Abstract
Congenital lung malformations (CLMs) include a group of different disorders. With widespread use of antenatal ultrasonography (aUS) and increased use of pre-natal magnetic resonance imaging (MRI), CLMs are increasingly detected, nevertheless the best postnatal imaging approach is not yet well defined: newborns usually undergo several chest X-rays and eventually computed tomography to confirm the diagnosis. In this case series, we show lung ultrasound features of three different cases of congenital lung malformations, describing prenatal and postnatal images comparing different imaging techniques.
Keywords: Lung ultrasound, Congenital lung malformation, Neonatal, Pulmonary sequestration
Introduction
Congenital lung malformations (CLMs), or congenital pulmonary airway malformation (CPAM), include a group of different disorders, the most common being congenital cystic-adenomatoid malformation (CCAM), bronchopulmonary sequestration (BPS) (either intra or extralobar), hybrid lesions that contain elements of both CCAM and BPS, bronchial atresia, congenital lobar emphysema (CLE), and bronchogenic cyst [1].
With widespread use of antenatal ultrasonography (aUS) and increased use of antenatal magnetic resonance imaging (aMRI), CLMs are increasingly detected. In any case, a prenatal diagnosis needs a post-natal confirmation and subsequently a multidisciplinary approach to decide the best management of the patient.
An appropriate management should consider choosing the best timing for further imaging, or choosing between conservative and surgical treatment, as well as the most appropriate time for surgery. Resection of symptomatic CLMs in the neonatal period is accepted; the best approach for asymptomatic newborns with a prenatal diagnosis of CLM currently is to undergo serial chest X-ray (CXR) and eventually thoracic Computed Tomography (CT) scan, since CXR may be negative or inconclusive [2].
In the last years, lung ultrasound (LUS) is increasingly used in pediatric and neonatal practice, but its role for the evaluation of CLMs has not yet been assessed. For this reason, here we report a case series of three newborns with CLMs evaluated according to current clinical practice, comparing standard radiological findings with LUS. Ethical consent was obtained by parents of all children.
Methods
LUS was performed by an experienced pediatrician specifically trained both in pediatric ultrasound (regularly certified by the Italian Society of Ultrasound in Medicine and Biology, SIUMB) and in lung ultrasound (certified by the Italian Academy of Thoracic Ultrasound, ADET). LUS was performed using an Esaote MyLab linear probe at 12 mHz, “small parts” preset. Longitudinal and transverse sections were collected on the anterior, lateral, and posterior chest wall, bilaterally. Images and clips were stored and archived.
Written informed consent was obtained before data collection from a parent/guardian. Our institution’s Ethical Committee approved the study (protocol FPG2406_2019). All patients’ data were analyzed anonymously.
Case 1
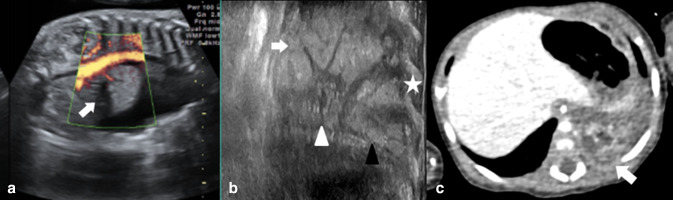
A term newborn with aUS diagnosis of hydrothorax and lung mass (Fig. 1a). Prenatally, at 32 weeks of gestation age a first thoracentesis and drainage of amniotic fluid were performed after fetal steroid prophylaxis. A second thoracentesis for persistence of hydrothorax and polyhydramnios was performed 7 days later. Born by cesarean section, presented respiratory distress and bradycardia at birth (APGAR 7-7). Arterial pH at birth was 7.22, base excess − 6.5. A thoracentesis performed in the delivery room yielded about 120 cc of serous material. The control CXR showed hypertensive pneumothorax with mediastinal shift; pleural drainage was placed with improvement of saturation and normalization of subsequent radiographs; no intrathoracic lesions were documented at CXR. Point-of-care lung ultrasound (Fig. 1b) showed, an echogenic, non-aired lesion in the basal left hemythorax. Subsequently a chest CT scan (Fig. 1c) confirmed the presence of an expansive mass in the left hemythorax, with a heterogeneous contrast enhancement and two feeding vessels (arterial afferents) originating from the thoracic aorta; these finding were consistent with an extralobar sequestration which was excised at 4 months of age
Fig. 1.
a Prenatal ultrasound showing an echogenic thoracic mass with a main vessel (with arrow); b post-natal thoracic ultrasound showing an echogenic thoracic mass (white arrow) with a characteristic central hypogenic “star-like mass” (black triangle), in contact with the diaphragm (black triangle) and ribs (white star); c CT scan confirms the presence of the thoracic lesion (white arrow)
Follow-up: the child underwent surgical resection at 3 month of age; currently, he is 8 months old and is in good clinical conditions.
