Abstract
This review article summarizes the patho-anatomy of the vortex veins, the major drainage channels for the choroid, and describes the various pathways of diseases associated with vortex vein abnormalities. This report also details the technical advancements to image the vortex veins, such as ultra-widefield indocyanine green angiography, which are critical to elucidate the importance of the vortices in various retino-choroidal disorders. Future applications of these advanced imaging systems to better understand the role of the vortex veins in health and disease are also discussed.
Keywords: choroid, optical coherence tomography angiography, pachychoroid disease, ultra-widefield imaging, vortex veins
Anatomy
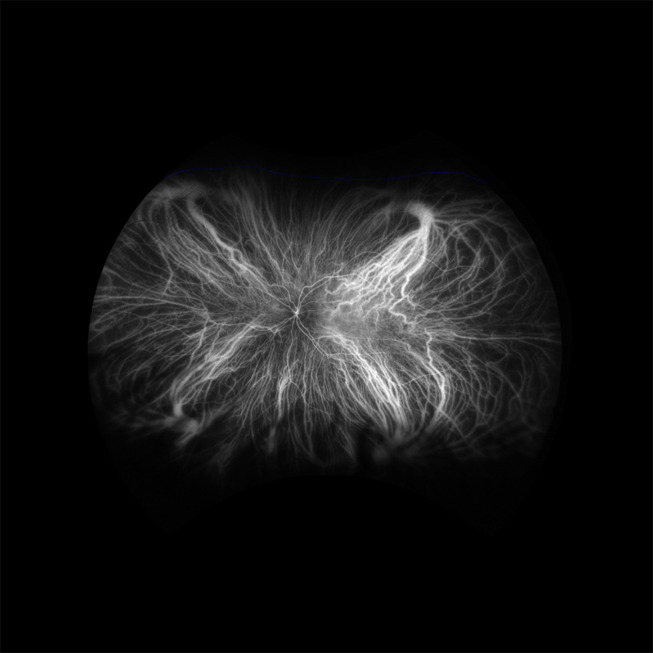
The vorticose veins, more commonly referred to as vortex veins, drain the ocular choroid. Some empty into the cavernous sinus through the superior orbital veins, whereas others drain into the pterygoid plexus through the inferior orbital veins.1 Each quadrant is traditionally thought to be associated with at least one vortex vein. When identified funduscopically, their number varies from 4 to 8, with the majority of the normal population having 4 (35%) or 5 (30%).2 Studies based on ultra-widefield indocyanine green angiography (ICGA), however, have estimated a higher average of 8 vortex veins per eye (Figure 1).3 This number includes smaller venous ampulla that would be otherwise missed on a routine fundus evaluation, as the smaller drainage channels may be invisible with ophthalmoscopic examination, as detailed later.3 There is great variability in terms of the location and number of these drainage channels in the human eye. This review highlights the importance of vortex vein imaging and its relevance for understanding normal choroidal physiology and choroidal vascular abnormalities in the context of retino-choroidal diseases.
Figure 1.
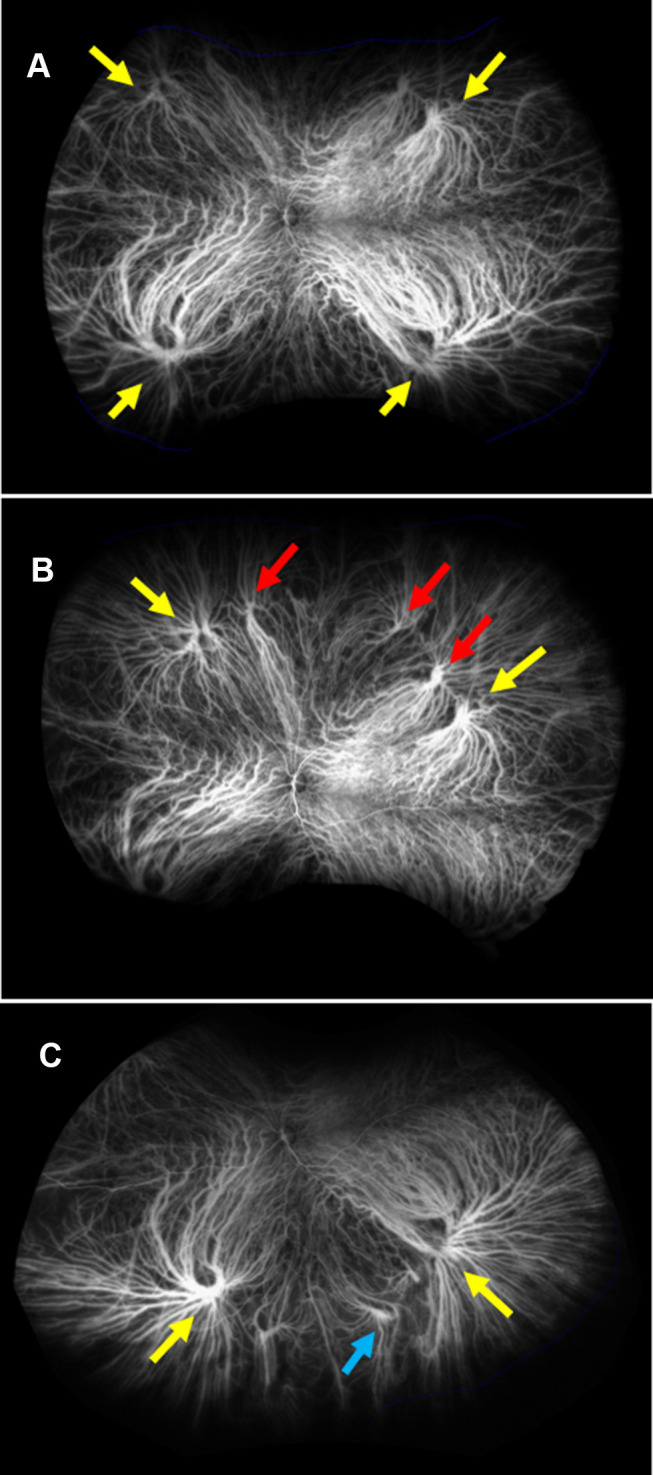
Ultra-widefield Indocyanine green angiography images depicting the presence of multiple vortex veins (yellow arrows) in a central frame (A). Superior steered (red arrows, B); and inferior steered (blue arrow, C) images revealing the presence of additional vortex veins in the same eye.
