Abstract
The rapid development of COVID-19 vaccines is a tremendous scientific response to the current global pandemic. However, vaccines per se do not save lives and restart economies. Their success depends on the number of people getting vaccinated. We used a survey experiment to examine the impact on vaccine intentions of a variety of public health messages identified as particularly promising: three messages that emphasize different benefits from the vaccines (personal health, the health of others, and the recovery of local and national economies) and one message that emphasizes vaccine safety. Because people will likely be exposed to multiple messages in the real world, we also examined the effect of these messages in combination. Based on a nationally quota representative sample of 3,048 adults in the United States, our findings suggest that several forms of public messages can increase vaccine intentions, but messaging that emphasizes personal health benefits had the largest impact.
Keywords: COVID-19, vaccine hesitancy, information
The COVID-19 pandemic remains a global threat to lives, livelihoods, and lifestyles. Related deaths worldwide exceeded 2.6 million 12 mo after the World Health Organization declared the outbreak a global pandemic, and the economic costs in the United States alone are estimated at $16 trillion when accounting for health costs and lost gross domestic product (1). The rapid development of effective vaccines and their widespread distribution can greatly curtail the threat, but the potential for saving lives and livelihoods depends on how many people get vaccinated. Recent surveys suggest that 60 to 70% of United States adults intend to get a COVID-19 vaccine, which falls short of the threshold identified by public health experts for herd immunity (2, 3).
Vaccine hesitancy, however, may be malleable, enabling public information campaigns to reduce hesitancy. Studies show nearly half of hesitant people indicate they will reconsider after more information is available (2). Research preceding the COVID-19 pandemic offer mixed results about the effectiveness of information on vaccinations in general (4–6), but recent studies suggest that public health messaging may increase COVID-19 vaccinations. Messages about vaccine safety (7, 8), benefits to self (9) and others (8–10), as well as vaccines allowing life to return to normal (8) have been found to increase intended or actual vaccinations for the studied population as a whole or for subgroups.
However, it is unclear what messages have the greatest effect on vaccinations, and whether it is important to emphasize one message or if combinations of multiple messages aimed to encourage vaccinations may be more or less effective. We examined what message, or combination of messages, generated the largest effect on COVID-19 vaccine intentions. The COVID-19 vaccine presents a novel context to study hesitancy because of the speed of the vaccine development and political polarization related to the pandemic and the vaccine. We focused on messages that appeal to motivations to take or abstain from taking vaccines (e.g., rather than to psychological effects) (11), and identified messages with particularly high potential to increase COVID-19 vaccinations, based on literature that examines messages aimed to boost childhood vaccines (12) and other COVID-19 preventive behavior (13), as well as worries that deter COVID-19 preventive behavior (14, 15).
We compared three messages that described the benefits from taking the vaccine—benefits from vaccination to personal health; benefits to the health of family, friends, and community members; and benefits to local and national economies—and a fourth message that emphasized the rigor and safety protocols of the vaccine development process. Henceforth we refer to these treatments as “private benefit,” “social benefit,” “economic benefit,” and “vaccine safety” messages. We designed a survey experiment (a quota representative sample of the United States population with n = 3,048) to examine the effect on vaccine intentions from the four information treatments alone and in combinations. Participants were randomly assigned to one of nine information treatments (Table 1) and then asked about their willingness to take a vaccine.
Table 1.
