The success of preventive measures of COVID-19 depends on a correct understanding of the transmission routes of the virus. Researchers had identified SARS-CoV-2 in the air sampling of the COVID-19 isolation ward and found that viruses in the aerosol can survive and remain infectious for quite a while. The culprit of multiple infection events in public transportation, apartments, shopping malls, restaurants, choirs, and other places appeared to be airborne transmission. As research showed, the suspension time of aerosol increased tenfold in a poorly ventilated space( SomsenGA et al., 2020/05/312020).1 With more and more academic evidence, World Health Organization (WHO) and the Centers for Disease Control and Prevention (US-CDC) have changed their positions recently, confirming that airborne transmission is an essential route of COVID-19 transmission.2 , 3 To reduce the air concentration of the virus and the viral exposure dose of people indoors, researchers also started to emphasize improving the ventilation and exhaust system as a core preventive suggestion, rather than maintaining safety social distance( BazantMZ, 2021).4
The current guidance reviews and summarizes five guidelines by WHO, Scientific Advisory Group for Emergencies-Environmental Modelling Group (SAGE-EMG) of the British Government, US-CDC, and American Society of Heating, Refrigerating, and Air-Condition Engineers (ASHRAE),5, 6, 7, 8, 9 and other relevant literature as well. We aim to help the readers improve their indoor spaces' ventilation to “flatten the curve” and curb the chain of community transmission. However, the guidance is for reference only in general. We recommend that the readers consult experienced experts in heating, ventilation, and air conditioning (HVAC) systems for specific scenarios and conditions first.
Determine the required ventilation rate of an indoor space based on the activity type
Humans produce aerosol particles during exhalation, but the size and numbers of aerosol produced in different activities vary, and requirements for ventilation are thus different. According to the WHO guideline, the minimum required ventilation rate for ordinary workplaces or public spaces is 10 L/s per person, i.e., 36 m3/h (CMH). This is also applicable to medical departments that are not expected to be exposed to confirmed or suspected COVID-19 cases, such as non-epidemic clinics or outpatient clinics that do not treat respiratory infections. A minimum of 15 L/s per person (i.e., 54 CMH) is required for an indoor space where much aerosol is generated through singing, loud speaking, aerobic exercise, or other activities.5
Example 1.
-
•
If there are eight people in the office, the minimum required ventilation rate is 80 L/s (i.e., 288 CMH).
-
•
If four people are in the karaoke box, the minimum required ventilation rate is 60 L/s (i.e., 216 CMH).
There is a particular association between the indoor ventilation volume and the indoor CO2 concentration in a steady state. Therefore, if no suitable instrument is available to measure the indoor ventilation volume, indoor CO2 concentration can be used as a proxy indicator. According to the SAGE-EMG guideline, we should control the CO2 concentration to 1000 ppm or below for ordinary indoor spaces. For indoor spaces where a large amount of aerosol is generated, we should control the CO2 concentration to 800 ppm or below. If the concentration reaches 1500 ppm or more, it should be listed as a top priority for improvement.6 The US-CDC guideline recommends recording the benchmark indoor CO2 concentration when much outside air is introduced. If the indoor CO2 concentration is found to exceed the benchmark value by 10% or more in the periodic measurement, the problem of the ventilation system should be investigated.7 However, it should be noted that the indoor CO2 concentration is currently unable to predict the infected persons, the number of infectious particles, and whether the HVAC system effectively dilutes or removes the virus concentration around the virus source.
Example 2.
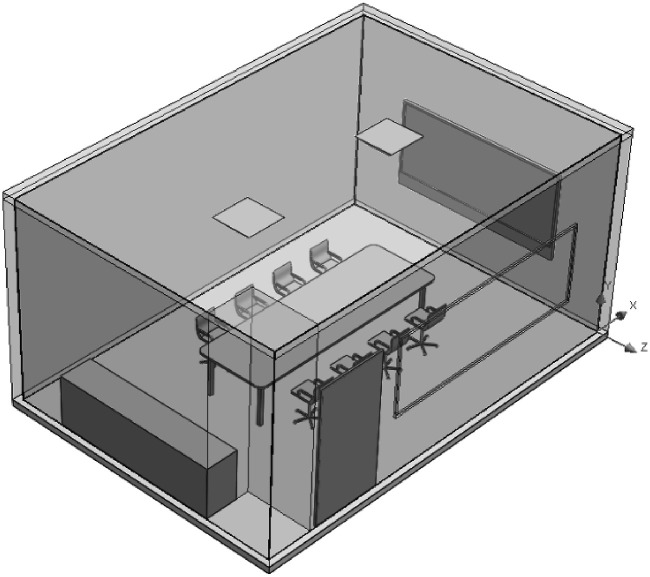
We had conducted an on-site measurement study of indoor CO2 concentration in a meeting room in a university. The volume of the room is about 78 m3 (the length, width, and height of the room are 6.2 m, 4.2 m, and 3 m, respectively). The room is without windows but equipped with a door and two air outlets for the air conditioning system, as shown in Fig. 1.