Historical Perspectives
Historically, studies on the subject of vortex veins were performed to outline the anatomic aspects and the related complications that may develop during extra-ocular muscle and scleral buckle surgeries.4–6 Most of the earlier anatomical studies analyzing vortex veins were performed on cadaver eyes. These studies demonstrated marked variations in the venous system of the orbit in humans.7 Variability was described with respect to the number of vortex veins in each quadrant, the scleral exit sites, and the distance from the nearest extra-ocular muscles.8
Vortex vein ampullae can be identified with ophthalmoscopic examination and their location serves as an important landmark to denote the equator of the globe (Figure 2). However, as these vortex veins traverse a short intra-scleral course before exiting the eye, the actual exit points are usually situated posterior to the equator. This anatomic characteristic is extremely important to keep in mind when manipulating extra-ocular muscles, as vortex veins can be inadvertently damaged during surgical manipulation. However, Hayreh in 1973 showed that experimental occlusion of less than three vortex veins did not appear to cause any deleterious effect on retinal or choroidal tissue.9 This, however, may not hold true in a clinical setting. Using ICGA, Takahishi et al demonstrated choroidal vascular remodeling and opening of new drainage channels following obstruction of the vortex vein outflow due to scleral buckle surgery, carotid cavernous sinus fistula and radiation choroidopathy.10–12 Development of inter-vortex collateral channels may explain these new drainage routes. Opening up of pre-existing, clinically invisible vortex drainage channels is another possibility, as ICGA based studies have demonstrated existence of higher number of vortex veins in healthy eyes as discussed later. In fact, in vivo studies by Hayreh et al dating back about 3 decades demonstrated that no anastomoses exist between vortex vein systems in healthy eyes under physiologic conditions.13 A detailed description of the applied anatomy of vortex veins in association with scleral buckle surgery is presented later.
Figure 2.
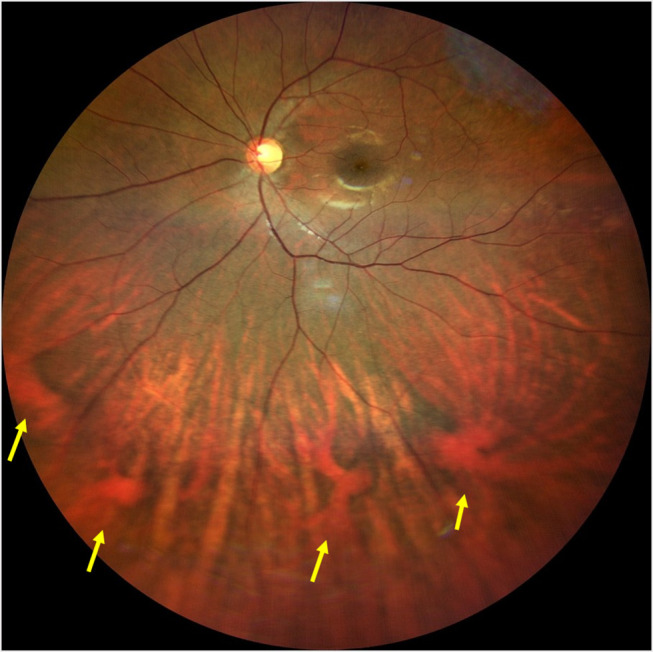
Widefield color fundus image of the left eye in a healthy patient showing the convergence of large choroidal veins to multiple vortex vein ampullae (yellow arrows) in the inferior hemisphere. The location of these ampullae roughly approximate the position of equator of the globe.
Imaging of Vortex Veins
A variety of imaging modalities have been used to characterize the vortex vein anatomy including color fundus photography, near-infrared reflectance imaging, fundus autofluorescence, fluorescein angiography, spectral-domain optical coherence tomography with enhanced depth imaging (SD-OCT + EDI), and swept source technique with deeper imaging capabilities, though ICGA may provide the best assessment.14,15 Various other imaging techniques have been employed, but these are largely research oriented.
The recent integration of ICGA on ultra-widefield (UWF) imaging platforms can facilitate assessment of the normal vortex vein anatomy (Figure 3).3 The use of stereographic projection software integrated into Optos UWF systems (Optos PLC, Dunfermline, UK) projects the peripheral and posterior segment features in corrected physical dimensions, thus allowing precise measurements to be obtained.16 Kakiuchi et al recently described a novel method of visualization of vortex veins without the need for dye injection. Their approach was based on isolating the 635nm scanning light in pseudo-color images obtained with Optos UWF systems to enhance visibility of the choroidal vessels.17 While these planar imaging techniques using the Optos UWF systems can encompass a wide field of view, they are limited by the lack of cross-sectional information. As a result, investigators have employed optical coherence tomography (OCT) and OCT angiography (OCTA) to perform depth-resolved and volumetric assessments of the retina and choroid. Choudhry et al analyzed the peripheral retinal structures using a steering based OCT technique to cover about 200 degrees of field of view.18 The vortex veins were seen as dilated hypo-reflective tubular structures in the choroid.
Figure 3.
Ultra-wide field Indocyanine green angiography image of the left eye in a young healthy adult showing the classical location of vortex vein ampulla in the superonasal, superotemporal, inferotemporal, and inferonasal quadrants. Each vortex vein appears to drain its associated quadrant.
Regardless of the imaging method employed, the number of vortex veins identified with imaging is consistently higher than the number observed during funduscopic examination. The average number observed with UWF pseudocolor montage images of healthy eyes is 8.1±1.4 in a recent study,19 whereas the UWF ICGA analysis of a healthy population revealed an average number of 8.0±2.1 vortex veins in each eye.3 This later study also uncovered some interesting facts about the distribution of vortex veins such as: vortex vein ampullae are located at an average distance of 14.2 ± 1.1 mm from the optic nerve; ampullae are never observed in the 3- and 9-o’clock meridians; and there is no relationship of the distribution or location of vortex vein ampullae with either age, gender, ethnicity or axial length. However, eyes with long axial lengths may display atypical locations of vortex veins including vortex veins exiting adjacent to the optic nerve and/or within the macula (further discussed in the section of pachychoroid diseases). The clinical significance of the number of vortex veins in an eye is discussed in the following sections.
The recently developed wide field OCT device (Canon Xephilio OCT-S1 SS-OCT, Canon Medical Systems, Zoetermeer, The Netherlands) enables the visualization of the en-face structural OCT mosaic image with a potential to show all the vortex veins. The device also has an option for OCT angiography; however, there is little information published on the OCTA characterization of vortex veins as of today.
