual competence was identified as a protective factor that contributed to resilience in primary caregivers by using religious teaching and gatherings, belief, hope, strength and faith obtained from spiritual support (Maneewat et al., 2016). Hence, spirituality was found as a positive factor that promoted resilience in spousal caregivers in the context of cancer.
Two studies identified that resilience was significantly related to the caregivers’ post‐traumatic growth (Jia et al., 2015; Palacio & Limonero, 2019). Both these articles showed that resilience was a positive predictor of post‐traumatic (R 2 = .058, F = 5.645, p = .044; R 2 = .155, t = 4.81, p < .05, respectively). Therefore, post‐traumatic growth can be used as the outcome variable to assess spousal caregiver resilience.
Internal factors that had negative effects on resilience
Eight articles found that the caregiver burden or perceived burden or stress was negatively related to resilience (Cassidy, 2013; Hwang et al., 2018; Jones et al., 2015; Li et al., 2018, 2019; Liu et al., 2018; Palacio et al., 2018; Tang et al., 2013). In a multiple regression analysis, resilience was negatively associated with caregiver burden (β = −0.28, p = .003; Liu et al., 2018), (β = −0.052, p < .05; Li et al., 2018). Thus, resilience had direct and indirect effects on caregiver burden and caregiver burden was a vulnerability factor; that is, the more resilient the spousal caregiver was, the more likely they were able to move towards lessened burden.
Six articles showed there was a relationship between resilience psychological distress (Cassidy, 2013; Hwang et al., 2018; Lim et al., 2014; Palacio & Limonero, 2019; Senneseth et al., 2017; Simpson et al., 2015). Psychological distress is a negative emotional state characterized by physical and/or emotional discomfort, pain, or anguish. For example, anxiety and depression, as emotional distress variables, were closely related to resilience and even no depression was a predictor of high resilience (p = .001, OR = 3.12, 95% CI = 1.5, 6.13; Hwang et al., 2018). In addition, resilience was also a strong predictor of personal psychological distress (z = −1.99, p < .05; Lim et al., 2014). However, one study (Palacio et al., 2018) found that resilience did not have a significant influence on emotional distress (r = −0.08, p > .05). In addition, if controlling for the QOL, the correlation between resilience and psychological distress was no longer significant (r = −0.18, p = .32; Senneseth et al., 2017), which may have been due to multicollinearity. Therefore, psychological distress, such as depression and anxiety, was a risk factor to reduce resilience but researchers may need to consider possible confounding variables.
Three articles reported that caregiver's individual physical health status was related to resilience (Hwang et al., 2018; Karatzias et al., 2017; Senneseth et al., 2017). In a multiple regression analysis, a good health status was a predictor of high resilience (p = .016, OR = 2.26, 95% CI = 1.16, 4.40; Hwang et al., 2018). Therefore, it is predicted that improving the spousal caregiver's health could increase resilience.
3.5.2. External factors
External factors that had positive effects on resilience
Nine articles described that individual external support from family and society was related to resilience (Cassidy, 2013; Greeff &Thiel, 2012; Hwang et al., 2018; Lim et al., 2014; Luo et al., 2019; McDonald et al., 2018; Opsomer et al., 2019; Senneseth et al., 2017; Tang et al., 2013). Family support included economic conditions, positive communication and internal efforts of the family and social support consisted of available external resources, professional services like palliative care, information on disease and healthy. One study found that there was no significant correlation between resilience and information needs (Simpson et al., 2015). In a multiple regression analysis, positive social support was a predictor of high resilience among caregivers of patients with cancer (Hwang et al., 2018; Luo et al., 2019). Therefore, family and social support serves as a protective factor that allows spousal caregivers to reinforce and value extant social support connections while building new social connections with patients and others to sustain resilience postcancer.
