Abstract
Objective
To systematically review the effectiveness of four types of traditional Chinese exercise (TCE) on patients with cognitive impairment (CI) and to rank these four TCE types.
Design
A Bayesian network meta‐analysis.
Methods
Four English databases, including PubMed, EMBASE, Cochrane Library and Web of Science, and three Chinese databases, including CNKI, VIP and Wanfang, were searched from their inception to December 2019. Randomized control trials conducted to verify the effects of TCE on patients with CI were included. We used network meta‐analysis to evaluate the relative effects and rank probabilities of the four types of TCE.
Results
The results of the network meta‐analysis indicated that baduanjin (N = 9), tai chi (N = 11), liuzijue (N = 2) and qigong (N = 1) all had significant benefits compared with control conditions. According to the ranking probabilities, baduanjin was most likely to be associated with substantial improvement in cognition, followed by tai chi, liuzijue and qigong.
Conclusion
Our study revealed the effectiveness of TCE for improving global cognition in adults with cognitive impairment. Baduanjin may be the most effective exercise type. The evidence summarized in our study still contains bias, and more research should be carried out to verify the validity of TCE.
Keywords: cognition function, cognitive impairment, network meta‐analysis, nursing, traditional Chinese exercise
1. INTRODUCTION
With the rapid ageing of the world population, the prevalence of cognitive impairment (CI) is dramatically increasing (Jia, 2016). Due to its high incidence and heavy burden on health care, CI has attracted increasing attention in the field of geriatric care (Andrén & Elmståhl, 2007). As a progressive stage of CI, dementia is characterized by multiple cognitive and behavioural disorders, it affects 50 million people around the world, and this number will roughly triple by 2050 (Ballard et al., 2011; WHO, 2017). Mild cognitive impairment (MCI) was defined by Petersen in the 1980s. As a transitional stage between age‐matched normal cognition and dementia, MCI is associated with a high risk of progressing to dementia (Song et al., 2018; Tschanz et al., 2006). Because the relevant symptoms are easily overlooked, MCI may affect many more people than has been reported (Petersen & Morris, 2005). Some studies have found that more than 60% of elderly individuals with MCI progress to dementia in the next 5–10 years (Hebert et al., 2003). CI severely affects functioning and quality of life, increases economic and psychological burden and increases stress in caregivers and families. Therefore, preventing the progression of cognitive decline and living well with CI is a priority for older people and the general healthcare system (Britain, 2009). The fundamental way to enable people with dementia and MCI to live with it is to slow and reverse the progression of CI.
2. BACKGROUND
We hope that the efforts we made can delay or reverse the progress of cognitive decline by applying various pharmacological and non‐pharmacological interventions. Evidence from systematic reviews does not support the utilization of pharmacological treatments for cognitive protection in patients with MCI due to their adverse effects, which has increased the attention being paid to non‐pharmacological interventions (Fink et al., 2018). Physical activity has been shown to improve cognitive function and delay the onset of cognitive impairment (Gheysen et al., 2018). Traditional Chinese exercise (TCE), as a type of exercise, is characterized by its low intensity, high level of safety, and ease of learning and by the fact that no special equipment is required, and it has shown its advantage in recent years. Recent randomized controlled trials (RCTs) and reviews have explored the effects of various types of TCE, such as tai chi (Chang et al., 2011), baduanjin (Zhu et al., 2015), qigong (Cai & Zhang, 2018) and liuzijue (Zheng et al., 2013). One systematic review in 2019 (Zhang et al., 2019) included five RCTs that shared the same usual care control groups without head‐to‐head comparisons of different TCE types. Due to the lack of pairwise randomized controlled trials (RCTs) and the lack of common control groups, we cannot compare alterations and rank the probabilities of these TCEs producing these changes in cognitive function in patients with CI based on the traditional pairwise meta‐analysis method. At the same time, some contradictory findings remain among studies. One review (Zhang et al., 2018) also reported that tai chi was beneficial for ameliorating cognitive function in older people. However, for those with CI, a subgroup analysis in a review in 2018 (Wang et al., 2018) showed that tai chi was not an effective method. As mentioned above, inconsistent results should be clarified to draw more solid conclusions.
Overall, this study provides practical recommendations for healthcare professionals and offers more options for patients with CI. This systematic review and Bayesian network meta‐analysis were performed to collect all of the direct and indirect evidence (Hoaglin et al., 2011) and to compare and rank the efficacy of different types of TCE in improving cognitive function in patients with CI.
3. METHOD
3.1. Aims
A Bayesian network analysis was used to compare and rank the efficacy of four TCE types on cognitive function in elderly individuals diagnosed with CI and to provide appropriate recommendations and possible directions for future clinical practice and research.
3.2. Design
The review was conducted according to the guidelines of the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) guidelines (Hutton et al., 2015).
3.3. Inclusion criteria
(a) Population: Participants were over 55 years old and diagnosed with CI, MCI or dementia. Cognition function was evaluated by using Mini‐Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) scales. (b) Intervention: TCE, including but not limited to tai chi, qigong, baduanjin and liuzijue. (c) Control: the intervention was compared to usual care or a different type of TCE. (d) Outcomes: cognitive function. (e) Study design: RCTs.
3.4. Search strategy
Four English databases, including PubMed, Cochrane Library, EMBASE and Web of Science, and three Chinese databases, including the China National Knowledge Infrastructure (CNKI), Weipu (VIP) and Wanfang Data, were searched from their inception to 01 December 2019. A search was also performed on search engines, including Google Scholar. The following keywords were chosen to screen studies: cognitive impairment, mild cognitive impairment, dementia, baduanjin, tai chi, qigong, liuzijue and cognition. The PubMed search strategy is presented in Appendix S1. We also reviewed the references of the included studies and reviews related to this field to avoid omission.
3.5. Quality assessment
The methodological quality of the included studies was appraised by using The Cochrane Collaboration “risk of bias” tool version 5.1.0. Six domains of bias were used to fully evaluate the quality of the included studies, including selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias. The quality was rated by two reviewers as low, moderate or high. All included studies were independently assessed, and scores were obtained through final consensus. Data abstraction involved two reviewers used a standardized form to abstract the relevant data, including the author, year of publication, control group details (e.g. length of intervention, type of intervention, frequency), country, baseline characteristics of participants, diagnosis, intervention, cognition function outcomes and measurement tools. Any disagreement was resolved by discussion or consultation with a third reviewer.
