Abstract
Objective
Where people with systemic sclerosis (SSc) (or scleroderma) obtain diet and nutrition information to manage their disease is not known. Objectives were to identify 1) resources used by people with SSc for nutrition and diet information and 2) perceived advantages and disadvantages of resources.
Methods
We conducted nominal group technique (NGT) sessions in which people with SSc reported nutrition and diet information resources they have used and perceived advantages and disadvantages of accessing and using resources. Participants indicated whether they had tried each resource. They rated helpfulness and importance of possible advantages and disadvantages. Items elicited across sessions were merged to eliminate overlap.
Results
We conducted four NGT sessions (three English language, one French language; 15 total participants) and identified 33 unique information resources, 147 resource‐specific advantages, and 118 resource‐specific disadvantages. Resource categories included health care providers, alternative and complementary practitioners, websites and other media platforms, events, and print materials. The most common themes for advantages and disadvantages included quality and individualization of information and accessibility of resources in terms of cost, location, and comprehensibility. Information provided by medical professionals was regarded as most credible and can be obtained through books, articles, and websites if individual consultation is not easily accessible. Web‐based information was considered highly accessible, although of variable credibility. In‐person events may be an important source of health information for people with SSc.
Conclusion
People with SSc obtain nutrition and diet information from multiple resources. They seek credible and accessible resources that provide SSc‐specific and individualized information.
INTRODUCTION
Systemic sclerosis (SSc) (or scleroderma) is a rare autoimmune connective tissue disease, characterized by vascular injury, immune dysfunction, and abnormal fibrotic processes, that can affect multiple organ systems, including the skin, lungs, gastrointestinal tract, and cardiovascular system (1). Gastrointestinal manifestations, which affect nearly 90% of people with SSc (2), may include microstomia, xerostomia, dental disease, dysphagia, odynophagia, dysmotility, gastroesophageal reflux disease, gastroparesis, gastric antral vascular ectasia, small intestinal bacterial overgrowth, chronic intestinal pseudo‐obstruction, diarrhea, constipation, and fecal incontinence (3). Gastrointestinal manifestations can lead to malabsorption, moderate to severe malnutrition, and weight loss (4) and are associated with reduced health‐related quality of life and mortality, especially in cases of severe dysmotility (2, 4).
Several clinical practice reviews and treatment guidelines recommend dietary modifications to manage SSc gastrointestinal concerns (5, 6, 7, 8), but implementation may be complicated by significant heterogeneity in gastrointestinal symptoms among patients with SSc (3). In addition, optimal management strategies may differ on the basis of other SSc manifestations or social determinants of health (eg, food insecurity, social support) (3). No well‐designed and conducted trials have evaluated effects of dietary modifications in SSc (9). In this context, people with SSc may seek nutrition and diet information and strategies for managing gastrointestinal symptoms from a variety of sources. Little is known, however, about the sources of information they use and perceived advantages and disadvantages of different resources.
The present study is the first step of the Scleroderma Patient‐Centered Intervention Network (SPIN) Diet and Nutrition (DINE) project. The SPIN‐DINE project aims to identify and address existing information gaps, with the long‐term goal of providing tools for people with SSc to find and access evidence‐based information and guidance on nutrition and diet. The objectives of the present study were to identify 1) resources used by people with SSc to obtain information on nutrition and diet and 2) perceived advantages and disadvantages of accessing and using different resources. The results will inform the next step of the SPIN‐DINE project, which is the development of a survey to be administered to the SPIN Cohort, a large multinational SSc patient cohort (10).
MATERIALS AND METHODS
This was a cross‐sectional study that used the nominal group technique (NGT) method (11). The study was approved by the Research Ethics Committee of the Center Intégré Universitaire de Santé et de Services Sociaux du Center‐Ouest‐de‐l'Île‐de‐Montréal (#2020‐2051). It is reported per the Consolidated Criteria for Reporting Qualitative Research checklist (12).
Participant eligibility and recruitment
We attempted to recruit up to eight participants for each NGT session. Eligible participants had SSc and were aged 18 years and older, fluent in English or French, and able to participate in a videoconference‐based session. We recruited participants through an announcement to participants in the SPIN Cohort, a large international SSc cohort (10, 13), and via social media posts (Facebook and Twitter) from SPIN and partner patient organizations.
Interested participants contacted the study coordinator by email. The coordinator confirmed eligibility, provided study information, and answered any questions, also by email. Potential participants logged into a Qualtrics online survey; there, they could provide informed consent or decline to participate, indicate scheduling availabilities, and complete study questionnaires.
Measures
Participants reported their sex, race/ethnicity, relationship status, education level, and occupational status, as well as SSc subtype, years since SSc diagnosis, and currently experienced gastrointestinal symptoms from a list of common SSc symptoms (diarrhea, constipation, acid reflux, heartburn, nausea, abdominal pain, dysphagia, regurgitation) (14, 15, 16), with an option to input additional symptoms they experienced. They also completed the University of California, Los Angeles Scleroderma Clinical Trial Consortium Gastrointestinal Tract 2.0 (UCLA SCTC GIT 2.0) instrument (16) and the Malnutrition Screening Tool (MST) (17). The UCLA SCTC GIT 2.0 characterizes SSc gastrointestinal tract involvement. It consists of seven multiitem scales (reflux, distention/bloating, fecal soilage, emotional well‐being, social functioning, diarrhea, and constipation). A total score (0.00‐2.83) reflects overall severity, a higher score indicating more severe gastrointestinal involvement (16). The MST is a two‐item screening tool that assesses unintentional weight loss and decreased appetite. It is used to identify adults at risk of malnutrition (MST score of <2, not at risk; ≥2, at risk) (18, 19).