Six articles showed a dyadic interaction between couples to increase resilience (Elliott et al., 2015; Gibbons et al., 2019; Lillie et al., 2018; Lim et al., 2014; McDonald et al., 2018; Roen et al., 2018). Couple interaction during long‐term caregiving revealed that the couple relationship was associated with resilience. This was a new discovery of resilience factors among spousal caregivers of patients with cancer who had no cognitive impairment. A good dyadic interaction between couples referred to coping processes, couple communication and partnerships mutuality. When intimate partners take on new roles as caregivers, everyday couple interactions take on a new and important role in managing both the transition and the adaptation to the change in health status. Gibbons et al. (2019) found that spousal caregivers who reported higher levels of closeness within their relationship reported significantly higher resilience levels. During the couple coping processes, resilience presented a dynamic trajectory over time and a poor marital relationship was associated with low resilience (Tang et al., 2013). In addition, studies of other medical illnesses also clearly showed that both resilience and distress after illness were significantly interrelated within dyads (Lim et al., 2014). Therefore, this study identified that a good dyadic interaction played a critical role for a good couple relationship quality.
Two articles showed that there was a positive correlation between resilience and the positive aspects of care (Cassidy, 2013; Palacio & Limonero, 2019). Positive aspects of caring means caregivers found benefit by defining caring in specific cultural context, such as acceptance, empathy, appreciation, family domain, positive self‐image, reprioritization and resilience. These were predictors of the benefit finding of caring (β = 0.29, p < .001; Cassidy, 2013). Hence, seeking positive aspects of caring is a good way to help spousal caregivers enhance their resilience. The relationship between resilience and benefit of caring during the stress‐coping process was evidenced in this study.
External factors that had negative effects on resilience
Seven studies found that patients’ health status was related to caregivers’ resilience. Better patient performance (OR = 1.92, 95% CI = 1.11–3.33, p = .020; Hwang et al., 2018), different therapy methods (F(2, 105) = 3.353, p = .039; Liu et al., 2018) and severity of disease and duration of care affected caregivers’ resilience (Bookwala, 2014; Hwang et al., 2018; Li et al., 2018, 2019; Opsomer et al., 2019; Saria et al., 2017). For instance, metastasis of brain cancer may increase caregiving coping difficulty, which decreases caregiver resilience (Saria et al., 2017) This also been demonstrated in caregivers of patients with dementia (Wilks et al., 2011). However, one study found that resilience was not related to the severity of the cancer and the author compared the different cancer stages of I, II, III and IV (Simpson et al., 2015). Furthermore, one study investigated that caregiver resilience was low during the early stages of a cancer diagnosis (F = 3.502, p < .05; Li et al., 2018), but one study found caregivers had high resilience in more recent diagnoses (≤5 years) due to a higher emotion‐focused coping strategy (Jones et al., 2015). Therefore, patients’ health status was a factor that influenced caregivers’ resilience, but whether it increased resilience or not still needs confirmation owing to the disease context.
Two articles showed adverse life events were associated with resilience (Karatzias et al., 2017; Opsomer et al., 2019). For instance, a higher resilience predicted greater subjective physical health and subjective mental health in the face of multiple adverse life events, such as a diagnosis of incurable cancer (β = −0.142, p = .001 and β = −0.572, p = .049, respectively; Karatzias et al., 2017). Therefore, adverse life events as an antecedent of resilience mediated the relationship between adverse life events and well‐being.
In summary, 12 resilience‐related factors were classified as internal and external elements including positive and negative influences. Resilience was examined from the aspect of positive and negative psychological outcomes that were used to reflect risk and protective factors of resilience.
4. DISCUSSION
The aims of this integrative review were to review and synthesize the literature on resilience in spousal caregivers of patients with cancer. In this review, resilience had direct and indirect effects on the QOL and caregiver burden and it was positively related to the post‐traumatic growth in the face of exposure to multiple traumatic events (Hwang et al., 2018; Karatzias et al., 2017). Spousal caregivers typically shoulder the responsibility such as activities of daily living, medication administration, physical care, emotional support and household management (Hlubocky, 2019; Vatter et al., 2018). Future comprehensive interventions in resilience that target the spouse of patients with cancer are required to increase spouse's emotional well‐being, reduce psychological distress, ameliorate the couple's communication and relationship, and make the partner a better caregiver (Kleine et al., 2019). Therefore, using resilience as an important psychological resource can improve both the cancer survivor and caregiver well‐being. The findings of this review help pave the way to identify resilience and the multiple factors related to resilience that could be used to improve nursing profession's understanding of resilience and create effective comprehensive strategies of health prevention and promotion for informal caregivers.