3.6. Statistical methods
Initial pairwise meta‐analyses were performed with RevMan 5.3 software. The end point of the primary outcome was extracted to evaluate the effectiveness of TCE. For different scales used in the cognitive function assessment, standardized mean differences (SMDs) and 95% confidence intervals (CIs) were computed to obtain pooled effect sizes. The I2 statistic was used to rate heterogeneity as low (<25%), moderate (25%–50%) or high (>50%) (Higgins et al. 2003). A random effects method was chosen if there was high level of heterogeneity in the pooled results; otherwise, a fixed effects method was chosen. Stata 12.0 and d GeMTC 0.14.3 were used to perform the network meta‐analysis. A consistency test was performed by using inconsistency factors and node‐splitting analysis. When the 95% credible intervals (CrIs) for an inconsistency factor contained 0 and the p value of node‐splitting analysis exceeded .05, the consistency model was used if there was no significant inconsistency to calculate the effect size of four TCE types and evaluate the rank probabilities (Higgins et al., 2012). Otherwise, the inconsistency model would be used. At the same time, the potential scale reduction factor (PSRF) was evaluated to manifest the convergence of the model. The closer the PSRF value is to 1, the better the convergence of the model is indicated (Brooks & Gelman, 1998). The range of rank probabilities was from 0%–100%, and probabilities closer to 100% imply better outcomes of the intervention.
4. RESULTS
4.1. Search results
Figure 1 illustrates the selection process. First, 768 potentially eligible articles were retrieved. After excluding 151 duplicate articles, 617 articles entered the next screening process for title and abstract assessment. After assessing the full text of the studies, 27 RCTs satisfying the inclusion criteria for inclusion were finally chosen.
FIGURE 1.
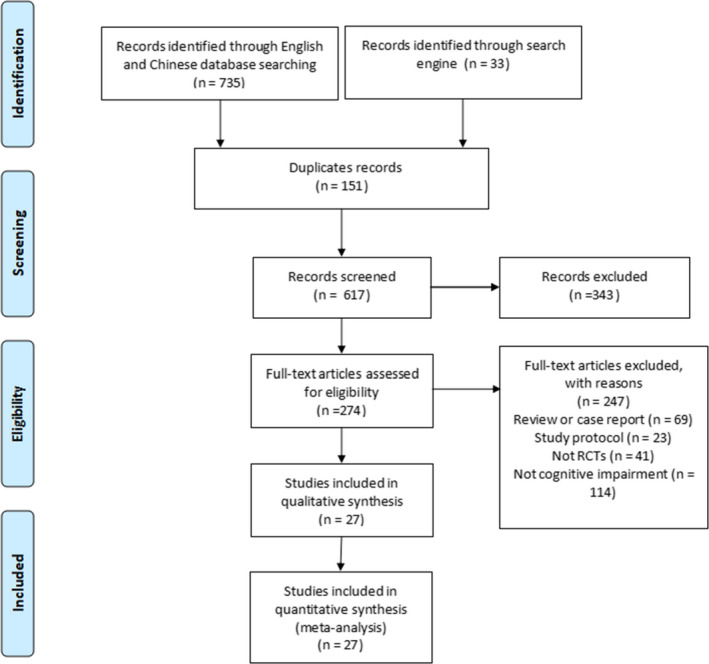
Flow diagram of studies included and excluded at each stage of review
4.2. Study characteristics
Table 1 demonstrates the characteristics of the included studies. The twenty‐seven included RCTs involved 2,414 patients with a clinical diagnosis of CI (1,133 in TCE groups and 1,281 in control groups), with sample sizes ranging from 10–194 (Burgener et al., 2008; Cai & Zhang, 2018; Chan et al., 2016; Chen & Luan, 2017; Cheng et al., 2014; Dechamps et al., 2010; Fogarty et al., 2016; Huang et al., 2019; Lam et al., 2011, 2012; Li, 2016, 2017; Lin, 2016, 2017; Liu et al., 2015, 2018; Siu & Lee, 2018; Sungkarat et al., 2018; Tsai et al., 2013; Wang et al., 2016; Xia, 2017; Xu, 2019; Young, 2018; Young et al., 2019; Zheng et al., 2013; Zhou et al., 2016; Zhu et al., 2015). Overall, 644 individuals participated in tai chi, 386 individuals participated in baduanjin, 75 individuals participated in liuzijue, and 28 individuals participated in qigong.
TABLE 1.
Characteristics of included studies of traditional Chinese exercise for patients with cognitive impairment
| Study | Diagnosis | Allocation, Age M(SD) | Intervention | Intervention length | Control |
Global cognition Outcomes measures |
|
|---|---|---|---|---|---|---|---|
| Baduanjin | Li (2016)/China | MCI |
N = 28 (66.59 ± 4.02) C1 = 29 (65.93 ± 5.13) C2 = 30 (67.35 ± 4.29) |
Baduanjin: 60 min for 3 sessions a week | 6 months |
C1: Health education C2 (Fast‐walk): 60 min for 3 sessions a week |
MoCA |
| Li (2017)/China | MCI |
N = 45 (66.16 ± 4.16) C1 = 45 (65.41 ± 4.09) C2 = 45 (66.08 ± 4.28) |
Baduanjin: 60 min for 3 sessions a week | 6 months |
C1: Health education C2 (Fast‐walk): 60 min for 3 sessions a week |
MoCA | |
| Lin (2016)/China | MCI |
N = 49 (NP) C = 49 (NP) |
Baduanjin: 60 min for 3 sessions a week | 6 months | Health education | MMSE, MoCA | |
| Lin (2017)/China | MCI |
N = 47 (NP) C = 47 (NP) |
Baduanjin: 60 min for 6 sessions a week | 6 months | Health education | MMSE, MoCA | |
| Liu et al. (2015)/China | MCI |
N = 28 (NP) C = 29 (NP) |
Baduanjin: 60 min for 6 sessions a week | 6 months | Usual lifestyle | MoCA | |
| Liu et al. (2018)/China | MCI |
N = 30 (71.60 ± 5.29) C = 30 (71.23 ± 5.53) |
Baduanjin: training (60 min for 6 sessions per week for three weeks) + practice (60 min for 6 sessions a week) | 6 months | Usual lifestyle | MoCA | |
| Xia (2017)/China | MCI |
N = 45 (66.16 ± 4.16) C1 = 45 (65.41 ± 4.09) C2 = 45 (66.08 ± 4.28) |
Baduanjin: 60 min for 3 sessions a week | 6 months |
C1: Health education C2 (Fast‐walk): 60 min for 3 sessions a week |
MoCA | |
| Young (2018)/China | CI |
N = 41 (80.05 ± 6.17) C = 39 (80.25 ± 5.33) |
Baduanjin: 15–20 min at the end of each cognitive stimulation therapy group session | 7 weeks | Interest classes and recreational activities | MMSE | |
| Young (2018)/China | Dementia |
N = 50 (80.53 ± 6.26) C = 51 (79.86 ± 6.59) |
Baduanjin: 15 min at the end of each cognitive stimulation therapy group session | 7 weeks | Usual lifestyle | MMSE | |
| Zhu et al. (2015)/China | MCI |
