Abstract
Thoracic outlet syndrome (TOS) is a rare neurovascular disorder generally caused by the presence of a cervical rib or hypertrophic scalene anterior muscle that can compress the brachial plexus and/or subclavian vessels. In the vascular form, the symptoms are caused by the compression of the artery and/or the subclavian vein. In the first case, the compression is caused by the cervical rib and leads to hypo-perfusion with cooling and cyanosis of the upper limb, while in the second case, the compression is caused by the anterior scalene muscle and leads to congestion, cyanosis, swelling and pain in the higher limb. In this paper, we describe a case with the simultaneous presence of a bilateral cervical rib and bilateral hypertrophy of the anterior scalene muscle. TOS diagnosis is based on neurological, clinical and instrumental tests, such as chest radiography and color Doppler ultrasonography. The treatment of these patients can be surgical or conservative.
Keywords: Anterior scalene, Thoracic outlet syndrome, Color Doppler
Introduction
Thoracic outlet syndrome (TOS) is a rare neurovascular pathology [1, 2] generally caused by the presence of cervical ribs [3–5] and/or hypertrophy of the anterior scalene muscle [6, 7] that, respectively, compress the brachial plexus with consequent neurological symptoms (neurological form) and/or compress subclavian vessels (vascular form). In the vascular form, symptoms may have an arterial origin, due to compression from the subclavian artery, or a venous origin by compression of the subclavian vein. In the first case, generally, symptomatology is due to the cervical rib, which causes hypo-perfusion with cooling and cyanosis of the upper limb. In the second case, symptomatology is due to hypertrophy of the anterior scalene muscle, which compresses the subclavian vein and causes venous stasis with cyanosis, swelling and pain in the upper limb.
The unilateral cervical rib is a common finding and may be asymptomatic, whereas the bilateral cervical rib is less frequent [8, 9]. The simultaneous presence of a bilateral cervical rib and bilateral anterior scalene muscle hypertrophy is very rare. This syndrome generally affects the female sex aged between 20 and 50 years. The diagnosis of TOS, in addition to neurological and clinical tests, involves instrumental investigations such as standard chest radiography and ultrasound, which can highlight the presence of cervical ribs and vascular alterations [10–12]. Patient treatment can be conservative or surgical. Conservative treatment, including physiotherapy, massage and kinesitherapy, as well as treatment with local anesthetic drugs, is generally aimed at reducing the vascular compression caused by muscular hypertrophy [13–16]. Surgical treatment, including scalenectomy and resection of the cervical rib or the first rib, is aimed at the decompression of vascular structures [17–19].
Case report
We describe the case of a 29-year-old patient who had been experiencing morning onset of swelling and pain in his upper limbs for the duration of a few weeks. The patient was paraplegic due to a vertebral injury caused by a car accident a few months before and was therefore confined to a wheelchair. The patient had already been diagnosed with a standard chest radiograph of bilateral cervical rib (Fig. 1), which did not provide clinical symptoms.
Fig. 1.

Standard chest X-ray. In this image, the right cervical rib (short arrow) and the left cervical rib (arrow heads) are easily identified
For this reason, a clinical examination was performed with the arms at 90° and arms raised (Adson’s test). This test was positive for a slight reduction in the radial pulses bilaterally. The patient was then subjected to ultrasonographic control with power Doppler, color Doppler and duplex ultrasonography of the subclavian vessels. The ultrasound was performed by an operator with decades of experience in the sector.
An Aplio XG (Toshiba) ultrasound system with a 7.5-MHz linear probe was used.
