Significance
Experiencing early life adversity may negatively impact mental health; however, many of these individuals display psychological resilience or positive psychological health despite experiences of early adversity. This positive capacity for mental health may extend to physical health benefits, including lower cardiometabolic disease. While research suggests that early adversity increases later disease risk, we found that individuals who display psychological resilience to early adversity did not have higher odds of developing cardiometabolic disease. Indeed, those who showed psychological resilience had similar odds of disease to peers who did not experience early adversity. These findings were also reflected in measures of biological cardiometabolic risk. Overall, findings suggest that individuals who manifest psychological resilience may have lower cardiometabolic disease risk later in life.
Keywords: psychological resilience, cardiometabolic disease, early adversity, biomarkers
Abstract
Early adversity is associated with poor cardiometabolic health, potentially via psychological distress. However, not everyone exposed to adversity develops significant distress. Psychological resilience and positive psychological health despite adversity may protect against unfavorable cardiometabolic outcomes that are otherwise more likely. We examined early adversity, psychological resilience, and cardiometabolic risk among 3,254 adults in the Midlife in the United States Study. Psychological resilience was defined according to both early psychosocial adversity and adult psychological health (characterized by low distress and high wellbeing) at Wave 1 (1994 to 1995). Categorical resilience was derived by cross-classifying adversity (exposed versus unexposed) and psychological health (higher versus lower). We also assessed count of adversities experienced and psychological symptoms as separate variables. Incident cardiometabolic conditions (e.g., heart attack, stroke, and diabetes) were self-reported at Waves 2 (2004 to 2005) and 3 (2013 to 2014). Secondary analyses examined biological cardiometabolic risk using a composite of biomarkers available within a Wave-2 subsample. Logistic and Poisson regressions evaluated associations of resilience with cardiometabolic health across 20 follow-up y, adjusting for relevant covariates. In this initially healthy sample, nonresilient (adversity-exposed, lower psychological health) versus resilient (adversity-exposed, high psychological health) individuals had 43% higher odds of cardiometabolic conditions (95% CI 1.10 to 1.85). Odds of cardiometabolic conditions were similar among resilient versus unexposed, psychologically healthy individuals. More adversity experiences were associated with increased odds, while better psychological health with decreased odds of cardiometabolic conditions, and effects were largely independent. Patterns were similar for objectively assessed cardiometabolic risk. Psychological resilience in midlife may protect against negative cardiometabolic impacts of early adversity.
Cardiometabolic conditions, including heart disease and diabetes, constitute leading causes of morbidity and mortality in US adults (1). However, known adult risk factors for these conditions are often poorly managed, and prevention strategies are underutilized, expensive, or of limited efficacy (1). A life course perspective may determine whether and how early life conditions can cause adverse health trajectories into adulthood, identifying early life predictors that may illuminate novel prevention and intervention targets to reduce later disease burden. Research has begun to identify early risk and protective factors beyond typical biological and behavioral domains, such as psychosocial stress and mental illness (2).
One such early life factor is psychosocial adversity, which can disrupt normal development and fail to facilitate healthy growth (3). Consistent evidence has demonstrated early adversity, including maltreatment and household dysfunction, confers negative mental and physical health consequences (4). Research is beginning to disentangle how early adversity impacts cardiometabolic risk through multiple biological, behavioral, and psychological pathways (2). However, an important unresolved issue is the role of psychological resilience in the relationship between early adversity and cardiometabolic outcomes. Psychological resilience, positive psychological functioning despite early adversity (5), is often considered a dynamic process influenced by internal and external factors underlying the capacity of individuals exposed to adversity to maintain or manifest psychological health (6). Psychological resilience encapsulates two domains: exposure to significant adversity and positive psychological functioning, characterized both by low distress and high wellbeing (5).
Early adversity and psychological distress have each been linked with cardiometabolic outcomes (2, 4). However, few studies examine resilience specifically with subsequent cardiometabolic risk. Among these, findings suggest higher resilience lowers risk of poor cardiometabolic outcomes (7–10). For example, in a study that defined stress resilience according to a psychologist’s rating of men’s capacity to cope with war-time stress based on a semistructured interview at age 18, low versus high stress resilience was associated with increased risk of heart disease (9), stroke (8), and diabetes (10). Another study of older civilian adults found “resilient” individuals (i.e., trauma exposed with no re-experiencing posttraumatic stress symptoms) had lower dementia risk than individuals unexposed to trauma (11). However, it is unclear whether resilient individuals are at risk levels comparable to peers unexposed to adversity—fully offsetting harmful effects of adversity. Furthermore, most studies to date are cross-sectional.
To evaluate these relationships, we used data from the Midlife in the United States (MIDUS) study, an ongoing longitudinal cohort of US adults. Evidence from MIDUS has demonstrated that early adversity increases odds of cardiovascular disease and diabetes (12), psychological distress increases risk of cardiometabolic conditions (13), and psychological wellbeing is generally protective against cardiometabolic conditions (14). However, no studies in MIDUS (or other population-based community cohorts) have specifically examined psychological resilience to early adversity and incident cardiometabolic conditions.
Resilience has been defined in several ways, including as an individual trait regardless of context or experience, as a dynamic process involving changes in psychological functioning over time, or as a capacity demonstrated by manifesting psychological health despite adversity (15). Measurement has consequently varied, from trait resiliency scales to trajectories of psychopathology posttrauma. Here, we conceptualize resilience as the product of life experience—a capacity manifested by positive psychological health in adulthood among individuals who experienced early adversity. While many studies consider resilience as the outcome and evaluate predictors of resilience, we examined psychological resilience as an exposure that could influence subsequent cardiometabolic outcomes. To operationalize resilience, we used two approaches common in developmental psychology, providing complementary information: person-focused (i.e., classifying individuals by relevant characteristics or capacities) and variable-focused (i.e., examining how specific factors link to outcomes) (16). As prior work has indicated that absence of negative psychological states does not necessarily entail positive functioning (17), we considered levels of both psychological distress and positive wellbeing, or capacity for generative experiences and positive emotions, to capture psychological health comprehensively (6).