According to resilience concept mapping (Garcia‐Dia et al., 2013), the definition of resilience involves a combination of inner strengths and outer resources and there is not a universal formula for becoming more resilient. As described above, there was a great variation in their conceptualization of assessing resilience. A total of five scales were used in the included review articles to measure resilience. The scales represented differed on the nature of the resilience that was evaluated, the time frame specified, the level of symptoms and the interpretation of the final score. For example, the CD‐RISC measurement looked at changes over time and resilience refers to the capacity of an individual to cope with stress, overcome adversity or adapt positively to change (Connor, 2003). Nevertheless, other scales looked at other general resilience results and personality traits. For instance, the Wagnild Resilience Scale focuses on individual psychological characteristics while dealing with adversity. Furthermore, an examination of resilience within the different conceptual contexts would provide greater insight into how resilience manifests for spousal caregivers of patients with cancer. For instance, using resilience‐related protective or risk outcome factors for an assessment is also a crucial way to reflect resilience. Here, resilience is not regarded as a quality or ability that is either present or absent in a person but rather a process that may vary across circumstances and time. As a result, some of the concepts overlap and no single concept is necessary or sufficient for explaining resilience. Considering culture issues, using targeted instruments or relevant variables to assess resilience are both suitable for predictive factor investigations, but they may be better suited to evaluate multiple psychological outcomes, such as resilience improvement in psychological intervention design studies.
The findings indicated resilience was related to multiple positive and negative factors. Different approaches have led to inconsistencies in the risk factors and protective processes involved with resilience (Engeli et al., 2016; Luo et al., 2019; Opsomer et al., 2019; Palacio & Limonero, 2019). Some researchers looked at outcomes as the indirect evidence of resilience (Bookwala, 2014; Gibbons et al., 2019), and some used successful coping processes as an indicator of resilience performance (Elliott et al., 2015; Lim et al., 2014). Within psychology, resilience, like inner strengthen, mindfulness and self‐efficacy, is referred to as a protective factor as they are thought to protect individuals from adversity or trauma. Hence, many researchers believe that enhancing a person's level of resilience may be an effective way to prevent health problems and improve well‐being (Walsh et al., 2018). Moreover, recent studies have proposed using the ecological system theory to evaluate resilience (Piel et al., 2017; Teahan et al., 2018). This socioecological framework provides multilevel insight by examining the microsystem, mesosystem, exosystem and macrosystem (Bronfenbrenner, 1979). As evidenced by the findings of this review, a substantial body of literature exists highlighting resilience and adversity in relation to multiple‐level factors, such as individual inner, community environment, national policies and the role of ideologies. This nested factor structure has a multilevel impact on supporting family caregivers. Further research should use hierarchical linear model to analyse resilience rather than a multiple regression or logistic regression in signal cross‐sectional levels.
5. LIMITATION
The limitation of this review was that conclusions from the current review were drawn from factors associated with resilience and not predictive factors of resilience. Second, external validity was a key issue for all included studies. Recruited target populations from locations such as existing support groups, communities or hospitals may represent a specific type of informal caregivers, such as those who are more likely to seek help. Moreover, the quality assessment criteria provided only a rough estimation of the studies' quality.