Choroidal Blood Flow Regulation
The choroidal circulation is an important component of the blood supply to the optic nerve head.20 The blood flow in the ocular tissues is usually non-uniform as it demonstrates a pulsatile nature of flow. Also, factors like intraocular pressure variations and a thick non-compliant scleral coat result in non-uniform blood flow dynamics. Therefore, regulatory mechanisms are needed to maintain a constant supply of nutrients and oxygen in the ocular tissues. Choroidal vessels have a parasympathetic and sympathetic innervation which is thought to be relevant to the regulation of flow in these vessels.21–23 The intrascleral portions of the vortex veins, however, are also thought to be an important site of choroidal blood flow regulation.24–26 Thus, there may be a hybrid control of choroidal blood flow with local and systemic mechanisms. Understanding mechanisms of choroidal blood flow regulation including the role of vortex vein ampullae and the anatomy of vortex vein exit sites is becoming more relevant in the light of new evidence regarding choroidal influence on various retinal pathologies. These pathways may also be important considerations for the development of suprachoroidal delivery as a route for administration of therapies to the posterior segment of the eye (discussed in later section).27,28
Clinical Significance of Vortex Vein Imaging
Vortex Vein Varices
Vortex vein ampullae can become enlarged, and this enlargement is termed a varix, a benign and incidental clinical finding. It is important to recognize these varices as they must be differentiated from mass lesions such as choroidal nevi, melanoma or metastatic lesions.29–31 Historically, there have been a number of eyes enucleated due to a varix of a vortex vein ampulla that was mistaken for a uveal tumor.32–34 Advances in imaging techniques have reduced the frequency of these unnecessary enucleations in recent years.35 Also, the dynamic nature of varices (ie, increased size with valsalva maneuver, reduced size with pressure on the globe, and dynamic change with different gaze and body posture, and a predominant nasal location) may assist in identifying these lesions accurately.8,15,30,36–38 An ultrasound B-scan is usually the first step to assess these varices once detected on a routine fundus evaluation.39 With sonography, they exhibit well-defined dome-shaped elevation with high echogenicity of the retino-choroidal layer and a low internal echogenicity, and they need to be differentiated from a small melanoma or a hemorrhagic retinal pigment epithelial detachment. On SD-OCT, vortex vein varices have been described as crescent-shaped elevations with larger choroidal veins merging towards the elevation.37–39 The diagnosis of a varix can be confirmed with ICGA imaging which shows pooling of the dye in the conglomerate of ampullary veins; and a fluctuating size of the varix on changing gaze positions and with pressure on the globe.14,40 There are also reports of posteriorly located varices of vortex veins, which can be easily misdiagnosed as intraocular tumors if a clinician is unaware of the variability in the location of vortex veins.41
Uveal Effusion Syndrome: Relation to Vortex Veins
The location of vortex veins is known to limit the extension of suprachoroidal effusion, creating the lobed appearance of choroidal elevation. Uveal effusion syndrome is a condition where absence of vortex veins or increased resistance at the level of these veins can represent a possible causative factor.42 As a result, surgical decompression or unroofing of the vortex veins may be a potential therapeutic option.43 Increased scleral thickness may impose as a factor in the pathogenesis of uveal effusion resulting from choroidal congestion due to impaired venous drainage, the same etiology which has also been implicated in the development of CSC.44 Imanaga et al also investigated the scleral thickness in eyes with CSC and found thicker sclera, especially surrounding the vortex veins.26 In support of this hypothesis, researchers further reported resolution of CSC with scleral fenestration surgery.45,46 These studies suggest impairment of vortex vein drainage flow as a possible pathophysiologic mechanism in at least some eyes with diseases featuring a congested choroid.
Pachychoroid Disease
The assessment of the vortex veins may also be relevant to understanding the pathophysiology of the pachychoroid disease spectrum, particularly since there is increasing evidence suggesting choroidal venous congestion as a common pathogenic background to this complex of clinical phenotypes.47–52 Supporting the initial ICGA observations of choroidal flow abnormalities in eyes with central serous chorioretinopathy (CSC),53–57 a number of more recent OCT-based studies have demonstrated dilatation and enlargement of choroidal vessels in the Haller’s layer in eyes with pachychoroid diseases.58–61 The venous side of the choroidal circulation represents the principal setting of these vascular alterations. Hiroe and coworkers have described patterns of asymmetric choroidal venous drainage in the macula of eyes with CSC.62 Processes of vascular remodeling including formation of inter-vortex venous anastomoses (Figure 4) have also been demonstrated in eyes with pachychoroid disease,63–65 similar to what has been described in eyes with carotid cavernous fistulas or vortex vein obstruction subsequent to scleral buckle procedures.62 The exact causes of choroidal venous congestion producing these alterations are still poorly understood and the regulatory mechanisms of choroidal blood flow possibly implicated in the pathogenesis of pachychoroid disease are currently being investigated. As the only exit routes of the choroidal venous circulation from the globe, vortex vein ampullae and the intra-scleral path of vortex veins may be important sites of choroidal outflow regulation through flow resistance modulation.25 In order to investigate this postulate, scleral thickness has been evaluated in eyes with CSC and found to be greater than in healthy controls, suggesting its possible role in reducing the trans-scleral resorption of choroidal fluid and causing obstruction to the choroidal blood outflow due to the longer intrascleral path of vortex veins.26,66 The thickened sclera may also impart increased resistance due to the mechanical compression over the intra-scleral course. The ability of UWF imaging to visualize a greater portion of the fundus compared to traditional devices can be useful in analyzing pachychoroid disease-related conditions. In 2016, Pang and coworkers described dilated choroidal vessels and engorged vortex vein ampullae in UWF ICGA images of eyes with CSC, suggesting outflow congestion as a possible contributing factor to the pathogenesis of this disease.67 With binarization of UWF ICGA images, Hirahara et al demonstrated significantly higher vascular density in the choroid of eyes with CSC as compared to healthy controls, including the macular region and peripheral areas.68 These data were attributed to variable increases in choroidal vessel diameters rather than increases in overall choroidal vessel count. Jung et al quantitatively analyzed UWF ICGA images by comparing the quadrant brightness relative to a reference quadrant within the same eye and demonstrated variations in choroidal venous outflow in both normal eyes and eyes with CSC and pachychoroid pigment epitheliopathy.52 These authors proposed that increased brightness levels along the inferior quadrants may suggest venous outflow congestion among eyes with pachychoroid diseases. Jeong et al evaluated UWF ICGA images of patients with polypoidal choroidal vasculopathy (PCV) and showed greater vortex vein engorgement and increased areas of choroidal hyperpermeability in the macula compared to normal controls.69 Researchers have also utilized artificial intelligence to evaluate UWF ICGA images for classifying pachychoroid disease, and associated engorgement of the outflow channels.70 Pachychoroid neovasculopathy and type 1 macular neovascularization in eyes with pachychoroid disease phenotype are differentiated from typical age-related macular degeneration with absence of features such as soft drusen.71 These eyes exhibit a significantly higher frequency of inter-vortex venous anastomoses between the dilated superior and inferior vortex veins in the macular region.61,64,72
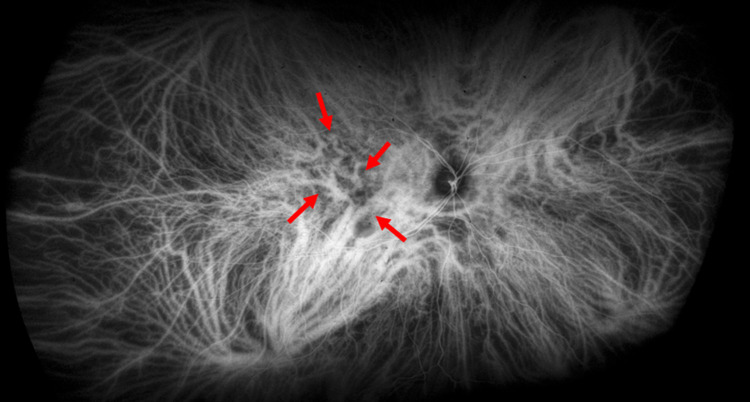
Figure 4.