Figure 1.
Conference room configuration.
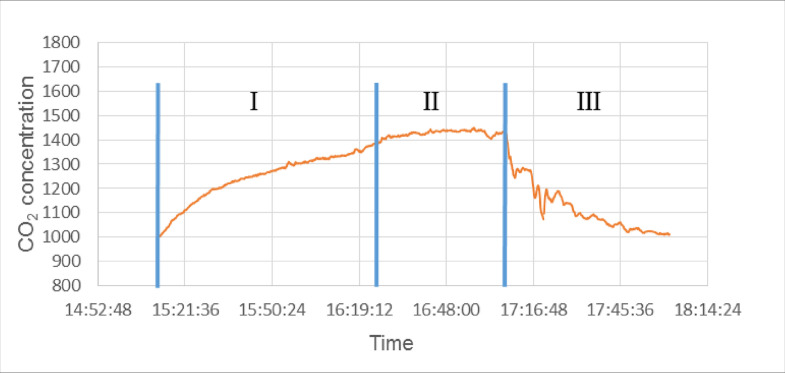
In the case of six people closed for use, the change in CO2 concentration is shown in Fig. 2 when the initial concentration is about 1000 ppm. The CO2 concentration increased rapidly in the beginning, reached more than 1400 ppm after about 60 min (zone I), and maintained a plateau of about 1440 ppm (zone II). The estimated ventilation flow was about 167 CMH (zone I and II) at this time, which is smaller than the required 36 CMH/person ∗ 6 people = 216 CMH People left the meeting room after 2 h of presence. With the door opened, it took 1 h for the CO2 concentration in an unused conference room to return to the initial concentration (zone III). If we set an indoor concentration of 800 ppm as the target, the estimated exhaust volume must reach about 450 CMH, which is bigger than the required 216 CMH.
Figure 2.
Changes in CO2 concentration in the conference room.
The advantage of indoor CO2 concentration as an alternative indicator is that it can reflect the real-time dynamic changes over time. For Example, in an indoor space with insufficient ventilation, the indoor CO2 concentration will gradually accumulate and rise, exceeding the standard after a while. Suppose the minimum requirements for ventilation volume cannot be met due to insufficient resources or other considerations. In that case, we can monitor indoor CO2 concentration in real-time and ensure that the risk of indoor air transmission is minimized by employing intermittent exhaust or limitation of residence time before exceeding the standard (see Part III of this guideline for details).
However, in an environment where other CO2 emitting sources (such as combustion) indoors and outdoors exist, the indoor CO2 concentration may be inaccurate, and the ventilation capacity of the room may be underestimated. An environment equipped with the recirculation device with a high-efficiency filter, including a portable HEPA filter and a ceiling-mounted HEPA-UV air filter, can effectively filter indoor air. However, the indoor CO2 concentration will accumulate continuously due to the lack of introducing fresh outdoor air into the room, leading to underestimating the ventilation capacity of the room.6 Therefore, we do not recommend using indoor CO2 concentration as a proxy indicator for indoor ventilation volume in the above situations.
The following technical requirements for the monitoring of indoor CO2 concentration should be followed:
-
1.
We recommend positioning the CO2 sensor at the height of 1.2–1.5 m from the ground or the height of the human breathing zone and at least 20 cm away from the CO2 emitting sources (like humans).
-
2.
Provided that the previous point is met, we recommend that the CO2 sensor be placed in the center of the personnel activity area.
-
3.
Make sure that the indoor air is evenly mixed. One CO2 sensor is sufficient for space smaller than 24 m2. For a space with an area larger than 24 m2, multiple CO2 sensors are needed.
-
4.
Avoid the CO2 sensor from direct contact with the airflow from the HVAC system or make-up air from windows to prevent underestimating the actual concentration.
