Abstract
Objective
Despite broad electronic health record (EHR) adoption in U.S. hospitals, there is concern that an “advanced use” digital divide exists between critical access hospitals (CAHs) and non-CAHs. We measured EHR adoption and advanced use over time to analyzed changes in the divide.
Materials and Methods
We used 2008 to 2018 American Hospital Association Information Technology survey data to update national EHR adoption statistics. We stratified EHR adoption by CAH status and measured advanced use for both patient engagement (PE) and clinical data analytics (CDA) domains. We used a linear probability regression for each domain with year-CAH interactions to measure temporal changes in the relationship between CAH status and advanced use.
Results
In 2018, 98.3% of hospitals had adopted EHRs; there were no differences by CAH status. A total of 58.7% and 55.6% of hospitals adopted advanced PE and CDA functions, respectively. In both domains, CAHs were less likely to be advanced users: 46.6% demonstrated advanced use for PE and 32.0% for CDA. Since 2015, the advanced use divide has persisted for PE and widened for CDA.
Discussion
EHR adoption among hospitals is essentially ubiquitous; however, CAHs still lag behind in advanced use functions critical to improving care quality. This may be rooted in different advanced use needs among CAH patients and lack of access to technical expertise.
Conclusions
The advanced use divide prevents CAH patients from benefitting from a fully digitized healthcare system. To close the widening gap in CDA, policymakers should consider partnering with vendors to develop implementation guides and standards for functions like dashboards and high-risk patient identification algorithms to better support CAH adoption.
Keywords: hospitals, EHR adoption, digital divide, critical access hospitals, data analytics
INTRODUCTION
Background and significance
In the 10 years following the Health Information Technology for Economic and Clinical Health (HITECH) Act,1 the goal of ubiquitous use of electronic health records (EHRs) in U.S. acute care hospitals has largely been achieved, with adoption of basic EHRs evenly distributed across various types of hospitals.2,3 While critical access hospitals (CAHs) have not lagged behind in basic EHR adoption,4,5 there was early evidence of an “advanced use” divide in which CAHs were less likely than non-CAHs to have adopted EHR functions that facilitate patient engagement and use electronic data to inform improvement efforts.6 Both patient engagement and clinical data analytics are important domains for hospitals to fully benefit from digitization efforts. Patient engagement tools facilitate efficient communication, improve access, and enable interoperability for care coordination, while clinical data analytics capabilities give hospitals the ability to leverage the data in their EHRs for quality improvement, research, and targeting high-risk patients with care management interventions.7–10 Both domains are integral to broader U.S. health system goals, including payment and delivery reforms and care quality initiatives, many of which are difficult if not impossible to achieve without advanced data analytics and efficient and meaningful engagement with patients. As a result, studying how advanced use adoption has evolved over time and across hospital types is critical for understanding distributional inequities and how policymakers might best support hospitals that lag in advanced EHR use and are less equipped to pursue various health policy goals.
The trajectory of the advanced use divide across CAHs and non-CAHs since the first cross-sectional evidence in 2015 is unclear. As payment and delivery reform models have proliferated, many have exempted (or excluded) CAHs; those that include CAHs—like the Meaningful Use EHR incentive program—often see lower rates of participation among CAHs.11 As a result, CAHs progress more slowly toward these programmatic goals relative to other hospitals, and may require assistance with specific technical prerequisites that non-CAHs find less onerous to adopt. CAH adoption of the requisite technological capabilities are an important indicator of CAH preparedness and barriers. Insight into persistent gaps and the barriers to adoption that cause them can guide finite resources toward the specific information technology (IT) capabilities continuing to hold CAHs back from broader delivery reform goals.
The intervening years since 2015 may have provided CAHs the time needed to make complementary investments and for technology to mature and, in turn, close the divide. In the initial adoption phase, EHRs may have represented such a substantial cost to CAHs that adoption crowded out investment in technical expertise required for advanced use. Non-CAHs may not have had to make this tradeoff, with access to sufficient resources to pursue advanced use in parallel or quick succession. CAHs also may have initially adopted EHRs with the minimum set of features to attest to Meaningful Use (now the Promoting Interoperability program), which did not require or incentivize advanced use functions and threatened many CAHs with financial penalties beginning in 2015 if they did not adopt at least basic systems.11 As those systems have been upgraded over time, functions like risk stratification tools and provider communication via patient portals have become more common from EHR vendors, and thus may have allowed CAHs to catch up to non-CAHs in these functions.