Early-mid phase ultra-widefield indocyanine green angiography image of the right eye of a 38-year-old man with complex central serous chorioretinopathy. There is marked congestion of choroidal veins that appear abnormally enlarged, especially in the inferotemporal and superonasal vortex vein systems. Note the dense network of inter-vortex venous anastomoses in the macular and peripapillary region connecting the superonasal, superotemporal and inferotemporal vortex vein systems (red arrows).
Abnormalities can be present in vortex veins draining specific posterior segment sectors in eyes with pachychoroid diseases. A study by Chung et al showed the presence of engorged vortex veins in specific quadrants in eyes with polypoidal choroidal vasculopathy.73 These engorged veins were associated with increased choroidal thickness in all the eyes. Other studies have reported dilatation of choroidal vessels in the early phase of ICGA in eyes with CSC, with this dilatation evident in more than 80% of studied eyes and extending along the entire length of the vessel up to the vortex vein ampulla in the late phases of the ICGA.62,73 Overall, these reports highlight the importance of evaluating the sites of choroidal blood outflow and visualizing the entire choroidal drainage pathways, including the vortex vein ampullae, in order to better understand the pathophysiology of the pachychoroid disease spectrum (Figure 5). Resolution of inter-vortex venous anastomoses and reduced dilation of sub-macular and peripheral choroidal veins following treatment may prove to be a useful endpoint biomarker to monitor therapeutic responses in such eyes.
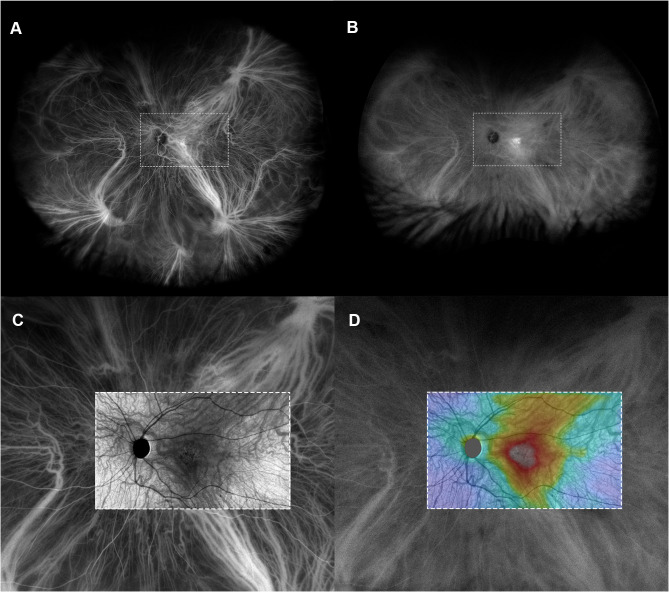
Figure 5.
(A) Early-mid phase ultra-widefield indocyanine green angiography (UWF ICGA) image of the left eye of a 57-year-old man with simple central serous chorioretinopathy. The superonasal vortex vein system appears relatively hypoplastic. Consequently, the overall choroidal venous drainage appears imbalanced, with inferior vortex vein systems draining a greater proportion of the post-equatorial fundus compared to the superior ones. Their ampullae and major venous branches appear dilated, suggesting choroidal venous congestion mostly involving the inferior quadrants. Major venous branches of the inferotemporal vortex vein system surround the optic disc and drain a large portion of the parapapillary region, not respecting the physiologic geometry of choroidal venous watersheds that usually pass horizontally through the disc and fovea, and vertically through the papillomacular region. (B) Mid-late phase UWF ICGA image of the same eye, showing choroidal vascular hyperpermeability in the macular region. Dashed boxes in (A and B) show the location of the SS-OCT scan displayed in (C and D). (C and D) Fifteen x 9 mm swept-source optical coherence tomography (SS-OCT) en face projection of structural signal and SS-OCT color-coded thickness heat map obtained segmenting the choroid from Bruch’s membrane to the choroid-scleral junction. The en face SS-OCT images are aligned and superimposed over the early-mid and mid-late UWF ICGA image displayed in (A and B), respectively, showing intervortex venous anastomoses between the temporal vortex vein systems and the area of maximal choroidal thickness corresponding to the region of choroidal vascular hyperpermeability.
Spaceflight-Associated Neuro-Ocular Syndrome
Astronauts who experience extended time (several months) in space may develop a number of abnormalities of the central nervous system and eye including ventricular enlargement in the brain, optic disc edema, enlargement of the optic nerve sheaths, choroidal thickening, a peculiar type of globe flattening, and hyperopic refractive shifts; all collectively known as spaceflight-associated neuro-ocular syndrome.74 The lack of gravitational forces associated with space travel is thought to shift the blood and cerebrospinal fluid towards the head, resulting in increased systemic venous pressure and leading to optic nerve sheath swelling, flattening of the posterior globe, and other associated features. The choroidal thickening and apparent choroidal vascular dilation in these patients may be related to engorged intrascleral vortex veins.75 These changes may persist long after termination of space flight due to permanent alteration of the choroidal blood flow physiology in these astronauts. The optic nerve congestion is also thought to derive from a reduced buffering capability of congested choroidal venous drainage channels leading to increased outflow resistance. Chronic venous insufficiency of the choroid that is thought be an important component of SANS, may also be relevant to other disorders including carotid cavernous sinus fistula and peripapillary pachychoroid syndrome.
Vortex Veins and Suprachoroidal Drug Delivery
The suprachoroidal space is being extensively investigated as a potential route for drug delivery because it targets the choroid, retinal pigment epithelium and retina with high bioavailability, while avoiding deeper intraocular penetration which can incur a greater risk of complications such as endophthalmitis, retinal detachment, and cataract formation.72 As drugs delivered to the suprachoroidal space tend to get cleared rapidly, long acting formulations enabling extended drug delivery are under evaluation.73,76,77 Understanding clearance mechanisms from the choroid and suprachoroidal space may be relevant to the development and optimization of these therapies.77,78 Although various static, dynamic and metabolic ocular barriers may be active, the effects of the choroidal circulation on drug clearance mechanisms are not yet clearly elucidated due to the difficulty in isolating the choroidal circulation in experimental studies.78 The high blood flow in the choroid may act as a sink causing faster drug clearance from the suprachoroidal space.79 In experimental eyes, with large amounts of drug injected into the suprachoroidal space, investigators have observed drug leakage through openings on the surface of the eye corresponding to vortex vein exit sites.80 Vortex veins and the sites of ciliary artery penetrance may also be associated with the circumferential spreading of suprachoroidal-delivered formulations.81 For these reasons, a precise localization of posterior ciliary arteries and vortex veins may be important for selecting the best possible injection strategies of suprachoroidal drug delivery to ensure adequate distribution of the drug to the desired site of action.
