Abstract
Background
The COVID-19 pandemic led to large-scale cancellation and deferral of elective surgeries. We quantified volume declines, and subsequent recoveries, across all hospitals in Maryland.
Materials and Methods
Data on elective inpatient surgical volumes were assembled from the Maryland Health Service Cost Review Commission for years 2019-2020. The data covered all hospitals in the state. We compared the volume of elective inpatient surgeries in the second (Q2) and fourth quarters (Q4) of 2020 to those same quarters in 2019. Analysis was stratified by patient, hospital, and service characteristics.
Results
Surgical volumes were 55.8% lower in 2020 Q2 than in 2019 Q2. Differences were largest for orthopedic surgeries (74.3% decline), those on Medicare (61.4%), and in urban hospitals (57.3%). By 2020 Q4, volumes for most service lines were within 15% of volumes in 2019 Q4. Orthopedic surgery remained most affected (44.5% below levels in 2019 Q4) and Plastic Surgery (21.9% lower).
Conclusions
COVID-19 led to large volume declines across hospitals in Maryland followed by a partial recovery. We observed large variability, particularly across service lines. These results can help contextualize case-specific experiences and inform research studying potential health effects of these delays and cancellations.
Keywords: COVID-19, Pandemic, Elective surgery, Surgical deferment
Background
Coronavirus disease 2019 (COVID-19) resulted in elective surgical and procedural suspensions and postponements throughout the United States starting in mid-March 2020.1 According to a recent national survey, a combination of fear of exposure to the virus and providers limiting services resulted in patients delaying or forgoing routine and elective care.2
While it is well known that COVID-19 led to a decline in elective surgical admissions in early 2020,3 new data are needed to show the variability of this decline and subsequent recovery. Using data covering all hospitals within the state of Maryland, we provide a more complete picture of surgical trends during the pandemic and present a relatively robust analysis of the heterogeneity underlying aggregate outcomes.
Specifically, the aims of this study were to utilize data from all hospitals in Maryland to: (1) quantify the impact of the pandemic on the volume of elective, inpatient surgery in the state in 2020 compared to the same period 2019, and (2) identify how volume declines, and subsequent rebounds, differed across patients, services, and hospitals.4 , 5 The answers to these questions can aid health systems and policymakers to understand where foregone care is most concentrated and inform efforts to allocate resources appropriately.
Materials and Methods
We utilized data maintained by the Maryland Health Service Cost Review Commission for adult inpatient admissions in all hospitals (n = 42) in 2019 and 2020. We defined “elective surgery” based on hospital reported variables: the admission type variable with a designation of “elective,” and the service type variable with a designation of “surgery.” Because the data cover all hospitals within the state and include detailed patient and service-level information, they allow us to disentangle where declines were most concentrated. Moreover, because the data cover the entirety of 2020, we can also document where declines were most persistent amid an incomplete recovery.
Specifically, we compared total volume of elective inpatient surgeries in the second (Q2) and fourth quarters (Q4) of 2020 to those same quarters in 2019. Changes through Q2 of 2020 allow us to understand where initial volume reductions were most pronounced, while data from Q4 help illustrate the differential rate of surgical volume recoveries. Analysis was stratified by service line, patient characteristics, and hospital characteristics. We tested whether there were statistically significant differences in the change in surgical volume over time within patient and hospital factors using Chi-squared tests and Poisson regression models. Analysis was conducted using STATA version 15.0 (StataCorp).
Results
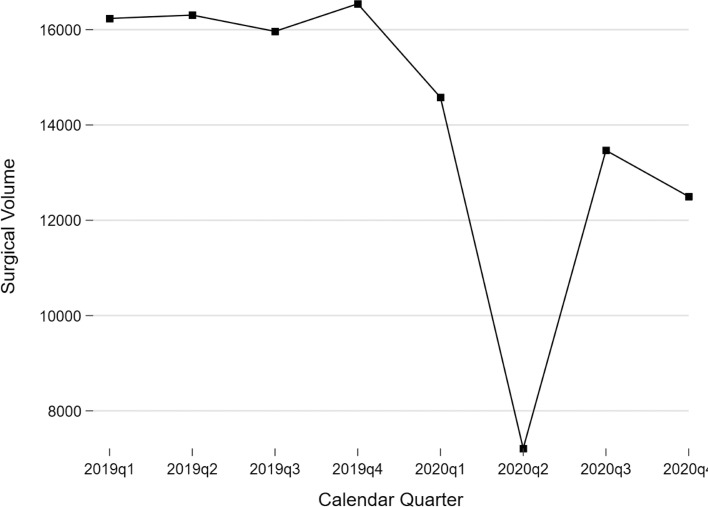
Figure 1 displays elective surgical admissions in 2019 and 2020. Elective surgical admissions declined substantially in 2020 Q2 followed by a partial rebound that stalled in the last quarter of 2020. Across all service lines, we observed a 55.8% decline between 2019 Q2 versus 2020 Q2 (16,306 versus 7,211; 95% CI[-54.5%,-57.0%]) (Table 1 ). Figure 2 shows the percentage change in volumes relative to 2019q4 for the six highest volume departments (for legibility). Orthopedic surgical services were most impacted with a 74.3% decline relative to the same quarter in 2019 (Table 1). Obstetrics and Gynecology was least impacted. Elective surgical volume reductions in 2020 Q2 were greatest for the elderly (≥65), those on Medicare, and those seeking care in urban hospitals. Volumes subsequently increased across all service lines, but to differing degrees. Orthopedic surgery remained most affected, with 2020 Q4 volumes 44.5% below their levels in Q4 of 2019 followed by Plastic Surgery that was 22% lower. Volumes for other service lines were within 15% of levels for the same quarter in 2019.