-
5.
Please calibrate and operate the CO2 sensor following the instrument manufacturer's instructions.
Method to achieve adequate ventilation rate
The WHO guideline recommends the use of mechanical ventilation or natural ventilation to achieve adequate ventilation.5 Options for mechanical ventilation include:
-
1.
Installation of mechanical exhaust fans directly on the wall or window.
-
2.
Installation of an air-conditioning system that can exhaust outward.
For these two mechanical ventilation methods, please refer to the rated ventilation volume provided by the manufacturer. Nevertheless, be aware of the gap between the rated exhaust volume and the actual performance due to pipeline resistance. In addition, the exhaust fan and air conditioning system also have significant restrictions. The exhaust fan requires additional installation, and it may compromise the cooling capacity of the operating air-conditioning system. Standard air-conditioning systems in Taiwan usually do not exhaust outward, and additional renovation is also needed. The following technical requirements for mechanical ventilation should be followed7 , 8:
-
1.
Adequate intake air volume (air supply) corresponding to the exhaust volume is required.
-
2.
If the air-conditioning system can introduce outdoor air, and the outdoor weather does not significantly affect the indoor temperature and humidity, it is recommended to open the outdoor air damper to reduce HVAC recirculation.
-
3.
If feasible, it is recommended to operate the HVAC system around the clock as much as possible. When the building is unused (before use and after use), it is recommended to operate the system for 2 h with maximum outdoor airflow. Nevertheless, if the CO2 concentration is below 1000 ppm or 800 ppm, the system can be shut down.
-
4.
The direction of the exhaust outlet is recommended to be downward or perpendicular to the outdoor airflow to prevent strong winds from blowing into the room.
-
5.
Turn off the “demand-controlled ventilation” (DCV) setting to ensure that the air supply does not decrease when the temperature or the number of people in the room change.
-
6.
If there is a thermostat, set the fan to “on” instead of “auto” to ensure the fan continuously operates when heating or air-conditioning is not required.
Subject to weather changes, it is challenging for natural ventilation to maintain stable ventilation volume. In addition, the indoor temperature and humidity will be affected by the outdoor, resulting in insufficient thermal comfort. Natural ventilation may compromise the cooling capacity of the operating air-conditioning system. Cross-ventilation (open doors and windows) ventilate better than single-sided ventilation (open windows only). When opening doors and windows, the formula for the estimated natural ventilation volume is as follows5:
Natural ventilation volume (m3/hour, CMH)=0.65 x wind speed (m/s) x minimum ventilation area (m2) x 3600 (s/hour).
Note: If the mosquito screen is installed, the estimated ventilation volume should be halved.
It can be seen that the larger the ventilation area, the larger the ventilation volume can be obtained. Measures that enhance natural ventilation effectiveness include placing an electric fan next to the window that exhausts outward or combining natural ventilation with sub-optimal alternatives such as recirculation or intermittent exhaust.
If minimum requirements for ventilation volume cannot be met by mechanical or natural ventilation due to insufficient resources or other considerations, the next best alternative is recirculation. The practical approach to utilize recirculation to assist in diluting the pollutant concentration and making up the gap to the required ventilation volume include5:
-
1.
Portable HEPA filter.
-
2.
Ceiling-mounted HEPA-UV air filter.
Example 3.
-
•
In a 6-person reading room (36 CMH/person) or a 4-person gym (54 CMH/person), the minimum requirement for ventilation volume is 216 CMH. If the room is not equipped with mechanical ventilation and natural ventilation cannot be applied, the ventilation volume of the stand-alone portable HEPA filter should be at least 216 CMH.
-
•
If the CADR (clean air delivery rate) of a commercially available air purifier is 270 CMH, it can meet the aforementioned scenario's required ventilation volume.