Case 2
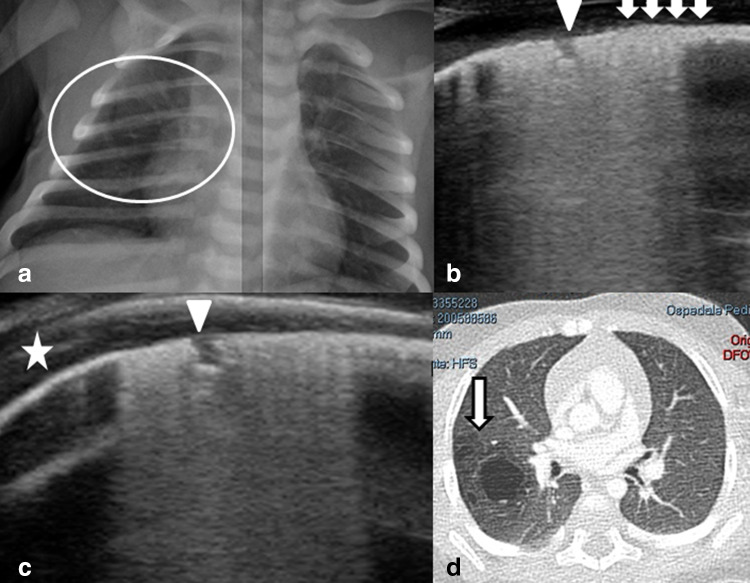
A term newborn was evaluated in the first day of life because of a pre-natal diagnosis of suspected CCAM; prenatal US obtained at 20 and 34 weeks gestational age showed a hyperechoic mass in the right lung; cystic areas were documented within the mass, the largest measuring 19 × 20 × 21 mm. He was born by vaginal delivery. At birth he presented good cardio-respiratory adaptation and normal clinical examination (APGAR 9-9). No blood tests were performed at birth given the stable conditions. At CXR an ovalar hyperinflated area was noticed; no pneumothorax, nor pleural effusion were documented (Fig. 2a). LUS showed an irregular pleural line in right hemythorax characterized by microcistic lesions (Fig. 2b) with a single bigger cyst (Fig. 2c) and confluent vertical artifacts beyond the pleural abnormalities (supplementary video shows how localized are these findings, surrounded by normal pleural line). CT scan (Fig. 2d) performed at 3 months of life showed parenchymal structural subversion of the upper right lobe, characterized by the presence of at least four cystic hypodense formations with a slight parietal profile, diameter of the cysts ranged between 2 and 24 mm.
Fig. 2.
a Chest X-ray showing a suspected hyperlucent ovalar lesion in the right hemy-thorax (white circle); b, c post-natal lung ultrasound shows a characteristic thickened pleura with microcistic-like hypoechoic lesions within the pleural line (white triangles), a bigger round subpleural lesion (white arrow) and posterior vertical artifacts. The close parts of the pleural line is normal (white star); d the CT scan confirmed the lung malformation (arrow)
Follow-up: the child underwent surgical resection at 3 month of age; currently, he is 5 months old and is in good clinical conditions.