Vortex Veins as a Possible Site of Complication During Surgery
Since the introduction of scleral buckle surgery for repair of rhegmatogenous retinal detachment, a known complication is injury to the vortex veins with associated clinical sequelae such as choroidal detachment, vitreous opacities, vitreous hemorrhage and elevated intra-ocular pressure.5 A retina surgeon must be aware of the possible variations in vortex vein locations in order to avoid these complications.4,5,7 Aside from surgical perforation, vortex veins are also susceptible to directly compression by bulky buckle elements. Takahishi et al studied the remodeling of choroidal drainage after vortex vein occlusion in sclera buckle surgeries using ICGA.10 The same group previously studied the remodeling effect on venous drainage of other choroidal diseases, as mentioned previously.11,12 They reported the formation of compensatory drainage routes 3 months after surgery. The authors postulate the formation of inter-vortex venous anastomoses or newer collateral channels as the possible mechanism for this vascular remodeling. Some of the smaller vortex vein channels evident on UWF ICGA may form the substrate for these choroidal collateral routes in cases where the larger ampullar trunk is damaged during the surgical procedure. The recent UWF ICGA studies showing a higher number of vortex vein ampullae than that previously described support this concept.3 The smaller clinically invisible ampullae may assume a larger role in drainage following occlusion of one or more larger channels. In support of this, as noted above, experimental occlusion of fewer than 3 vortex veins in previous studies showed no deleterious effects on retinal or choroidal tissue, indicating the maintained patency of the outflow pathways.9 We would speculate that the presence or opening up of smaller vortex vein channels in the same quadrants as the occluded larger veins may justify this observation.
Vortex vein injury can be associated with peri-operative and post-operative complications. Suprachoroidal buckling is a rarely used technique to repair rhegmatogenous retinal detachment, where injection of viscoelastic material into the suprachoroidal space is used to create a chorioretinal adhesion and closure of the retinal break.82,83 A possible complication resulting from direct damage to the vortex vein during this procedure is suprachoroidal hemorrhage, which is thought to result from injury to this highly vascular region of the choroid.84 Furthermore, a recent report has associated a vortex vein varix with recurrent suprachoroidal hemorrhage which occurred in close proximity to the varix.85 A better understanding of vortex vein anatomy and its variations in healthy and diseased states may curb the unnecessary investigations by retinal surgeons dealing with such eyes.
In summary, advances in imaging techniques, in particular UWF ICGA, has allowed improved in vivo visualization of the vortex veins and a better evaluation of the choroidal drainage system in its complexity. These choroidal outflow pathways may affect the pathophysiology and/or the expression of various posterior segment diseases with great impact on the general population. The advent of therapeutics delivered to the suprachoroidal space further highlights the importance of understanding choroidal drainage pathways.
Funding Statement
There is no funding for this review article.
Abbreviations
CSC, Central Serous Chorioretinopathy; ICGA, Indocyanine Green Angiography; OCT, Optical Coherence Tomography; OCTA, Optical Coherence Tomography Angiography; UWF, Ultra-widefield.
Data Sharing Statement
This is a review article and therefore, data availability policy is not applicable.
Ethics Approval and Informed Consent
This is a review paper and no ethics approval is needed.
Consent for Publication
The details of the images attached with the manuscript can be published, and all the co-authors have provided consent for the article contents to be published. Authors are prepared to provide copies of signed consent forms to the journal editorial office if requested.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr David Sarraf report grants, personal fees from Amgen, personal fees from Bayer, grants from Genentech, non-financial support from Heidelberg, personal fees from Novartis, personal fees, non-financial support from Optovue, grants from Regeneron, non-financial support from Topcon, personal fees from Iveric Bio, outside the submitted work; Dr K Bailey Freund report personal fees from Heidelberg Engineering, personal fees from Carl Zeiss Meditec, during the conduct of the study; grants, personal fees from Genentech, Inc., Roche, personal fees from Allergan, personal fees from Bayer HealthCare, personal fees from Regeneron, outside the submitted work; Dr Srinivas R Sadda report personal fees from Amgen, personal fees from Apellis, personal fees from Allergan, non-financial support from Carl Zeiss Meditec, non-financial support from Centervue, personal fees, non-financial support from Heidelberg Engineering, personal fees, non-financial support from Optos, personal fees, non-financial support from Nidek, personal fees, non-financial support from Topcon, personal fees from Bayer, personal fees from Novartis, personal fees from Roche/Genentech, personal fees from Oxurion, personal fees from 4DMT, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Brismar J. Orbital phlebography. II. Anatomy of superior ophthalmic vein and its tributaries. Acta Radiol Diagn. 1974;15(5):481–496. doi: 10.1177/028418517401500503 [DOI] [PubMed] [Google Scholar]
- 2.Kutoglu T, Yalcin B, Kocabiyik N, Ozan H. Vortex veins: anatomic investigations on human eyes. Clin Anat. 2005;18(4):269–273. doi: 10.1002/ca.20092 [DOI] [PubMed] [Google Scholar]
- 3.Verma A, Maram J, Alagorie AR, et al. Distribution and location of vortex vein ampullae in healthy human eyes as assessed by ultra-widefield indocyanine green angiography. Ophthalmol Retina. 2020;4(5):530–534. doi: 10.1016/j.oret.2019.11.009 [DOI] [PubMed] [Google Scholar]
