Abstract
Neuromyelitis optica spectrum disorder (NMOSD) is an autoimmune neurological disease that can cause blindness and disability. As the major mediators in the central nervous system, microglia plays key roles in immunological regulation in neuroinflammatory diseases, including NMOSD. Microglia can be activated by interleukin (IL)-6 and type I interferons (IFN-Is) during NMOSD, leading to signal transducer and activator of transcription (STAT) activation. Moreover, complement C3a secreted from activated astrocytes may induce the secretion of complement C1q, inflammatory cytokines and progranulin (PGRN) by microglia, facilitating injury to microglia, neurons, astrocytes and oligodendrocytes in an autocrine or paracrine manner. These processes involving activated microglia ultimately promote the pathological course of NMOSD. In this review, recent research progress on the roles of microglia in NMOSD pathogenesis is summarized, and the mechanisms of microglial activation and microglial-mediated inflammation, and the potential research prospects associated with microglial activation are also discussed.
Keywords: microglia, neuromyelitis optica spectrum disorder, demyelination, microglial activation
Introduction
Neuromyelitis optica (NMO) is a demyelinating autoimmune disease in which the optic nerves and spinal cord are most commonly involved 1, and was first described by Eugène Devic's team in 1894 2. Some NMO patients will eventually become blind and disabled that even need to be wheelchair-bound 3, which will greatly reduce quality of life and cause a great economic burden.
Similar to multiple sclerosis (MS), NMO is also an inflammatory demyelinating disease. However, in NMO, astrocytes are the targets of immune attack, rather than oligodendrocytes, as occurs in in MS. These two diseases could be reliably distinguished by the detection of the biomarker aquaporin-4 (AQP4)-IgG, which is present in the majority of NMO patients but usually absent in cases of MS 4. On this basis, the concept of neuromyelitis optica spectrum disorder (NMOSD) was first proposed and defined in 2007 5. In 2015, the latest diagnostic guidelines included NMO in NMOSD and divided NMOSD into AQP4-IgG-positive and AQP4-IgG-negative forms according to the expression of the AQP4 antibody 6. In addition to AQP4-IgG, another biomarker, myelin oligodendrocyte glycoprotein (MOG)-IgG, has been identified and used for the diagnosis of NMOSD; AQP4-IgG has been detected in approximately 70% of NMOSD patients globally, and MOG-IgG has been detected in approximately 40% of AQP4-Ab-negative NMOSD patients 7. According to many epidemiological studies, NMOSD has great importance in the prevalence in different regions and racial groups worldwide 8, 9. Although the prevalence of NMOSD is limited, severe autoimmune attacks may cause spinal cord and optic nerve involvement, which leads to paralysis and blindness in the patients 10, 11.
Immunosuppressive therapies have been used to prevent relapses and decrease attack severity in patients with NMOSD 12. For instance, because the repopulation of B cells is relevant to the relapse rate of NMOSD, immunotherapies targeting B cells and related proteins were demonstrated to be effective in treating NMOSD 13, 14, and several drugs have been licenced and applied as clinical therapies 15, 16. In addition to B cell depletion therapy, numerous kinds of treatments have been demonstrated to be effective in treating NMOSD, such as interleukin (IL)-6 receptor antagonists, complement blockers and other monoclonal antibodies (such as aquaporumab, bevacizumab and ublituximab) 17. The efficacy of novel therapies (including eculizumab to target the complement system, satralizumab to target the IL-6 receptor, and inebilizumab to target B cells) has been assessed by randomized controlled trials of patients with NMOSD, and the results show that these therapies were beneficial in preventing autoimmune attacks, but the studies also show various efficacy, safety, tolerability, and practical considerations associated with these drugs 18.