We estimated whether psychological resilience was associated with developing cardiometabolic conditions across 20 y, adjusting for sociodemographic, health-related, and behavioral covariates selected according to prior literature. Our person-focused hypotheses were as follows: relative to individuals exposed to early adversity with favorable psychological functioning (i.e., resilient), those who were unexposed to early adversity with favorable psychological functioning would not have decreased cardiometabolic risk whereas those with unfavorable psychological functioning with adversity (i.e., nonresilient) would have greater risk. Our variable-focused hypotheses were that higher adversity exposure would be associated with greater cardiometabolic risk, while higher psychological health would be associated with decreased risk. Furthermore, as we anticipated that manifesting high psychological health would offset the negative impact of adversity, we hypothesized effect modification whereby the effect of adversity on cardiometabolic risk would depend on psychological health—among those with high adversity, higher psychological health would buffer negative effects of adversity. To examine an objective indicator of cardiometabolic health, we examined the association between resilience and biological cardiometabolic risk among a subset of the analytic sample.
Materials and Methods
Study Population.
Data are from MIDUS, a cohort of noninstitutionalized, English-speaking US adults enrolled in 1995 to 1996 who completed telephone interviews and mailed self-administered questionnaires (SAQ) across three data collection waves (18). Wave 1 (W1) included 7,108 participants (age 25 to 74) sampled through random-digit dialing; 6,325 completed both telephone and SAQ assessments. All W1 respondents were contacted for Wave 2 (W2) in 2004 to 2006, with 4,041 participating (64% response rate), and all W2 respondents were contacted for Wave 3 (W3) in 2013 to 2015, with 2,717 participating in all waves (67% response rate). Telephone and SAQ data from all three waves were utilized for current analyses.
At W1, 5,388 participants had complete exposure and covariate information required for the current study. We excluded individuals with any cardiometabolic conditions at W1 (n = 450, 8%) and those who did not participate in W2 (n = 1,684, 31% were lost to follow-up by W2; n = 347 due to death) for an analytic sample of 3,254 participants. Further attrition occurred from W2 to W3: 211 (7%) participants died prior to W3 by non–cardiometabolic-related causes, and 788 (24%) were otherwise lost to follow-up by W3.
Contemporaneous to W2, a subset of our analytic sample (n = 757) completed a clinical visit for biological assessments to identify biopsychosocial pathways contributing to health outcomes (19). In this subset, we further excluded 103 individuals who reported hypertension or high cholesterol at W1 to include only individuals with low baseline cardiometabolic risk. In this biomarker subsample (n = 654), we assessed resilience at W1 with biological cardiometabolic risk 10 y later.
All participants provided informed consent and the study was approved by Institutional Review Boards at the University of Wisconsin–Madison, Georgetown University, and the University of California, Los Angeles.
Measures.
Psychological resilience.
Psychological resilience was characterized using information from two domains: childhood/adolescent adversity exposure and adult psychological health, encompassing distress and wellbeing.
Early adversity exposure was assessed via retrospective reporting at W1 of experiencing four specific adversities (yes/no) prior to age 18. Adversities included emotional abuse, physical abuse, parental separation/divorce, and parental death occurring in childhood/adolescence, all measured using items from the Conflict Tactics Inventory (20). Individuals were considered exposed if they reported experiencing any of the adversity types before age 18 (SI Appendix). We summed exposures across adversity types to create a cumulative count of adversity exposures (range 0 to 4) (21). To facilitate classifying individuals categorically, we created a binary adversity exposure variable defined as exposed (≥1 adversities) and unexposed (0 adversities). As only four early adversities were assessed, any experience was conservatively considered exposure, consistent with research indicating elevated risk of negative health consequences following any childhood adversity (relative to none) (22).
Psychological health was assessed using separate self-reported measures of distress and of positive wellbeing. Both dimensions of the psychological experience are necessary to comprehensively capture psychological health (23, 24) and are particularly relevant in the context of manifesting psychological resilience to adversity (25). Psychological distress at W1 was ascertained according to past-year depression and generalized anxiety levels obtained from the validated Composite International Diagnostic Interview-Short Form scales (26). Major depression and generalized anxiety were identified based on validated clinical criteria (SI Appendix). Overall psychological distress was characterized as a continuous variable by summing standardized depressive and anxiety symptom scores and as a high (clinically elevated depression or anxiety) versus low (not meeting clinical criteria for depression and anxiety) binary variable.
Positive wellbeing was ascertained at W1 using the validated Ryff psychological wellbeing scales (27). The overall psychological wellbeing score (range 18 to 126) was derived by summing responses to 18 items total across six domains: self-acceptance, positive relations with others, personal growth, purpose in life, environmental mastery, and autonomy (27). As there are no standard cut-points for wellbeing, the sample top tercile was used to indicate high wellbeing, and the bottom two terciles indicated lower wellbeing (23). This dichotomy is notably conservative, whereby only those with the highest wellbeing were designated as “high.”
A composite continuous psychological health variable was derived by summing the inverse of standardized depressive and anxiety symptoms with standardized wellbeing scores, resulting in a continuous composite variable where higher scores indicate better psychological health. Similar composite measures for distress (28) and wellbeing (29) have been derived in prior work; our combined measure was created to capture the sum of both psychological dimensions, such that those with low distress and high wellbeing had the highest levels, while either low distress or high wellbeing alone had moderate levels, and high distress without wellbeing had the lowest levels. Similarly, categorical psychological health was defined a priori as high (lower symptoms for both distress measures and high wellbeing) versus lower (elevated symptoms on either distress measure or lower wellbeing) psychological health.