- 4.Robertson DM. Anterior segment ischemia after segmental episcleral buckling and cryopexy. Am J Ophthalmol. 1975;79(5):871–874. doi: 10.1016/0002-9394(75)90748-5 [DOI] [PubMed] [Google Scholar]
- 5.Doi N, Uemura A, Nakao K. Complications associated with vortex vein damage in scleral buckling surgery for rhegmatogenous retinal detachment. Jpn J Ophthalmol. 1999;43(3):232–238. doi: 10.1016/S0021-5155(99)00009-X [DOI] [PubMed] [Google Scholar]
- 6.Cheung N, McNab AA. Venous anatomy of the orbit. Invest Ophthalmol Vis Sci. 2003;44(3):988–995. doi: 10.1167/iovs.02-0865 [DOI] [PubMed] [Google Scholar]
- 7.Okamura ID, Schepens CL, Brockhurst RJ, Regan CDJ, McMeel JW. Scleral buckling procedures. IX. Complications during operation. Arch Ophthalmol. 1966;75(5):615–625. doi: 10.1001/archopht.1966.00970050617006 [DOI] [PubMed] [Google Scholar]
- 8.Lim MC, Bateman JB, Glasgow BJ. Vortex vein exit sites. Scleral coordinates. Ophthalmology. 1995;102(6):942–946. doi: 10.1016/S0161-6420(95)30930-X [DOI] [PubMed] [Google Scholar]
- 9.Hayreh SS, Baines JA. Occlusion of the vortex veins. An experimental study. Br J Ophthalmol. 1973;57(4):217–238. doi: 10.1136/bjo.57.4.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takahashi K, Kishi S. Remodeling of choroidal venous drainage after vortex vein occlusion following scleral buckling for retinal detachment. Am J Ophthalmol. 2000;129(2):191–198. doi: 10.1016/S0002-9394(99)00425-0 [DOI] [PubMed] [Google Scholar]
- 11.Sutoh N, Muraoka K, Takahashi K, Ikeda F, Shimizu K. Remodeling of choroidal circulation in carotid cavernous sinus fistula. Retina. 1996;16(6):497–504. doi: 10.1097/00006982-199616060-00005 [DOI] [PubMed] [Google Scholar]
- 12.Takahashi K, Kishi S, Muraoka K, Tanaka T, Shimizu K. Radiation choroidopathy with remodeling of the choroidal venous system. Am J Ophthalmol. 1998;125(3):367–373. doi: 10.1016/S0002-9394(99)80148-2 [DOI] [PubMed] [Google Scholar]
- 13.Hayreh SS. Physiological anatomy of the choroidal vascular bed. Lnt Ophthalmol. 1983;6(2):85–93. [DOI] [PubMed] [Google Scholar]
- 14.Veronese C, Staurenghi G, Pellegrini M, et al. Multimodal imaging in vortex vein varices. Retin Cases Brief Rep. 2019;13(3):260–265. doi: 10.1097/ICB.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 15.Yannuzzi LA. Indocyanine green angiography: a perspective on use in the clinical setting. Am J Ophthalmol. 2011;151(5):745–751. doi: 10.1016/j.ajo.2011.01.043 [DOI] [PubMed] [Google Scholar]
- 16.Tan CS, Chew MC, van Hemert J, Singer MA, Bell D, Sadda SR. Measuring the precise area of peripheral retinal non-perfusion using ultra-widefield imaging and its correlation with the ischaemic index. Br J Ophthalmol. 2015;100(2):235–239. doi: 10.1136/bjophthalmol-2015-306652 [DOI] [PubMed] [Google Scholar]
- 17.Kakiuchi N, Sonoda S, Terasaki H, et al. Choroidal vasculature from ultra-widefield images without contrast dye and its application to Vogt-Koyanagi-Harada disease. Ophthalmol Retina. 2019;3(2):161–169. doi: 10.1016/j.oret.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 18.Choudhry N, Golding J, Manry MW, Rao RC. Ultra-widefield steering-based spectral-domain optical coherence tomography imaging of the retinal periphery. Ophthalmology. 2016;123(6):1368–1374. doi: 10.1016/j.ophtha.2016.01.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Funatsu R, Sonoda S, Terasaki H, et al. An analysis of vortex veins using a 3-dimensional eye model based upon ultra-wide field images. Invest Ophthalmol Vis Sci. 2020;61(7):2233. [Google Scholar]
- 20.Spalton DJ. Microvasculature of the human optic nerve. Am J Ohthalmol. 1996;121(4):452–453. doi: 10.1016/S0002-9394(14)70449-0 [DOI] [PubMed] [Google Scholar]
- 21.Chou P, Lu DW, Chen JT. Bilateral superior cervical ganglionectomy increases choroidal blood flow in the rabbit. Ophthalmologica. 2000;214(6):421–425. doi: 10.1159/000027536 [DOI] [PubMed] [Google Scholar]
- 22.Steinle JJ, Krizsan-Agbas D, Smith PG. Regional regulation of choroidal blood flow by autonomic innervation in the rat. Am J Physiol Regul Integr Comp Physiol. 2000;279(1):R202–209. doi: 10.1152/ajpregu.2000.279.1.R202 [DOI] [PubMed] [Google Scholar]
- 23.Bill A. Aspects of the regulation of the uveal venous pressure in rabbits. Exp Eye Res. 1962;1(3):193–199. doi: 10.1016/S0014-4835(62)80001-3 [DOI] [PubMed] [Google Scholar]
- 24.Bill A. Some aspects of the ocular circulation. Friedenwald lecture. Invest Ophthalmol Vis Sci. 1985;26(4):410–424. [PubMed] [Google Scholar]
- 25.Spaide RF. Choroidal blood flow: review and potential explanation for the choroidal venous anatomy including the vortex vein system. Retina. 2020;40(10):1851–1864. doi: 10.1097/IAE.0000000000002931 [DOI] [PubMed] [Google Scholar]
- 26.Imanaga N, Terao N, Nakamine S, et al. Scleral thickness in central serous chorioretinopathy. Ophthalmol Retina. 2021;5(3):285–291. doi: 10.1016/j.oret.2020.07.011 [DOI] [PubMed] [Google Scholar]
- 27.Chiang B, Jung JH, Prausnitz MR. The suprachoroidal space as a route of administration to the posterior segment of the eye. Adv Drug Deliv Rev. 2018;126:58–66. doi: 10.1016/j.addr.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olsen TW, Feng X, Wabner K, Csaky K, Pambuccian S, Cameron JD. Pharmacokinetics of pars plana intravitreal injections versus microcannula suprachoroidal injections of bevacizumab in a porcine model. Invest Ophthalmol Vis Sci. 2011;52(7):4749–4756. doi: 10.1167/iovs.10-6291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buettner H. Varix of the vortex ampulla simulating a choroidal melanoma. Am J Ophthalmol. 1990;109(5):607–608. doi: 10.1016/S0002-9394(14)70701-9 [DOI] [PubMed] [Google Scholar]
- 30.Gündüz K, Shields CL, Shields JA. Varix of the vortex vein ampulla simulating choroidal melanoma: report of four cases. Retina. 1998;18(4):343–347. [DOI] [PubMed] [Google Scholar]
- 31.Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: the 2006 Taylor R. Smith Lecture. Retina. 2005;25(6):767–771. doi: 10.1097/00006982-200509000-00013 [DOI] [PubMed] [Google Scholar]