If, however, CAHs were not able to catch up in their adoption and use of advanced EHR functions, a persistent or widening gap suggests that explicit actions may be needed in response. Potential solutions may vary depending on the drivers of the underlying gap. CAHs may be unable to close the advanced use divide due to a lack of technical expertise and resources, which would call for targeted programs like a renewed Regional Extension Center (REC) program to facilitate CAH adoption and use of advanced functions.12 Alternatively, if CAHs have less business need for certain advanced EHR functions, different policy prescriptions would be warranted. For example, on the one hand, if CAHs are less likely to adopt advanced technology due to lack of participation in population-based payment models that incentivize use of those tools,13–15 policymakers will need to modify current programs to include CAHs more readily or develop new payment models tailored to CAHs. On the other hand, if CAH patients simply don’t demand certain advanced functions, different policy goals should be set for CAH technology advancement. Understanding not only the overall gap, but how the gap varies across individual functions, is critical for informing any policy response attempting to close observed gaps. Furthermore, differences in specific functions may tell us whether some appear more challenging than others, signaling whether the gap is rooted in resource availability generally or in particular challenges with more technically complex functions.
OBJECTIVE
In this study, we analyze the most recently available data from the American Hospital Association (AHA) Annual Survey of Hospitals IT Supplement to report measures of EHR adoption in U.S. hospitals and to assess the trajectory of the advanced use divide between CAHs and non-CAHs. We address 3 research questions. First, what is the current level of EHR adoption overall and across CAHs and non-CAHs? Second, have levels of advanced use for patient engagement and for clinical data analytics continued to lag among CAHs compared with non-CAHs? Third, what specific advanced capabilities demonstrate the largest gaps in adoption between CAHs and non-CAHs? We also examine the degree to which factors associated with advanced use across both CAHs and non-CAHs remain independently associated with advanced use among CAHs in particular. This analysis aids in focusing interventions on factors that may facilitate advanced use across hospitals but present distinct challenges for CAHs (ie, those factors associated for all hospitals but not for CAHs). Our findings are critically important for policymakers seeking to understand the long-term impact of the HITECH Act and identify remaining gaps in U.S. hospital IT infrastructure, as well as inform the next steps in policy priorities and incentives to ensure that all provider organizations are able to use a robust set of EHR functionalities.
MATERIALS AND METHODS
Data and sample
The AHA Annual IT Supplement Survey collects information about a wide range of clinical and operational technologies, including EHR adoption and hospital use of EHR data for patient engagement, clinical analytics, and performance improvement, among others. The survey is sent to all U.S. hospitals, and the most appropriate individual, typically the chief executive or a delegate, completes the survey online or by mail, with multiple follow-up mailings and calls aiming to improve response rates. The most recent survey was fielded from December 2018 to March 2019 and received a 64% response rate. We used AHA IT supplement data from 2014 through 2018. We included hospitals who responded at least once, producing an analytic sample consisting of 3643 unique U.S. nonfederal acute care hospitals in an unbalanced panel.
Measures: EHR adoption and advanced EHR use
We defined EHR adoption as either “basic” or “comprehensive,” for comparison with adoption measures in prior literature.6,16 Implementation of 10 specific EHR functions in at least 1 clinical unit in the hospital is considered “basic” EHR adoption, those functions being patient demographics, physician notes, nursing assessments, problem lists, medication lists, medication order entry, diagnostic test results, discharge summaries, and reports from radiology and laboratory. Comprehensive EHR use comprises all basic functions along with 14 additional functions implemented across all clinical units in the hospital. Further details regarding these definitions of EHR adoption have been reported in prior literature.6,16
We determined advanced use across 2 domains: patient engagement and clinical data analytics. To define these functions, we used additional questions regarding hospital IT functions and use from the AHA IT survey that are not components of basic or comprehensive EHR adoption. First, we identified hospitals reporting 10 different EHR functions for patient engagement.6 These functions were patient ability to view electronic data, download that data, send electronic versions of their health information, request that data in their medical record be changed, request prescription refills online, schedule appointments online, pay bills online, submit patient-generated health data to their medical record, message providers via secure messaging tools, and designate which caregivers or family members could access their medical record. A hospital reporting at least 8 of these was considered an “advanced user” in patient engagement.6
Second, we identified hospitals reporting 10 different EHR functions pertinent to clinical data analytics.6 These functions were organizational performance dashboards, unit-level dashboards, individual user performance dashboards, query tools for clinicians, measuring clinical guideline adherence, identifying care gaps for different patient populations, informing strategic planning with reports generated from the EHR, using data to support continuous process improvement efforts, monitoring patient safety, and stratifying patients as high risk to facilitate follow-up care. Hospitals reporting at least 8 of these were considered “advanced users” in the clinical data analytics domain. Both measures of advanced EHR use became available in the data starting in 2014. For both measures, the specific functions included and the thresholds are consistent with the prior cross-sectional study on the advanced use divide.6
Measures: Hospital characteristics
Our primary independent variable of interest was CAH status, a binary indicator for whether or not a hospital was recognized as a CAH. To stratify hospitals and adjust for observable factors, we included several hospital characteristics in our analysis of the advanced use divide. We measured hospital size by number of beds, with hospitals with over 400 beds categorized as large, between 100 and 400 beds as medium-sized, and fewer than 100 beds as small. Hospital ownership was categorized as private nonprofit, private for profit, or owned by a local government entity. We did not include federally owned or specialty hospitals in our sample. We also captured measures of teaching status, membership in a health care system, participation in accountable care organizations (ACOs), patient-centered medical homes, or bundled payment programs, location in an urban or rural setting, and U.S. Census region.