NGT sessions
The NGT method was designed to structure group discussions to share experiences and reach consensus (20). It is used to generate survey or questionnaire items directly from stakeholders, including in SSc (21, 22). The NGT method typically structures small group discussions according to four sequential steps: 1) silent generation of ideas in writing, 2) round‐robin sharing of ideas, 3) discussion, and 4) rating or ranking.
We conducted 90‐ to 120‐minute videoconference NGT sessions via GoToMeeting. Several days prior to their session, participants were sent the first question (“What resources have you used to get nutrition information or advice to manage gastrointestinal issues or other symptoms related to SSc, or to maintain good nutritional status?”) via email with a Qualtrics link to list resources. We subsequently emailed participants their lists to share during their session.
We adapted an NGT topic guide (see Supplementary Methods) from a previous NGT study (22) and pilot tested it with SPIN personnel prior to the first session. Sessions were moderated by four investigators with experience in interview‐based research. A master’s student (SH) and an undergraduate student (NØ) moderated the English‐language sessions. An experienced research associate (M‐EC) and a research assistant (AB) moderated the French‐language session. The number of sessions was determined on the basis of data redundancy and consistency. There were three English‐language sessions and one French‐language session. The second and third English‐language sessions built on items generated in the earlier English‐language session.
Protocols for first English‐language session and French‐language session
After instructions were provided, participants shared items from their preprepared resources list in a round‐robin format until all items were shared. Participants were instructed to avoid repetition of items provided by others but to share items that differed, even if minimally. They were encouraged to add any items that came to mind during the process. As necessary, moderators used probes to gain a clearer understanding of items. As items were shared, they were simultaneously recorded and screen shared with participants. Once all resources were shared, moderators led a discussion among participants to review items, edit unclear items, remove or merge overlapping items, and separate single items with multiple components into more than one item. Items were revised on the basis of group feedback until there was consensus.
Next, participants were presented with the second research question: “Reflect on your own personal experience with using, attempting to use, or thinking about using these resources. For each resource in the list, what do you think are the advantages and disadvantages of using and accessing each resource?” Participants silently and independently recorded (on paper or via word processing program) perceived advantages and disadvantages, then shared them resource by resource, using the same procedure as with the first question.
As each group developed its list of resources, advantages, and disadvantages, the list was transferred into a Qualtrics survey. At the end of the session, the survey was emailed to participants, who responded by indicating if they had ever used each resource, rating the perceived helpfulness of each resource on an 11‐point Likert scale from 0 (not at all helpful) to 10 (extremely helpful), and rating each advantage and disadvantage from 0 (not at all important) to 10 (extremely important).
NGT protocol for second and third English sessions
The length of the first English NGT session surpassed our planned 90‐minute duration, so we altered the protocol for subsequent sessions to reduce duration and participant burden. Thus, in the subsequent English‐language sessions, investigators identified overlapping items from previous sessions initially and only solicited new, nonoverlapping items during round‐robin sharing. To facilitate this, prior to the second and third English‐language sessions, investigators compared resources generated in prior session(s) with those newly submitted and created a table with, separately, 1) potentially redundant resources and 2) newly submitted novel resources. For each potentially redundant resource, participants were asked 1) if the newly submitted resource was adequately captured by the previous version, 2) if the previous version needed editing to capture all aspects of the newly submitted version, or 3) if the newly submitted resource was not redundant and should be considered separately. Each newly submitted novel resource was considered one by one by using discussion and consensus to edit unclear resources, remove or merge overlapping resources, and separate multicomponent items.
Next, for resources in the redundant list, participants were shown advantages and disadvantages from the previous session(s) and were prompted to generate any additional, substantively different advantages and disadvantages. For the list of newly generated novel resources, advantages and disadvantages were discussed and revised as in the first session. Lastly, we emailed a survey to participants to rate new and overlapping resources and both new and existing advantages and disadvantages for new and overlapping resources in that session.
Data processing, revision, and analysis
Sociodemographic characteristics and gastrointestinal symptoms were reported descriptively. French‐language NGT session responses were translated into English by using a standard forward–backward translation method (23). Then all resources were compiled into a single list. Study investigators, including members of the SPIN‐DINE Patient Advisory Team (Appendix A), reviewed all resources, advantages, and disadvantages; merged overlapping items; and reworded some items to improve general applicability (eg, “wait times may be long in Quebec” changed to “wait times may be long”), with final decisions based on consensus.
We used qualitative content analysis (24) to group resources using five categories that emerged from the data: 1) health care providers, 2) alternative and complementary practitioners, 3) websites and other media platforms, 4) events, and 5) print materials. Resources were initially classified by one investigator, reviewed by the team, and revised on the basis of suggestions and consensus. Data processing and analyses were done with Microsoft Excel.