- 32.Ferry AP. Lesions mistaken for malignant melanoma of the posterior uvea. A clinicopathologic analysis of 100 cases with ophthalmoscopically visible lesions. Arch Ophthalmol. 1964;72:463–469. doi: 10.1001/archopht.1964.00970020463004 [DOI] [PubMed] [Google Scholar]
- 33.Shields JA, Zimmerman LE. Lesions simulating malignant melanomas of the posterior uvea. Arch Ophthalmol. 1973;89(6):466–471. doi: 10.1001/archopht.1973.01000040468004 [DOI] [PubMed] [Google Scholar]
- 34.Chang M, Zimmerman LE, McLean I. The persisting pseudomelanoma problem. Arch Ophthalmol. 1984;102(5):726–727. doi: 10.1001/archopht.1984.01040030582024 [DOI] [PubMed] [Google Scholar]
- 35.Shields JA, McDonald PR. Improvements in the diagnosis of posterior uveal melanomas. Arch Ophthalmol. 1974;91(4):259–264. doi: 10.1001/archopht.1974.03900060269004 [DOI] [PubMed] [Google Scholar]
- 36.Tomasini DN. Varix of the vortex ampulla: a dynamic phenomenon. Clin Eye Vis Care. 2000;12(3–4):151–154. doi: 10.1016/S0953-4431(00)00050-3 [DOI] [PubMed] [Google Scholar]
- 37.Levy J, Yagev R, Shelef I, Lifshitz T. Varix of the vortex vein ampulla: a small case series. Eur J Ophthalmol. 2005;15(3):424–427. doi: 10.1177/112067210501500320 [DOI] [PubMed] [Google Scholar]
- 38.Hu Y, Wang S, Dong Y, Zhou X, Yu W, Xu C. Imaging features of varix of the vortex vein ampulla: a small case series. J Clinic Exp Ophthalmol. 2011;2:2. doi: 10.4172/2155-9570.1000173 [DOI] [Google Scholar]
- 39.Singh AD, De Potter P, Shields CL, Shields JA. Indocyanine green angiography and ultrasonography of a varix of vortex vein. Arch Ophthalmol. 1993;111(9):1283–1284. doi: 10.1001/archopht.1993.01090090135031 [DOI] [PubMed] [Google Scholar]
- 40.Kang HK, Beaumont PE, Chang AA. Indocyanine green angiographic features of varix of the vortex vein ampulla. Clin Experiment Ophthalmol. 2000;28(4):321–323. doi: 10.1046/j.1442-9071.2000.00326.x [DOI] [PubMed] [Google Scholar]
- 41.Gass JD. Uveal effusion syndrome: a new hypothesis concerning pathogenesis and technique of surgical treatment. Trans Am Ophthalmol Soc. 1983;81:246. [PMC free article] [PubMed] [Google Scholar]
- 42.Brockhurst RJ. Vortex vein decompression for nanophthalmic uveal effusion. Arch Ophthalmol. 1980;98(11):1987. doi: 10.1001/archopht.1980.01020040839008 [DOI] [PubMed] [Google Scholar]
- 43.Terao N, Koizumi H, Kojima K, et al. Short axial length and hyperopic refractive error are risk factors of central serous chorioretinopathy. Br J Ophthalmol. 2020;104(9):1260–1265. [DOI] [PubMed] [Google Scholar]
- 44.Venkatesh P, Chawla R, Tripathy K, Singh HI, Bypareddy R. Scleral resection in chronic central serous chorioretinopathy complicated by exudative retinal detachment. Eye Vis. 2016;3(1):23. doi: 10.1186/s40662-016-0055-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maggio E, Mete M, Maraone G, Arena F, Pertile G. Scleral thinning surgery for bullous retinal detachment with retinal pigment epithelial tear in central serous chorioretinopathy: a case report. BMC Ophthalmol. 2020;20(1):133. doi: 10.1186/s12886-020-01409-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghadiali Q, Tan A, Freund KB. Unusual posterior varix of a vortex vein ampulla. Retin Cases Brief Rep. 2017;11(Suppl 1):S163–S165. doi: 10.1097/ICB.0000000000000401 [DOI] [PubMed] [Google Scholar]
- 47.Cheung CMG, Lee WK, Koizumi H, Dansingani K, Lai TYY, Freund KB. Pachychoroid disease. Eye. 2019;33(1):14–33. doi: 10.1038/s41433-018-0158-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freund KB, Fine HF. Pachychoroid disease. Ophthalmic Surg Lasers Imaging Retina. 2020;51(4):206–209. doi: 10.3928/23258160-20200326-01 [DOI] [PubMed] [Google Scholar]
- 49.Yanagi Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol. 2020;64(4):323–337. doi: 10.1007/s10384-020-00740-5 [DOI] [PubMed] [Google Scholar]
- 50.Kaye R, Chandra S, Sheth J, Boon CJF, Sivaprasad S, Lotery A. Central serous chorioretinopathy: an update on risk factors, pathophysiology and imaging modalities. Prog Retin Eye Res. 2020;79:100865. [DOI] [PubMed] [Google Scholar]
- 51.Castro-Navarro V, Behar-Cohen F, Chang W, et al. Pachychoroid: current concepts on clinical features and pathogenesis. Graefes Arch Clin Exp Ophthalmol. 2020. doi: 10.1007/s00417-020-04940-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jung JJ, Yu DJG, Ito K, Rofagha S, Lee SS, Hoang QV. Quantitative assessment of asymmetric choroidal outflow in pachychoroid eyes on ultra-widefield indocyanine green angiography. Invest Ophthalmol Vis Sci. 2020;61(8):50. doi: 10.1167/iovs.61.8.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hayashi K, Hasegawa Y, Tokoro T. Indocyanine green angiography of central serous chorioretinopathy. Int Ophthalmol. 1986;9(1):37–41. doi: 10.1007/BF00225936 [DOI] [PubMed] [Google Scholar]
- 54.Scheider A, Nasemann JE, Lund O-E. Fluorescein and indocyanine green angiographies of central serous choroidopathy by scanning laser ophthalmoscopy. Am J Ophthalmol. 1993;115(1):50–56. doi: 10.1016/S0002-9394(14)73524-X [DOI] [PubMed] [Google Scholar]
- 55.Piccolino FC, Borgia L. Central serous chorioretinopathy and indocyanine green angiography. Retina. 1994;14(3):231–242. doi: 10.1097/00006982-199414030-00008 [DOI] [PubMed] [Google Scholar]
- 56.Prünte C, Flammer J. Choroidal capillary and venous congestion in central serous chorioretinopathy. Am J Ophthalmol. 1996;121(1):26–34. doi: 10.1016/S0002-9394(14)70531-8 [DOI] [PubMed] [Google Scholar]
- 57.Iida T, Kishi S, Hagimura N, Shimizu K. Persistent and bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina. 1999;19(6):508–512. doi: 10.1097/00006982-199919060-00005 [DOI] [PubMed] [Google Scholar]
- 58.Imamura Y, Fujiwara T, Margolis R, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29(10):1469–1473. doi: 10.1097/IAE.0b013e3181be0a83 [DOI] [PubMed] [Google Scholar]
- 59.Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T. Subfoveal choroidal thickness in fellow eyes of patients with central serous chorioretinopathy. Retina. 2011;31(8):1603–1608. doi: 10.1097/IAE.0b013e31820f4b39 [DOI] [PubMed] [Google Scholar]