Description of information treatments and number of participants in each treatment
| Treatment | Description | n |
| Control | No extra information. | 313 |
| Private benefit | Information about how health risks of COVID-19 can be avoided with vaccination. | 346 |
| Social benefit | Information about how health risks to family, friends, and community members can be avoided with vaccination. | 336 |
| Economic benefit | Information about how widespread vaccination enables economic recovery at the local and national level. | 356 |
| Vaccine safety | Information about the clinical trial and development process with an emphasis on the safety and rigor of the process. | 345 |
| Private and social benefit | Information from both the private benefit message and the social benefit message. | 343 |
| Private and economic benefit | Information from both the private benefit message and the economic benefit message. | 341 |
| Social and economic benefit | Information from both the social benefit message and the economic benefit message. | 334 |
| Private, social, and economic benefit | Information from all three benefit messages. | 334 |
Results
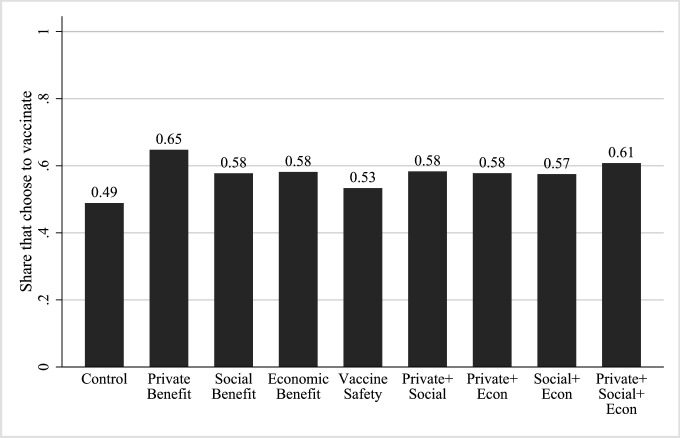
Fig. 1 shows the proportion of participants who intend to get vaccinated across treatment groups. In the control group, 49% of participants were willing to take a COVID-19 vaccine, which falls within the range of similar studies around the same time period (16). The group exposed to the private benefit message had the highest intended vaccination rate (65% vs. 49% for the control group; adjusted P < 0.001). Intentions to vaccinate among participants exposed to messages that emphasized social benefits and economic benefits were 9 percentage points higher than in the control group (adjusted P = 0.063 and 0.062, respectively). According to our results, a message that highlights private health benefits is the most effective at increasing vaccine intentions. Previous research also indicates that a private benefits message may be at least as effective as a prosocial message in boosting COVID-19 vaccinations (9). Vaccine uptake may therefore respond differently to information, compared to other behaviors that protect against COVID-19. Intentions to maintain physical distance and wear masks seem more affected by prosocial messages than by messages that emphasize personal benefits (17, 18).
Fig. 1.
Share who intends to get a COVID-19 vaccine across a control treatment, a vaccine safety information treatment, and different types of benefit information treatments.
Even though safety concerns are a primary reason for COVID-19 vaccine hesitancy (14), intentions to vaccinate were only slightly higher in the group exposed to the vaccine safety message than in the control group (53% vs. 49%; adjusted P = 0.250). Combinations of private and social benefit messages, social and economic benefit messages, and economic and private benefit messages all increased the proportion who would vaccinate by about 9 percentage points relative to the control group (adjusted P = 0.057, 0.048, and 0.068, respectively).
Intentions to vaccinate in the treatment group that received all three types of benefit messages was second highest among all groups (61%), representing a 12-percentage point increase, or 24% increase, relative to the control group (adjusted P = 0.010). Compared to the treatment that presented private benefits alone, intended vaccination rates were lower in the treatments with combined messages, although differences are not statistically significant. This suggests there are no benefits to communicating several different types of benefits (potentially due to information overload) (19).
In an exploratory analysis (not preregistered), we found some evidence of modest heterogeneity in the response of vaccine intentions to different types of information, especially across annual individual income. Low income (less than $25,000) earners responded the most to the combined social, private, and economic benefit messages; medium income ($25,000 to $99,999) earners to the private benefit message only; high income ($100,000 and above) earners to the combined social and private benefit message. If we target each income group with their most effective type of information, the overall intended vaccination rate increases by 20 percentage points, compared to 16 percentage points with the uniform private benefit message, or 12 percentage points with the combination of all benefit messages. Targeted information campaigns have been used in other health contexts with some success (20), but it is unclear whether the estimated 4- to 8-percentage point increase in vaccination rates would justify the costs of targeting the messages, especially considering the likelihood of imperfect targeting in the field.
Marginal effects from a probit model indicate that women are 8 percentage points less likely to want a vaccine, and those with low (high) trust in government agencies are 14 percentage points less (6 percentage points more) likely to want a vaccine, compared to those with medium trust. Participants who had a flu vaccine in the last 2 y are 14 percentage points more likely to want a COVID-19 vaccine, and those confident in vaccines are 24 percentage points more likely, compared to those who lack such confidence. All effects are highly statistically significant (P < 0.001). Survey responses imply that of those who do not want the vaccine, 90% worry about the vaccine’s side effects and novelty, and 75% lack trust in vaccine developers and the Food and Drug Administration to truthfully disclose a vaccine’s efficacy and risks. Our vaccine safety message did little to overcome a lack of confidence in the vaccine.