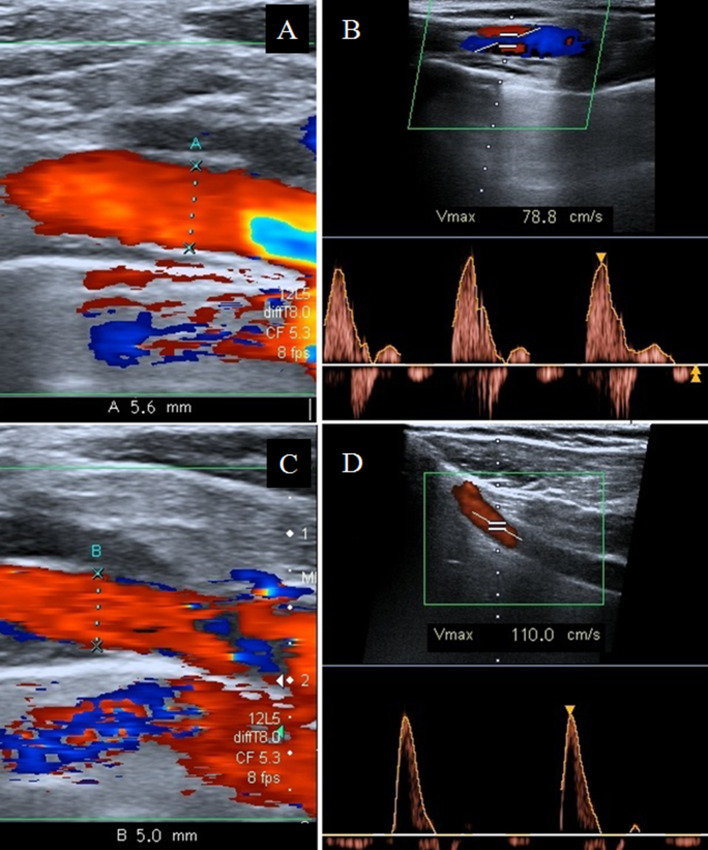
Ultrasonographic tests of the subclavian vessels were performed with the patient seated, with arms lowered, with arms at 90° and with arms raised. Longitudinal and transverse subclavian scans were performed. The ultrasound control with arms raised, performed in the middle section of the right and left subclavian arteries, highlighted a slight bilateral reduction in caliber and a slight increase in systolic peak velocity (Fig. 2a–d); the results are summarized in Table 1.
Fig. 2.
Sub-clavicular ultrasound scan. The color Doppler and Duplex ultrasonography study, performed in the middle section of the right subclavian artery with lowered arms, shows: a a regular diameter (5.6 mm) (arrow) and b regular systolic peak velocity (78.8 cm/s). The ultrasound scan, performed with arms raised, shows: c a slight diameter reduction (5 mm) (arrow) and d a slight increase in the systolic velocity (110 cm/s)
Table 1.
Summary of results
| Right subclavian artery | Left subclavian artery | |||
|---|---|---|---|---|
| Diameter (mm) | Systolic peak velocity (cm/s) | Diameter (mm) | Systolic peak velocity (cm/s) | |
| Arms lowered | 5.6 | 78.8 | 5.8 | 56.6 |
| Arms raised | 5 | 110 | 5.2 | 97.6 |
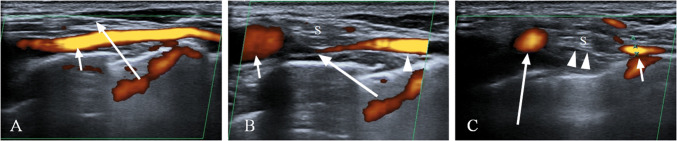
The study of the venous vessels on the right, at the level of the inter-scalene triangle, revealed significant stenosis of the right subclavian vein with arms at 90° and complete stenosis with arms raised (Fig. 3a–c); on the left, there was a significant reduction in the caliber of the subclavian vein with arms at 90° and almost complete stenosis with arms raised. The stenosis of the subclavian veins was caused by the anterior scalene muscle, which compressed them during the lifting of the limbs. No further vascular changes were noted. Subsequently, the patient was subjected to combined physical and osteopathic therapy, which led to a notable improvement in symptoms. The patient signed the informed consent form.
Fig. 3.