N = 37 (NP) C = 41 (NP) |
Baduanjin: 40 min for 5 sessions a week | 6 months | Health education | MoCA | |
| Liuzijue | Chen and Luan (2017)/China | MCI |
N = 30 (NP) C = 30 (NP) |
Liuzijue: 90 min for 1 session a week | 3 months | Usual lifestyle | MMSE |
| Zheng et al. (2013)/China | MCI |
N = 45 (65.3 ± 5.34) C = 45 (64.22 ± 5.4) |
Liuzijue: 60 min for 5 sessions a week | 6 months | Routine lifestyle | MMSE, MoCA | |
| Qigong | Cai and Zhang (2018)/China | MCI |
N = 28 (67.53 ± 6.33) C = 30 (66.75 ± 5.27) |
Qigong: 1 week basic training and 90 min for 5 sessions a week | 6 months | Usual lifestyle | MMSE, MoCA |
| Tai chi | Burgener et al. (2008)/America | MCI |
N = 24 (77.9 ± 7.9) C = 19 (76.0 ± 8.1) |
Tai chi: 60 min for 3 sessions a week | 10 months | Usual lifestyle | MMSE |
| Chan et al. (2016)/China | CI |
N = 27 (78.4 ± 7.1) C = 25 (82.2 ± 6.7) |
Tai chi and qigong: basic training and 60 min for 2 sessions a week | 2 months | Health education | MMSE | |
| Cheng et al. (2014)/China | Dementia |
N = 39 (81.8 ± 7.4) C = 35 (80.9 ± 7.2) |
Tai chi: 60 min for 3 sessions a week | 3 months | Usual lifestyle | MMSE | |
| Dechamps et al. (2010)/France | CI |
N = 26 (80.8 ± 8.7) C = 26 (80.6 ± 9.2) |
Tai chi: 30 min for 4 sessions a week | 6 months | Usual care | MMSE | |
| Fogarty et al. (2016)/England | CI |
N = 26 (71.55 ± 9.33) C = 22 (72.61 ± 5.78) |
Tai chi + MIP: twice weekly for 90 min | 2.5 months | MIP |
Memory: HVLT; RBMT Executive function: TMT‐A; TMT‐B |
|
| Huang et al. (2019)/China | Dementia |
N = 36 (81.9 ± 6.0) C = 38 (81.9 ± 6.1) |
Tai chi: 20 min for 2 sessions a week | 10 months | Usual care | MMSE, MoCA | |
| Lam et al. (2011)/China | MCI |
N = 171 (77.2 ± 6.3) C = 218 (78.3 ± 6.6) |
Tai chi: 30 min for 3 sessions a week | 5 months | Stretching and toning exercise | MMSE | |
| Lam et al. (2012)/China | aMCI |
N = 92 (77.2 ± 6.3) C = 169 (78.3 ± 6.6) |
Tai chi: 30 min for 3 sessions a week | 12 months | Muscle‐stretching and toning exercises | MMSE; ADAS‐Cog | |
| Siu and Lee (2018)/China | MCI |
N = 80 (NP) C = 80 (NP) |
Tai chi: programme 60 min for 2 sessions a week | 4 months | Usual care | CMMSE | |
| Sungkarat et al. (2018)/Thailand | MCI |
N = 33 (68.3 ± 6.7) C = 33 (67.5 ± 7.3) |
Tai chi: 9 learning sessions (3 times per week for 3 weeks) and practice sessions (3 times per week for 6 months) | 6 months | Routine lifestyle |
Memory: WMS, visuospatial ability, Executive function: TMT |
|
| Tsai et al. (2013)/America | CI |
N = 28 (78.9 ± 6.9) C = 27 (78.9 ± 8.3) |
Tai chi: 20–40 min for 3 sessions per week | 5 months | Health education | MMSE | |
| Wang et al. (2016)/China | CI |
N = 43 (NP) C = 49 (NP) |
Tai chi: learning sessions (5 times per week for 2 weeks) and practice sessions (4 times per week for 3 months) | 3 months | Routine lifestyle |
Memory: Auditory Verbal Learning Test, AVLT Executive function: TMT |
|
| Xu (2019)/China | MCI |
N = 32 (61.77 ± 6.50) C = 31 (58.15 ± 5.42) |
Baduanjin: 60 min for 3 sessions a week | 3 months | Usual lifestyle | MoCA | |
| Zhou et al. (2016)/China | Dementia |
N = 31 (67.13 ± 4.88) C = 29 (67.50 ± 4.76) |
Tai chi: 60 min for 5 sessions a week | 8 months | Jogging | MMSE |
Abbreviations: C, control group; CI, cognitive impairment; MCI, mild cognitive impairment; MIP, memory intervention programme; MMSE, Mini‐Mental State Examination; MoCA, Montreal Cognitive Assessment; NP, not provided; SD, standard deviation; TCE, traditional Chinese exercise; TMT, Trail Making Test; WMS, Wechsler Memory Scale.
The participants in the included studies were diagnosed with dementia (N = 4), MCI (N = 17) and CI (N = 6). Most of the included studies were implemented in developing countries (22 in China, 1 in Thailand), and the remaining were implemented in developed countries (1 in America, 1 in England, 1 in France). The measures adopted in the control groups were health education (N = 8), usual lifestyle (N = 14) or leisure activities (N = 4). In one study, tai chi was integrated with the control intervention. After discussion, we agreed that the measures in the control groups were regarded as usual lifestyle conditions. The intervention lengths were 7 weeks to 25 months, 1–6 times per week and 30–90 min each time. Two studies (Li, 2017; Xia, 2017) divided participants into three groups (TCE, fast walking and control groups) and compared the effects of TCE and fast walking. However, we did not use the fast walking group for analysis. The scales for the cognitive assessments were the Mini‐Mental State Examination (MMSE), its Chinese version (CMMSE) and the Montreal Cognitive Assessment (MoCA). The methodological quality of each study is presented in Table 2. Overall, all included studies showed a relatively moderate risk of bias. All studies reported randomization, but allocation concealment details were not found in most studies. To some extent, potential selection bias may have influenced the results.
TABLE 2.