Discussion
Vaccine intentions seem responsive to information messages, which suggests that public information campaigns may boost COVID-19 vaccinations in the United States. Consistent with studies about flu and MMR vaccines (12, 21), we found the most effective message communicates private health benefits of vaccinating, which increased intended vaccinations by 16 percentage points, one-third larger than the rate of intended vaccinations in the control group. The strong response to the private benefit message may partly reflect the political polarization of vaccine hesitancy in the United States. Conservatives are more hesitant and have particularly individualistic worldview (16, 22). They might, therefore, be particularly responsive to information that stresses private benefits. Our data offer some support for this idea: the effect of the private benefit message on vaccine intentions is larger for conservatives than for moderates or liberals.
Three limitations of our study should be noted. First, we considered one-shot information treatments, which may understate the potential impact from an ongoing information campaign. Second, while we purposefully focused on messages that appeal to different motivations, messages that appeal to psychological effects (e.g., the endowment effect) also have been found to increase COVID-19 vaccinations (11). Third, we examined intentions to get vaccinated, rather than actual behavior, because the timing of the survey preceded widespread availability of COVID-19 vaccines. It has been found that vaccine intentions and actual behavior are highly correlated (23), but an intention–behavior gap has been documented in the context of flu vaccines and other health behaviors (4).
The source of information also likely matters, and trusted sources may vary across subgroups. For example, messages promoting social distancing are more effective coming from a family physician than from a governor or private citizen (24). Also, those who obtain most of their COVID-19 vaccine information from social media are the most vaccine hesitant (25), which suggests social media may be an effective information channel to target those who could most benefit from information about the vaccines. Future research may explore the effectiveness of different information channels for promoting COVID-19 vaccines.
Materials and Methods
After informed consent, study participants were exposed to one of nine information message treatments and then asked if they would take a hypothetical COVID-19 vaccine that was 85% effective in preventing symptomatic COVID-19 and had a 15% chance of causing mild side effects. See SI Appendix for a full description of the survey experiment. The study was approved by the Institutional Review Board at the University of Wyoming and preregistered in the American Economic Association’s registry for randomized controlled trials (AEARCTR-0006885). Participants were recruited by Qualtrics, with the requirement of being quota representative of the general United States population with respect to gender, age, regional residency, income, and education. Data were collected mid-December 2020 to mid-January 2021. We found no meaningful pairwise differences in normalized means of covariates across treatment groups, suggesting our randomization worked (26). To control the rate of type 1 errors when testing multiple hypotheses, we corrected for multiple comparisons using a bootstrap procedure (27). When presenting results, we show adjusted P values from Pearson χ2 tests. We have deposited data and code in openICPSR https://www.openicpsr.org/openicpsr/project/139461/version/V8/view (28).
Supplementary Material
Acknowledgments
This project was funded by the Wyoming Health and Bioscience Innovation Hub COVID Grant-1044 (Project nr: CARES-HUB3).
Footnotes
The authors declare no competing interest.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2108225118/-/DCSupplemental.
Data Availability
Original data have been deposited in openICPSR https://www.openicpsr.org/openicpsr/project/139461/version/V8/view (28).
References
- 1.Cutler D. M., Summers L. H., The COVID-19 pandemic and the $16 trillion virus. JAMA 324, 1495–1496 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Funk C., Tyson A., Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases. Pew Research Center (2020), https://www.pewresearch.org/science/2020/12/03/intent-to-get-a-covid-19-vaccine-rises-to-60-as-confidence-in-research-and-development-process-increases/. Accessed 15 February 2021.
- 3.Iboi E. A., Ngonghala C. N., Gumel A. B., Will an imperfect vaccine curtail the COVID-19 pandemic in the U.S.? Infect. Dis. Model. 5, 510–524 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bronchetti E. T., Huffman D. B., Magenheim E., Attention, intentions, and follow-through in preventive health behavior: Field experimental evidence on flu vaccination. J. Econ. Behav. Organ. 116, 270–291 (2015). [Google Scholar]
- 5.Yokum D., Lauffenburger J. C., Ghazinouri R., Choudhry N. K., Letters designed with behavioural science increase influenza vaccination in Medicare beneficiaries. Nat. Hum. Behav. 2, 743–749 (2018). [DOI] [PubMed] [Google Scholar]
- 6.Nyhan B., Reifler J., Richey S., Freed G. L., Effective messages in vaccine promotion: A randomized trial. Pediatrics 133, e835–e842 (2014). [DOI] [PubMed] [Google Scholar]
- 7.Palm R., Bolsen T., Kingsland J. T., The effect of frames on COVID-19 vaccine hesitancy. medRxiv [Preprint] (2021). 10.1101/2021.01.04.21249241. Accessed 19 January 2021. [DOI]
- 8.Hallsworth M., Mirpuri S., Toth C., Four messages that can increase uptake of the COVID-19 vaccines. Behavioural Insights (2021), https://www.bi.team/blogs/four-messages-that-can-increase-uptake-of-the-covid-19-vaccines/. Accessed 20 June 2021.