The ASHRAE guideline recommends that the minimum efficiency reporting value (MERV) of the filtration system be targeted to 13 or more, providing that the HVAC system's performance and user comfort are not affected.8 , 9 On the other hand, the WHO guideline recommends MERV 14. MERV 13 can capture 50% of particles 0.3–1.0 μm in size and 85% of particles 1–3 μm in size; while MERV 14 can capture 75% of particles 0.3–1.0 μm in size and 90% of particles 1–3 μm in size.5
The US-CDC recommends the “2/3 rule”. The air purifier should provide a minimum CADR flow rate (unit: ft3/min, i.e., CFM) of more than 2/3 times the room area (unit: ft2). For conversion to the metric system, providing that 1 ft is about 0.3048 m, the flow rate (unit: CMH) should be 2/3∗ 2 ∗ (0.3048 m/ft)3 ∗ 60 min/h=12.192 times the room area (unit: m2). For Example, for a room with an area of 300 ft2 (approximately 27.87 m2), the CADR should be 200 CFM (approximately 339.80 CMH). If the height of this room exceeds 8 feet (approximately 2.44 m), the required minimum CADR needs to be divided by 8 feet (or 2.44 m) and then multiplied by the actual room height.7 The ASHRAE guideline suggests that high-risk spaces such as waiting rooms, prisons, and shelters may prioritize UV sterilization devices.8 , 9
The following technical requirements for recirculation should also be followed:
-
1.
The HEPA filter should be placed as close as possible to the personnel activity area to increase the collection efficiency. The farther the distance, the worse the collection efficiency.
-
2.
The ventilation volume provided by recirculation does not reduce the indoor CO2 concentration. Therefore, it is not recommended to use the indoor CO2 concentration as a proxy indicator of indoor ventilation volume when applying recirculation.
-
3.
The filtration material should be replaced regularly and should be deemed contaminated during replacement. The personnel responsible for replacement should wear appropriate personal protective equipment, and the replaced material should be sealed in a plastic bag before discarding.
Even if adequate ventilation is achieved by mechanical or natural ventilation or recirculation, there may still exist localized regions in the room that can be described as poorly ventilated dead spaces or air-retaining air pockets, potentially leading to accumulation of viral concentration. It is suggested that the following approaches can be utilized to enhance the evenly mixing of indoor air5:
-
1.
Electric fan
-
2.
Ceiling fan
-
3.
Split-type air conditioner
The US-CDC guideline reminds us to avoid placing an electric fan in a position where (potentially contaminated) air may flow directly from one person to another. It is suggested that the fan blows toward unoccupied corners and wall spaces or the top of occupied areas, and high-speed settings should be avoided.7 The ceiling fan should blow downward and mix the air with the jet flow, which is more efficient.
Alternatives when adequate ventilation volume is unable to reach
If mechanical or natural ventilation or recirculation is not feasible or does not work in practice, alternative suggestions include intermittent exhaust and limiting the number of occupants or residence time.
Intermittent exhaust refers to the use of an exhaust fan with sufficient ventilation volume to perform a short period of rapid ventilation (e.g., 10–20 min per hour) so that it can balance comfort during most of the time and sufficient ventilation volume. In combination with real-time monitoring of indoor CO2 concentration and not exceeding the standard, the intermittent exhaust is a practical way of ventilation.
When it is entirely impossible to improve the ventilation of the indoor space with engineering controls, administrative controls can be used to the number of occupants or residence time. When the number of occupants is reduced, the total required ventilation volume of the room will correspondingly decrease. In an indoor space with insufficient ventilation volume, the indoor CO2 concentration will gradually accumulate and rise, exceeding the standard after a while. Therefore, if the limited number of occupants is small enough, the indoor CO2 concentration may not exceed the standard during the stay; if the limited residence time is short enough, it can be stipulated that the stay should end before the indoor CO2 concentration exceeds the standard. In addition to real-time monitoring of indoor CO2 concentration not exceeding the standard, the Wells–Riley model can also be applied to estimate the maximum number of occupants or the maximum residence time allowed in a specific indoor space in advance.
In short, the Wells–Riley model is a risk assessment method of airborne transmission suitable for confined indoor spaces. The basic concept in the model, “quantum of infection,” refers to the minimum dose for infectious particles that can cause 63% of susceptible hosts to get infected. It is not an actual physical unit but a hypothetical dose calculated based on epidemiological literature, combining infectious particles numbers produced, infectivity, and respiratory deposition characteristics. The original formula of the Well-Riley model can be rewritten as following after derivation10:
: basic reproduction number.
: the number of occupants.
: residence time.
: indoor CO2 concentration, which is affected by . Measurement is required.
: outdoor CO2 concentration. Measurement is required.
: quantum generation rate, which is a constant. For COVID-19, the reference value from existing literature ranges between 14-48.11
Input the number of occupants and residence time according to the current situation or demands, and input the indoor and outdoor CO2 concentration based on the measurement, then the estimate can be calculated based on the above formula. For Example, the team lead by Professor Brian Pavilonis of The City University of New York (CUNY) used this approach to estimate the infection risk of New York public schools and nail salons.12 Moreover, the maximum number of occupants or the longest residence time in the indoor space can also be estimated backward. The goal is to make less than 1 or 0.9 to slow down the indoor air transmission.