6. CONCLUSIONS
The current findings add to our understanding of resilience as a distinct trajectory of adjustment and provide further knowledge on resilience associated factors. Caring for patients with cancer can be a form of stress and impact health and well‐being of spousal caregivers. Resilience did play an important role in promoting positive adaptation in spite of adversity among caregivers of patients with cancer. However, there was still little strong evidence regarding ways to measure resilience and the role of related factors on resilience among spouses of patients, particularly within a couple interaction context. In addition, resilience was measured using resilience scales or relevant psychological variables in the literature and there was a lack of measurement by molecular level objective laboratory indicators. As such, future work focusing on resilience would benefit by integrating psychological assessment with other interdisciplinary methods. This review used a developmental lens to consolidate recent empirical studies on resilience among spousal caregivers caring for their loved ones. Despite ongoing debates on how best to define and assess resilience, key themes and central factors that emerged from this review can offer directions for future nursing research. With the uniqueness of resilience‐related studies among spousal caregivers of people with cancer, ways to assess resilience and identify its associated factors deserve more attention. These would help pave the way for the development of educational and psychological support for spouses of patients with cancer.
CONFLICT OF INTEREST
All authors of this study declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Supporting information
Table S1
Tables S2 and S3
Haiyan S, Yang Q, Hengudomsub P. Factors associated with resilience in spousal caregivers of patients with cancer: An integrative review. Nurs Open. 2021;8:2131–2141. 10.1002/nop2.771
Funding information
This work was supported by following funding for the research: Nursing Program of Health Commission Foundation of Jiangsu Province of China (grant number: N2017004); Jiangsu Health Vocational Colleges Culture Research in China (grant number: JCK202001).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the supplementary material of this article. Meanwhile, the data that support the findings of this study are also available from the first author upon reasonable request.
REFERENCES
- Bartone, P. T., Ursano, R. J., Wright, K. M., & Ingraham, L. H. (1989). The impact of a military air disaster on the health of assistance workers. Journal of Nervous and Mental Disease, 177(6), 317–328. 10.1097/00005053-198906000-00001 [DOI] [PubMed] [Google Scholar]
- Bookwala, J. (2014). Spouse health status, depressed affect and resilience in mid and late life: A longitudinal study. Developmental Psychology, 50(4), 1241–1249. 10.1037/a0035124 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1979). The ecology of human development. Harvard University Press. [Google Scholar]
- Campbell‐Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the connor–davidson resilience scale (cd‐risc): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Cassidy, T. (2013). Benefit finding through caring: The cancer caregiver experience. Psychology and Health, 28(3), 250–266. 10.1080/08870446.2012.717623 [DOI] [PubMed] [Google Scholar]
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Elliott, K.‐E.‐ J., Scott, J. L., Monsour, M., & Nuwayhid, F. (2015). Profiles of dyadic adjustment for advanced prostate cancer to inform couple‐based intervention. Psychology and Health, 30(11), 1259–1273. 10.1080/08870446.2015.1043301 [DOI] [PubMed] [Google Scholar]
- Engeli, L., Moergeli, H., Binder, M., Drabe, N., Meier, C., Buechi, S., Dummer, R., & Jenewein, J. (2016). Resilience in patients and spouses faced with malignant melanoma. A qualitative longitudinal study. European Journal of Cancer Care, 25(1), 122–131. 10.1111/ecc.12220 [DOI] [PubMed] [Google Scholar]