Summary of methodological quality assessment of included studies
| Study | Random sequence generation | Allocation concealment | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | Global rating |
|---|---|---|---|---|---|---|---|---|
| Burgener et al. (2008) | Strong | Unclear | Unclear | Strong | Strong | Strong | Unclear | B |
| Cai and Zhang (2018) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Chan et al. (2016) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Chen and Luan (2017) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Low | B |
| Cheng et al. (2014) | Strong | Low | Low | Low | Strong | Strong | Unclear | B |
| Dechamps et al. (2010) | Strong | Low | Low | Low | Strong | Strong | Unclear | B |
| Fogarty et al. (2016) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Huang et al. (2019) | Strong | Unclear | Unclear | Strong | Strong | Strong | Strong | B |
| Lam et al. (2011) | Strong | Unclear | Unclear | Strong | Strong | Strong | Strong | B |
| Lam et al. (2012) | Strong | Unclear | Unclear | Strong | Strong | Strong | Strong | B |
| Li (2016) | Strong | Unclear | Unclear | Strong | Strong | Strong | Unclear | B |
| Li (2017) | Strong | Strong | Low | Strong | Strong | Strong | Strong | B |
| Lin (2016) | Strong | Low | Unclear | Unclear | Strong | Strong | Unclear | B |
| Lin (2017) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Liu et al. (2015) | Strong | Unclear | Low | Unclear | Strong | Strong | Unclear | B |
| Liu et al. (2018) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Siu and Lee (2018) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Strong | B |
| Sungkarat et al. (2018) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Strong | B |
| Tsai et al. (2013) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Wang et al. (2016) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Unclear | B |
| Xia (2017) | Strong | Strong | Low | Strong | Strong | Strong | Strong | B |
| Xu (2019) | Strong | Strong | Unclear | Strong | Strong | Strong | Unclear | B |
| Young (2018) | Strong | Unclear | Unclear | Strong | Strong | Strong | Unclear | B |
| Young (2018) | Strong | Unclear | Unclear | Strong | Strong | Strong | Unclear | B |
| Zheng et al. (2013) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Strong | B |
| Zhou et al. (2016) | Strong | Unclear | Unclear | Unclear | Strong | Strong | Strong | B |
| Zhu et al. (2015) | Strong | Unclear | Low | Unclear | Strong | Strong | Unclear | B |
4.3. Analyses of outcomes
The pairwise comparisons of the four types of TCE are shown in Figure 2. The pooled effect size of the included studies showed that baduanjin [N = 9, I2 = 24%, SMD = 0.96, 95% CI (0.80, 1.12), p < .00001], tai chi [N = 11, I2 = 89%, SMD = 0.66, 95% CI (0.27, 1.04), p < .00001], liuzijue [N = 2, I2 = 0%, 95% CI (0.16, 0.82), p = .003] and qigong [N = 1, I2 not applicable, 95% CI (0.24, 2.36), p = .02] had significant improvements on global cognition as measured by the MMSE or MoCA. The I2 values indicated no heterogeneity in the baduanjin and liuzijue groups and high heterogeneity in the tai chi group but was not applicable in the qigong group.
FIGURE 2.
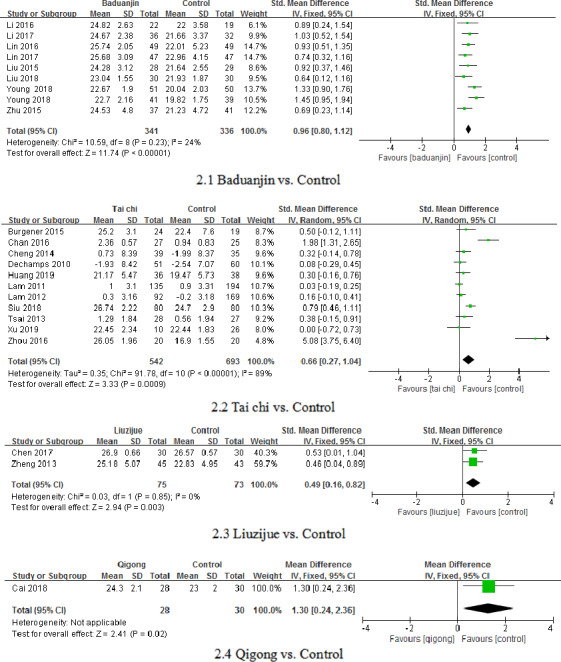
The direct comparisons of different types of TCE and the control
In the network meta‐analysis, 23 two‐arm studies of 27 studies were included. Eleven studies compared tai chi with control conditions, 9 studies compared baduanjin with control conditions, 2 studies compared liuzijue with control conditions, and only 1 study compared qigong with control conditions. As shown in Figure 3, a consistency test was performed by using node‐splitting analysis. The results showed that the 95% CI of the inconsistency factor contained 0, and the PSRF value was 1, indicating that the consistency model could be selected. The relative effects of the four types of TCE are presented in Table 3. The network analysis demonstrated that baduanjin [SMD = 2.73, 95% CI (1.27, 4.23)], tai chi [SMD = 1.94, 95% CI (0.56, 3.34)], liuzijue [SMD = 1.20, 95% CI (−1.94, 4.46)] and qigong [SMD = 0.04, 95% CI (−5.47, 5.48)] all had positive effects on cognitive functions in the participants with CI compared to the controls.
FIGURE 3.
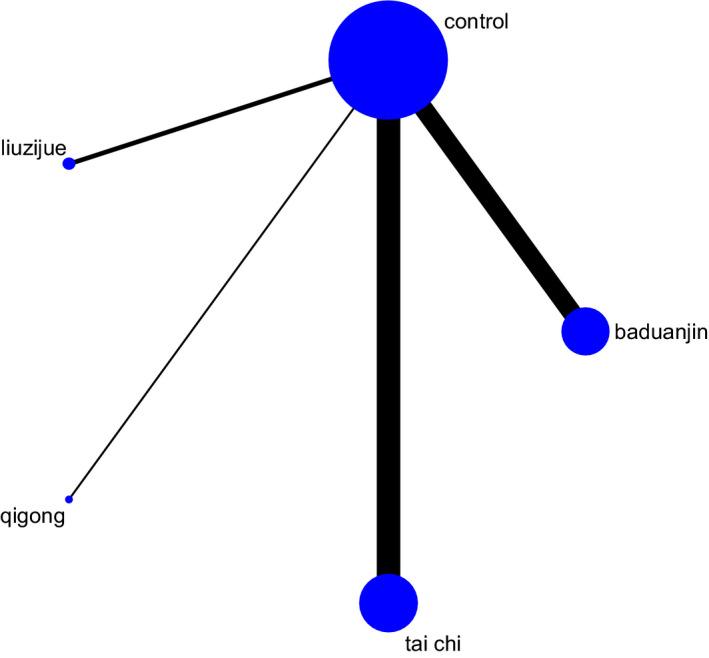
Network map for the comparison of different interventions
TABLE 3.