RESULTS
We conducted four NGT sessions (three English, one French) in February 2020; data saturation and consistency was achieved after the fourth session. The number of participants per session ranged from two to five (total 15); three additional people registered but did not attend.
Participant characteristics
Participant characteristics are shown in Table 1. There were 12 women (80%), ages ranged from 37 to 71 years (median 58 years), most participants were White, and all had at least some college or university education. Approximately half had limited SSc (n = 8; 53%), and the median time since SSc diagnosis was 9 years. The number of gastrointestinal symptoms ranged from 1 to 11 (median [interquartile range] 4 [3–8]), with at least six symptoms reported by six participants (40%). The median (interquartile range) total UCLA SCTC GIT 2.0 score was 0.55 (0.37‐1.26). Four (27%) participants had an MST score of ≥2, indicating risk of malnutrition.
Table 1.
Participant characteristics
| Variable | Participants (N = 15) |
|---|---|
| Female sex, n (%) | 12 (80) |
| Age, years | |
| Median (range) | 58.0 (37‐71) |
| Mean (SD) | 56.5 (10.3) |
| Race/ethnicity,a n (%) | |
| White | 14 (93) |
| Asian | 1 (7) |
| Indigenous | 1 (7) |
| Country of residence, n (%) | |
| Canada | 10 (66) |
| United States | 2 (13) |
| United Kingdom | 1 (7) |
| The Netherlands | 1 (7) |
| Tunisia | 1 (7) |
| Relationship status, n (%) | |
| Married or living as married | 14 (93) |
| Widowed | 1 (7) |
| Highest level of education, n (%) | |
| Some college or university | 6 (40) |
| College or university degree | 6 (40) |
| Postgraduate degree | 3 (20) |
| Occupational status,b n (%) | |
| Unemployed | 1 (7) |
| Part‐time employed | 1 (7) |
| Full‐time employed | 4 (26) |
| Homemaker | 1 (7) |
| Retired | 7 (46) |
| On leave of absence | 1 (7) |
| On disability | 1 (7) |
| Full‐time student | 1 (7) |
| Systemic sclerosis subtype, n (%) | |
| Limited | 8 (53) |
| Diffuse | 6 (40) |
| Participant did not know subtype | 1 (7) |
| Years since systemic sclerosis diagnosis | |
| Median (range) | 9 (0.5‐30) |
| Mean (SD) | 11 (8.6) |
| Gastrointestinal symptoms, n (%)c | |
| Diarrhea | 9 (60) |
| Constipation | 10 (67) |
| Acid reflux | 12 (80) |
| Heartburn | 11 (73) |
| Nausea | 9 (60) |
| Abdominal pain | 6 (40) |
| Dysphagia | 9 (60) |
| Regurgitation | 8 (53) |
| Bloatingd | 2 (13) |
| Malabsorptiond | 2 (13) |
| Esophageal aperistalsisd | 1 (7) |
Participants could select more than one race/ethnicity. One participant identified as White and Asian.
Participants could select more than one occupation. One participant reported being on disability and unemployed; another reported being a homemaker and on leave of absence.
The total percentage does not equal 100% because participants could indicate more than one gastrointestinal symptom.
Bloating, malabsorption, and esophageal aperistalsis were not in the original list of common symptoms but were reported by participants as other symptoms they experience.
Resources and advantages and disadvantages
Figure 1 illustrates the number of resources, advantages, and disadvantages generated in each NGT session. In the second and third English‐speaking sessions, six and three identified resources, respectively, overlapped with resources from a previous session and were merged. The four NGT sessions generated a list of 44 total resources, 167 resource‐specific advantages, and 129 resource‐specific disadvantages. After we merged items by combining similar items and removing duplicates from the English and French sessions, the final list of items comprised 33 resources (see Table 2), 147 resource‐specific advantages, and 118 resource‐specific disadvantages (see Supplementary Table 1).
Figure 1.
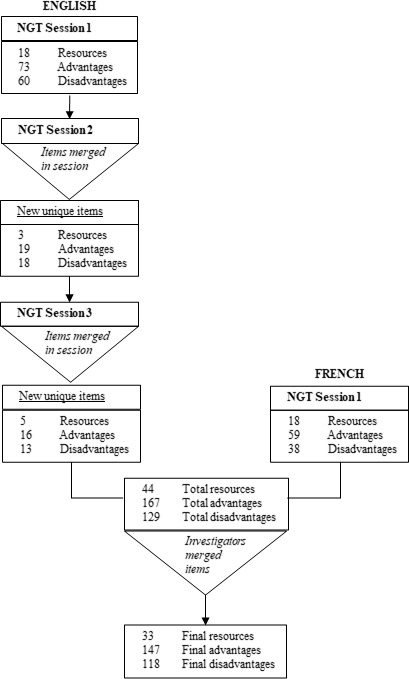
Flow diagram from initial items (resources, advantages, and disadvantages) to final items. NGT, nominal group technique.
Table 2.