- Ferlay, J., Colombet, M., Soerjomataram, I., Mathers, C., Parkin, D. M., Piñeros, M. et al (2019). Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer, 144(8), 1941–1953. 10.1002/ijc.31937 [DOI] [PubMed] [Google Scholar]
- Fung, S.‐F. (2020). Validity of the brief resilience scale and brief resilient coping scale in a Chinese sample. International Journal of Environmental Research and Public Health, 17(4), 1265. 10.3390/ijerph17041265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia‐Dia, M. J., DiNapoli, J. M., Garcia‐Ona, L., Jakubowski, R., & O'Flaherty, D. (2013). Concept analysis: Resilience. Archives of Psychiatric Nursing, 27(6), 264–270. 10.1016/j.apnu.2013.07.003 [DOI] [PubMed] [Google Scholar]
- Gibbons, S. W., Ross, A., Wehrlen, L., Klagholz, S., & Bevans, M. (2019). Enhancing the cancer caregiving experience: Building resilience through role adjustment and mutuality. European Journal of Oncology Nursing, 43, 101663. 10.1016/j.ejon.2019.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeff, A., & Thiel, C. (2012). Resilience in families of husbands with prostate cancer. Educational Gerontology, 38(3), 179–189. 10.1080/03601277.2010.532068 [DOI] [Google Scholar]
- Hlubocky, F. J., Sher, T., Cella, D., Ratain, M. J., & Daugherty, C. (2019). Till death do us part: Existential loneliness (EL), psychosocial distress and survival of advanced cancer patients (ACPs) and their spousal caregivers (SCs). Journal of Clinical Oncology, 37, 11628. 10.1200/JCO.2019.37.15_suppl.11628 [DOI] [Google Scholar]
- Hwang, I. C., Kim, Y. S., Lee, Y. J., Choi, Y. S., Hwang, S. W., Kim, H. M., & Koh, S.‐J. (2018). Factors associated with caregivers' resilience in a terminal cancer care setting. The American Journal of Hospice and Palliative Care, 35(4), 677–683. 10.1177/1049909117741110 [DOI] [PubMed] [Google Scholar]
- Jia, M., Li, J., Chen, C., & Cao, F. (2015). Post‐traumatic stress disorder symptoms in family caregivers of adult patients with acute leukemia from a dyadic perspective. Psycho‐oncology, 24(12), 1754–1760. 10.1002/pon.3851 [DOI] [PubMed] [Google Scholar]
- Joanna Briggs Institute . (2014). Joanna Briggs Institute reviewers’ manual: 2014 edition. Australia: The Joanna Briggs Institute. [Google Scholar]
- Joling, K. J., Windle, G., Droes, R. M., Meiland, F., van Hout, H. P., MacNeil Vroomen, J., & Woods, B. (2016). Factors of resilience in informal caregivers of people with dementia from integrative international data analysis. Dementia and Geriatric Cognitive Disorders, 42(3–4), 198–214. 10.1159/000449131 [DOI] [PubMed] [Google Scholar]
- Jones, S. B., Whitford, H. S., & Bond, M. J. (2015). Burden on informal caregivers of elderly cancer survivors: Risk versus resilience. Journal of Psychosocial Oncology, 33(2), 178–198. 10.1080/07347332.2014.1002657 [DOI] [PubMed] [Google Scholar]
- Jorgensen, I. E., & Seedat, S. (2008). Factor structure of the Connor‐Davidson Resilience Scale in South African adolescents. International Journal of Adolescent Medicine and Health, 20(1), 23–32. 10.1515/IJAMH.2008.20.1.23 [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Jowett, S., Yan, E., Raeside, R., & Howard, R. (2017). Depression and resilience mediate the relationship between traumatic life events and ill physical health: Results from a population study. Psychology, Health and Medicine, 22(9), 1021–1031. 10.1080/13548506.2016.1257814 [DOI] [PubMed] [Google Scholar]
- Kim, Y., Carver, C. S., Shaffer, K. M., Gansler, T., & Cannady, R. S. (2015). Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer, 121(2), 302–310. 10.1002/cncr.29040 [DOI] [PubMed] [Google Scholar]