Power Doppler of the inter-scalene triangle. a The ultrasound scan, performed with lowered arms, shows a regular course and morphology of the right subclavian vein (short arrow). The anterior scalene muscle (long arrow). b The ultrasound scan, performed with arms at 90°, shows significant stenosis of the right subclavian vein (long arrow) and congestion in the pre-stenotic tract (short arrow) caused by the anterior scalene muscle (S). The stenotic tract of the subclavian vein (arrow heads). c In the ultrasound scan performed with arms raised, the anterior scalene muscle (arrow heads) can be seen causing the complete stenosis of the right subclavian vein, with dilatation of the pre-stenotic tract (long arrow) and diameter reduction in the post-stenotic tract (short arrow)
Discussion
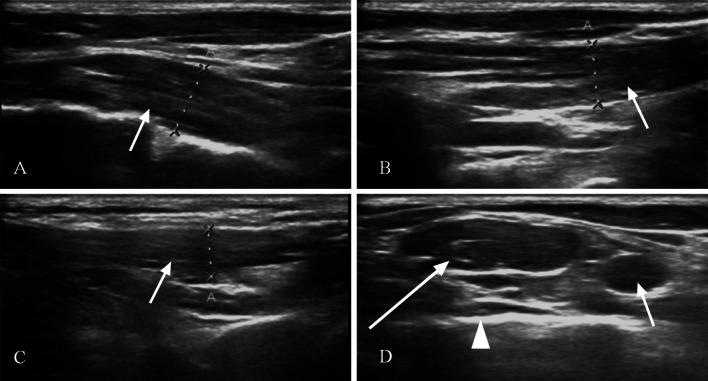
Pain, swelling, cyanosis and/or paresthesia of the upper limb in patients with cervical ribs are almost always due to TOS; symptoms, which are generally chronic, are more frequently due to cervical ribs that compress the brachial plexus and/or subclavian vessels in the costal-clavicular triangle (Figs. 4, 5). In our case, recent symptomatology could not be justified by the cervical ribs, which were present from birth, but probably could be explained by the hypertrophy of the scalene muscles. For this reason, and after excluding significant alterations to the subclavian arteries, we focused on the inter-scalene triangle, which is the anatomical space involved in the compression of subclavian veins that is formed anteriorly by anterior scalene muscle, posteriorly by the medial scalene muscle and inferiorly from the medial face of the first rib (Figs. 6a–d, 7). Within the inter-scalene triangle, the subclavian vein was easily compressed by a hypertrophic scalene anterior, especially when the patient raised his arms. The data emerging from the arterial vessels are therefore in agreement with the clinical history of the patient who, before becoming paraplegic, was asymptomatic. Significant elements have instead emerged from the ultrasound study of the subclavian veins: Scans performed with arms at 90° and with raised arms both showed the progressive compression of the subclavian veins at the level of the inter-scalene triangle caused by anterior scalene muscles. These data accord with the recent onset of the patient’s symptoms (swelling and morning pain in the upper limbs) and can be correlated, as reported in the literature [20], with the frequent physical efforts made by the patient to manually push the wheelchair.
Fig. 4.
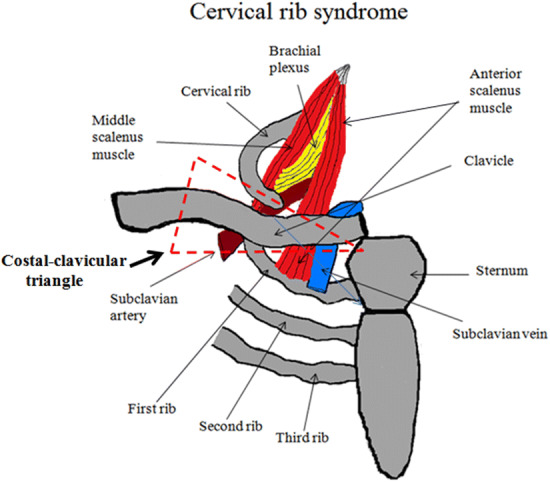
The costal-clavicular triangle, the space involved in cervical rib syndrome, consists anteriorly of the middle third of the clavicle, posteromedially from the first rib and posterolaterally from the upper profile of the scapula
Fig. 5.
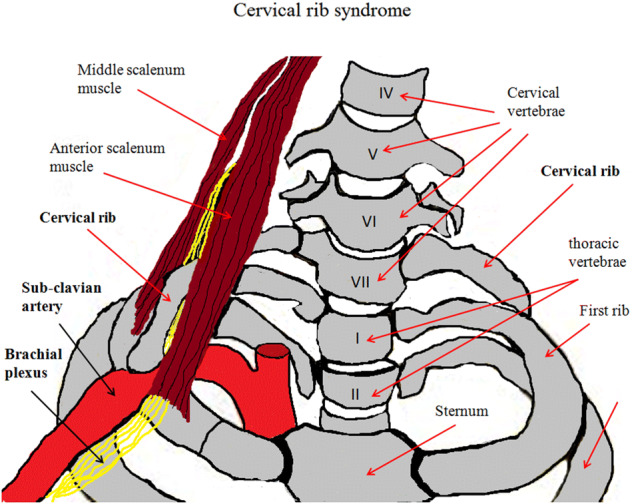
In cervical rib syndrome, the cervical rib may cause compression of the subclavian artery and brachial plexus
Fig. 6.
B-Mode ultrasound. The laterocervical, longitudinal scans show: a anterior scalene muscle (arrow). b Medium scalene muscle (arrow). c Posterior scalene muscle. d In this scan, the inter-scalene triangle is highlighted, along with the anterior scalene muscle (long arrow), the subclavian vein (short arrow) and the first rib (arrow head)
Fig. 7.