As an essential inflammatory cytokine, IL-6 has been reported to be highly expressed in the serum and cerebrospinal fluid (CSF) of NMO patients, and IL-6 levels were positively associated with disease severity 19. It is reported that Th1 and Th17 cytokines/chemokines are upregulated in NMO 20, and the dominant Th17-related response in NMO patients is positively correlated with neurological disability 21. Moreover, the serum concentrations of CXCL6/GCP-2, Midkine and C5/C5a are significantly altered between AQP4-positive NMO and MOG-positive NMO cases, which indicates different immunological mechanisms of NMO pathogenesis that are associated with these two kinds of antibodies 22.
As native macrophages in the central nervous system (CNS), microglia plays diverse roles and has phagocytic and pro- and anti-inflammatory functions in numerous neurological diseases 23, 24. Microglia also plays a key role in the immunoregulation of neuroinflammatory diseases 25. However, in recent years, investigations on NMO have often focused on astrocytes, while the regulatory roles of microglia have been largely neglected 26. Histopathological analysis demonstrates prominent infiltration and activation of macrophages/microglia in NMO lesions 27. Microglia are the major mediators of CNS inflammation, and AQP4-IgG can induce cytokine production by activating astrocytes and lead to bystander activation towards microglia 28. As one of the major antibody-mediated effects of NMOSD, microglial activation has both protective and disruptive effects, while the regulation of these two opposing effects remains to be further studied 29. Chen et al. indicate that with the involvement of complement, astrocyte-microglia crosstalk plays a critical role in promoting the development of NMO 30. Therefore, microglia are thought to be potential therapeutic targets in treating NMO 26.
In this review, we summarize the recent research progress on the roles of microglia in NMOSD pathogenesis, and the mechanisms of microglial activation and microglial-mediated inflammation are also discussed. We also suggest the potential research prospects of microglial activation in the context of basic research and clinical practice.
The upstream mechanism of microglial activation in NMOSD
IL-6
Activated microglia can recruit macrophages and neutrophilic granulocytes to the NMO lesions, induce the production of IL-1β, IL-6, IL-17, and high-mobility group box 1 protein (HMGB1), which might be involved in NMO pathogenesis 31. IL-17/IL-8 axis activation in cerebrospinal fluid (CSF) and the increase in HMGB1 in the plasma of NMOSD patients have been determined 32, 33. More importantly, CSF levels of IL-6 in NMOSD patients are much higher compared to MS patients, and there is strong evidence showing that IL-6 may play a key role in the pathogenesis of NMOSD 34.
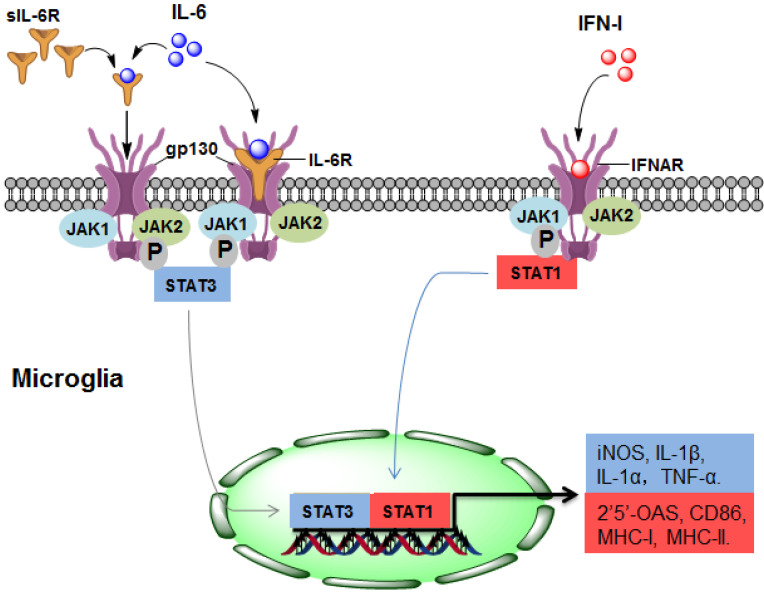
As a potent regulator of cellular communication, the inflammatory factor IL-6 is responsible for both innate and adaptive inflammatory responses by interacting with IL-6 receptor-α (IL-6R) 35. Many CNS-resident cells can produce IL-6, but IL-6R is expressed on a limited subset of cells. IL-6R is mainly found on the surface of microglia but not on the surface of astrocytes, oligodendrocytes, endothelial cells, or neurons 36. IL-6 binds to membrane-bound IL-6R on microglia, triggering gp130 homodimerization to form a functional receptor complex. The homodimerization of the receptor complex activates Janus kinase 1 (JAK1) and JAK2, leading to the activation of signal transducers and activators of transcription (STAT) 3 37. Thus, activated STAT3 may translocate into the nuclei and mediate the expression of IL-6-regulated genes (Figure 1).