We used two approaches to characterize psychological resilience. A person-focused approach classified individuals according to their resilience status (16), which compared groups with defining features. Categorical psychological resilience was defined using binary cutoffs for exposed versus unexposed to early adversity and lower versus high psychological health. This produced four resilience categories: favorable psychological functioning with adversity (resilient; adversity-exposed, high psychological health), unfavorable psychological functioning with adversity (nonresilient; adversity-exposed, lower psychological health), unfavorable psychological functioning without adversity (adversity-unexposed, lower psychological health), and favorable psychological functioning without adversity (adversity-unexposed, high psychological health) (30–32). A variable-focused approach concurrently included adversity and psychological health as separate exposures in analytic models (16), which maximized statistical power and examined fine-grained relationships between variables. With this approach, psychological resilience may be considered on a continuum, with higher levels characterized by having higher psychological health in the presence of greater adversity exposure, by examining main and interaction effects.
Cardiometabolic conditions and biological cardiometabolic risk.
Cardiometabolic conditions included five conditions (i.e., heart attack, heart failure, coronary artery disease, stroke, diabetes [type 2 only]) reported at each wave, or death due to cardiometabolic-related causes. For each condition, individuals reported having ever been diagnosed/taking relevant medications at W1 and diagnosed/taking relevant medications since the previous assessment at W2 and W3. The MIDUS study ascertained cause of death from various data sources (e.g., mortality closeout interviews, National Death Index); deaths due to cardiometabolic-related conditions based on International Classification of Diseases, Tenth Revision (ICD-10) codes among individuals over follow-up with no prior reported cardiometabolic conditions were considered cases. To capture incidence of any cardiometabolic condition, we defined a composite binary variable as having any versus none of the conditions or cardiometabolic-related death at each follow-up (W2 and W3) among individuals with no prior conditions (e.g., those reporting conditions at W2 were not at risk for W3).
Biological cardiometabolic risk was assessed at a clinical visit, with measures taken by study staff. Participants provided fasting blood samples, blood pressure, and anthropomorphic measurements from which eight cardiometabolic biomarkers were obtained: systolic blood pressure (SBP), diastolic blood pressure (DBP), triglycerides, high-density lipoprotein (HDL), low-density lipoprotein (LDL), glycosylated hemoglobin (HbA1c), waist circumference, and C-reactive protein (CRP) (SI Appendix). Following previous work (33), raw values were used to derive relevant indicators for each biomarker. Extreme levels were removed for triglycerides >2,000 mg/dL, HbA1c >15%, waist circumference >200 cm, and CRP >10 mg/L, which may indicate outliers, incorrect values, or active infection (34). Participants also reported current heart (i.e., hypertensive medication, aspirin, cardiovascular agents, and coagulation modifiers), cholesterol (i.e., antihyperlipidemic agents), and diabetes (i.e., antidiabetic agents) medication use. Each raw biomarker value was dichotomized (elevated risk = 1, not elevated risk = 0) based on clinical cut-points and/or medication use (Table 1). A cardiometabolic risk score was calculated by summing dichotomized biomarkers to indicate count of elevated risk parameters (range 0 to 8), representing cumulative biological risk in cardiovascular and metabolic domains that are known to increase risk of cardiometabolic conditions consistent with prior work (33, 35).
Table 1.
Description of cardiometabolic risk biomarkers (n = 654)
| Cardiometabolic risk biomarker | Mean (SD) | Risk threshold | Elevated risk, N (%) |
| SBP | 124.3 (19.3) | ≥130 mmHg or on heart medication (42) | 488 (74.6) |
| DBP | 61.6 (11.9) | ≥85 mmHg or on heart medication (42) | 422 (64.5) |
| Triglycerides | 125.9 (74.8) | ≥150 mg/dL or on cholesterol medication (48) | 303 (46.3) |
| HDL | 55.1 (17.7) | <40 mg/dL in men, <50 mg/dL in women or on cholesterol medication (42) | 309 (46.3) |
| LDL | 108.9 (34.1) | ≥160 mg/dL or on cholesterol medication (49) | 216 (33.0) |
| HbA1c | 5.8 (0.6) | ≥7% or on diabetes medication (48) | 41 (6.3) |
| Waist circumference | 95.3 (15.4) | ≥94 cm in men, ≥80 cm in women (42) | 471 (72.0) |
| CRP | 2.1 (2.2) | >3 mg/L (50) | 157 (24.0) |
CRP, C-reactive protein; DBP, diastolic blood pressure; HbA1c, glycosylated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Covariates.
Covariates were self-reported at W1. Sociodemographic covariates included age (continuous years), sex (male, female), race/ethnicity (white, non-white), parental education (highest of mother or father; less than high school, GED or high school, some college/2-y college, 4-y college, or greater), family financial status growing up (financial level during childhood relative to average families; 1 = a lot worse to 7 = a lot better off), and family history of cardiovascular disease (any cardiovascular disease in immediate family, no family history); these variables constituted potential confounders. Adult circumstances included marital status (married, separated/divorced, widowed, or never married), education (less than high school, GED or high school, some college/2-y college, or 4-y college or greater), annual household income (≤$25,000, $25,001 to 45,000, $45,001 to 70,000, or ≥$70,001), and health insurance coverage (insured, not currently insured); these factors might be impacted by early adversity and may also subsequently impact psychological health, thus may be associated with the process of developing (or not) psychological resilience (12). Adult biobehavioral factors included body mass index (BMI; calculated from self-reported height and weight, continuous in kg/m2), smoking (current smoker, not current smoker) and physical activity (regularly active, not regularly active, or inactive), which could be confounders or pathway variables linking adversity and psychological resilience to cardiometabolic risk.
Analyses.
Group differences between the analytic sample and those excluded (due to exclusion criteria and attrition) suggested potential selection bias (SI Appendix). To account for this, we created separate stabilized inverse probability weights for differential initial inclusion and loss to follow-up. The product of the stabilized selection and attrition weights were included in all analytic models (SI Appendix) (36). We assessed distributions of resilience, cardiometabolic outcomes, and covariates, as well as bivariate associations between covariates and resilience status.