Analytic approach
To answer our first research question, we measured the proportion of all hospitals reporting basic and comprehensive EHR adoption from 2008 to 2018, then compared the proportion of EHR adoption, as well as the proportion of hospitals who had adopted at least 8 patient engagement and clinical data analytics advanced EHR use functions, between CAHs and non-CAHs from 2014, the first year of data availability for those measures, through 2018. To answer our second research question, we calculated the raw percentage point difference between CAH non-CAH hospitals in each year 2014 through 2018 for adoption of advanced patient engagement, clinical data analytics, and at least basic EHR adoption, with 2-sided t tests with unequal variances to test for statistically significant differences in each year. We then ran a multivariable ordinary least squares linear probability model for each of the 2 dichotomous advanced use measures as dependent variables to determine the difference in probability of adoption between CAHs and non-CAHs, holding potential observed confounders constant. Hospital characteristics included basic and comprehensive EHR adoption, size, ownership, teaching status, location, region, and year fixed effects; standard errors were clustered at the hospital level. An interaction term between CAH status and year captured the change in the relationship between CAH status and our advanced use outcomes over time. Finally, to answer our third research question, we compared each of the 10 patient engagement and clinical data analytics functions between CAH and non-CAH hospitals as of 2018, using chi-square tests for statistical significance. To shed light on the barriers and facilitators CAHs may face in adopting advanced use functions and to better target interventions, we also analyzed factors associated with advanced EHR use among CAHs. We ran the same multivariate ordinary least squares linear probability model for both outcomes, limiting the sample to CAHs in 2018. All models used weights generated by an inverse probability model to account for nonresponse bias and create nationally representative estimates for each year. The model predicted survey response based on hospital size, teaching status, system membership, location in a rural or urban area, ownership, availability of a cardiac intensive care unit, and region.
RESULTS
EHR adoption
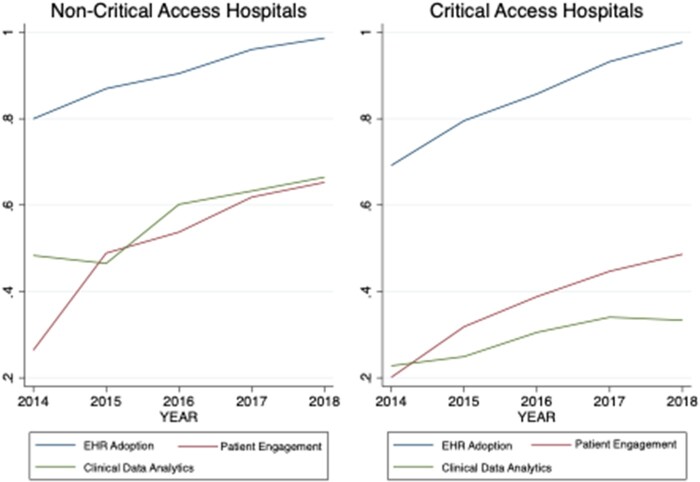
In 2018, 98.3% of hospitals had adopted either a basic or comprehensive EHR, up from 75.2% in 2014 (Supplementary Figure 1). There were no differences in EHR adoption rates across CAH and non-CAH hospitals in 2018, with 97.8% of CAHs and 98.4% of non-CAHs having adopted at least a basic EHR (Figure 1). In our analysis of the 2 domains of advanced EHR use, 58.7% of all hospitals had adopted at least 8 of 10 patient engagement functions in 2018 and 55.6% of all hospitals had adopted at least 8 of 10 clinical data analytics functions.
Figure 1.
Electronic health record (EHR) adoption and advanced EHR functions by critical access status. Plots show adoption of EHRs, patient engagement functions, and clinical data analytics functions over time for critical access hospitals and noncritical access hospitals. The differences between these lines are plotted in Figure 2. Data Source: Authors’ analysis of the American Hospital Association Annual Survey IT Supplement.