Figure 1.
The upstream mechanism of microglial activation in NMOSD. (1) IL-6 activates microglia by directly binding to IL-6R/gp130 (classical signalling) or sIL-6R (trans-signalling), leading to STAT3 activation and ultimately promoting the gene expression of iNOS, IL-1α, IL-1β and TNF-α. (2) In response to IFN-I, STAT1 is activated in microglia, resulting in the gene expression of 2'5'-OAS, CD86, MHC-I and MHC-II. IL-6, interleukin-6; IFN-I: type I interferon; sIL-6R, soluble IL-6R; JAK, Janus kinase; STAT, signal transducer and activator of transcription; MHC, major histocompatibility complex.
During the pathogenesis of NMOSD, the promoting effect of IL-6 may be mainly due to IL-6-mediated activation of microglia through binding with IL-6R. In CNS cells lacking IL-6R, soluble IL-6R (sIL-6R) mediates the response to IL-6, which is called trans-signalling 38. Compared with IL-6R, sIL-6R lacks cytoplasmic and transmembrane regions, binds to IL-6 and activates downstream signalling via ubiquitously expressed gp130 on the cell surface 39, which may also contribute to the pathological process of NMOSD (Figure 1).
Type I interferon (IFN-I)
Type I interferons (IFN-Is), which are group of polypeptides associated with intracellular antimicrobial programmes, are crucial in mediating innate and adaptive immune responses 40. It has been determined that the chronic production of IFN-Is in the CNS is the causal factor driving the development of NMOSD (Figure 1). The IFN-I family consists of many subtypes, the human IFN-I family includes IFN-α, IFN- β, IFN- ε, IFN-κ, and IFN-ω, and the mouse origin includes IFN-α, IFN-β, IFN-ε, IFN-κ, and IFN-ζ 25, 41. The serum level of IFN-α in patients with NMOSD is increased, which is positively correlated with disease severity 42. IFN-β is widely used for treating MS, but it has no treatment effect in NMOSD, and even aggravates the severity of the disease 43.
Almost every CNS-resident cell can express and secrete IFN-I, including microglia, neurons, astrocytes and endothelial cells. IFNAR1 and IFNAR2, the IFN-I receptor genes, are also widely expressed in the CNS 25. Therefore, IFN-I binds to IFNAR and activates downstream signalling which may regulate 2'5'-OAS, CD86, MHC-Ⅰ and MHC-Ⅱ, and this effect may be widespread in different cell types of the CNS 25 (Figure 1). Importantly, the response of microglia to IFN-I is more pronounced than that of astrocytes or neurons 44, indicating that microglia may account for the major cell population that responds to IFN-I in NMOSD. A recent study determined that IFN-β treatment exacerbates the severity of NMOSD and induces microglial activation, as indicated by the expansion of a CD11c+ subset of microglia, suggesting that IFNI-activated microglia play a pathologic role in NMOSD 43.