For person-focused analyses, we conducted a series of regression models to examine associations of categorical resilience with incident cardiometabolic conditions across follow-up. Using repeated measures logistic regression with generalized estimating equations (GEE), we determined odds of any conditions associated with resilience status. GEE models with repeated measures determine marginal, population-level effects while accounting for correlated, longitudinal data with robust variance estimates (37). Models account for within-person (i.e., repeated measures) and between-person (i.e., sibling clustering, n = 1,337 [41%] had ≥1 sibling) correlation by specifying a compound symmetry covariance structure that assumes correlated errors. Quasi-likelihood estimation derives reliable and valid marginal regression coefficients and SEs corrected for clustering in the data. All models included inverse probability weights to account for selection and differential attrition (36). We used the favorable psychological functioning with adversity (resilient) group as the reference to assess whether associations with cardiometabolic outcomes differed between those who were versus were not resilient or compared to individuals who had not faced adversity. Post hoc Tukey analyses assessed all two-way comparisons of resilience status for odds of developing cardiometabolic conditions. Sequentially adjusted models adjusted first for sociodemographic variables (M1), M1 plus adult circumstances (M2), and M2 plus biobehavioral factors (M3).
For variable-focused analyses, the same series of models were estimated with continuous exposures for adversity count and psychological health. We first examined adversity count and psychological health in separate models with covariates, second, including these variables simultaneously in a model with covariates (i.e., coadjusting for adversity count and psychological health), and third, testing the multiplicative adversity count–psychological health interaction. In sensitivity analyses, we disaggregated psychological health into its components (i.e., depressive symptoms, anxiety symptoms, and psychological wellbeing) to examine whether particular components were driving associations.
As prior work has suggested sex differences in levels of resilience (6), we tested for sex effect modification using interaction terms in primary models. We found no evidence for sex differences and therefore present results for the total sample.
In secondary analyses, we examined resilience and biological cardiometabolic risk among the biomarker subsample. Using the same set of adjusted models, we ran Poisson regression models with robust SEs to determine associations between psychological resilience and cardiometabolic risk score.
Results
The analytic sample was 46.2 (SD = 12.1) y old on average at baseline, 56% female, and 94% white (Table 2). There was a range of childhood socio-economic status (SES), indicated by parental education and financial status growing up. Most of the sample was married, 39% completed college or greater, and 42% had an annual household income greater than $70,000. Average BMI was 26.4 (SD = 5.0), 80% were nonsmokers, and 73% were regularly physically active.
Table 2.
Distribution of baseline covariates by psychological resilience
| Covariates | Total sample | Psychological resilience | |||
| Favorable Psychological Functioning with Adversity n = 501 (15.4) | Unfavorable Psychological Functioning with Adversity n = 1,273 (38.0) | Unfavorable Psychological Functioning without Adversity n = 918 (28.2) | Favorable Psychological Functioning without Adversity n = 598 (18.4) | ||
| Age, mean (SD) | 46.2 (12.1) | 46.5 (11.8) | 44.7 (11.5) | 47.3 (12.3) | 47.4 (12.6) |
| Sex | |||||
| Male | 1,440 (44.3) | 233 (46.5) | 546 (44.1) | 407 (44.3) | 254 (42.5) |
| Female | 1,814 (55.8) | 268 (53.5) | 691 (55.9) | 511 (55.7) | 344 (57.5) |
| Race/ethnicity | |||||
| White | 3,069 (94.3) | 468 (93.4) | 1,147 (92.7) | 882 (96.1) | 572 (95.7) |
| Non-White | 185 (5.7) | 33 (6.6) | 90 (7.3) | 36 (3.9) | 26 (4.4) |
| Parental education | |||||
| Less than high school | 767 (23.6) | 124 (24.8) | 323 (26.1) | 198 (21.6) | 122 (20.4) |
| GED or high school | 1,182 (36.3) | 182 (36.3) | 496 (40.1) | 329 (35.8) | 175 (29.3) |
| Some college/2-y college | 522 (16.0) | 83 (16.6) | 174 (14.1) | 146 (15.9) | 119 (19.9) |
| 4-y college or greater | 783 (24.1) | 112 (22.4) | 244 (19.7) | 245 (26.7) | 182 (30.4) |
| Youth financial status, mean (SD) | 4.1 (1.3) | 4.0 (1.3) | 3.8 (1.4) | 4.3 (1.2) | 4.3 (1.2) |
| Family history of CVD present | 1,207 (37.1) | 196 (39.1) | 458 (37.0) | 349 (38.0) | 204 (34.1) |
| Marital status | |||||
| Married | 2,342 (72.0) | 382 (76.3) | 811 (65.6) | 660 (71.9) | 489 (81.8) |
| Separated or divorced | 450 (13.8) | 63 (12.6) | 234 (18.9) | 111 (12.1) | 42 (7.0) |
| Widowed | 116 (3.6) | 11 (2.2) | 48 (3.9) | 45 (4.9) | 12 (2.0) |
| Never married | 346 (10.6) | 45 (9.0) | 144 (11.6) | 102 (11.1) | 55 (9.2) |
| Education | |||||
| Less than high school | 164 (5.0) | 23 (4.6) | 88 (7.1) | 37 (4.0) | 16 (2.7) |
| GED or high school | 859 (26.4) | 107 (21.4) | 376 (30.4) | 254 (27.7) | 122 (20.4) |
| Some college/2-y college | 979 (30.1) | 154 (30.7) | 405 (32.7) | 268 (29.2) | 152 (25.4) |
| 4-y college or greater | 1,252 (38.5) | 217 (43.3) | 368 (29.8) | 359 (39.1) | 308 (51.5) |
| Household income level | |||||
| <$25,000 | 498 (15.3) | 51 (10.2) | 247 (20.0) | 145 (15.8) | 55 (9.2) |
| $25,001–$45,000 | 652 (20.0) | 85 (17.0) | 260 (21.0) | 200 (21.8) | 107 (17.9) |
| $45,001–$70,000 | 732 (22.5) | 110 (22.0) | 292 (23.6) | 200 (21.9) | 130 (21.7) |
| >$70,001 | 1,372 (42.2) | 255 (50.9) | 438 (35.4) | 373 (40.6) | 306 (51.2) |
| Current health insurance coverage | 2,957 (90.9) | 462 (92.2) | 1,104 (89.3) | 826 (90.0) | 565 (94.5) |
| BMI, mean (SD) | 26.4 (5.0) | 26.3 (5.0) | 26.9 (5.4) | 26.3 (5.0) | 25.8 (4.5) |
| Current smoker | 639 (19.6) | 93 (18.6) | 322 (26.0) | 149 (16.2) | 75 (12.5) |
| Physical activity | |||||
| Regularly active | 2,371 (72.9) | 405 (80.8) | 875 (70.7) | 623 (67.9) | 468 (78.3) |
| Not regularly active | 785 (24.1) | 86 (17.2) | 315 (255) | 261 (28.4) | 123 (20.6) |
| Inactive | 98 (3.0) | 10 (2.0) | 47 (3.8) | 34 (3.7) | 7 (1.2) |
All entries are provided as N (%).