- 9.Motta M., Sylvester S., Callaghan T., Lunz-Trujillo K., Encouraging COVID-19 vaccine uptake through effective health communication. Social Science & Medicine 272, 1–8 (2021). [Google Scholar]
- 10.Duquette N., “Heard” immunity: Messages emphasizing the safety of others increase intended uptake of a COVID-19 vaccine in some groups. COVID Econ 52, 39–67 (2020). [Google Scholar]
- 11.Dai H., et al., Behavioral nudges increase COVID-19 vaccinations: Two randomized controlled trials. medRxiv [Preprint] (2021). 10.1101/2021.04.12.21254876. Accessed 20 June 2021. [DOI]
- 12.Hendrix K. S., et al., Vaccine message framing and parents’ intent to immunize their infants for MMR. Pediatrics 134, e675–e683 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherry T. L., James A. G., Murphy J., The impact of public health messaging and personal experience on the acceptance of mask wearing during the COVID-19 pandemic. J. Econ. Behav. Organ. 187, 415–430 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thunström L., Ashworth M., Finnoff D., Newbold S. C., Hesitancy toward a COVID-19 vaccine. EcoHealth, 1–17, 10.1007/s10393-021-01524-0 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Probst T. M., Lee H. J., Bazzoli A., Economic stressors and the enactment of CDC-recommended COVID-19 prevention behaviors: The impact of state-level context. J. Appl. Psychol. 105, 1397–1407 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Loomba S., de Figueiredo A., Piatek S. J., de Graaf K., Larson H. J., Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 5, 337–348 (2021). [DOI] [PubMed] [Google Scholar]
- 17.Capraro V., Barcelo H., The effect of messaging and gender on intentions to wear a face covering to slow down COVID-19 transmission. arXiv (2020), https://arxiv.org/abs/2005.05467. Accessed 11 February 2021.
- 18.Jordan J., Yoeli E., Rand D., Don’t get it or don’t spread it? Comparing self-interested versus prosocial motivations for COVID-19 prevention behaviors. PsyArXiv (2020), 10.31234/osf.io/yuq7x. Accessed 19 April 2021. [DOI] [PMC free article] [PubMed]
- 19.Siebenhaar K. U., Köther A. K., Alpers G. W., Dealing with the COVID-19 infodemic: Distress by information, information avoidance, and compliance with preventive measures. Front. Psychol. 11, 567905 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Randolph W., Viswanath K., Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annu. Rev. Public Health 25, 419–437 (2004). [DOI] [PubMed] [Google Scholar]
- 21.Milkman K. L., et al., A mega-study of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s appointment. Social Science Research Network (2021), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3780267. Accessed 19 April 2021.
- 22.Sheldon K. M., Nichols C. P., Comparing Democrats and Republicans on intrinsic and extrinsic values. J. Appl. Soc. Psychol. 39, 589–623 (2009). [Google Scholar]
- 23.Lambooij M. S., et al., Consistency between stated and revealed preferences: A discrete choice experiment and a behavioural experiment on vaccination behaviour compared. BMC Med. Res. Methodol. 15, 19 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okuhara T., Okada H., Kiuchi T., Examining persuasive message type to encourage staying at home during the COVID-19 pandemic and social lockdown: A randomized controlled study in Japan. Patient Educ. Couns. 103, 2588–2593 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy J., et al., Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 12, 29 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imbens G. W., Rubin D. B., Causal Inference for Statistics, Social, and Biomedical Sciences: An Introduction (Cambridge University Press, 2015), 10.1017/CBO9781139025751. Accessed 15 February 2021. [DOI]
- 27.List J. A., Shaikh A. M., Xu Y., Multiple hypothesis testing in experimental economics. Exp. Econ. 22, 773–793 (2019). [Google Scholar]
- 28.Ashworth M., Thunström L., Cherry T. L., Newbold S. C., Finnoff D. C., Messaging to boost COVID-19 vaccinations: emphasize personal health benefits. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. https://www.openicpsr.org/openicpsr/project/139461/version/V8/view. Deposited 28 June 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Original data have been deposited in openICPSR https://www.openicpsr.org/openicpsr/project/139461/version/V8/view (28).