Comparing CAHs and non-CAHs
Descriptively, CAHs differed from non-CAHs across several characteristics beyond the expected differences in size and rurality. CAHs were less likely to have adopted a comprehensive EHR, were more likely to be publicly owned, and were more commonly located in the Midwest (Table 1). CAHs reported lower levels of advanced EHR use than non-CAHs in all time periods (Figure 1). From 2014 to 2018, advanced EHR use for patient engagement grew from 24.4% to 63.3% of non-CAHs (38.9 percentage points; 159%) and from 19.1% to 46.6% (27.5 percentage points; 169%) of CAHs. Advanced use for clinical data analytics grew from 47.4% to 64.5% (17.1 percentage points; 36%) of non-CAHs, and from 22.6% to 32.0% of CAHs (9.4 percentage points; 42%).
Table 1.
Descriptive statistics, U.S. nonfederal acute care hospitals (N = 13 040 Hospital-Year Observations)
| Hospital Descriptive Statistics 2014-2018 |
Overall |
CAHs |
Non-CAHs |
|||
|---|---|---|---|---|---|---|
| n (Hospital-Year Observations) | % | n (Hospital-Year Observations) | % | n (Hospital-Year Observations) | % | |
| Less than basic EHR | 1418 | 10.9 | 497 | 14.9 | 921 | 9.5 |
| Basic EHR | 4841 | 37.1 | 1552 | 46.6 | 3289 | 33.9 |
| Comprehensive EHR | 6781 | 52.0 | 1280 | 38.4 | 5501 | 56.6 |
| Critical access hospital | 3329 | 25.5 | 3329 | 100 | 0 | 0 |
| Size small (fewer than 100 beds) | 5678 | 43.5 | 3156 | 94.8 | 2522 | 26.0 |
| Size medium (100-399 beds) | 5598 | 42.9 | 172 | 5.2 | 5426 | 55.9 |
| Size Large (400+ beds) | 1764 | 13.5 | 1 | 0.0 | 1763 | 18.2 |
| Private, nonprofit | 8602 | 66.0 | 1830 | 55.0 | 6772 | 69.7 |
| Private, for profit | 1648 | 12.6 | 100 | 3.0 | 1548 | 15.9 |
| Public, nonfederal | 2790 | 21.4 | 1399 | 42.0 | 1391 | 14.3 |
| Teaching hospital | 4746 | 36.4 | 118 | 3.5 | 4628 | 47.7 |
| Urban | 8113 | 62.2 | 640 | 19.2 | 7473 | 77.0 |
| Region: West | 2204 | 16.9 | 606 | 18.2 | 1598 | 16.5 |
| Region: Midwest | 4502 | 34.5 | 1831 | 55.0 | 2671 | 27.5 |
| Region: South | 4540 | 34.8 | 714 | 21.4 | 3826 | 39.4 |
| Region: Northeast | 1792 | 13.7 | 178 | 5.3 | 1614 | 16.6 |
CAH: critical access hospital; EHR: electronic health record.
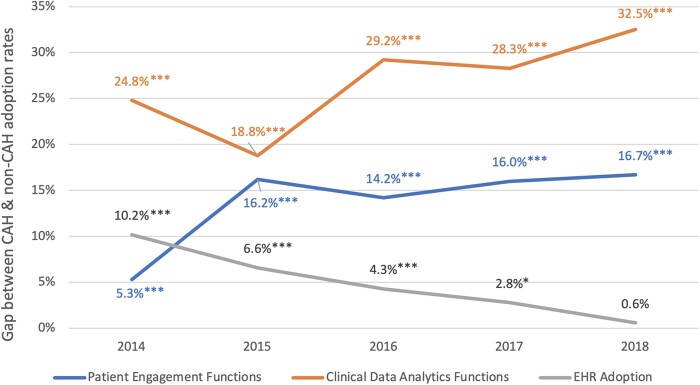
The adoption gap between non-CAHs and CAHs grew from 5.3% to 16.7% for advanced patient engagement, and from 24.8% to 32.5% for clinical data analytics. In contrast, over the same period, the gap between non-CAHs and CAHs narrowed for at least basic EHR adoption, dropping from 10.2% in 2014 to 0.6% in 2018 (Figure 2). We found similar results in multivariable models, with the gap in patient engagement persisted throughout the study period (B2018 = -0.09, P < .001) (Supplementary Table 1), while the gap in clinical data analytics grew larger (B2018 = -0.05, P = .03) (Supplementary Table 2). In model specifications with outcome variables as counts 0 to 10 for 2018 only, CAHs had adopted fewer clinical data analytics functions than non-CAHs (Supplementary Table 3).
Figure 2.
Gap between critical access hospital (CAH) and non-CAH electronic health record (EHR) and advanced functionality adoption over time. The plot shows the difference between CAH and non-CAH adoption rates of EHRs (gray), patient engagement functions (blue), and clinical data analytics functions (orange) over time. Stars indicate statistical significance of adoption gap between CAHs and non-CAHs from 2-sided t tests with unequal variances. *P < .05; **P < .01; ***P < .001. Data Source: Authors’ analysis of the American Hospital Association Annual Survey IT Supplement.