Similar to other MIDUS studies, 53% of the sample (n = 1,738) were exposed to at least one early adversity type, with 846 (26%) exposed to one type, 716 (22%) exposed to two, and 176 (6%) exposed to three or four types. Emotional abuse (n = 1,151, 35%) and physical abuse (n = 1,043, 32%) were frequent, while parental separation/divorce (n = 328, 10%) and parental death (n = 297, 9%) were less frequent.
The average level of psychological wellbeing was 101.0 (range = 37 to 126; SD = 13.7) with 392 (12%) individuals meeting criteria for depression and 77 (2%) meeting criteria for generalized anxiety disorder. Adversity count and continuous psychological health were modestly negatively correlated (r = −0.20). With regard to resilience status, among those with adversity, 15% of the sample had favorable psychological functioning, and 38% had unfavorable psychological functioning; among those without adversity, 28% had unfavorable psychological functioning, and 18% had favorable psychological functioning.
Across follow-up, 713 individuals experienced an incident cardiometabolic condition (44 were cardiometabolic-related deaths). Frequently reported conditions included diabetes (n = 380), heart attack (n = 155), stroke (n = 136), and coronary artery disease (n = 133), with fewer reports of heart failure (n = 30). There was moderate comorbidity, with 132 individuals reporting ≥2 incident cardiometabolic conditions.
Psychological Resilience and Incident Cardiometabolic Conditions.
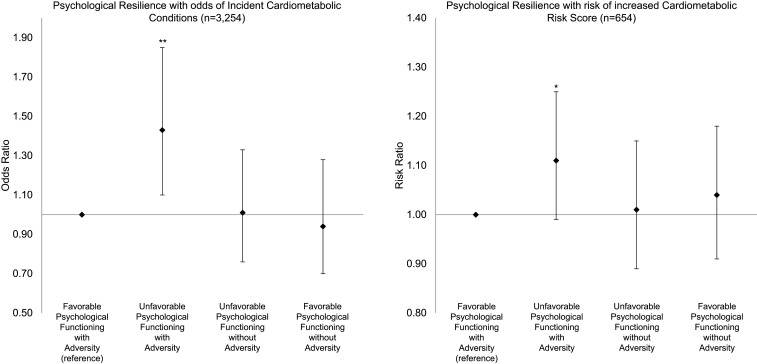
Associations between psychological resilience and incident cardiometabolic conditions are presented in Fig. 1 (estimates in SI Appendix, Table S1). Odds of developing cardiometabolic conditions among resilient individuals did not significantly differ compared to those unexposed to adversity, with or without favorable psychological functioning. Among those exposed to adversity, unfavorable versus favorable psychological functioning was associated with 43% higher odds of incident cardiometabolic conditions, adjusting for sociodemographic confounders (M1: adjusted Odds Ratio (aOR)unfavorable PF with adversity = 1.43, 95% CI 1.10 to 1.85). The odds remained elevated but attenuated slightly when adjusting for adult circumstances (M2) and further when adjusting for adult BMI and health behaviors (M3).
Fig. 1.
Associations between psychological resilience with cardiometabolic conditions and cardiometabolic risk score. Odds ratios represent odds of developing incident cardiometabolic conditions across follow-up for each resilience group relative to the group reporting Favorable Psychological Functioning with Adversity (reference group); odds ratios > 1 represent elevated odds of incident cardiometabolic conditions. Risk ratios represent risk of elevated cardiometabolic risk scores for each resilience group relative to the group reporting Favorable Psychological Functioning with Adversity (reference group); risk ratios >1 represent elevated risk of higher cardiometabolic risk scores. Models are adjusted for sociodemographics (age, sex, race/ethnicity, parental education attainment, financial level growing up, and family history of cardiovascular disease). **P < 0.05; *P < 0.10
Findings were similar when considering associations of continuous adversity and psychological health measures with incident cardiometabolic conditions (SI Appendix, Table S3). Each additional adversity exposure was associated with 15% higher odds of developing cardiometabolic conditions, adjusting for sociodemographics confounders (M1: aORadversity = 1.15, 95% CI 1.05 to 1.26). Conversely, each unit increase in psychological health associated with 10% lower odds of incident cardiometabolic conditions (M1: aORpsychological health = 0.90, 95% CI 0.86 to 0.93). In models accounting for both adversity and psychological health, the association of incident cardiometabolic conditions with adversity was slightly attenuated and with psychological health was largely unchanged. The interaction was not statistically significant, indicating no multiplicative effect of adversity by psychological health. When examining psychological health components separately, depression and wellbeing were associated with higher odds of cardiometabolic conditions when adjusting for adversity (SI Appendix, Table S5).