Resource categories and items
| Health care providers |
| Registered dietitian for advice on what foods to eat or avoid and advice on general diet to address gastrointestinal problems (N = 11) |
| Rheumatologist for advice, resources, or referrals (to a dietitian) on what foods and supplements to eat or avoid to address scleroderma problems in general and gastrointestinal problems (N = 9) |
| Internal medicine physician to learn about experiences of other patients with scleroderma and for advice on what foods or supplements to eat and/or dietary modifications to make to address gastrointestinal problems (eg, reflux and bloating) and other scleroderma symptoms (N = 8) |
| Dietitian specialized in scleroderma for advice on dietary modifications to address gastrointestinal problems (N = 6) |
| Functional medicine physician for advice on supplements (eg, digestive enzyme) or specific dietary modifications to get enough nutrients to address scleroderma problems (eg, inflammation) (N = 5) |
| Gastroenterologist for advice on what foods to eat or avoid to address gastrointestinal problems and other scleroderma issues (eg, swallowing) and for the purpose of weight gain (N = 4) |
| Gastroenterologist for behavioral advice (eg, when to eat or lying down after eating) to address gastrointestinal problems (N = 4) |
| Nurse or medical professional to provide information on knowing your body and how your specific gastrointestinal tract responds to certain foods to create a diet protocol tailored to you to address gastrointestinal problems caused by scleroderma (N = 4) |
| Nutritionist, aiming at weight loss, for general nutritional purposes to maintain a healthy lifestyle (N = 4) |
| Nutritionist, aiming at weight gain, for nutritional advice specific to scleroderma‐related gastrointestinal symptoms (N = 4) |
| Alternative and complementary practitioners |
| Health food stores that hire nutritionists for advice on diets and dietary modification to address specific symptoms (eg, inflammation) (N = 4) |
| Homeopath, for nutritional advice, for general nutritional purposes (N = 4) |
| Naturopath for advice on what foods to eat to address scleroderma issues (eg, gastrointestinal problems and pain) (N = 4) |
| Holistic nutritionist for advice on what foods to eat to improve health and maintain good nutritional status (N = 4) |
| Websites and other media platforms |
| Organization website for patients with scleroderma (eg, publications or videos of conference presenters) with advice on general nutrition (eg, foods to prioritize or avoid) by medical doctors and specialists (N = 15) |
| General healthy lifestyle/eating websites (Pinterest) or Facebook groups for advice on diets (eg, renal diets or meal plans suggested by family doctor) and how to eat to address individual problems (N = 9) |
| Facebook groups with patients with scleroderma for advice on general nutrition for symptom management (N = 8) |
| Website created by functional medicine doctor for advice on dietary modifications to maintain overall health for general population (N = 5) |
| Facebook groups with patients with autoimmune diseases for advice on general nutrition for symptom management (N = 4) |
| Website of a university‐ or research institution‐based scleroderma care center (eg, University of Montreal), for nutritional advice, to maintain a healthy lifestyle specific to rheumatoid diseases (N = 4) |
| Website or Facebook pages for individual medical professionals (eg, functional medicine specialists) for advice on general nutrition for symptom management (N = 4) |
| Websites focused on scleroderma for advice on general nutrition and advice on what foods to eat or dietary tips to maintain good nutritional status (N = 4) |
| Events |
| Support groups by and for patients with scleroderma or autoimmune diseases for advice on specific problems presented in the group (N = 11) |
| Congress on scleroderma with invited speakers and the ability to meet with patients to obtain nutritional information for a better management of the disease and gastrointestinal symptoms (N = 4) |
| Conference by a nurse, in a community center or social service, for healthy lifestyle advice related to aging for general nutrition purposes (N = 4) |
| Conference by a nutritionist, in a community center or social service, for nutritional advice to maintain a healthy lifestyle (N = 4) |
| Events held by organizations for patients with scleroderma (eg, charitable organization) for advice on general nutrition by medical doctors and specialists (N = 4) |
| Local events with other patients with scleroderma (share their experiences) and medical specialists (eg, rheumatologist or dietitian) for advice on what foods to avoid or eat to address general nutrition (N = 4) |
| Print materials |
| Books and magazines written by medical professionals (eg, doctors or nutritionist) for behavioral advice or advice on what foods to eat or avoid to address overall health of people with autoimmune diseases (N = 9) |
| Organization magazine for patients with scleroderma with a thematic section written by a nutritionist for nutritional advice for general nutrition purposes (N = 4) |
| Books and magazines written by people living with scleroderma for advice on what foods to eat to address scleroderma issues (N = 4) |
| Regular newsletter provided by a national health organization for updates on the latest research regarding diet and gastrointestinal problems for the general population or specific diseases (N = 2) |
| Academic journals for information on specific diets, the success rate of these diets, and nutrition that is specific to your own needs (N = 2) |
Numbers in parentheses show how many participants rated each resource. Numbers >4 indicate that the resource was reported in more than one nominal group technique session.
Of the 33 resources, 10 (30%) were categorized as health care providers and included physicians (rheumatologists, internists, gastroenterologists), registered dietitians with and without specialization in SSc, nurses, and other health care professionals; four (12%) were categorized as alternative and complementary practitioners, which included nutritionists, naturopaths, and homeopaths; eight (24%) were categorized as websites and other media platforms and included online material from medical professionals, patient‐run social media groups, SSc‐specific websites (eg, organization for patients with SSc), and general rheumatology websites (eg, academic department); six (18%) were categorized as events and included conferences by medical professionals, local events, patient support groups, and events organized by SSc organizations; and five (15%) were categorized as print materials, which included books and magazines written by medical professionals or people living with SSc, academic journals, newsletters, and patient organization magazines.