- Kleine, A. K., Hallensleben, N., Mehnert, A., Honig, K., & Ernst, J. (2019). Psychological interventions targeting partners of cancer patients: A systematic review. Critical Reviews in Oncology/Hematology, 140, 52–66. 10.1016/j.critrevonc.2019.05.008 [DOI] [PubMed] [Google Scholar]
- Kmet, L. M., Cook, L. S., & Lee, R. C. (2004). Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research. [Google Scholar]
- Li, Q., Mak, Y., & Loke, A. (2013). Spouses' experience of caregiving for cancer patients: A literature review. International Nursing Review, 60(2), 178–187. 10.1111/inr.12000 [DOI] [PubMed] [Google Scholar]
- Li, Y., Qiao, Y., Luan, X., Li, S., & Wang, K. (2019). Family resilience and psychological well‐being among Chinese breast cancer survivors and their caregivers. European Journal of Cancer Care, 28(2), e12984. 10.1111/ecc.12984 [DOI] [PubMed] [Google Scholar]
- Li, Y., Wang, K., Yin, Y., Li, Y., & Li, S. (2018). Relationships between family resilience, breast cancer survivors' individual resilience and caregiver burden: A cross‐sectional study. International Journal of Nursing Studies, 88, 79–84. 10.1016/j.ijnurstu.2018.08.011 [DOI] [PubMed] [Google Scholar]
- Li, Y., Zhao, Y., Zhang, J., Lou, F., & Cao, F. (2016). Psychometric properties of the shortened Chinese version of the Family Resilience Assessment Scale. Journal of Child and Family Studies, 25(9), 2710–2717. 10.1007/s10826-016-0432-7 [DOI] [Google Scholar]
- Lillie, H. M., Venetis, M. K., & Chernichky‐Karcher, S. M. (2018). “He would never let me just give up”: Communicatively constructing dyadic resilience in the experience of breast cancer. Health Communication, 33(12), 1516–1524. 10.1080/10410236.2017.1372049 [DOI] [PubMed] [Google Scholar]
- Lim, J. W., Shon, E. J., Paek, M., & Daly, B. (2014). The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Supportive Care in Cancer, 22(12), 3209–3217. 10.1007/s00520-014-2334-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y., Li, Y., Chen, L., Li, Y., Qi, W., & Yu, L. (2018). Relationships between family resilience and posttraumatic growth in breast cancer survivors and caregiver burden. Psycho‐oncology, 27(4), 1284–1290. 10.1002/pon.4668 [DOI] [PubMed] [Google Scholar]
- López‐Pina, J.‐A., Meseguer‐Henarejos, A.‐B., Gascón‐Cánovas, J.‐J., Navarro‐Villalba, D.‐J., Sinclair, V. G., & Wallston, K. A. (2016). Measurement properties of the brief resilient coping scale in patients with systemic lupus erythematosus using rasch analysis. Health and Quality of Life Outcomes, 14(1), 128. 10.1186/s12955-016-0534-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, R. Z., Zhang, S., & Liu, Y. H. (2019). Short report: Relationships among resilience, social support, coping style and posttraumatic growth in hematopoietic stem cell transplantation caregivers. Psychology, Health and Medicine, 25(4), 389–395. 10.1080/13548506.2019.1659985 [DOI] [PubMed] [Google Scholar]
- Lutfi, N. M., & Al Lami, F. (2019). Prevalence and determinants of depression among caregivers of children with leukaemia in Iraq. Eastern Mediterranean Health Journal, 25(6), 374–384. 10.26719/emhj.19.005 [DOI] [PubMed] [Google Scholar]
- Maneewat, T., Lertmaharit, S., & Tangwongchai, S. (2016). Development of caregiver resilience scale (CRS) for Thai caregivers of older persons with dementia. Cogent Medicine, 3(1), 1257409. 10.1080/2331205X.2016.1257409 [DOI] [Google Scholar]
- McDonald, J., Swami, N., Pope, A., Hales, S., Nissim, R., Rodin, G., & Zimmermann, C. (2018). Caregiver quality of life in advanced cancer: Qualitative results from a trial of early palliative care. Palliative Medicine, 32(1), 69–78. 10.1177/0269216317739806 [DOI] [PubMed] [Google Scholar]
- Mulud, Z. A., & McCarthy, G. (2017). Caregiver burden among caregivers of individuals with severe mental illness: Testing the moderation and mediation models of resilience. Archives of Psychiatric Nursing, 31(1), 24–30. 10.1016/j.apnu.2016.07.019 [DOI] [PubMed] [Google Scholar]