Psychological Resilience and Biological Cardiometabolic Risk.
Among the biomarker subsample (n = 654), mean cardiometabolic risk score was 3.68 (SD = 2.0). Relative to the analytic sample, individuals in the biomarker subsample were younger, had higher SES, lower BMI, and healthier behaviors, but the proportion of individuals in each resilience group was comparable. A higher cardiometabolic risk score was associated with higher odds of developing cardiometabolic conditions (aOR = 1.61, 95% CI 1.41 to 1.84, age, sex, and race/ethnicity adjusted).
Likelihood of having a higher cardiometabolic risk score was greater for those with unfavorable versus favorable psychological functioning among adversity-exposed individuals (M2: RR unfavorable PF with adversity = 1.13, 95% CI 1.01 to 1.27) but did not differ comparing resilient individuals with those unexposed to adversity who had either unfavorable or favorable psychological functioning when adjusting for sociodemographic confounders and adult circumstances (Fig. 1 and SI Appendix, Table S2). Considering continuous adversity and psychological health with cardiometabolic risk (SI Appendix, Table S4), effects were modest; however, adversity and psychological health were each associated with likelihood of elevated cardiometabolic risk in expected directions (M1: aORadversity = 1.03, 95% CI 0.98 to 1.08; aORpsychological health = 0.98, 95% CI 0.97 to 1.00). When coadjusting adversity and psychological health, independent effects remained largely similar. Patterns were similar when disaggregating psychological health components (SI Appendix, Table S6).
Discussion
We examined whether being more versus less psychologically resilient to early adversity was associated with lower likelihood of developing cardiometabolic conditions across 20 y of follow-up in mid-late adulthood. Findings largely support our hypotheses; odds of developing cardiometabolic conditions did not differ substantially between resilient and unexposed, psychologically healthy individuals. Individuals who experienced adversity with unfavorable psychological functioning had the highest odds of developing cardiometabolic conditions. Interestingly, individuals with poor psychological health without early adversity did not demonstrate increased cardiometabolic risk, suggesting the combination of early adversity and later poor psychological health may be more damaging than poor psychological health alone. Such findings accord with other work on trauma and severe psychological distress (e.g., posttraumatic stress disorder) in relation to cardiometabolic disease risk (38).
When considered continuously, adversity was associated with increased odds of developing cardiometabolic conditions and psychological health with decreased odds, each in a graded fashion. We did not find a multiplicative interaction between adversity and psychological health on likelihood of cardiometabolic conditions—effects of adversity did not depend on the effects of psychological health for cardiometabolic conditions or biological risk. Findings suggest early adversity and later psychological health may have independent effects on cardiometabolic health. Despite the lack of multiplicative interaction, the complementary person-focused findings do indicate relevant differences across groups categorized by levels of adversity exposure, clinically elevated distress, and psychological wellbeing. Indeed, while continuous and categorical resilience operationalizations relied on the same underlying constructs, the more-stringent criteria for categorical resilience may have identified specific subgroups of particular relevance. While we focused on resilience as a construct encapsulating both early adversity and manifesting psychological health, an important related question for future research is whether and to what extent psychological health is mediating the effects of early adversity on later cardiometabolic health.
Our evaluation of an objective measure of cardiometabolic risk derived from eight biomarkers largely mirrored our primary findings. Higher adversity count was associated with elevated risk, while better psychological health was associated with decreased risk. Furthermore, among those adversity-exposed, those with unfavorable psychological functioning had increased cardiometabolic risk versus those with favorable psychological functioning. These findings are also consistent with prior work in MIDUS considering psychological factors in relation to individual or sets of biomarkers. For example, child abuse was associated with greater dysregulation across 28 biomarkers (39), and wellbeing trajectories over 10 y were associated with healthier lipid levels (40). Our analyses extend these findings by considering adversity and psychological health concurrently, capturing potential protective effects of resilience.
Our results suggest that resilience may disrupt the effect of adversity on cardiometabolic risk, evident with self-reported cardiometabolic conditions (potentially subject to common method variance) and objectively assessed indicators. Despite different operationalizations of psychological resilience, our findings of increased cardiometabolic risk among adversity-exposed individuals with unfavorable psychological functioning (i.e., nonresilient individuals) are similar to prior longitudinal studies, where lower stress resilience increased risk of cardiometabolic outcomes (8–10). One other longitudinal study of 1,662 older adults defined resilience as being trauma exposed but not showing re-experiencing symptoms, a hallmark of posttraumatic stress disorder (7). In contrast to our findings, this study found both resilient and nonresilient (trauma exposed with re-experiencing symptoms) individuals had increased risk of cardio-ischemic disease relative to trauma-unexposed individuals, with resilient and nonresilient exhibiting comparable risk (7). However, our current study used a more-comprehensive and stringent definition of psychological health (i.e., low distress and high wellbeing), which may in part account for differences in findings.
Prior research suggests early adversity and psychological distress increase cardiometabolic risk through physiological dysregulation (e.g., hypothalamic–pituitary–adrenal axis dysfunction) and unhealthy behaviors (e.g., smoking and physical inactivity) (2). Psychological resilience may disrupt these pathways; lowering distress may decrease physiological dysregulation and promote more-healthful behavior. In our analyses, adjusting for baseline BMI and health behaviors attenuated the increased cardiometabolic risk in nonresilient individuals, suggesting that some of the effect of resilience on cardiometabolic conditions may be mediated through more-unfavorable levels of these biobehavioral factors in those nonresilient.