Case 3
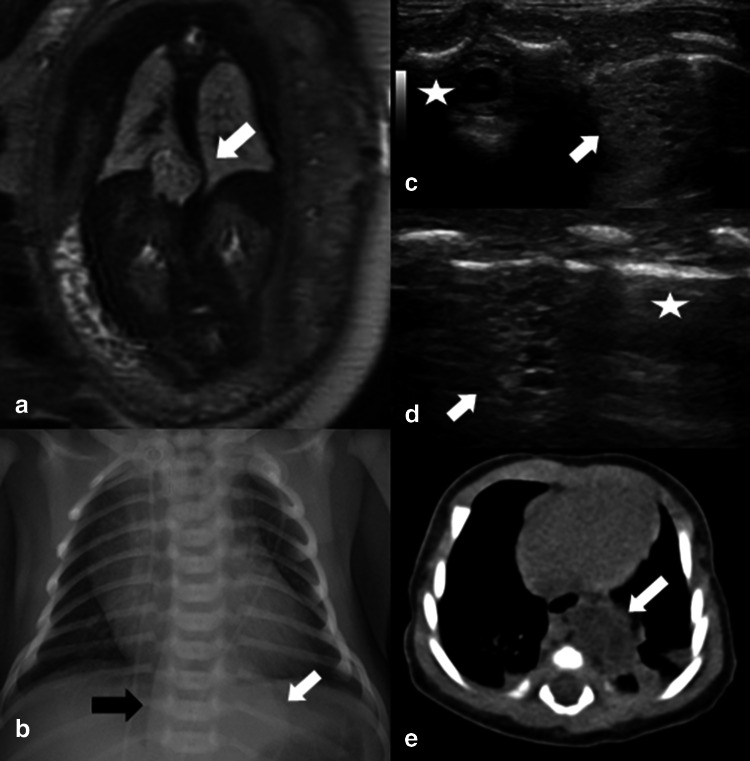
A term newborn was evaluated in the first day of life because of suspected CLM. Prenatal ultrasound showed a hyperechoic lesion in the left hemi-thorax and a cutaneous lymphangioma. The fetal MRI (Fig. 3a) showed a hyper-intense thoracic mass displacing the thoracic aorta, consistent with pulmonary sequestration. He was born by vaginal delivery. At birth, the child had good cardio-respiratory adaptation (APGAR 9-10). Physical examination was normal. No blood tests were performed at birth given the stable conditions. At CXR (Fig. 3b) a hyperechoic lesion and displacement of the thoracic aorta were documented. These findings were confirmed at echocardiography. LUS examination (Fig. 3c) showed a hypoechoic mass having inside multiple hypoechoic microcystic; two main vessels entered the lesion (one artery and one vein). CT scan confirmed the presence of an extralobar pulmonary sequestration with arterial supply by left gastric artery.
Fig. 3.
a Prenatal MRI showing a thoracic mass with deviation of the aorta (white arrow). b Chest X-ray showed a suspected left supra diaphragmatic lesion (white arrow) and deviation of the aorta through the right (black arrow); c post natal lung ultrasound (intercostal/transvers view) shows an echogenic lesion, having inside multiple hypoechoic microcystic lesions (white arrow), close to the vertebrae (white star); d lung ultrasound (longitudinal view) shows the same lesion (white arrow) surrounded by normal pleural line (white star); e CT scan confirmed the presence of the thoracic lesion (white arrow)
Follow-up: the child he is 2 months old and is in good clinical conditions; surgical resection is planned at around 4–5 months of age.
Discussion
The antenatal course of congenital lung lesions varies from complete resolution to hydrops and fetal death; nevertheless, the ability to predict the postnatal course by a US is limited [3]. In any case, prenatal diagnosis needs a post-natal confirmation, since some cases can have an antenatal resolution. In fact, while some prenatal indicators (mediastinal shift, diaphragratic inversion, mass volume ratio, polihydramnios, hydrothorax, hydrops, etc.) may be useful, they are not very accurate for prediction of rare prenatal complications or postnatal course. On this regard, Cavoretto et al. [4] recently described the antenatal management and outcome of 193 fetuses with an echogenic lung lesion, showing that hat CHAOS is a serious abnormality, whereas CCAM and BPS in the absence of hydrops are associated with a good prognosis. In general, in about 60% of these cases no lesions can be demonstrated by postnatal CXR [4]. Although it is known that CLMs are often not detected at CXR, postnatal assessment is still made by plain CXR. For this reason, whatever the result of CXR, CT scan is mandatory to confirm or rule out the antenatal diagnosis. CT scan is the best predictor of the presence of the lesion, and correlates well with surgical and histological findings. Also, chest MRI use is increasing in some neonatal unit showing promising results, although this is a technically more difficult exam not always available.