- Nishi, D., Uehara, R., Yoshikawa, E., Sato, G., Ito, M., & Matsuoka, Y. (2013). Culturally sensitive and universal measure of resilience for J apanese populations: T achikawa R esilience S cale in comparison with R esilience S cale 14‐item version. Psychiatry and Clinical Neurosciences, 67(3), 174–181. 10.1111/pcn.12028 [DOI] [PubMed] [Google Scholar]
- Northouse, L. L., & McCorkle, R. (2010). Spouse caregivers of cancer patients. In Holland J. C., Breitbart W. S., Jacobsen P. B., Lederberg M. S., Loscalzo M. J., & McCorkle R. (Eds.), Psycho‐Oncology (pp. 516–521). Oxford University Press. [Google Scholar]
- Notario‐Pacheco, B., Solera‐Martínez, M., Serrano‐Parra, M. D., Bartolomé‐Gutiérrez, R., García‐Campayo, J., & Martínez‐Vizcaíno, V. (2011). Reliability and validity of the Spanish version of the 10‐item Connor‐Davidson Resilience Scale (10‐item CD‐RISC) in young adults. Health and Quality of Life Outcomes, 9(1), 63. 10.1186/1477-7525-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opsomer, S., Pype, P., Lauwerier, E., & De Lepeleire, J. (2019). Resilience in middle‐aged partners of patients diagnosed with incurable cancer: A thematic analysis. PLoS One, 14(8), e0221096. 10.1371/journal.pone.0221096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Rourke, N., Kupferschmidt, A. L., Claxton, A., Smith, J. Z., Chappell, N., & Beattie, B. L. (2010). Psychological resilience predicts depressive symptoms among spouses of persons with Alzheimer disease over time. Aging and Mental Health, 14(8), 984–993. 10.1080/13607863.2010.501063 [DOI] [PubMed] [Google Scholar]
- Palacio, C., Krikorian, A., & Limonero, J. T. (2018). The influence of psychological factors on the burden of caregivers of patients with advanced cancer: Resiliency and caregiver burden. Palliative and Supportive Care, 16(3), 269–277. 10.1017/S1478951517000268 [DOI] [PubMed] [Google Scholar]
- Palacio, C., & Limonero, J. T. (2019). The relationship between the positive aspects of caring and the personal growth of caregivers of patients with advanced oncological illness: Postraumattic growth and caregiver. Supportive Care in Cancer, 28(7), 3007–3013. 10.1007/s00520-019-05139-8 [DOI] [PubMed] [Google Scholar]
- Piel, M. H., Geiger, J. M., Julien‐Chinn, F. J., & Lietz, C. A. (2017). An ecological systems approach to understanding social support in foster family resilience. Child and Family Social Work, 22(2), 1034–1043. 10.1111/cfs.12323 [DOI] [Google Scholar]
- Roen, I., Stifoss‐Hanssen, H., Grande, G., Brenne, A. T., Kaasa, S., Sand, K., & Knudsen, A. K. (2018). Resilience for family carers of advanced cancer patients‐how can health care providers contribute? A qualitative interview study with carers. Palliative Medicine, 32(8), 1410–1418. 10.1177/0269216318777656 [DOI] [PubMed] [Google Scholar]
- Saria, M. G., Courchesne, N., Evangelista, L., Carter, J., MacManus, D. A., Gorman, M. K., & Maliski, S. (2017). Cognitive dysfunction in patients with brain metastases: Influences on caregiver resilience and coping. Supportive Care in Cancer, 25(4), 1247–1256. 10.1007/s00520-016-3517-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senneseth, M., Hauken, M. A., Matthiesen, S. B., Gjestad, R., & Laberg, J. C. (2017). Facing spousal cancer during child‐rearing years: Do social support and hardiness moderate the impact of psychological distress on quality of life? Cancer Nursing, 40(3), E24–E34. 10.1097/NCC.0000000000000379 [DOI] [PubMed] [Google Scholar]
- Shaffer, S. M., Dunagin, M. C., Torborg, S. R., Torre, E. A., Emert, B., Krepler, C., & Xiao, M. (2017). Rare cell variability and drug‐induced reprogramming as a mode of cancer drug resistance. Nature, 546(7658), 431. 10.1038/nature22794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson, G. K., Dall'Armi, L., Roydhouse, J. K., Forstner, D., Daher, M., Simpson, T., & White, K. J. (2015). Does resilience mediate carer distress after head and neck cancer? Cancer Nursing, 38(6), E30–E36. 10.1097/NCC.0000000000000229 [DOI] [PubMed] [Google Scholar]