Relative effects of different interventions
| Baduanjin | −2.73 (−4.23, −1.27) | −1.52 (−5.00, 2.06) | −1.46 (−6.12, 3.21) | −0.79 (−2.82, 1.23) |
|---|---|---|---|---|
| 2.73 (1.27, 4.23) | Control | 1.20 (−1.94, 4.46) | 1.27 (−3.14, 5.70) | 1.94 (0.56, 3.34) |
| 1.52 (−2.06, 5.00) | −1.20 (−4.46, 1.94) | Liuzijue | 0.04 (−5.47, 5.48) | 0.79 (−2.81, 4.16) |
| 1.46 (−3.21, 6.12) | −1.27 (−5.70, 3.14) | −0.04 (−5.48, 5.47) | Qigong | 0.70 (−3.87, 5.30) |
| 0.79 (−1.23, 2.82) | −1.94 (−3.34, −0.56) | ‐ 0.79 (−4.16, 2.81) | −0.70 (−5.30, 3.87) | Tai chi |
The rank probabilities of the four types of TCE are shown in Table 4 and Figure 4. Baduanjin was most likely to rank first (53%), tai chi was most likely to rank second (40%), liuzijue was most likely to rank third (26%), and qigong was most likely to rank fourth (26%). The results indicated that baduanjin produced more positive outcomes than the other three TCE types.
TABLE 4.
Rank probability of the efficacy of different interventions
| Intervention | Rank 1 | Rank 2 | Rank 3 | Rank 4 | Rank 5 |
|---|---|---|---|---|---|
| Baduanjin | 0.53 | 0.32 | 0.12 | 0.02 | 0.00 |
| Control | 0.00 | 0.00 | 0.06 | 0.38 | 0.56 |
| Liuzijue | 0.14 | 0.15 | 0.26 | 0.27 | 0.18 |
| Qigong | 0.22 | 0.13 | 0.20 | 0.20 | 0.26 |
| Tai chi | 0.12 | 0.40 | 0.35 | 0.13 | 0.00 |
FIGURE 4.
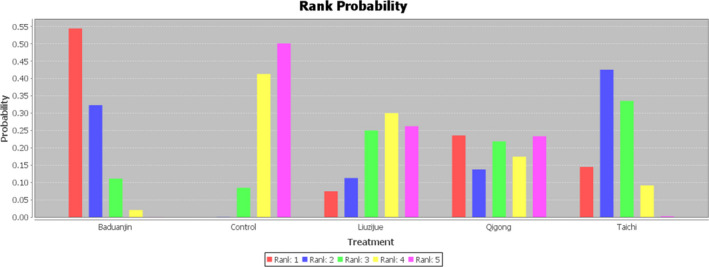
Rank probability of the efficacy of different interventions
4.4. Adverse events
Most of the included studies reported adverse events, but no events related to TCE had occurred. One study (Sungkarat et al., 2018) reported that one participant from each group experienced a fall with a bone fracture during the intervention period. The cause of the fall was not related to the interventions and occurred outside of the exercise space. One study (Li, 2016) reported the number of falls in the past 12 months, and the average for the intervention group was 0.4, while that for the control group was 0.6; there was no difference between the two groups.
5. DISCUSSION
5.1. Main findings and interpretation
Our analysis was based on 27 studies including 2,414 individuals randomly assigned to 4 different TCE, tai chi, baduanjin, qigong and liuzijue. This review showed that significant benefits were found with improved cognitive function in elderly individuals with CI, as measured by MMSE and MoCA scales. Bayesian network analysis including the four types of TCE showed their respective advantages in promoting cognition. According to the analysis of the rank probabilities, baduanjin was the most advantageous in terms of promoting cognitive functions.
Our results showed that baduanjin and tai chi improved cognitive function in various populations, consistent with previous studies (Chang et al., 2011; Tao et al., 2017; Wayne et al., 2014). As types of mind‐body interventions, baduanjin and tai chi decrease the speed of cognitive decline by training slow motions that allow elderly individuals to avoid the consequences and complications of CI. Regarding the opposite conclusions of the two reviews (Wang et al., 2018; Zhang et al., 2019), this may be possibly be due to the sample size, the number of included studies and the types of TCE, which may have partly led to differences in the findings.
We included two studies examining the efficacy of liuzijue and only one examining qigong, and positive outcomes were shown. The study of qigong (Ladawan et al., 2017) that investigated enhanced global cognitive functions in individuals also revealed significant improvements in global cognitive functions following aerobic exercise. However, regarding studies investigating liuzijue, most studies have focused on chronic obstructive pulmonary disease (Wu et al., 2018). In our study, the evidence provides little support for cognitive improvement with liuzijue. Therefore, more RCTs related to qigong and liuzijue should be carried out in older individuals with CI to confirm their efficacy.
Thus, changes in cognitive assessment scores do not equal a clinically relevant change (Cohen Mansfield & Billig, 1986). Two included studies (Li, 2017; Xia, 2017) explored the potential mechanisms for the positive outcomes and revealed that TCE practice significantly increased the functional activity in the bilateral putamen, left hippocampus, left inferior frontal gyrus, etc.; TCE may improve global cognitive function and memory in MCI patients through this potential neurological mechanism. Although positive outcomes were shown in biological parameters and complex neurological functions, the existing evidence does not provide solid proof of the underlying mechanisms. Further research should adopt objective and comprehensive measurement tools to explore the mechanisms of TCE on cognition. In the meantime, healthcare professionals should aim to detect cognitive impairment and adopt suitable measures early.
The results (Bamidis et al., 2015) indicated dose‐dependent training benefits on global cognition, and these benefits varied by intervention durations and intensities. The included studies shared the same TCE theory but used different training forms, training protocols, and exercise frequencies and doses. The length of the intervention in seven of the included studies was less than 6 months, and most studies performed the intervention for 6 months or longer, even as long as 12 months. Future trials should explore reasonable choices from among the training and practice types, doses and durations to maximize the treatment adherence of patients with cognitive impairment.
TCE is composed of simple, brief movements with low physical and cognitive demand and can be self‐learned and practised (An et al., 2008). One meta‐analysis included 180 reviews and suggested that exercise increases the odds of adverse events but not of serious adverse events, such as falls (Niemeijer et al., 2019). Our study also reviewed the rate of adverse events, and no related adverse events were reported during TCE training in the included studies. This evidence suggests that TCE, as a relatively safe intervention, should be widely promoted. To some extent, it is thought that TCE is cost‐effective and can reduce the substantial burden of medical costs and healthcare needs in families and society in the long run. Given these considerations and the increasing availability of TCE in various settings, clinicians may consider recommending TCE to persons with cognitive impairment.
Exergaming is a feasible and relatively safe intervention that offers an environment in which physical and cognitive exercise is combined (Colombo et al., 2012). One study (Hsieh et al., 2018) revealed that VR tai chi had a significant protective effect on cognitive and physical outcomes. The application of VR programmes with tai chi also showed high attendance (Lan et al., 2013). One review showed that hardly any robust scientific research has been conducted on exergaming and dementia (Van Santen et al., 2018), and further studies should adopt TCE with advanced technology to adapt this intervention to home‐based applications in individuals with cognitive impairment. To ameliorate cognitive functions, individuals with CI should be encouraged to practise TCE during daily life, and Baduanjin is recommended as the first choice. Furthermore, as TCE is easy to learn and practise, it might be a useful strategy to decrease caregivers’ burden. Therefore, TCE should be recommended as an integral part of treatment for patients and family caregivers.