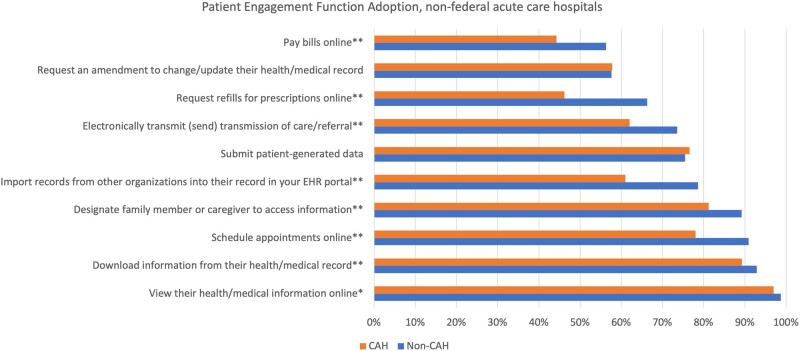
The individual functions comprising our measures of advanced EHR use demonstrated wide variation in adoption levels, with many exhibiting gaps between CAHs and non-CAHs (Figures 3 and 4 and Supplementary Table 4). In patient engagement, 2 functions had low adoption for both CAHs and non-CAHs: paying bills online and requesting amendments to change or update medical records (both <60%). Three functions demonstrated high non-CAH adoption and low CAH adoption: allowing online refill requests (CAHs 46.2% vs non-CAHs 66.3%; P < .01); importing records from other organizations (61.0% vs 78.6%; P < .01); and sending electronic care summaries to third parties (62.0% vs 73.6%; P < .01). The remaining functions in this domain had >75% adoption across hospital types, but CAHs still had lower rates of adoption than non-CAHs. All patient engagement functions except requesting changes to the medical record and submission of patient-generated data demonstrated statistically significant differences across CAHs and non-CAHs.
Figure 3.
Patient engagement functions adoption, critical access hospitals (CAHs) and non-CAHs in 2018. The plot shows the difference between CAH (orange) and non-CAH (blue) adoption rates of individual patient engagement functions as of 2018. Stars indicate statistical significance of adoption gap between CAHs and non-CAHs from chi-square tests. Rates of adoption for CAHs and non-CAHs are reported in Supplementary Table 4. *P < .05; **P < .01; ***P < .001. Data Source: Authors’ analysis of the American Hospital Association Annual Survey IT Supplement. EHR: electronic health record.
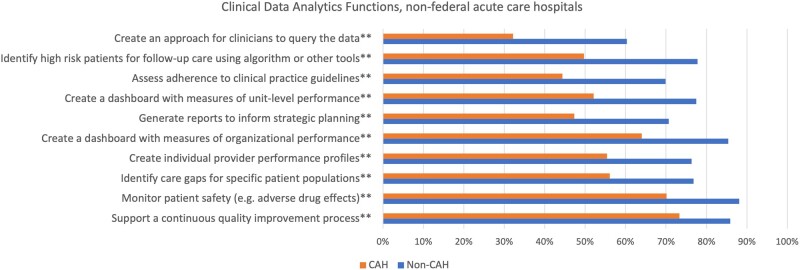
Figure 4.
Clinical data analytics functions adoption, critical access hospitals (CAHs) and non-CAHs in 2018. The plot shows the difference between CAH (orange) and non-CAH (blue) adoption rates of individual clinical data analytics functions as of 2018. Stars indicate statistical significance of adoption gap between CAHs and non-CAHs from chi-square tests. Rates of adoption for CAHs and non-CAHs are reported in Supplementary Table 4. *P < .05; **P < .01; ***P < .001. Data Source: Authors’ analysis of the American Hospital Association Annual Survey IT Supplement.
In clinical data analytics, non-CAHs had adoption rates over 60% for all 10 functions—only 3 functions had CAH adoption >60%: dashboards for organizational performance (64.0%), monitoring patient safety (70.1%), and supporting a continuous quality improvement process (73.3%). In addition to low overall adoption rates among CAHs, 4 functions demonstrated adoption gaps in 2018 >25 percentage points: allowing clinicians to query EHR data (32.2% vs 60.3%; P < .01), identifying high-risk patients via algorithm for follow-up (49.7% vs 77.8%; P < .01), assessing clinical guideline adherence (44.4% vs 69.9%; P < .01), and creating dashboards with unit-level performance (52.2% vs 77.5%; P < .01). All 10 clinical data analytics functions demonstrated statistically significant differences in adoption rates across CAHs and non-CAHs.