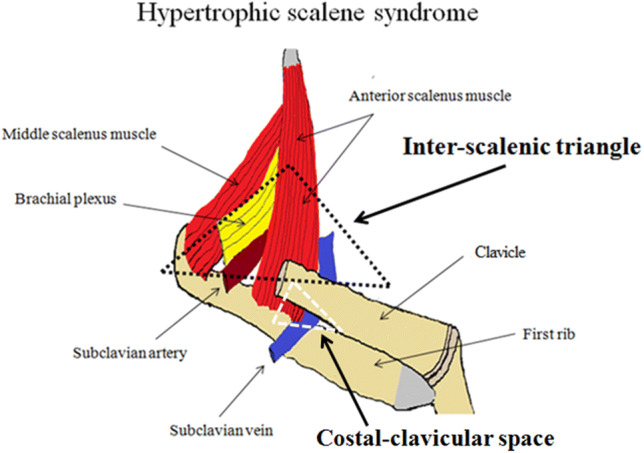
The inter-scalene triangle, the anatomical space involved in the hypertrophic scalene syndrome, is formed anteriorly by the anterior scalene muscle, posteriorly by the medial scalene muscle and inferiorly from the medial face of the first rib (black triangle). In the costal-clavicular space (white triangle), compression of the subclavian vein generally occurs following hypertrophy of the anterior scalene muscle
The morning prevalence of symptoms is explained by the posture assumed by the patient during sleep: prone, with arms alternately bent at 90°, as confirmed by a dynamic study of the subclavian veins with power and duplex Doppler. An ultrasound enabled us to carry out an accurate morphological study of the subclavian vessels and the inter-scalene triangle structures [21] and to identify the cervical ribs (Fig. 8) and their influence on the vascular structures dynamically. Ultrasonography, as in other forms of vascular compression—aortomesenteric syndrome [22], Dunbar syndrome [23], May–Thurner syndrome [24], etc.—allows rapid diagnostic classification and should be used, in our opinion, as a first-degree examination on suspicion of TOS.
Fig. 8.
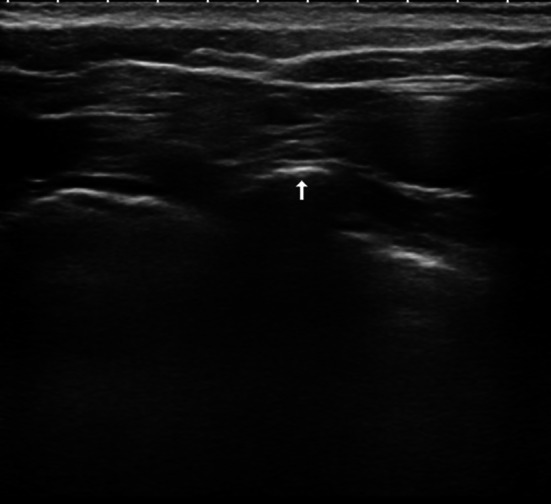
B-mode ultrasound: transverse subclavian scan showing a cervical rib (arrow)
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by RF, PVF, FAI, AC, AF, AC, MP, SS and AB. The first draft of the manuscript was written by RF, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Formal consent
For this type of study formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Klaassen Z, Sorenson E, Tubbs RS, et al. Thoracic outlet syndrome: a neurological and vascular disorder. Clin Anat. 2014;27(5):724–732. doi: 10.1002/ca.22271. [DOI] [PubMed] [Google Scholar]
- 2.Jones MR, Prabhakar A, Viswanath O, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5–18. doi: 10.1007/s40122-019-0124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang S, Shen H, Tan WQ, et al. Arterial thoracic outlet syndrome caused by cervical ribs-an unusual case report. Medicine (Baltimore) 2019;98(11):e14778. doi: 10.1097/MD.0000000000014778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang KZ, Likes K, Davis K, et al. The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg. 2013;57(3):771–775. doi: 10.1016/j.jvs.2012.08.110. [DOI] [PubMed] [Google Scholar]
- 5.Ozoa G, Alves D, Fish DE. Thoracic outlet syndrome. Phys Med Rehabil Clin N Am. 2011;22(3):473–483. doi: 10.1016/j.pmr.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Tucciarone L, Anaclerio S, Tomassini A, et al. Anterior scalenus syndrome in pediatric age. Report of a case. Minerva Pediatr. 1996;48(10):461–464. [PubMed] [Google Scholar]
- 7.Bortolani E, Miani S, D’Armini A, et al. Role of anterior scalene muscle hypertrophy in thoracic outlet syndrome. Minerva Chir. 1989;44(8):1305–1309. [PubMed] [Google Scholar]
- 8.Cu N, Ec I, Rt E, et al. Thoracic outlet syndrome from bilateral cervical ribs—a clinical case report. J Orthop Case Rep. 2018;8(2):78–80. doi: 10.13107/jocr.2250-0685.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan A, Rattihalli RR, Hussain N, et al. Bilateral thoracic outlet syndrome: an uncommon presentation of a rare condition in children. Ann Indian Acad Neurol. 2012;15(4):323–325. doi: 10.4103/0972-2327.104349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim TI, Sarac TP, Orion KC. Intravascular ultrasound in venous thoracic outlet syndrome. Ann Vasc Surg. 2019;54:118–122. doi: 10.1016/j.avsg.2018.08.077. [DOI] [PubMed] [Google Scholar]