6. LIMITATIONS
First, and perhaps most notably, neither the methodological quality of nor the heterogeneity among the studies included in the meta‐analysis was strong enough to draw a solid conclusion. Most studies did not report the allocation details. Although it may have been hard to blind the experimental group, the assessors could have been blinded; to some extent, measurement bias could have been reduced. Most of the included studies were performed in China, which may result in the results suffering from certain degrees of selection bias. To make clearer recommendations, future studies should include larger sample sizes with rigorous study designs and provide more information on the potential mechanisms of the applied TCE.
7. CONCLUSIONS
For patients with CI, our network meta‐analysis suggests that four different types of TCE have potential therapeutic use in improving general cognitive function compared with control conditions. Baduanjin may be the most effective, followed by tai chi, liuzijue and qigong. Multi‐arm RCTs are necessary to confirm the effects of TCE on additional aspects of CI to provide more options for healthcare professionals.
CONFLICT OF INTEREST
The authors state no conflicts of interest.
AUTHOR CONTRIBUTIONS
Chen Li and Dongxiang Zheng searched articles, Chen Li and Jinglan Luo performed the data extraction and analysis, and Chen Li wrote this paper.
ETHICAL APPROVAL
There is no ethical statement for this trial.
STATEMENTS
The authors contributed to this review equally and approved the final version of the manuscript, which has not been previously published.
Supporting information
Appendix S1
Appendix S2
Appendix S3
ACKNOWLEDGMENTS
The authors thank Mingyue Hu from the School of Nursing, Xiangya School of Medicine, for her guidance on the development of this article.
Li C, Zheng D, Luo J. Effects of traditional Chinese exercise on patients with cognitive impairment: A systematic review and Bayesian network meta‐analysis. Nurs Open. 2021;8:2208–2220. 10.1002/nop2.799
Contributor Information
Chen Li, Email: chencare@126.com.
Dongxiang Zheng, Email: zhengdongxiang2018@126.com.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- An, B., Dai, K., Zhu, Z., Wang, Y., Hao, Y., Tang, T., & Yan, H. (2008). Baduanjin alleviates the symptoms of knee osteoarthritis. The Journal of Alternative and Complementary Medicine, 14(2), 167–174. [DOI] [PubMed] [Google Scholar]
- Andrén, S., & Elmståhl, S. (2007). Relationships between income, subjective health and caregiver burden in caregivers of people with dementia in group living care: A cross‐sectional community‐based study. International Journal of Nursing Studies, 44(3), 435–446. 10.1016/j.ijnurstu.2006.08.016 [DOI] [PubMed] [Google Scholar]
- Ballard, C., Gauthier, S., Corbett, A., Brayne, C., Aarsland, D., & Jones, E. (2011). Alzheimer's disease. The Lancet, 377(9770), 1019–1031. 10.1016/S0140-6736(10)61349-9 [DOI] [PubMed] [Google Scholar]
- Bamidis, P. D., Fissler, P., Papageorgiou, S. G., Zilidou, V., Konstantinidis, E. I., Billis, A. S., Romanopoulou, E., Karagianni, M., Beratis, I., Tsapanou, A., Tsilikopoulou, G., Grigoriadou, E., Ladas, A., Kyrillidou, A., Tsolaki, A., Frantzidis, C., Sidiropoulos, E., Siountas, A., Matsi, S., … Kolassa, I.‐T. (2015). Gains in cognition through combined cognitive and physical training: The role of training dosage and severity of neurocognitive disorder. Frontiers in Aging Neuroscience, 7, 152. 10.3389/fnagi.2015.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britain G. Department of Health (2009). Living well with dementia: A national dementia strategy. Retrieved November 23, 2009. [Google Scholar]
- Brooks, S. P., & Gelman, A. (1998). General methods for monitoring convergence of iterative simulations. Journal of Computational and Graphical Statistics, 7(4), 434–455. [Google Scholar]
- Burgener, S. C., Yang, Y., Gilbert, R., & Marsh‐Yant, S. (2008). The effects of a multimodal intervention on outcomes of persons with early‐stage dementia. American Journal of Alzheimer's Disease & Other Dementias®, 23(4), 382–394. 10.1177/1533317508317527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, J., & Zhang, Z. (2018). Effects of continuous qigong exercise on mild cognitive impairment in the elderly. Journal of Baicheng Normal University, 32(06), 65–69. [Google Scholar]
- Chan, A. W. K., Yu, D. S. F., Choi, K. C., Lee, D. T. F., Sit, J. W. H., & Chan, H. Y. L. (2016). Tai chi qigong as a means to improve night‐time sleep quality among older adults with cognitive impairment: A pilot randomized controlled trial. Clinical Interventions in Aging, 11, 1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, J. Y., Tsai, P. F., Beck, C., Hagen, J. L., Huff, D. C., Anand, K. J. S., Roberson, P. K., Rosengren, K. S., & Beuscher, L. (2011). The effect of tai chi on cognition in elders with cognitive impairment. Medsurg Nursing, 20(2), 63. [PMC free article] [PubMed] [Google Scholar]
- Chen, C., & Luan, L. (2017). Clinical study on the effect of fitness qigong six‐character formula on brain wave in patients with mild cognitive dysfunction. Shanghai Journal of Traditional Chinese Medicine, 12, 54–57. [Google Scholar]
- Cheng, S. T., Chow, P. K., Song, Y. Q., Yu, E. C. S., Chan, A. C. M., Lee, T. M. C., & Lam, J. H. M. (2014). Mental and physical activities delay cognitive decline in older persons with dementia. The American Journal of Geriatric Psychiatry, 22(1), 63–74. [DOI] [PubMed] [Google Scholar]
- Cohen Mansfield, J., & Billig, N. (1986). Agitated behaviors in the elderly: I. A conceptual review. Journal of the American Geriatrics Society, 34(10), 711–721. [DOI] [PubMed] [Google Scholar]
- Colombo, M., Marelli, E., Vaccaro, R., Roberta, V. E., Colombaril, S., Garolfi, S., Fossi, S., Guaita, A., & Polesel, E. (2012). Virtual reality for persons with dementia: An exergaming experience. In ISARC. Proceedings of the international symposium on automation and robotics in construction (Vol. 29, pp. 1). IAARC Publications. [Google Scholar]
- Dechamps, A., Diolez, P., Thiaudière, E. et al (2010). Effects of exercise programs to prevent decline in health‐related quality of life in highly deconditioned institutionalized elderly persons: A randomized controlled trial. Archives of Internal Medicine, 170(2), 162–169. 10.1001/archinternmed.2009.489 [DOI] [PubMed] [Google Scholar]