Factors associated with advanced EHR use among CAHs
Among CAHs, certain characteristics were associated with adoption of both advanced use domains. Teaching status and system membership were positively associated with adoption of both patient engagement and clinical data analytics (P < .001 for both) (Supplementary Table 5). Participation in bundled payment programs and medical homes were positively associated with advanced use of clinical data analytics and patient engagement, respectively (P < .001 for both) (Supplementary Table 5). ACO participation was not associated with CAH adoption of either advanced use domain. However, this null estimate is likely to be attributable in part to small sample sizes that are underpowered to detect associations in the presence of low ACO participation rates among CAHs at baseline.
DISCUSSION
Basic EHR adoption among nonfederal acute care hospitals in the United States is essentially ubiquitous: fewer than 2% of hospitals lacked an EHR as of 2018. While our measure of basic EHR adoption2,6,16,17 understates hospitals’ progress toward EHR adoption prior to HITECH,18 the end result is that nearly all U.S. acute care hospitals have adopted at least a basic EHR system, including CAHs. Less than a decade after the passage of the HITECH Act, the digitization of U.S. acute care hospitals is largely complete, a testament to ongoing hospital digitization efforts, the incentives of the HITECH Act, and continued focus from policymakers.2 As EHR adoption has become universal, the need to measure hospital use of advanced EHR functions that go beyond the digitization of clinical data to deliver value to patients and clinicians grows increasingly important. Our measures of advanced EHR use in the domains of patient engagement and clinical data analytics show lower levels of adoption than basic EHRs, with slightly over half of our sample reporting that they had adopted at least 8 functionalities in each domain. A delay between basic EHR adoption and advanced use is expected as systems mature, although there are no normative standards for how long it should take a hospital to progress through different stages of technological sophistication. Hospitals likely vary widely in both desire and ability to implement advanced functions after initial EHR adoption, owing to organizational culture and appetite for change, financial resources and access to capital, technological expertise, and complementary expertise, among other factors.13,19,20 Still, both advanced use measures have increased since 2014, when 22.9% of hospitals reported at least 8 of 10 patient engagement functions and 40.8% of hospitals reported at least 8 of 10 clinical data analytics functions.6 Our findings also reveal that advanced EHR use in both domains has consistently lagged behind for CAHs compared with non-CAHs, and advanced use adoption has demonstrated wider and more persistent gaps than EHR adoption among CAHs. This may be explained by specific features of the HITECH Act. In addition to direct financial incentives for EHR adoption and use of basic functions, the HITECH Act included other provisions intended to support less-resourced hospitals. For example, 62 RECs were established in 2010 throughout the United States to support EHR adoption among primary care practices and to provide implementation and adoption support to CAHs.12 These additional supports were largely focused on assisting hospitals adoption of new EHRs, rather than on optimizing or improving existing systems. While REC funding was miniscule compared with incentive payments for EHR adoption,18 RECs were explicitly aimed at supporting hospitals like CAHs facing additional barriers to EHR adoption. However, they were not designed or funded to help these hospitals customize and advance their EHR use beyond basic functionalities.
The different magnitude of adoption gap across specific advanced functions provides further insight into the potential drivers. Enabling certain patient engagement functions may not be high priority for CAHs due to readily available analog substitutes. For example, 3 of the 4 functions with the largest gap between CAHs and non-CAHs (online prescription refills, appointment scheduling, and bill pay) are largely addressable over the phone. In contrast, CAHs prioritized investment in novel digital functions including downloading patient information from the portal, which demonstrates high adoption (89.3% of CAHs), likely due to mandates in Meaningful Use and Promoting Interoperability. CAHs were less likely to have adopted patient engagement functions that relied on outside organizations. For example, importing records from other organizations and sending referral summaries to third parties both demonstrate lower CAH adoption (61.0% and 62.0%, respectively), compared with viewing information online (97.0% of CAHs), which only requires IT capability internal to the CAH. This suggests that CAHs may struggle with the expensive task of building connectivity to other healthcare delivery organizations. It may also be possible that CAHs, often located in rural areas, see less value in building information exchange functions if their patient population is less likely to receive care from other providers.
In the clinical data analytics domain, mechanisms underlying differential levels of adoption of individual functions are less clear, owing to more uniform gaps and low overall adoption among CAHs. Eight of the 10 functions for this measure demonstrate 20-percentage-point gaps between CAHs and non-CAHs, equal to the single largest gap in patient engagement functions. Generally, workforce capacity constraints and access to technical expertise may underpin low CAH adoption of clinical data analytics functions. A number of these functions demand substantial time investment from clinicians initially to implement and subsequently to maintain, for example, approaches for clinicians to query the EHR and assessing clinical guideline adherence. These implementation efforts may strain the clinical workforce of CAHs. Other functions like identifying high-risk patients for follow-up care and identifying care gaps require less direct clinical engagement in implementation but need both technical expertise to implement algorithms and support staff like care managers to manage these population health tools. Regardless of what is driving these gaps, they are problematic, as they have implications for patient care. Specifically, without the tools to measure quality, stratify patient populations, and more generally leverage clinical data from EHRs for organizational priorities, CAHs will likely struggle with undertaking and tracking quality improvement efforts, as these capabilities are prerequisites to many quality improvement and population health goals.