This study had several limitations. First, self-reported cardiometabolic conditions were subject to reporting biases; however, self-reports of serious health conditions are generally accurate (41). Additionally, we replicated our findings using objectively assessed biomarkers suggesting that self-report biases are unlikely to explain identified associations. Second, early adversity was retrospectively reported in adulthood, potentially subject to recall bias, and included only four types of adversity. Retrospective childhood adversity is often underreported (42), thus may bias estimates toward the null if underreporting is nondifferential. Furthermore, as we were unable to capture a broader range of early adversities, we are likely underestimating overall adversity exposure. Third, psychological health was assessed once in adulthood. Given the dynamic nature of psychological health and resilience, misclassification was possible. Fourth, there was significant attrition, and those excluded differed in important ways from the analytic sample. These concerns are somewhat mitigated, as we utilized inverse probability weighting to account for potential selection bias and attrition. Fifth, although MIDUS includes a large sample of community-dwelling US adults, the cohort is largely white with relatively high SES, limiting generalizability.
We provide prospective evidence that psychological resilience may protect against harmful cardiometabolic effects of early adversity in a large, community-based sample. Manifesting psychological health despite early adversity may be an important target for prevention and intervention efforts to decrease cardiometabolic disease burden in adulthood. While psychological resilience is a desirable endpoint in its own right, promotion of psychological resilience may extend to support physical health across the life course.
Supplementary Material
Acknowledgments
We thank the staff and participants of the MIDUS Study for their important contributions. Publicly available data from the MIDUS study was used for this research. Since 1995, the MIDUS study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), and National Institute on Aging (U19-AG051426). The biomarker data collection was further supported by the NIH National Center for Advancing Translational Sciences Clinical and Translational Science Award program as follows: UL1TR001409 (Georgetown), UL1TR001881 (University of California, Los Angeles), and 1UL1RR025011 (University of Wisconsin–Madison). K.M.N. was supported by National Institute of Mental Health T32 MH017119, the Lee Kum Sheung Center for Health and Happiness Dissertation Research Award, and the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the San Francisco Veterans Affairs Healthcare System (SFVAHCS), and the Department of Veterans Affairs Sierra-Pacific Mental Illness Research, Education, and Clinical Center (MIRECC). B.A.C. was supported by NIH ES000002.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2102619118/-/DCSupplemental.
Data Availability
Previously published data were used for this work (http://midus.wisc.edu/data/index.php) (43–47).
References
- 1.Kahn R., Robertson R. M., Smith R., Eddy D., The impact of prevention on reducing the burden of cardiovascular disease. Diabetes Care 31, 1686–1696 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suglia S. F., et al., Childhood and adolescent adversity and cardiometabolic outcomes: A scientific statement from the American Heart Association. Circulation 137, e15–e28 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cicchetti D., Valentino K., “An ecological-transactional perspective on child maltreatment: Failure of the average expectable environment and its influence on child development” in Risk, Disorder, and Adaptation, Cicchetti D., Cohen D. J., Eds. (Wiley, 2006), pp. 129–201. [Google Scholar]
- 4.Merrick M. T., et al., Vital signs: Estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention—25 States, 2015–2017. MMWR Morb. Mortal. Wkly. Rep. 68, 999–1005 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luthar S. S., Cicchetti D., Becker B., The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 71, 543–562 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonanno G. A., Mancini A. D., The human capacity to thrive in the face of potential trauma. Pediatrics 121, 369–375 (2008). [DOI] [PubMed] [Google Scholar]
- 7.Chaudieu I., et al., Late-life health consequences of exposure to trauma in a general elderly population: The mediating role of reexperiencing posttraumatic symptoms. J. Clin. Psychiatry 72, 929–935 (2011). [DOI] [PubMed] [Google Scholar]
- 8.Bergh C., et al., Stress resilience in male adolescents and subsequent stroke risk: Cohort study. J. Neurol. Neurosurg. Psychiatry 85, 1331–1336 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergh C., Udumyan R., Fall K., Almroth H., Montgomery S., Stress resilience and physical fitness in adolescence and risk of coronary heart disease in middle age. Heart 101, 623–629 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crump C., Sundquist J., Winkleby M. A., Sundquist K., Stress resilience and subsequent risk of type 2 diabetes in 1.5 million young men. Diabetologia 59, 728–733 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nilaweera D., et al., The long-term consequences of trauma and posttraumatic stress disorder symptoms on later life cognitive function and dementia risk. Psychiatry Res. 294, 113506 (2020). [DOI] [PubMed] [Google Scholar]
- 12.Friedman E. M., Montez J. K., Sheehan C. M., Guenewald T. L., Seeman T. E., Childhood adversities and adult cardiometabolic health: Does the quantity, timing, and type of adversity matter? J. Aging Health 27, 1311–1338 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsenkova V. K., Karlamangla A., Depression amplifies the influence of central obesity on 10-year incidence of diabetes: Findings from MIDUS. PLoS One 11, e0164802 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keyes C. L. M., Chronic physical conditions and aging: Is mental health a potential protective factor? Ageing Int. 30, 88–104 (2005). [Google Scholar]
- 15.Choi K. W., Stein M. B., Dunn E. C., Koenen K. C., Smoller J. W., Genomics and psychological resilience: A research agenda. Mol. Psychiatry 24, 1770–1778 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masten A. S., et al., Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Dev. Psychopathol. 11, 143–169 (1999). [DOI] [PubMed] [Google Scholar]
- 17.Kubzansky L., Boehm J. K., Segerstrom S. C., Positive psychological functioning and the biology of health. Soc. Personal. Psychol. Compass 9, 645–660 (2015). [Google Scholar]