Example 4.
-
1.
There are 20 people in an office, and the measured indoor CO2 concentration is 650 ppm. The is calculated to reach 1.49.
-
2.
The company implements a policy for employees to take turns to come into the office. Ten people work from home, and ten people are left in the office. The measured indoor CO2 concentration is 500 ppm, and the can be reduced to 0.57.
-
3.
The office maintains 20 people, but the stay time is reduced to 4 h, and the can be reduced to 0.76.
| Occupants (persons) | Residence time (hour) | Measured indoor CO2 concentration (ppm) | Measured outdoor CO2 concentration (ppm) | Estimated ∗ |
|---|---|---|---|---|
| 20 | 8 | 650 | 400 | 1.49 [0.69–2.25] |
| 10 | 8 | 500 | 400 | 0.57 [0.26–0.87] |
| 20 | 4 | 650 | 400 | 0.76 [0.35–1.16] |
∗Note that the estimate is calculated by inputting the average of the range of : (14 + 48)/2 = 31. The upper and lower bound of the , calculated with the maximum value 48 and the minimum q value 14, respectively, is also provided.
Conclusion
While effective measures for droplet transmission (e.g., mask-wearing and social distancing) and contact transmission (e.g., hand washing and surface cleaning) remained the primary focus for COVID-19 infection control in Taiwan and most countries in the world, we should not underrate the importance of containing airborne transmission by improving the ventilation system. Even in countries with an adequate level of vaccination, the epidemic could recur without appropriately addressing issues on indoor ventilation. The governments should acknowledge the scientific evidence and take measures to establish official regulations and guidelines for ventilation of indoor spaces to reduce COVID-19 transmission.
Declaration of competing interest
We declare no potential financial and nonfinancial conflicts of interest.
References
- 1.Somsen G.A., vanRijn C., Kooij S., Bem R.A., Bonn D. Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. Lancet Respir Med. 2020;8(7):658–659. doi: 10.1016/S2213-2600(20)30245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US-CDC . Vol. 2021. 2021. Scientific brief: SARS-CoV-2 transmission.https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html [Internet]Available from: [Google Scholar]
- 3.WHO . Vol. 2021. World Health Organization; 2020. Coronavirus disease (COVID-19): how is it transmitted?https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted [Internet]Available from: [Google Scholar]
- 4.Bazant M.Z., Bush J.W.M. A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci U S A. 2021 doi: 10.1073/pnas.2018995118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . vol. 38. 2021. Roadmap to improve and ensure good indoor ventilation in the context of COVID-19. [Google Scholar]
- 6.SAGE-EMG . 2020. EMG: role of ventilation in controlling SARS-CoV-2 transmission.https://www.gov.uk/government/publications/emg-role-of-ventilation-in-controlling-sars-cov-2-transmission-30-september-2020 - GOV.UK [Internet]. 2020 [cited 2021 Aug 1]. Available from: [Google Scholar]
- 7.US-CDC . 2021. Ventilation in buildings | CDC. [Internet]. [cited 2021 Aug 1]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html. [Google Scholar]
- 8.Schoen L.J. Guidance for building operations during the COVID-19 pandemic. ASHRAE J. May 2020:72–74. [Google Scholar]
- 9.ASHRAE . 2020. ASHRAE position document on infectious aerosols.https://www.ashrae.org/file library/technical resources/ashrae journal/2020journaldocuments/72-74_ieq_schoen.pdf [Internet]. [cited 2021 Aug 1]. Available from: [Google Scholar]
- 10.Rudnick S.N., Milton D.K. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air. 2003;13(3):237–245. doi: 10.1034/j.1600-0668.2003.00189.x. [DOI] [PubMed] [Google Scholar]
- 11.Dai H., Zhao B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Build Simul. 2020:1–7. doi: 10.1007/s12273-020-0703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pavilonis B., Ierardi A.M., Levine L., Mirer F., Kelvin E.A. Estimating aerosol transmission risk of SARS-CoV-2 in New York City public schools during reopening. Environ Res. 2021;195:110805. doi: 10.1016/j.envres.2021.110805. [DOI] [PMC free article] [PubMed] [Google Scholar]