Implications for policy and practice
Closing the gap between CAHs and non-CAH adoption of advanced EHR functions should be a priority for policymakers, targeting clinical data analytics functions. It may be appropriate to allocate resources similar to the RECs to promote advanced EHR use among hospitals less equipped to pursue these functions independently. Given that within CAHs, we found those that are members of a health care system—which frequently comes with additional resources such as IT support staff—were more likely to have both patient engagement and clinical data analytics functions, providing these types of resources and support may be key to speeding CAH advanced EHR use. These efforts could involve targeted financial and technical support from federal and state organizations along with sharing of best practices, specifically from hospitals in the region with which the CAH shares a substantial number of patients. Furthermore, federal regulators should consider developing implementation standards and partner with EHR vendors to create resources on best practices and common uses for analytics functions. Development and dissemination of templates for building dashboards, high-risk patient identification algorithms, and clinician data querying tools would be of particular value, as CAHs trail far behind non-CAHs in these functions. This would help to close the advanced use divide, and support CAHs in their own internal quality improvement efforts and participation in delivery reform programs.
Existing efforts to encourage adoption of technical standards to enable interoperability are likely to increase CAHs’ growth in patient engagement functions that involve outside organizations. While the enforcement dates for providers to adopt standard application programming interfaces (APIs) for patient access to data have been pushed back due to the COVID-19 (coronavirus disease 2019) pandemic,21 rural providers may be poised to use these technologies, as 40% of rural hospitals and CAHs had adopted APIs by 2017, compared with 32% of non-CAHs.22 Given that interoperability-based patient engagement functions are driving part of the advanced use divide, the 21st Century Cures Act Final Rule mandating the exchange of standard data elements via APIs should not be further delayed. While these mandates may help close the gap in patient engagement functions, these are unlikely to be enough for some CAHs, so technical outreach efforts should focus on CAHs that have struggled to adopt APIs to date.
Limitations
Our study has a number of limitations. First, differences in how measures of EHR adoption are constructed can lead to different estimates. For consistency with past studies, we used an established measure of EHR adoption, though more flexible measures that accurately reflect hospitals’ technological sophistication are needed going forward. To this end, our measures of advanced EHR use only required hospitals adopt any 8 of the 10 functions included in each domain. This allows for more combinations of functions to be counted as “advanced use,” and gives hospitals credit for prioritizing more strategically important advanced functions in lieu of others that may have substitutes. Moreover, we found similar results when running regression models that allowed for even more flexibility in adoption, with the number of advanced use functions adopted (0-10) as the outcome (Supplementary Table 4). Second, while we focus on 2 broadly important domains of advanced EHR use, we were unable to measure some factors that may be related to advanced EHR use in these 2 domains. For example, it may be that some hospitals have chosen to focus on other EHR projects not measured in our dependent variables, such as improving usability for clinicians23 or other functionalities not captured in the AHA IT supplement. Also, the survey instrument does not capture usability differences for each functionality across EHR vendors or hospitals, which may in turn play a role in adoption. Third, our study is also limited in that the AHA Survey and IT Supplement are self-reported surveys that are subject to both social desirability bias and nonresponse bias. However survey items have shown good reliability and we weighted our analyses to adjust for nonresponse bias, allowing for generalizable estimates.24 Finally, our analyses are descriptive, and we cannot determine if CAH status is causally related to less advanced EHR use. However, our results describe an important gap that should be addressed by policymakers regardless of the causal mechanism.
CONCLUSION
While EHR adoption has reached parity at a high level across U.S. acute care hospitals, the advanced use divide in advanced use among CAHs and non-CAHs has not been diminished in recent years. CAHs continue to lag in patient engagement functions, and have fallen further behind in clinical data analytics. These functions underpin many quality improvement and population health efforts, and may prevent patients who receive care at CAHs from benefitting from a fully digitized health care system. Policymakers should develop programs that can provide technical expertise and consider implementation standards for advanced analytics functions in order to help CAHs catch up in these advanced EHR uses.
FUNDING
This study had no direct funding. NCA was supported by the Agency for Healthcare Research and Quality under award T32HS026116.
AUTHOR CONTRIBUTIONS
All authors conceptualized and designed the study. NCA drafted the manuscript and provided critical feedback and edits. AJH drafted the manuscript, conducted data analysis, and built all figures and tables. JAM drafted the manuscript and advised on study design.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
DATA AVAILABILITY STATEMENT
The data underlying this article were provided by the American Hospital Association under license to Wharton Research Data Services. Data must be licensed from the American Hospital Association for access.