Resources in the category of print materials had the highest proportion of raters who indicated having used the resources, with a mean of 85% of raters who reported having used each resource. This was followed by websites and other media platforms (77%), health care providers (58%), events (57%), and alternative and complementary practitioners (38%).
The number of ratings per resource and resource‐specific advantages and disadvantages depended on the number of participants in sessions in which the resource was elicited and the number of sessions in which the resource was elicited. This is because a resource was only rated by participants in sessions in which it was elicited by a group member. Figure 2 shows the distribution of ratings of the helpfulness of resources and the numbers of participants who rated the resources. Helpfulness ratings varied widely between and within categories. There were nine (27%) resources for which 75% to 100% of participants who rated the resource gave a helpfulness rating of ≥8 and 12 (36%) resources for which 50% to 74% of participants who rated the resource gave a helpfulness rating of ≥8. The number of resource‐specific advantages per resource ranged from 1 to 11 (median [interquartile range] 4 [3–6]), and the number of disadvantages ranged from zero to nine (median [interquartile range] 3 [2–4]). Of the 147 advantages, there were 66 (45%) advantages for which 75% to 100% of participants who rated the advantage gave a rating of ≥8 for importance and 53 (36%) advantages for which 50% to 74% of participants who rated the advantage gave a rating of ≥8 for importance. Of the 118 disadvantages, there were 40 (34%) for which 75% to 100% of participants who rated the disadvantage gave a rating of ≥8 for importance and 44 (37%) disadvantages for which 50% to 74% of participants who rated the disadvantage gave a rating of ≥8 for importance.
Figure 2.
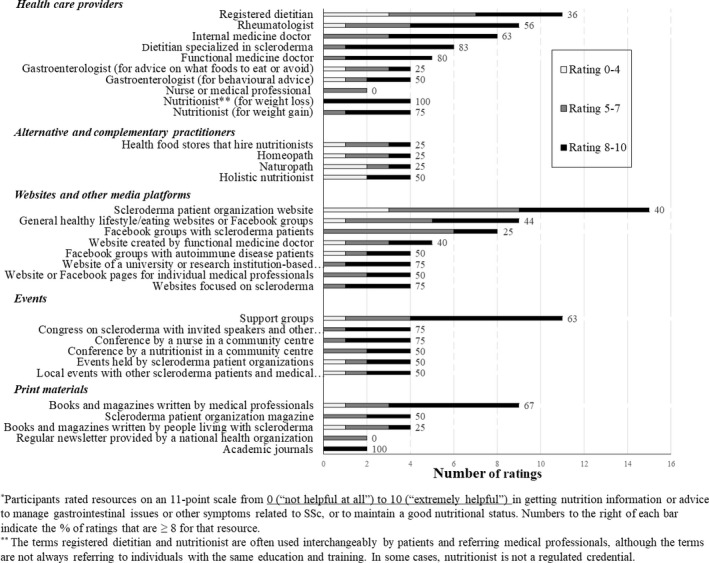
Distribution of ratings for resources.
Resource‐specific advantages and disadvantages were listed if reported by at least one participant in a group. Supplementary Table 1 shows the advantages and disadvantages that participants reported for each resource. Within the health care providers category, the resource‐specific advantages that were reported for the most resources in the category were individualized information (reported by at least one participant for 7 of 10 resources) and credibility of information (reported by at least one participant for 5 of 10 resources). The most reported resource‐specific disadvantages pertained to accessibility, including long wait times (reported by at least one participant for 5 of 10 resources) and travel time or geographical inaccessibility (reported by at least one participant for 8 of 10 resources). The only two health care providers for whom geographical inaccessibility was not listed as a disadvantage to using or accessing their services were registered dietitians and internal medicine doctors.
The most reported advantages in the alternative and complementary practitioners category included the alternative or holistic approach taken by the practitioner (three of four resources) and individualized information (three of four resources). The most reported disadvantage was inaccessibility due to cost (three of four resources). Inaccessibility due to location or travel was less frequently reported as a disadvantage (one of four resources). Homeopaths and holistic nutritionists were both listed as inaccessible due to geographical inaccessibility and cost of consultation.
The most reported advantages in the websites and other media platforms category included SSc‐specific information (five of eight resources), accessibility (four of eight resources), and ability to connect with others (four of eight resources). Most reported disadvantages included poor credibility or potentially biased information (four of eight resources), often in the case of websites that advertise for certain products or otherwise have commercial interests. Whether the resource provided individualized information was resource‐dependent; three of eight resources were noted to not provide individualized information, whereas this was listed as an advantage for two of eight resources.
The most reported resource‐specific advantage in events was the ability to connect with other patients and share information, which was listed as an advantage in six of six resources. Information credibility was split evenly as both an advantage (three of six resources) and a disadvantage (three of six resources), dependent on whether a participant sharing a perceived advantage or disadvantage regarded information from other patients as credible information. Most reported disadvantages related to inaccessibility, including high travel costs and travel time (five of six resources), and pertained to most types of events, with the exception of certain local events.