- Fink, H. A., Jutkowitz, E., McCarten, J. R., Hemmy, L. S., Butler, M., Davila, H., Ratner, E., Calvert, C., Barclay, T. R., Brasure, M., Nelson, V. A., & Kane, R. L. (2018). Pharmacologic interventions to prevent cognitive decline, mild cognitive impairment, and clinical Alzheimer‐type dementia: A systematic review. Annals of Internal Medicine, 168(1), 39–51. 10.7326/M17-1529 [DOI] [PubMed] [Google Scholar]
- Fogarty, J. N., Murphy, K. J., McFarlane, B., Montero‐Odasso, M., Wells, J., Troyer, A. K., Trinh, D., Gutmanis, I., & Hansen, K. T. (2016). Taoist Tai Chi® and memory intervention for individuals with mild cognitive impairment. Journal of Aging and Physical Activity, 24(2), 169–180. 10.1123/japa.2014-0062 [DOI] [PubMed] [Google Scholar]
- Gheysen, F., Poppe, L., DeSmet, A., Swinnen, S., Cardon, G., De Bourdeaudhuij, I., Chastin, S., & Fias, W. (2018). Physical activity to improve cognition in older adults: Can physical activity programs enriched with cognitive challenges enhance the effects? A systematic review and meta‐analysis. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 63. 10.1186/s12966-018-0697-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert, L. E., Scherr, P. A., Bienias, J. L., Bennett, D. A., & Evans, D. A. (2003). Alzheimer disease in the US population: Prevalence estimates using the 2000 census. Archives of Neurology, 60(8), 1119–1122. 10.1001/archneur.60.8.1119 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Jackson, D., Barrett, J. K., Lu, G., Ades, A. E., & White, I. R. (2012). Consistency and inconsistency in network meta‐analysis: Concepts and models for multi‐arm studies. Research Synthesis Methods, 3(2), 98–110. 10.1002/jrsm.1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta‐analyses. BMJ, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoaglin, D. C., Hawkins, N., Jansen, J. P., Scott, D. A., Itzler, R., Cappelleri, J. C., Boersma, C., Thompson, D., Larholt, K. M., Diaz, M., & Barrett, A. (2011). Conducting indirect‐treatment‐comparison and network‐meta‐analysis studies: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 2. Value in Health, 14(4), 429–437. 10.1016/j.jval.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Hsieh, C.‐C., Lin, P.‐S., Hsu, W.‐C., Wang, J.‐S., Huang, Y.‐C., Lim, A.‐Y., & Hsu, Y.‐C. (2018). The effectiveness of a virtual reality‐based tai chi exercise on cognitive and physical function in older adults with cognitive impairment. Dementia and Geriatric Cognitive Disorders, 46(5–6), 358–370. 10.1159/000494659 [DOI] [PubMed] [Google Scholar]
- Huang, N., Li, W., Rong, X., Champ, M., Wei, L., Li, M., Mu, H., Hu, Y., Ma, Z., & Lyu, J. (2019). Effects of a modified tai chi program on older people with mild dementia: A randomized controlled trial. Journal of Alzheimer's Disease, 72(3), 947–956. 10.3233/JAD-190487 [DOI] [PubMed] [Google Scholar]
- Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., Ioannidis, J. P. A., Straus, S., Thorlund, K., Jansen, J. P., Mulrow, C., Catalá‐López, F., Gøtzsche, P. C., Dickersin, K., Boutron, I., Altman, D. G., & Moher, D. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta‐analyses of health care interventions: Checklist and explanations. Annals of Internal Medicine, 162(11), 777–784. 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- Jia, J. J. (2016). Screening and diagnosis of cognitive impairment in older adults. Chinese Journal of Cerebral Vascular Disease Heart, 18, 337–338. [Google Scholar]
- Ladawan, S., Klarod, K., Philippe, M., Menz, V., Versen, I., Gatterer, H., & Burtscher, M. (2017). Effect of Qigong exercise on cognitive function, blood pressure and cardiorespiratory fitness in healthy middle‐aged subjects. Complementary Therapies in Medicine, 33, 39–45. 10.1016/j.ctim.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Lam, L. C. W., Chau, R. C. M., Wong, B. M. L., Fung, A. W. T., Lui, V. W. C., Tam, C. C. W., Leung, G. T. Y., Kwok, T. C. Y., Chiu, H. F. K., Ng, S., & Chan, W. M. (2011). Interim follow‐up of a randomized controlled trial comparing Chinese style mind body (Tai Chi) and stretching exercises on cognitive function in subjects at risk of progressive cognitive decline. International Journal of Geriatric Psychiatry, 26(7), 733–740. 10.1002/gps.2602 [DOI] [PubMed] [Google Scholar]
- Lam, L. C. W., Chau, R. C. M., Wong, B. M. L., Fung, A. W. T., Tam, C. W. C., Leung, G. T. Y., Kwok, T. C. Y., Leung, T. Y. S., Ng, S. P., & Chan, W. M. (2012). A 1‐year randomized controlled trial comparing mind body exercise (Tai Chi) with stretching and toning exercise on cognitive function in older Chinese adults at risk of cognitive decline. Journal of the American Medical Directors Association, 13(6), 568.e15–568.e20. 10.1016/j.jamda.2012.03.008 [DOI] [PubMed] [Google Scholar]
- Lan, C., Chen, S. Y., Lai, J. S., & Wong, A. M. (2013). Tai chi chuan in medicine and health promotion. Evidence‐Based Complementary and Alternative Medicine: ECAM, 2013, 502131. 10.1155/2013/502131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, M. (2017). Study of Baduanjin exercise intervention on functional imaging of mild cognitive impairment based on default network. [Google Scholar]
- Li, S. (2016). The effect of Baduanjin exercise on the overall cognitive function and memory of the elderly with mild cognitive impairment. [Google Scholar]
- Lin, Q. (2016). The effect of Baduanjin exercise on cognitive function of patients with mild cognitive impairment. Shandong Medicine, 56(21), 50–51. [Google Scholar]
- Lin, Q. (2017). The effect and improvement of cognitive function of Baduanjin exercise in elderly patients with mild cognitive impairment. Chinese Journal of Gerontology, 14, 3558–3560. [Google Scholar]
- Liu, T., Bai, S., & Huang, Y. (2015). Effects of exercise intervention on cognitive level and cerebrospinal fluid related indicators in patients with mild cognitive impairment. Shaanxi Medical Journal, 10, 1388–1390. [Google Scholar]
- Liu, T., Guo, S., & Bai, S. (2018). Baduanjin on cognitive level of patients with mild cognitive impairment. Chinese Rehabilitation Theory and Practice, 24(7), 854–859. [Google Scholar]