CONFLICT OF INTEREST STATEMENT
None.
Supplementary Material
REFERENCES
- 1.Blumenthal D.Launching HITECH. N Engl J Med 2010; 362: 382–5. [DOI] [PubMed] [Google Scholar]
- 2.Adler-Milstein J, Jha AK.. HITECH Act drove large gains in hospital electronic health record adoption. Health Aff (Millwood) 2017; 36 (8): 1416–22. [DOI] [PubMed] [Google Scholar]
- 3.Office of the National Coordinator for Health Information Technology. Non-federal Acute Care Hospital Electronic Health Record Adoption. 2017. https://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php. Accessed February 5, 2021.
- 4.DesRoches CM, Worzala C, Joshi MS, et al. Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood) 2012; 31: 1092–9. [DOI] [PubMed] [Google Scholar]
- 5.Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood) 2014; 33: 1664–71. [DOI] [PubMed] [Google Scholar]
- 6.Adler-Milstein J, Holmgren AJ, Kralovec P, et al. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc 2017; 24 (6): 1142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Persell SD, Kaiser D, Dolan NC, et al. Changes in performance after implementation of a multifaceted electronic-health-record-based quality improvement system. Med Care 2011; 49 (2): 117–25. [DOI] [PubMed] [Google Scholar]
- 8.Persell SD, Lloyd-Jones DM, Friesema EM, et al. Electronic health record-based patient identification and individualized mailed outreach for primary cardiovascular disease prevention: a cluster randomized trial. J Gen Intern Med 2013; 28 (4): 554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irizarry T, DeVito Dabbs A, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17: e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Irizarry T, Shoemake J, Nilsen ML, et al. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res 2017; 19 (3): e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DesRoches CM, Worzala C, Bates S.. Some hospitals are falling behind in meeting ‘Meaningful Use’ criteria and could be vulnerable to penalties in 2015. Health Aff (Millwood) 2013; 32: 1355–60. [DOI] [PubMed] [Google Scholar]
- 12.Lynch K, Kendall M, Shanks K, et al. The Health IT Regional Extension Center Program: evolution and lessons for health care transformation. Health Serv Res 2014; 49: 421–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabriel MH, Jones EB, Samy L, et al. Progress and challenges: implementation and use of health information technology among critical-access hospitals. Health Aff (Millwood) 2014; 33: 1262–70. [DOI] [PubMed] [Google Scholar]
- 14.Lin SC, Hollingsworth JM, Adler-Milstein J.. Alternative payment models and hospital engagement in health information exchange. Am J Manag Care 2019; 25: e1–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher ES, McClellan MB, Bertko J, et al. Fostering accountable health care: moving forward in Medicare. Health Aff (Millwood) 2009; 28: w219–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med 2009; 360: 1628–38. [DOI] [PubMed] [Google Scholar]
- 17.Henry J, Pylypchuk Y, Searcy T, et al. Adoption of electronic health record systems among US non-federal acute care hospitals: 2008-2015. ONC Data Brief 2016; 35: 1–9. [Google Scholar]
- 18.Everson J, Rubin JC, Friedman CP.. Reconsidering hospital EHR adoption at the dawn of HITECH: implications of the reported 9% adoption of a “basic” EHR. J Am Med Inform Assoc 2020; 27: 1198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dranove D, Forman C, Goldfarb A, et al. The Trillion Dollar Conundrum: complementarities and health information technology. Am Econ J Econ Policy 2014; 6 (4): 239–70. [Google Scholar]
- 20.McCullough J, Casey M, Moscovice I, et al. Meaningful use of health information technology by rural hospitals. J Rural Health 2011; 27: 329–37. [DOI] [PubMed] [Google Scholar]
- 21.Landi H. Enforcement of interoperability rules to be relaxed to ease burden on providers. Fierce Healthcare. 2020. https://www.fiercehealthcare.com/tech/hhs-will-relax-enforcement-interoperability-rules-to-ease-burden-providers. Accessed February 5, 2021.
- 22.Holmgren AJ, Apathy NC.. Hospital adoption of API-enabled patient data access. Health (Amst) 2019; 7 (4): 100377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hettinger AZ, Melnick ER, Ratwani RM.. Advancing electronic health record vendor usability maturity: progress and next steps. J Am Med Inform Assoc 2021; 28 (5): 1029–31. doi:10.1093/jamia/ocaa329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Everson J, Lee S-YD, Friedman CP.. Reliability and validity of the American Hospital Association’s national longitudinal survey of health information technology adoption. J Am Med Inform Assoc 2014; 21: e257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by the American Hospital Association under license to Wharton Research Data Services. Data must be licensed from the American Hospital Association for access.