Despite the widespread use of LUS, there are only two reports about the use of LUS for CLMs comparing LUS, CXR and CT scan [5, 6].
Yousef et al. [5] reported on four cases diagnosed with CLM plus one case of CLM associated with congenital diaphragmatic hernia. For all the five patients, the suspicion of CLMs had been raised by the antenatal scans. They showed a high correspondence between CT scan and LUS findings, suggesting the role of LUS for the diagnosis of pulmonary malformations [5].
Quercia et al. [6] described seven cases (4 CPAM, 2 pulmunary sequestrations), describing (1) complete atelectasis of the left lower lobe, (2) pulmonary consolidation, (3) and macro and microcysts.
Our series confirms the utility of LUS to detected suspected CLMs and the limited utility of CXR, which may show unclear findings, adding new detailed images to the limited literature available. Moreover, our report is the first one comparing antenatal and postnatal imaging. In our series, all cases were easily described by LUS; the examination was performed at bed-side, with minimal discomfort for the newborn and no radiation exposure. Additionally LUS has the potential to allow close follow up of the patient during the outpatient visits while waiting for the pre surgical CT scan (or pMRI) that is mandatory to plan the best surgical approach. Nevertheless, it is important to emphasize the possible risks of LUS, despite the ever-growing enthusiasm for standardizing a method that is easily accessible and handy, especially to non-specialized practitioners [7]. Both false negatives and false positives are possible, as well as vertical artifacts can be misinterpreted. Also, needs of training of operators and minimum equipment requirements are needed and every institution (and national organizations) should certify minimal standards before implementing and routinely introducing the technique.
In conclusions, we think that our series widen the potential use of LUS [7] and that LUS could be potentially used to evaluate newborns with a prenatal diagnosis of CLMs, to confirm diagnosis, to follow-up the patient and to reduce radiation exposure.
Further, prospective and multi-centric studies are needed to confirm the advantages of LUS in CLMs, from birth to long-term post-surgical procedures.
Acknowledgements
We are grateful to Morgan Witkin for English editing.
Compliance with ethical standards
Conflict of interests
The authors have no conflict of interests to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kotecha S, Barbato A, Bush A, et al. Antenatal and postnatal management of congenital cystic adenomatoid malformation. Paediatr Respir Rev. 2012;13:162–170. doi: 10.1016/j.prrv.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Mon RA, Johnson KN, Ladino-Torres M. Diagnostic accuracy of imaging studies in congenital lung malformations. Arch Dis Child Fetal Neonatal Ed. 2018;104:F372–F377. doi: 10.1136/archdischild-2018-314979. [DOI] [PubMed] [Google Scholar]
- 3.Saeed A, Kazmierski M, Khan A, McShane D, Gomez A, Aslam A. (2013) Congenital lung lesions: preoperative three-dimensional reconstructed CT scan as the definitive investigation and surgical management. Eur J Pediatr Surg. 2013;23:53–56. doi: 10.1055/s-0033-1333890. [DOI] [PubMed] [Google Scholar]
- 4.Cavoretto P, Molina F, Poggi S, Davenport M, Nicolaides KH. Prenatal diagnosis and outcome of echogenic fetal lung lesions. Ultrasound Obstet Gynecol. 2008;32:769–783. doi: 10.1002/uog.6218. [DOI] [PubMed] [Google Scholar]
- 5.Yousef N, Mokhtari M, Durand P, et al. Lung ultrasound findings in congenital pulmonary airway malformation. Am J Perinatol. 2018;35(12):1222–1227. doi: 10.1055/s-0038-1645861. [DOI] [PubMed] [Google Scholar]
- 6.Quercia M, Panza R, Calderoni G, Di Mauro A, Laforgia N. Lung ultrasound: a new tool in the management of congenital lung malformation. Am J Perinatol. 2019;36(S02):S99–S105. doi: 10.1055/s-0039-1692131. [DOI] [PubMed] [Google Scholar]
- 7.Rea G, Sperandeo M, DiSerafino M, Vallone G, Tomà P. Neonatal and pediatric thoracic ultrasonography. J Ultrasound. 2019;22(2):121–130. doi: 10.1007/s40477-019-00357-6. [DOI] [PMC free article] [PubMed] [Google Scholar]