- 60.Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF. Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology. 2010;117(9):1792–1799. doi: 10.1016/j.ophtha.2010.01.023 [DOI] [PubMed] [Google Scholar]
- 61.Dansingani KK, Balaratnasingam C, Naysan J, Freund KB. En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina. 2016;36(3):499–516. doi: 10.1097/IAE.0000000000000742 [DOI] [PubMed] [Google Scholar]
- 62.Hiroe T, Kishi S. Dilatation of asymmetric vortex vein in central serous chorioretinopathy. Ophthalmol Retina. 2018;2(2):152–161. doi: 10.1016/j.oret.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 63.Matsumoto H, Hoshino J, Arai Y, et al. Quantitative measures of vortex veins in the posterior pole in eyes with pachychoroid spectrum diseases. Sci Rep. 2020;10:19505. doi: 10.1038/s41598-020-75789-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matsumoto H, Hoshino J, Mukai R, et al. Vortex vein anastomosis at the watershed in pachychoroid spectrum diseases. Ophthalmol Retina. 2020;4(9):938–945. doi: 10.1016/j.oret.2020.03.024 [DOI] [PubMed] [Google Scholar]
- 65.Spaide RF, Ledesma-Gil G, Gemmy cheung CM. Intervortex venous anastomosis in pachychoroid-related disorders. Retina. 2021;41(5):997–1004. doi: 10.1097/IAE.0000000000003004 [DOI] [PubMed] [Google Scholar]
- 66.Lee YJ, Lee YJ, Lee JY, Lee S. A pilot study of scleral thickness in central serous chorioretinopathy using anterior segment optical coherence tomography. Sci Rep. 2021;11(1):5872. doi: 10.1038/s41598-021-85229-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pang CE, Shah VP, Sarraf D, Freund KB. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol. 2014;158(2):362–371.e2. doi: 10.1016/j.ajo.2014.04.021 [DOI] [PubMed] [Google Scholar]
- 68.Hirahara S, Yasukawa T, Kominami A, Nozaki M, Ogura Y. Densitometry of choroidal vessels in eyes with and without central serous chorioretinopathy by wide-field indocyanine green angiography. Am J Ophthalmol. 2016;166:103–111. doi: 10.1016/j.ajo.2016.03.040 [DOI] [PubMed] [Google Scholar]
- 69.Jeong A, Lim J, Sagong M. Choroidal vascular abnormalities by ultra-widefield indocyanine green angiography in polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2021;62(2):29. doi: 10.1167/iovs.62.2.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim IK, Lee K, Park JH, Baek J, Lee WK. Classification of pachychoroid disease on ultrawide-field indocyanine green angiography using auto-machine learning platform. Br J Ophthalmol. 2021;105:856–861. doi: 10.1136/bjophthalmol-2020-316108 [DOI] [PubMed] [Google Scholar]
- 71.Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35(1):1–9. doi: 10.1097/IAE.0000000000000331 [DOI] [PubMed] [Google Scholar]
- 72.Matsumoto H, Kishi S, Mukai R, Akiyama H. Remodeling of macular vortex veins in pachychoroid neovasculopathy. Sci Rep. 2019;9(1):14689. doi: 10.1038/s41598-019-51268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chung SE, Kang SW, Kim JH, et al. Engorgement of vortex vein and polypoidal choroidal vasculopathy. Retina. 2013;33(4):834–840. doi: 10.1097/IAE.0b013e31826af540 [DOI] [PubMed] [Google Scholar]
- 74.Zhang LF, Hargens AR. Spaceflight-induced intracranial hypertension and visual impairment: pathophysiology and countermeasures. Physiol Rev. 2018;98(1):59–87. doi: 10.1152/physrev.00017.2016 [DOI] [PubMed] [Google Scholar]
- 75.Nelson ES, Mulugeta L, Myers JG. Microgravity-induced fluid shift and ophthalmic changes. Life. 2014;4(4):621–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang M, Liu W, Lu Q, et al. Pharmacokinetic comparison of ketorolac after intracameral, intravitreal, and suprachoroidal administration in rabbits. Retina. 2012;32(10):2158–2164. doi: 10.1097/IAE.0b013e3182576d1d [DOI] [PubMed] [Google Scholar]
- 77.Abarca EM, Salmon JH, Gilger BC. Effect of choroidal perfusion on ocular tissue distribution after intravitreal or suprachoroidal injection in an arterially perfused ex vivo pig eye model. J Ocul Pharmacol Ther. 2013;29(8):715–722. doi: 10.1089/jop.2013.0063 [DOI] [PubMed] [Google Scholar]
- 78.Kim SH, Galbán CJ, Lutz RJ, et al. Assessment of subconjunctival and intrascleral drug delivery to the posterior segment using dynamic contrast-enhanced magnetic resonance imaging. Invest Ophthalmol Vis Sci. 2007;48(2):808–814. doi: 10.1167/iovs.06-0670 [DOI] [PubMed] [Google Scholar]
- 79.Amrite AC, Edelhauser HF, Singh SR, Kompella UB. Effect of circulation on the disposition and ocular tissue distribution of 20 nm nanoparticles after periocular administration. Mol Vis. 2008;14:150–160. [PMC free article] [PubMed] [Google Scholar]
- 80.Patel SR, Lin AS, Edelhauser HF, Prausnitz MR. Suprachoroidal drug delivery to the back of the eye using hollow microneedles. Pharm Res. 2011;28(1):166–176. doi: 10.1007/s11095-010-0271-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chiang B, Kim YC, Edelhauser HF, Prausnitz MR. Circumferential flow of particles in the suprachoroidal space is impeded by the posterior ciliary arteries. Exp Eye Res. 2016;145:424–431. doi: 10.1016/j.exer.2016.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.El Rayes EN, Mikhail M, El Cheweiky H, Elsawah K, Maia A. Suprachoroidal buckling for the management of rhegmatogenous retinal detachments secondary to peripheral retinal breaks. Retina. 2017;37(4):622–629. doi: 10.1097/IAE.0000000000001214 [DOI] [PubMed] [Google Scholar]
- 83.Mikhail M, El-Rayes EN, Kojima K, Ajlan R, Rezende F. Catheter-guided suprachoroidal buckling of rhegmatogenous retinal detachments secondary to peripheral retinal breaks. Graefes Arch Clin Exp Ophthalmol. 2017;255(1):17–23. doi: 10.1007/s00417-016-3530-8 [DOI] [PubMed] [Google Scholar]
- 84.Antaki F, Dirani A, Ciongoli MR, Steel DHW, Rezende F. Hemorrhagic complications associated with suprachoroidal buckling. Int J Retin Vitr. 2000;6:10. doi: 10.1186/s40942-020-00211-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Milani P, Mazzola M, Bergamini F. Suprachoroidal haemhorrage and vortex vein varix: a potential association. Eur J Ophthalmol. 2020:1120672120964033. doi: 10.1177/1120672120964033 [DOI] [PubMed] [Google Scholar]