Fig. 1.
Elective surgery admissions in Maryland, 2019-2020
Note: This figure shows total elective surgical volume from the first quarter of 2019 through the fourth quarter of 2020. Data are from the Maryland Health Service Cost Review Commission CaseMix System.
Table 1.
Elective surgical volume in Maryland hospitals, 2019-2020 Quarter 2 and Quarter 4.
| 2019q2 | 2020q2 | % Change | P-value* | 2019q4 | 2020q4 | % Change | P-value* | |
|---|---|---|---|---|---|---|---|---|
| Total | 16,306 | 7,211 | -55.78% | 16,543 | 12,498 | -24.45% | ||
| Age group | ||||||||
| Non-elderly | 12,055 | 5,439 | -54.88% | ref | 12,288 | 9,185 | -25.25% | ref |
| Elderly (>65) | 4,251 | 1,772 | -58.32% | 0.015* | 4,255 | 3,313 | -22.14% | 0.130 |
| Gender | ||||||||
| Female | 9,994 | 4,571 | -54.26% | ref | 9,799 | 7,554 | -22.91% | ref |
| Male | 6,308 | 2,640 | -58.15% | 0.004* | 6,744 | 4,944 | -26.69% | 0.038* |
| Race/ethnicity | ||||||||
| Non-Hispanic Caucasian | 10,766 | 4,650 | -56.81% | ref | 10,921 | 7,898 | -27.68% | ref |
| African-American | 4,146 | 1,860 | -55.14% | 0.25 | 4,199 | 3,448 | -17.89% | <0.001* |
| Hispanic | 543 | 296 | -45.49% | 0.002* | 559 | 498 | -10.91% | 0.001* |
| Asian | 350 | 162 | -53.71% | 0.474 | 396 | 289 | -27.02% | 0.908 |
| Other | 501 | 243 | -51.50% | 0.148 | 468 | 365 | -22.01% | 0.29 |
| Primary payor | ||||||||
| Commercial | 6,966 | 3,215 | -53.85% | ref | 7,296 | 5,507 | -24.52% | ref |
| Medicare | 6,887 | 2,655 | -61.45% | 0.502 | 6,796 | 4,870 | -28.34% | 0.045* |
| Medicaid | 1,799 | 1,101 | -38.80% | <0.001* | 1,772 | 1,644 | -7.22% | <0.001* |
| Worker's compensation | 103 | 42 | -59.22% | <0.001* | 121 | 70 | -42.15% | 0.079 |
| Other | 551 | 198 | -64.07% | 0.003* | 558 | 407 | -27.06% | 0.612 |
| Hospital size† | ||||||||
| Small | 1,014 | 462 | -54.44% | ref | 1,199 | 865 | -27.86% | ref |
| Medium | 5,125 | 2,324 | -54.65% | 0.938 | 5,169 | 3,456 | -33.14% | 0.126 |
| Large | 10,167 | 4,425 | -56.48% | 0.437 | 10,175 | 8,177 | -19.64% | 0.022* |
| Hospital type | ||||||||
| Academic | 9,694 | 4,487 | -53.71% | ref | 9,814 | 7,466 | -23.93% | ref |
| Non-academic | 6,612 | 2,724 | -58.80% | <0.001* | 6,728 | 5,032 | -25.21% | 0.481 |
| Hospital location | ||||||||
| Urban | 13,426 | 5,728 | -57.34% | ref | 13,582 | 10,312 | -24.08% | ref |
| Rural | 2,880 | 1,483 | -48.51% | <0.001* | 2,960 | 2,186 | -26.15% | 0.373 |
| Service line | ||||||||
| Orthopaedic surgery | 6,378 | 1,637 | -74.33% | ref | 6,408 | 3,556 | -44.51% | ref |
| General surgery | 2,608 | 1,055 | -59.55% | <0.001* | 2,677 | 2,304 | -13.93% | <0.001* |
| Neurosurgery | 810 | 441 | -45.56% | <0.001* | 877 | 781 | -10.95% | <0.001* |
| Cardiothoracic surgery | 1,013 | 554 | -45.31% | <0.001* | 1,032 | 946 | -8.33% | <0.001* |
| Vascular surgery | 903 | 519 | -42.52% | <0.001* | 917 | 872 | -4.91% | <0.001* |
| Obstetrics & gynecology | 865 | 556 | -35.72% | <0.001* | 832 | 799 | -3.97% | <0.001* |
| Urology | 1,208 | 604 | -50.00% | <0.001* | 1,136 | 967 | -14.88% | <0.001* |
| Plastic surgery | 742 | 335 | -54.85% | <0.001* | 797 | 622 | -21.96% | <0.001* |
| Otolaryngology | 206 | 94 | -54.37% | <0.001* | 217 | 200 | -7.83% | <0.001* |
| Other | 1,573 | 1,416 | -9.98% | <0.001* | 1,650 | 1,451 | -12.06% | <0.001* |
Significance at P<0.05.