In print materials, advantages and disadvantages varied greatly by resource. Information credibility was both a commonly reported advantage (two of five resources) and disadvantage (two of five resources), depending on the perceived credibility of the person or organization that authored the information. The most reported disadvantage in this category was difficulty understanding the information provided due to scientific or medical technical language, which was reported for three of five resources. The degree to which information was recent was described as both a possible advantage and a disadvantage, depending on whether the information in a specific print resource was considered up to date.
DISCUSSION
We identified 33 nutrition information resources used by people with SSc, 147 perceived resource‐specific advantages, and 118 perceived resource‐specific disadvantages. There were five types of resources. Health care providers was the largest category, with nearly one third of all resources. The other categories included websites and other media platforms, events, print materials, and alternative and complementary practitioners. Resources differed in terms of advantages and disadvantages in three main domains: 1) the quality of information provided (credible, evidence based, up to date), 2) specificity of advice for individuals with SSc (information provided is SSc specific or personalized to individual), and 3) accessibility (cost, location, comprehensibility). Web‐based resources and print materials were often regarded as more accessible than events and health care providers, whereas information provided by health care professionals was generally regarded as more credible across categories, independent of the medium through which the information was shared (in‐person, events, online, print materials).
This study is the first to elicit nutrition and diet information resources directly from people with SSc. Four of the identified categories, health care providers, alternative and complementary practitioners, print materials, and web‐based resources, are consistent with results from other studies that have identified health information sources in other populations, including in primary care and oncology (25, 26). Studies with general population samples have also identified similar categories among healthy adults (27, 28). We do not know of any taxonomy of advantages and disadvantages of using and accessing health information resources, but the domains we identified were consistent with existing research on considerations of users in selecting information resources (27, 29). Quality of information and accessibility are important considerations. Our findings also highlight the importance of disease‐specific and individualized information for people with SSc, which is supported by previous research that has identified specificity and relevance of information as important factors for people when seeking health information (27). This may be particularly important for individuals with rare and complex conditions like SSc because it may be more difficult to find relevant information.
Our findings add to existing evidence in a few important ways. First, previous studies of the general population and other disease populations report two categories of health information resources that were not reported by people with SSc, interpersonal or social network (eg, family, friends, coworkers) (27, 28) and television or broadcast media (27, 28, 30). They were likely not noted in our study because of the unique nutrition and diet needs of people with SSc, which may limit the usefulness of generic advice from family, friends, and television. With a rare disease like SSc, individuals are unlikely to encounter people in their social circle who understand their condition or can provide useful nutrition and diet information. People with SSc did, however, report consulting with other people with SSc (eg, support groups, books written by others with SSc). Second, previous studies have not identified events or gatherings as a category of health information resources. Our findings indicate that they may be an important source of information for people with SSc. This category consisted of different types of events and gatherings, where information is typically provided by medical professionals, alternative medicine or other health service providers, and people with SSc or other autoimmune conditions.
Obtaining accurate and accessible nutrition and diet information can be an important tool for patients with SSc to effectively manage their symptoms and potentially improve quality of life. As evidenced by our study, people with SSc use a range of nutrition and diet‐related information sources to target a variety of SSc‐related symptoms and to maintain good nutritional status. Knowledge about the information‐seeking behavior of people with SSc and their perceptions about advantages and disadvantages of different sources is important to be able to disseminate information more effectively to patients through a variety of channels. Recent research on health information seeking has focused on the increased use of web‐based resources by both people with medical conditions and the general public (26). Web‐based resources are able to provide accessible, disease‐specific, and individualized information, but the credibility or quality of the information provided by these sources varies widely. Simultaneously, our findings support the existing literature that identifies medical professionals as the most credible sources of health information for people with health conditions (26), with an additional benefit of individualized information; however, inaccessibility is an important concern. Developing accessible web‐based resources by credible health care providers could improve access, although it would limit individualization of information. Increased telehealth access to medical professionals with SSc expertise could be a solution that could address accessibility concerns while retaining the advantages of credible and individualized information.
Because the evidence base to support nutrition and diet modifications for SSc‐related symptoms is limited (9), health care providers should continue to individualize the information provided to people with SSc as best as possible by helping them to understand the possible benefits and potential harms of different dietary modifications, taking into account their SSc manifestations and social determinants of health. This fits with a shared decision‐making framework (31, 32), which integrates personal preferences for health information and empowers people to be active participants in their own care and informed partners in the decision‐making process (27, 33, 34).
The present study was the first phase of the SPIN‐DINE project. On the basis of the results of the present study, a survey will be administered to more than 1700 people with SSc enrolled in the SPIN Cohort to investigate how common the use of identified resources are, as well as to investigate the perceived helpfulness of these resources and the importance of their associated advantages and disadvantages.
Interpretation of our results should consider limitations. First, our study involved a small sample of people with SSc. It is therefore possible that we might not have identified some resources that are used by people with SSc. To minimize this limitation, our data were reviewed by the SPIN‐DINE Patient Advisory Team members, who were able to suggest additional resources that will be included in the next phase of SPIN‐DINE research. Second, because of the small sample size, it is not appropriate to make quantitative inferences based on the helpfulness ratings of resources or importance ratings of the advantages and disadvantages. Third, all participants in the study had at least some university education, which is not representative of the whole SSc population. Thus, our sample may have had disproportionally high levels of health literacy compared with the SSc population at large, potentially limiting generalizability. Finally, this study was conducted before the coronavirus disease 2019 (COVID‐19) pandemic resulted in major shifts in the availability of virtual events, support, medical care, and education. Thus, our results do not address the recent growth of virtually held events and telemedicine or the implications of COVID‐19 on the accessibility of resources across categories. To account for these limitations, we will recruit a much larger sample of patients with SSc for the next phase of SPIN‐DINE research via a survey administered to the SPIN Cohort.