- Niemeijer, A., Lund, H., Stafne, S. N., Ipsen, T., Goldschmidt, C. L., Jørgensen, C. T., & Juhl, C. B. (2019). Adverse events of exercise therapy in randomised controlled trials: A systematic review and meta‐analysis. British Journal of Sports Medicine, 54, 1073–1080. [DOI] [PubMed] [Google Scholar]
- Petersen, R. C., & Morris, J. C. (2005). Mild cognitive impairment as a clinical entity and treatment target. Archives of Neurology, 62(7), 1160–1163. 10.1001/archneur.62.7.1160 [DOI] [PubMed] [Google Scholar]
- Siu, M., & Lee, D. T. F. (2018). Effects of tai chi on cognition and instrumental activities of daily living in community dwelling older people with mild cognitive impairment. BMC Geriatrics, 18(1), 37. 10.1186/s12877-018-0720-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, D., Yu, D. S. F., Li, P. W. C., & Lei, Y. (2018). The effectiveness of physical exercise on cognitive and psychological outcomes in individuals with mild cognitive impairment: A systematic review and meta‐analysis. International Journal of Nursing Studies, 79, 155–164. 10.1016/j.ijnurstu.2018.01.002 [DOI] [PubMed] [Google Scholar]
- Sungkarat, S., Boripuntakul, S., Kumfu, S., Lord, S. R., & Chattipakorn, N. (2018). Tai Chi improves cognition and plasma BDNF in older adults with mild cognitive impairment: A randomized controlled trial. Neurorehabilitation and Neural Repair, 32(2), 142–149. 10.1177/1545968317753682 [DOI] [PubMed] [Google Scholar]
- Tao, J., Chen, X., Egorova, N., Liu, J., Xue, X., Wang, Q., Zheng, G., Li, M., Hong, W., Sun, S., Chen, L., & Kong, J. (2017). Tai Chi Chuan and Baduanjin practice modulates functional connectivity of the cognitive control network in older adults. Scientific Reports, 7, 41581. 10.1038/srep41581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, P.‐F., Chang, J. Y., Beck, C., Kuo, Y.‐F., & Keefe, F. J. (2013). A pilot cluster‐randomized trial of a 20‐week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: Effects on pain and other health outcomes. Journal of Pain and Symptom Management, 45(4), 660–669. 10.1016/j.jpainsymman.2012.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschanz, J. T., Welsh‐Bohmer, K. A., Lyketsos, C. G., Corcoran, C., Green, R. C., Hayden, K., Norton, M. C., Zandi, P. P., Toone, L., West, N. A., & Breitner, J. (2006). Conversion to dementia from mild cognitive disorder: The Cache County Study. Neurology, 67(2), 229–234. 10.1212/01.wnl.0000224748.48011.84 [DOI] [PubMed] [Google Scholar]
- Van Santen, J., Dröes, R. M., Holstege, M. et al (2018). Effects of exergaming in people with dementia: Results of a systematic literature review. Journal of Alzheimer's Disease, 63(2), 741–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Q., Shengyu (2016). The effect of Tai Chi Chuan on memory and executive function of the elderly with mild cognitive impairment. Journal of Shandong Institute of Physical Education, 32(3), 68–72. [Google Scholar]
- Wang, S., Yin, H., Jia, Y., Zhao, L., Wang, L., & Chen, L. I. (2018). Effects of mind‐body exercise on cognitive function in older adults with cognitive impairment: A systematic review and meta‐analysis. The Journal of Nervous and Mental Disease, 206(12), 913–924. 10.1097/NMD.0000000000000912 [DOI] [PubMed] [Google Scholar]
- Wayne, P. M., Walsh, J. N., Taylor‐Piliae, R. E., Wells, R. E., Papp, K. V., Donovan, N. J., & Yeh, G. Y. (2014). Effect of Tai Chi on cognitive performance in older adults: Systematic review and meta‐analysis. Journal of the American Geriatrics Society, 62(1), 25–39. 10.1111/jgs.12611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2017). WHO dementia. WHO. Retrieved from http://www.who.int/mediacentre/factsheets/fs362/en/ [Google Scholar]
- Wu, W., Liu, X., Li, P., Li, N., & Wang, Z. (2018). Effect of Liuzijue exercise combined with elastic band resistance exercise on patients with COPD: A randomized controlled trial. Evidence‐Based Complementary and Alternative Medicine, 2018, 1–12. 10.1155/2018/2361962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia, R. (2017). Baduanjin on the attention of the elderly with mild cognitive impairment. [Google Scholar]
- Xu, Y. (2019). Study of the neurological mechanism of tai chi combined with t DCS on cognitive function in patients with MCI based on multi‐modal MRI. [Google Scholar]
- Young, D. K. W. (2018). Multicomponent intervention combining a cognitive stimulation group and tai chi to reduce cognitive decline among community‐dwelling older adults with probable dementia: A multi‐center, randomized controlled trial. Dementia, 19(6), 2073–2089. 10.1177/1471301218814637 [DOI] [PubMed] [Google Scholar]
- Young, D. K., Ng, P. Y., Kwok, T., Ho, F., Cheng, D., Mak, V., & Lau, A. (2019). The effects of an expanded cognitive stimulation therapy model on the improvement of cognitive ability of elderly with mild stage Dementia living in a community—A randomized waitlist controlled trial. Aging & Mental Health, 23(7), 855–862. [DOI] [PubMed] [Google Scholar]
- Zhang, Q. I., Hu, J., Wei, L., Cao, R. I., Ma, R., Song, H., & Jin, Y. I. (2019). Effects of traditional Chinese exercise on cognitive and psychological outcomes in older adults with mild cognitive impairment: A systematic review and meta‐analysis. Medicine, 98(7), e14581. 10.1097/MD.0000000000014581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y., Li, C., Zou, L., Liu, X., & Song, W. (2018). The effects of mind‐body exercise on cognitive performance in elderly: A systematic review and meta‐analysis. International Journal of Environmental Research and Public Health, 15(12), 2791. 10.3390/ijerph15122791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, X., Yu, J., & Tu, R. (2013). Liuzijue on rehabilitation of mild cognitive impairment. International Journal of Traditional Chinese Medicine, 35(11), 968–972. [Google Scholar]
- Zhou, Y., Zhao, S., & Zhao, M. (2016). The effect of Tai Chi Softball on patients with Alzheimer. Liaoning Sports Science and Technology, 1, 72–74. [Google Scholar]
- Zhu, H., Zhang, N., & Ji, C. (2015). Study on the effect of Baduanjin on mild cognitive impairment in elderly diabetic patients. Chinese Journal of Practical Nursing, 31(16), 1202–1204. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2
Appendix S3
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