Fig. 2.
Volume change in elective surgical admissions in Maryland, 2019-2020
Note: This figure shows elective surgical volume for selected high-volume service lines from the first quarter of 2019 through the fourth quarter of 2020. For ease of comparison, volume in each quarter is illustrated as a percent of volume for that service line in the fourth quarter of 2019. Data are from the Maryland Health Service Cost Review Commission CaseMix System.
Conclusion
Our results demonstrate that the COVID-19 pandemic resulted in a significant decline in elective inpatient surgical admissions in Maryland followed by an incomplete recovery through the end of 2020. In part, the attenuation of volume recoveries in 2020 Q4 may reflect the beginnings of the “second wave” of COVID-19 in the UnitedStates These findings are consistent with literature documenting declines in a variety of admission in other settings;4 , 6 but help to quantify both the scale of declines in elective surgery, specifically, and illustrate large heterogeneity in the pandemic's effects across surgical service lines and patient types. While we have focused on summarizing the experience of a relatively large number of hospitals, these data can also provide a benchmark for individual hospitals or health systems to contextualize their experiences through the end of 2020.
These results may indicate development of a substantial surgical backlog, particularly in areas like orthopedic surgery7 , 8 and among certain subpopulations of patients, like the elderly. The elderly and those on Medicare appear to be less willing to return to prepandemic rates of elective surgery, possibly due to the increased risk of death with COVID-19 infection for those over 65. Thus, hospital administrators and decision makers may consider prioritizing these groups by allocating additional health system resources, such as operating room time, when planning surgical recovery efforts. Further, in our study, we noted that patients on Medicaid have had their elective surgical volume in Maryland return the fastest of all insurance types. This may partly be due to increases in Medicaid enrollment in 2020 due to widespread loss of employer-sponsored insurance, or differences in ages of patients between insurance types or differential risk tolerance.9
The relatively exogenous decline in surgical volumes documented here also provides an opportunity for future researchers. In particular, further studies can leverage the variation in delays and/or cancellations across hospitals, service lines, and patients to study whether larger surgical declines are associated with greater deterioration of relevant quality metrics. The answer can help inform ongoing debates about the prevalence (or lack thereof) of low-value surgical care, particularly among fields such as orthopedics which experienced the largest volume decline.
Limitations of the study include our definition of elective surgery was based on administratively assigned variables, as opposed to procedure codes; this was done to avoid bias in assignment of marginally elective procedures. In addition, we are unable to ascertain whether admissions did not occur due to patient election or surgical posting restrictions.
Funding
This project was supported by the Hopkins Business of Health Initiative.
Acknowledgment
Joseph F. Levy, Benedic N. Ippolito, and Kevin Y. Wang performed statistical analysis. All authors wrote the research letter. Amit Jain, Joseph F. Levy and Benedic N. Ippolito, provided the data source, research idea, research outline, and Amit Jain provided supervision of the project. All authors critically reviewed the final work.
Disclosure
None.
Footnotes
All work was performed at the Johns Hopkins University School of Medicine, Department of Orthopaedic Surgery and the Bloomberg School of Public Health.
References
- 1.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M... Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gonzalez D., Karpman M., Kenney G.M., Zuckerman S. Delayed and forgone health care for nonelderly adults during the COVID-19 pandemic. 2021;2020(May 2020).
- 3.McClelland PH., Cheng O., Hu J., et al. Operative shutdown and recovery: restructuring surgical operations during the SARS-CoV-2 pandemic, [published online ahead of print, 2021 Jun 16] J Surg Res. 2021;268:181–189. doi: 10.1016/j.jss.2021.06.009. Alderman Drive, Alpharetta, GA 30005, USA:Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birkmeyer J.D., Barnato A., Birkmeyer N., Bessler R., Skinner J... The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 2020;39:2010–2017. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nepogodiev D., Omar O.M., Glasbey J.C., et al. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baum A., Schwartz M... Admissions to veterans affairs hospitals for 198 emergency conditions during the COVID-19 pandemic. JAMA. 2020;324:96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain A., Jain P., Aggarwal S... SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68. doi: 10.2106/JBJS.20.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salenger R., Etchill E.W., Ad N., et al. The surge after the surge: cardiac surgery post–COVID-19. Ann Thorac Surg. 2020;110:2020–2025. doi: 10.1016/j.athoracsur.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corallo B, Rudowitz R. Analysis of Recent National Trends in Medicaid and CHIP Enrollment. Kaiser Family Foundation. San Francisco, California. https://www.kff.org/coronavirus-covid-19/issue-brief/analysis-of-recent-national-trends-in-medicaid-and-chip-enrollment/.