People with SSc reported using many nutrition and diet resources across five categories (health care providers, alternative and complementary practitioners, websites and other media platforms, events, and print materials) and highlighted resource‐specific advantages and disadvantages. The most commonly reported advantages and disadvantages related to the credibility and individualization of the information provided and the accessibility of the resources in terms of cost, location, and comprehensibility. The list of resources generated in this study will inform a survey with a much larger number of people with SSc to gain an understanding of the prevalence of usage of different resources, the helpfulness of these resources, and the importance of their associated advantages and disadvantages, as perceived by people with SSc, in managing gastrointestinal symptoms and other SSc‐related symptoms and maintaining good nutritional status.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Thombs had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Østbø, Jimenez, Harb, Thombs.
Acquisition of data
Østbø, Harb, Bourgeault, Carrier.
Analysis and interpretation of data
Østbø, Jimenez, Thombs, members of the SPIN‐DINE Patient Advisory Team.
Supporting information
Table S1
Supplementary Material
APPENDIX A. MEMBERS OF THE SPIN‐DINE PATIENT ADVISORY TEAM
Members of the SPIN‐DINE Patient Advisory Team are as follows: Deani Baillie (London, UK); Cathleen Dobbs, PhD (Joliet, IL); Amy Gietzen (Buffalo, NY); Genevieve Guillot (Longueuil, Québec, Canada); Jennifer Johnston (Edmonton, Alberta, Canada); Dorothy M. Kurylo, MD (Danville, IL); and Laura Simmons (Halifax, Nova Scotia, Canada).
The Scleroderma Patient‐Centered Intervention Network (SPIN) has received funding for its core activities from the Canadian Institutes of Health Research, the Arthritis Society, the Lady Davis Institute for Medical Research of the Jewish General Hospital (Montreal, Quebec, Canada), the Jewish General Hospital Foundation (Montreal, Quebec, Canada), McGill University (Montreal, Quebec, Canada), the Scleroderma Society of Ontario, Scleroderma Canada, Sclérodermie Québec, Scleroderma Manitoba, Scleroderma Atlantic, the Scleroderma Association of British Columbia, the Scleroderma Association of Saskatchewan, Scleroderma Australia, Scleroderma New South Wales, Scleroderma Victoria, and Scleroderma Queensland. Mr. Harb’s work was supported by a Canadian Institutes of Health Research Canada Graduate Scholarships Masters Award. Dr. Thombs’ work was supported by a Tier 1 Canada Research Chair.
Dr. Jimenez reports a contract from the Academy of Nutrition and Dietetics outside the submitted work. No other disclosures relevant to this article were reported.
REFERENCES
- 1.Allanore Y, Simms R, Distler O, Trojanowska M, Pope J, Denton CP, et al. Systemic sclerosis. Nat Rev Dis Primers 2015;1:15002. [DOI] [PubMed] [Google Scholar]
- 2.McFarlane IM, Bhamra MS, Kreps A, Iqbal S, Al‐Ani F, Saladini‐Aponte C, et al. Gastrointestinal manifestations of systemic sclerosis. Rheumatology (Sunnyvale) 2018;8:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagaraja V, McMahan ZH, Getzug T, Khanna D. Management of gastrointestinal involvement in scleroderma. Curr Treatm Opt Rheumatol 2015;1:82–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krause L, Becker MO, Brueckner CS, Bellinghausen C‐J, Becker C, Schneider U, et al. Nutritional status as marker for disease activity and severity predicting mortality in patients with systemic sclerosis. Ann Rheum Dis 2010;69:1951–7. [DOI] [PubMed] [Google Scholar]
- 5.Sakkas LI, Simopoulou T, Daoussis D, Liossis S‐N, Potamianos S. Intestinal involvement in systemic sclerosis: a clinical review. Dig Dis Sci 2018;63:834–44. [DOI] [PubMed] [Google Scholar]
- 6.Baron M, Bernier P, Côté L‐F, Delegge MH, Falovitch G, Friedman G, et al. Screening and management for malnutrition and related gastro‐intestinal disorders in systemic sclerosis: recommendations of a North American expert panel. Clin Exp Rheumatol 2010;28Suppl 58:S42–6. [PubMed] [Google Scholar]
- 7.Hansi N, Thoua N, Carulli M, Chakravarty K, Lal S, Smyth A, et al. Consensus best practice pathway of the UK scleroderma study group: gastrointestinal manifestations of systemic sclerosis. Clin Exp Rheumatol 2014;32Suppl 86:S214–21. [PubMed] [Google Scholar]
- 8.Shah AA, Wigley FM. My approach to the treatment of scleroderma. Mayo Clin Proc 2013;88:377–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith E, Pauling JD. The efficacy of dietary intervention on gastrointestinal involvement in systemic sclerosis: a systematic literature review. Semin Arthritis Rheum 2019;49:112–8. [DOI] [PubMed] [Google Scholar]