- Sinclair, V. G., & Wallston, K. A. (2004). The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment, 11(1), 94–101. 10.1177/1073191103258144 [DOI] [PubMed] [Google Scholar]
- Sixbey, M. T. (2005). Development of the family resilience assessment scale to identify family resilience constructs. University of Florida. [Google Scholar]
- Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Street, A. F., Couper, J. W., Love, A. W., Bloch, S., Kissane, D. W., & Street, B. C. (2010). Psychosocial adaptation in female partners of men with prostate cancer. European Journal of Cancer Care, 19(2), 234–242. 10.1111/j.1365-2354.2008.01012.x [DOI] [PubMed] [Google Scholar]
- Tang, S. T., Huang, G. H., Wei, Y. C., Chang, W. C., Chen, J. S., & Chou, W. C. (2013). Trajectories of caregiver depressive symptoms while providing end‐of‐life care. Psycho‐Oncology, 22(12), 2702–2710. 10.1002/pon.3334 [DOI] [PubMed] [Google Scholar]
- Teahan, Á., Lafferty, A., Mcauliffe, E., Phelan, A., O'Sullivan, L., O'Shea, D., & Fealy, G. (2018). Resilience in family caregiving for people with dementia: A systematic review. International Journal of Geriatric Psychiatry, 33(12), 1582–1595. 10.1002/gps.4972 [DOI] [PubMed] [Google Scholar]
- Vatter, S., McDonald, K. R., Stanmore, E., Clare, L., McCormick, S. A., & Leroi, I. (2018). A qualitative study of female caregiving spouses' experiences of intimate relationships as cognition declines in Parkinson's disease. Age and Ageing, 47(4), 604–610. 10.1093/ageing/afy049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagnild, G. (2009). A review of the Resilience Scale. Journal of Nursing Measurement, 17(2), 105–113. 10.1891/1061-3749.17.2.105 [DOI] [PubMed] [Google Scholar]
- Wagnild, G. M., & Young, H. (1993). Development and psychometric. Journal of Nursing Measurement, 1(2), 165–17847. [PubMed] [Google Scholar]
- Walsh, D. M. J., Morrison, T. G., Conway, R. J., Rogers, E., Sullivan, F. J., & Groarke, A. (2018). A model to predict psychological and health‐related adjustment in men with prostate cancer: The Role of Post Traumatic Growth, Physical Post Traumatic Growth. Resilience and Mindfulness. Frontiers in Psychology, 9, 136. 10.3389/fpsyg.2018.00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks, S. E., Little, K. G., Gough, H. R., & Spurlock, W. J. (2011). Alzheimer's aggression: Influences on caregiver coping and resilience. Journal of Gerontological Social Work, 54(3), 260–275. 10.1080/01634372.2010.544531 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2020). WHO report on cancer: Setting priorities, investing wisely and providing care for all.
- Yang, H. K., Shin, D. W., Kim, S. Y., Cho, J., Chun, S. H., Son, K. Y., & Park, J. H. (2013). Validity and reliability of the Korean version of the Caregiver Reaction Assessment Scale in family caregivers of cancer patients. Psycho‐oncology, 22(12), 2864–2868. 10.1002/pon.3364 [DOI] [PubMed] [Google Scholar]
- Yoon, S., Howell, K., Pei, F., Shockley McCarthy, K., Dillard, R., & Napier, T. (2019). Resilience following child maltreatment: Definitional considerations and developmental variations. Trauma Violence and Abuse, 12, 1524838019869094. 10.1177/1524838019869094 [DOI] [PubMed] [Google Scholar]
- Yu, X., & Zhang, J. (2007). Factor analysis and psychometric evaluation of the Connor‐Davidson Resilience Scale (CD‐RISC) with Chinese people. Social Behavior and Personality: An International Journal, 35(1), 19–30. 10.2224/sbp.2007.35.1.19 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Tables S2 and S3
Data Availability Statement
The data that support the findings of this study are available in the supplementary material of this article. Meanwhile, the data that support the findings of this study are also available from the first author upon reasonable request.