- 11.Nichols AW. Diagnosis and management of thoracic outlet syndrome. Curr Sports Med Rep. 2009;8(5):240–249. doi: 10.1249/JSR.0b013e3181b8556d. [DOI] [PubMed] [Google Scholar]
- 12.Napoli V, Vignali C, Braccini G, et al. Echography and echo-Doppler in the study of thoracic outlet syndrome. Correlation with angiographic data. Radiol Med. 1993;85(6):733–740. [PubMed] [Google Scholar]
- 13.Vanti C, Natalini L, Romeo A, et al. Conservative treatment of thoracic outlet syndrome A review of the literature. Eura Medicophys. 2007;43(1):55–70. [PubMed] [Google Scholar]
- 14.Hanif S, Tassadaq N, Rathore MF, et al. Role of therapeutic exercises in neurogenic thoracic outlet syndrome. J Ayub Med Coll Abbottabad. 2007;19(4):85–88. [PubMed] [Google Scholar]
- 15.Buonocore M, Manstretta C, Mazzucchi G, et al. The clinical evaluation of conservative treatment in patients with the thoracic outlet syndrome. G Ital Med Lav Ergon. 1998;20(4):249–254. [PubMed] [Google Scholar]
- 16.Weaver ML, Hicks CW, Fritz J, et al. Local anesthetic block of the anterior scalene muscle increases muscle height in patients with neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2019;59:28–35. doi: 10.1016/j.avsg.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 17.Morel J, Pirvu A, Elie A, et al. Functional results of cervical rib resection for thoracic outlet syndrome: impact on professional activity. Ann Vasc Surg. 2019;56:233–239. doi: 10.1016/j.avsg.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Sen S, Dişçigil B, Boga M, et al. Thoracic outlet syndrome with right subclavian artery dilatation in a child transaxillary resection of the pediatric cervical rib. Thorac Cardiovasc Surg. 2007;55(5):339–341. doi: 10.1055/s-2006-955875. [DOI] [PubMed] [Google Scholar]
- 19.Degeorges R, Reynaud C, Becquemin JP. Thoracic outlet syndrome surgery: long-term functional results. Ann Vasc Surg. 2004;18(5):558–565. doi: 10.1007/s10016-004-0078-6. [DOI] [PubMed] [Google Scholar]
- 20.Baltopoulos P, Tsintzos C, Prionas G, et al. Exercise-induced scalenus syndrome. Am J Sports Med. 2008;36(2):369–374. doi: 10.1177/0363546507312166. [DOI] [PubMed] [Google Scholar]
- 21.Domkundwar S, Autkar G, Khadilkar SV, et al. Ultrasound and EMG–NCV study (electromyography and nerve conduction velocity) correlation in diagnosis of nerve pathologies. J Ultrasound. 2017;20:111–122. doi: 10.1007/s40477-016-0232-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farina R, Foti PV, Cocuzza G, et al. Wilkie’s syndrome. J Ultrasound. 2017;20(4):339–342. doi: 10.1007/s40477-017-0257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamamoto M, Itamoto T, Oshita A, et al. Celiac axis stenosis due to median arcuate ligament compression in a patient who underwent pancreatoduodenectomy; intraoperative assessment of hepatic arterial flow using Doppler ultrasonography: a case report. J Med Case Rep. 2018;12(1):92. doi: 10.1186/s13256-018-1614-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moudgill N, Hager E, Gonsalves C, et al. May-Thurner syndrome: case report and review of the literature involving modern endovascular therapy. Vascular. 2009;17(6):330–335. doi: 10.2310/6670.2009.00027. [DOI] [PubMed] [Google Scholar]