Factors secreted by activated microglia are involved in the pathogenesis of NMOSD
Complement
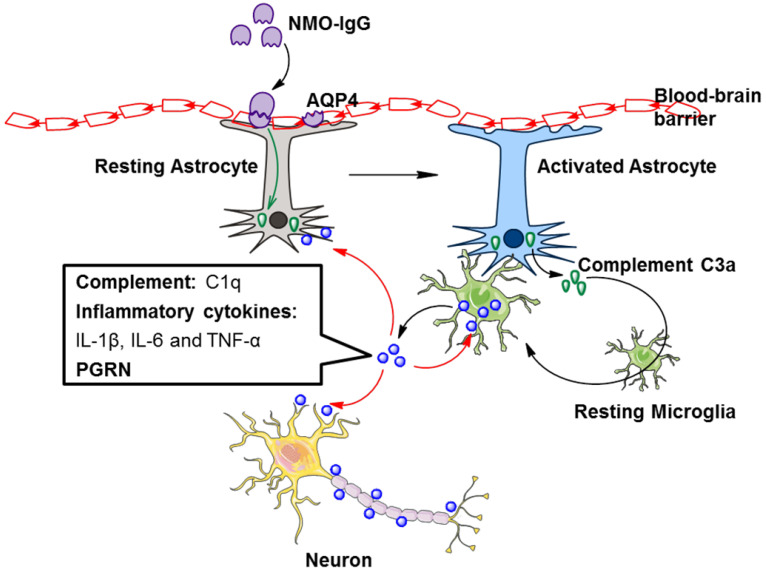
AQP4 is mainly distributed on astrocyte foot processes located in the blood-brain barrier. AQP4-specific antibody (NMO-IgG) supports the cooperation between the cellular and humoral arms of adaptive immunity in NMOSD pathogenesis 45 which is capable of activating complement. Complement proteins are involved in astrocyte destruction and secondary demyelination during the pathological process of NMOSD 27. Therefore, NMOSD is also considered a complement-mediated astrocytopathy.
It is accepted that NMO-IgG can induce massive production of C3 by astrocytes 46, and C3a receptor (C3aR) is mostly expressed on microglia 47. Whether in healthy or pathological conditions, astrocytes and microglia coordinate their functions 48. We may speculate that astrocytes could promote microglial activation through the C3 cleavage product C3a. A recent study showed that NMO-IgG binds to AQP4 on astrocyte endfoot processes, resulting in AQP4 internalization, decreased cell surface AQP4 expression, and astrocyte activation 30. Elevated C3 produced by activated astrocytes is cleaved to form C3a and C3b. Secreted C3a binds with C3aR on resting microglia, which promotes microglial activation, the production of C1q, and the convergence towards astrocytes 30. C1q derived from activated microglia facilitates localized injury to neurons and oligodendrocytes 30 (Figure 2). In addition, C1q may activate the classic complement cascade, leading to sustained CNS tissue damage in NMOSD 26.
Figure 2.
Factors secreted by activated microglia are involved in the pathogenesis of NMOSD. NMO-IgG binds to AQP4 on astrocytes, resulting in astrocyte activation. Activated astrocytes secrete complement C3a, which binds with C3aR on resting microglia, leading to microglial activation. The secretion of complement C1q, inflammatory cytokines and PGRN by activated microglia is increased. These secretions further promote microglial activation in an autocrine manner and facilitate localized injury to neurons, astrocytes and oligodendrocytes in a paracrine manner. AQP4, aquaporin 4; NMO-IgG, neuromyelitis optica immunoglobulin; PGRN, progranulin.
In addition to complement, TGF-β derived from astrocytes induces neuronal release of complement, which ultimately acts upon microglia 48. Astrocyte-derived IL-1 could change the permeability of the blood-brain barrier, accordingly allowing microglial activation 48. Astrocytes and microglia directly affect each other via molecules such as IL-1a, TNF, and IL-33 48. Hence, astrocyte-microglial communication may be a target of NMOSD therapy (Figure 2).
Inflammatory cytokines
Microglial activation is a two-edged sword in NMOSD. Microglial activation may lead to demyelination 49, while it has also been reported to contribute to remyelination 50. Microglia is capable to secrete both pro- and anti-inflammatory cytokines in response to external stimuli 51. Correspondingly, activated microglia can be mainly polarized into two functional phenotypes: M1 and M2 phenotype 52-55.