- 10.Kwakkenbos L, Jewett LR, Baron M, Bartlett SJ, Furst D, Gottesman K, et al. The Scleroderma Patient‐centered Intervention Network (SPIN) cohort: protocol for a cohort multiple randomised controlled trial (cmRCT) design to support trials of psychosocial and rehabilitation interventions in a rare disease context. BMJ Open 2013;3:e003563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallagher M, Hares T, Spencer J, Bradshaw C, Webb I. The nominal group technique: a research tool for general practice? Fam Pract 1993;10:76–81. [DOI] [PubMed] [Google Scholar]
- 12.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 13.Dougherty DH, Kwakkenbos L, Carrier M‐E, Salazar G, Assassi S, Baron M, et al. The Scleroderma Patient‐centered Intervention Network cohort: baseline clinical features and comparison with other large scleroderma cohorts. Rheumatology (Oxford) 2018;57:1623–31. [DOI] [PubMed] [Google Scholar]
- 14.Shreiner AB, Murray C, Denton C, Khanna D. Gastrointestinal manifestations of systemic sclerosis. J Scleroderma Relat Disord 2016;1:247–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bharadwaj S, Tandon P, Gohel T, Corrigan ML, Coughlin KL, Shatnawei A, et al. Gastrointestinal manifestations, malnutrition, and role of enteral and parenteral nutrition in patients with scleroderma. J Clin Gastroenterol 2015;49:559–64. [DOI] [PubMed] [Google Scholar]
- 16.Khanna D, Hays RD, Maranian P, Seibold JR, Impens A, Mayes MD, et al. Reliability and validity of the University of California, Los Angeles scleroderma clinical trial consortium gastrointestinal tract instrument. Arthritis Rheum 2009;61:1257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferguson M, Capra S, Bauer J, Banks M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999;15:458–64. [DOI] [PubMed] [Google Scholar]
- 18.Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, et al. Position of the Academy of Nutrition and Dietetics: malnutrition (undernutrition) screening tools for all adults. J Acad Nutr Diet 2020;120:709–13. [DOI] [PubMed] [Google Scholar]
- 19.Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, et al. Adult malnutrition (undernutrition) screening: an evidence analysis center systematic review. J Acad Nutr Diet 2020;120:669–708. [DOI] [PubMed] [Google Scholar]
- 20.Delbecq AL, van de Ven AH , Gustafson DH. Group techniques for program planning: a guide to nominal group and Delphi processes. Glenview, IL: Scott, Foresman and Company; 1975. [Google Scholar]
- 21.Harb S, Cumin J, Rice DB, Peláez S, Hudson M, Bartlett SJ, et al. Identifying barriers and facilitators to physical activity for people with scleroderma: a nominal group technique study. Disabil Rehabil 2020. E‐pub ahead of print. 10.1080/09638288.2020.1742391 [DOI] [PubMed] [Google Scholar]
- 22.Rice DB, Canedo‐Ayala M, Turner KA, Gumuchian ST, Malcarne VL, Hagedoorn M, et al. Use of the nominal group technique to identify stakeholder priorities and inform survey development: an example with informal caregivers of people with scleroderma. BMJ Open 2018;8:e019726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization . Process of translation and adaptation of instruments. URL: https://www.who.int/substance_abuse/research_tools/translation/en/.
- 24.Mayring P. Qualitative content analysis. Forum Qual Soc Res 2000;1(2):20. [Google Scholar]
- 25.Nagler RH, Romantan A, Kelly BJ, Stevens RS, Gray SW, Hull SJ, et al. How do cancer patients navigate the public information environment? Understanding patterns and motivations for movement among information sources. J Cancer Educ 2010;25:360–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramsey I, Corsini N, Peters MD, Eckert M. A rapid review of consumer health information needs and preferences. Patient Educ Couns 2017;100:1634–42. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y. Beyond quality and accessibility: source selection in consumer health information searching. J Assoc Inf Sci Technol 2014;65:911–27. [Google Scholar]
- 28.Jacobs W, Amuta AO, Jeon KC. Health information seeking in the digital age: an analysis of health information seeking behavior among US adults. Cogent Soc Sci 2017;3:1302785. [Google Scholar]
- 29.Rains SA. Perceptions of traditional information sources and use of the world wide web to seek health information: findings from the health information national trends survey. J Health Commun 2007;12:667–80. [DOI] [PubMed] [Google Scholar]
- 30.Meissner HI, Potosky AL, Convissor R. How sources of health information relate to knowledge and use of cancer screening exams. J Community Health 1992;17:153–65. [DOI] [PubMed] [Google Scholar]
- 31.Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681–92. [DOI] [PubMed] [Google Scholar]
- 32.Charles C, Gafni A, Whelan T. Decision‐making in the physician–patient encounter: revisiting the shared treatment decision‐making model. Soc Sci Med 1999;49:651–61. [DOI] [PubMed] [Google Scholar]
- 33.Murray E, Charles C, Gafni A. Shared decision‐making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Educ Couns 2006;62:205–11. [DOI] [PubMed] [Google Scholar]
- 34.Elwyn G, Frosch D, Thomson R, Joseph‐Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Supplementary Material