- 18.Brim O. G., Ryff C. D., Kessler R. C., "The MIDUS National Survey: An overview" in How Healthy Are We?: A National Study of Well-Being at Midlife (University of Chicago Press, 2004), pp. 1–34. [Google Scholar]
- 19.Dienberg Love G., Seeman T. E., Weinstein M., Ryff C. D., Bioindicators in the MIDUS national study: Protocol, measures, sample, and comparative context. J. Aging Health 22, 1059–1080 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Straus M. A., Hamby S. L., Boney-McCoy S. U. E., Sugarman D. B., The revised conflict tactics scales (CTS2). J. Fam. Issues 17, 283–316 (2016). [Google Scholar]
- 21.Evans G. W., Li D., Whipple S. S., Cumulative risk and child development. Psychol. Bull. 139, 1342–1396 (2013). [DOI] [PubMed] [Google Scholar]
- 22.McCrory C., Dooley C., Layte R., Kenny R. A., The lasting legacy of childhood adversity for disease risk in later life. Health Psychol. 34, 687–696 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Keyes C. L., The mental health continuum: From languishing to flourishing in life. J. Health Soc. Behav. 43, 207–222 (2002). [PubMed] [Google Scholar]
- 24.Westerhof G. J., Keyes C. L., Mental illness and mental health: The two continua model across the lifespan. J. Adult Dev. 17, 110–119 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonanno G. A., Diminich E. D., Annual research review: Positive adjustment to adversity—Trajectories of minimal-impact resilience and emergent resilience. J. Child Psychol. Psychiatry 54, 378–401 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler R. C., Andrews G., Mroczek D., Ustun B., Wittchen H.-U., The World Health Organization composite international diagnostic interview short-form (CIDI-SF). Int. J. Methods Psychiatr. Res. 7, 171–185 (1998). [Google Scholar]
- 27.Ryff C. D., Keyes C. L., The structure of psychological well-being revisited. J. Pers. Soc. Psychol. 69, 719–727 (1995). [DOI] [PubMed] [Google Scholar]
- 28.Pimple P., et al., Psychological distress and subsequent cardiovascular events in individuals with coronary artery disease. J. Am. Heart Assoc. 8, e011866 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Winefield H. R., Gill T. K., Taylor A. W., Pilkington R. M., Psychological well-being and psychological distress: Is it necessary to measure both? Psychol. Well-Being: Theory, Res. Pract. 2, 1–14 (2012). [Google Scholar]
- 30.Bowen E., The impact of intimate partner violence on preschool children’s peer problems: An analysis of risk and protective factors. Child Abuse Negl. 50, 141–150 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hopkins K. D., Shepherd C. C., Taylor C. L., Zubrick S. R., Relationships between psychosocial resilience and physical health status of western Australian urban aboriginal youth. PLoS One 10, e0145382 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wingo A. P., Fani N., Bradley B., Ressler K. J., Psychological resilience and neurocognitive performance in a traumatized community sample. Depress. Anxiety 27, 768–774 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Non A. L., et al., Childhood social disadvantage, cardiometabolic risk, and chronic disease in adulthood. Am. J. Epidemiol. 180, 263–271 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pearson T. A., et al., Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107, 499–511 (2003). [DOI] [PubMed] [Google Scholar]
- 35.King K. E., Morenoff J. D., House J. S., Neighborhood context and social disparities in cumulative biological risk factors. Psychosom. Med. 73, 572–579 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Howe C. J., Cole S. R., Lau B., Napravnik S., Eron J. J. Jr, Selection bias due to loss to follow up in cohort studies. Epidemiology 27, 91–97 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang M., Generalized estimating equations in longitudinal data analysis: A review and recent developments. Adv. Stat. 2014, 303728 (2014). [Google Scholar]
- 38.Sumner J. A., et al., Trauma exposure and posttraumatic stress disorder symptoms predict onset of cardiovascular events in women. Circulation 132, 251–259 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee C., Coe C. L., Ryff C. D., Social disadvantage, severe child abuse, and biological profiles in adulthood. J. Health Soc. Behav. 58, 371–386 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Radler B. T., Rigotti A., Ryff C. D., Persistently high psychological well-being predicts better HDL cholesterol and triglyceride levels: Findings from the midlife in the U.S. (MIDUS) longitudinal study. Lipids Health Dis. 17, 1 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okura Y., Urban L. H., Mahoney D. W., Jacobsen S. J., Rodeheffer R. J., Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J. Clin. Epidemiol. 57, 1096–1103 (2004). [DOI] [PubMed] [Google Scholar]
- 42.Hardt J., Rutter M., Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. J. Child Psychol. Psychiatry 45, 260–273 (2004). [DOI] [PubMed] [Google Scholar]
- 43.Brim O. G., et al., Midlife in the United States (MIDUS 1), 1995–1996. Inter-university Consortium for Political and Social Research [distributor], 2020-09-28. 10.3886/ICPSR02760.v19. Accessed 1 October 2017. [DOI]
- 44.Ryff C., et al., Midlife in the United States (MIDUS 2), 2004–2006. Inter-university Consortium for Political and Social Research [distributor], 2017-11-20. 10.3886/ICPSR04652.v7. Accessed 1 October 2017. [DOI]
- 45.Ryff C., et al., Midlife in the United States (MIDUS 3), 2013–2014. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2019-04-30. 10.3886/ICPSR36346.v7. Accessed 1 October 2017. [DOI]
- 46.Ryff C., et al., Midlife in the United States: Core Sample Mortality Data, 2016. Inter-university Consortium for Political and Social Research [distributor], 2020-04-28. 10.3886/ICPSR37237.v3. Accessed 1 October 2018. [DOI]
- 47.Ryff C. D., Seeman T., Weinstein M., Midlife in the United States (MIDUS 2): Biomarker Project, 2004–2009. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2019-03-27. 10.3886/ICPSR29282.v9. Accessed 1 October 2018. [DOI]
- 48.Alberti K. G., et al., Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009). [DOI] [PubMed] [Google Scholar]
- 49.O’Sullivan C. J., et al., Haemoglobin A1c (HbA1C) in non-diabetic and diabetic vascular patients. Is HbA1C an independent risk factor and predictor of adverse outcome? Eur. J. Vasc. Endovasc. Surg. 32, 188–197 (2006). [DOI] [PubMed] [Google Scholar]
- 50.Grundy S. M., et al., Detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Circulation 106, 3143–3421 (2002). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Previously published data were used for this work (http://midus.wisc.edu/data/index.php) (43–47).