In the initial stage of CNS diseases, activated microglia are dominated by the M2 phenotype, which is related to the release of several anti-inflammatory cytokines, including IL-10, IL-4, IL-13 and TGF-β, and proinflammatory cytokine production is suppressed 56. Meanwhile M1 phenotype activation is connected with the release of proinflammatory cytokines, such as IL-1β, IL-6 and TNF-α, and an excess accumulation of these factors caused by chronic activation of microglia can result in damage to the surrounding neuronal cells 51. These proinflammatory cytokines are involved in the pathological process of NMOSD 57. For example, IL-1β induces neuromyelitis optica-like lesions in a in vivo study 58. Collectively, M1/M2 polarization might regulate microglial activation as a dual role in NMOSD. However, the regulatory role of inflammatory cytokines derived from microglial activation in NMOSD has not been deeply studied and might be a potential research field.
Progranulin (PGRN)
Progranulin (PGRN), a secreted glycosylated protein, was originally considered to be a growth factor that regulates immune responses and cancer growth 59. PGRN has been reported to be highly enriched in microglia and neurons 60. Kimura et al. reported that CSF levels of PRRN in NMOSD patients are notably higher than those in MS patients and controls without inflammation 61. They also demonstrated that CSF levels of PGRN have a significant correlation with cell counts and protein levels in CSF. It also affects total spinal cord lesion length, which may be related to the severity of spinal cord inflammation in NMOSD 61. Furthermore, there is a positive correlation between IL-6 and PGRN levels in patients with NMOSD and MS 61. As IL-6 triggers PGRN expression in cancer studies 62, 63, IL-6 may serve as a crucial regulator of PGRN in response to microglial activation. It has also been indicated that PGRN enhances IL-6 expression in adipocytes 64. Therefore, CSF PGRN in NMOSD may be mainly derived from microglia and may have interactive regulation with IL-6.
A growing body of evidence suggests that PGRN functions as an autocrine neuroprotective factor by modulating neuroinflammation 59. PGRN-deficient mice are hypersusceptible to neuroinflammation and neuronal loss in response to the injury, and PGRN exhibits a neuroprotective effect by decreasing proinflammatory cytokines and increasing anti-inflammatory cytokines 60, 65-67. In view of this evidence and recent research advances on the role of PGRN in NMOSD, PGRN derived from activated microglia may provide negative feedback in NMOSD (Figure 2).
Prospects and potential applications
Recently, microglia has been identified as potential modulators and targets for NMOSD diagnosis and therapy because of their important roles in neurological disorders.
Regulation by noncoding RNAs
Although they are never translated into proteins, noncoding RNAs (ncRNAs) have been recognized as playing essential regulatory roles in the human CNS, as well as in neurological diseases 68. It has been indicated that microRNAs (miRNAs) are significantly altered in the whole blood of NMOSD patients when compared to MS patients69, 70, while long noncoding RNAs (lncRNAs), the another kind of ncRNA, are differentially expressed in peripheral blood mononuclear cells (PBMCs) of NMOSD patients compared to those of controls 71. Circulating miRNAs from whole blood, as well as serum exosomal miRNAs, might serve as potential biomarkers for the diagnosis and prognosis of NMOSD 72, 73, and several miRNAs are also capable of discriminating NMOSD from MS or neuropsychiatric systemic lupus erythematosus (NPSLE) 74, 75. It has been revealed that different kinds of ncRNAs (miRNAs 76, lncRNAs 77, circular RNAs (circRNAs) 78, etc.) are involved in the regulation of microglia in the pathogenesis of neurological diseases such as MS and epilepsy. The mechanisms include regulating gene expressions and microglia polarization, and acting as a molecular sponge. However, the relevance and mechanisms of microglia and ncRNAs in NMOSD remain unclear and deserve to be further investigated.
Utilization of other novel technologies
Recently, many new technologies have been used to study NMOSD and other autoimmune neurological disorders. For example, single-cell sequencing technologies have been applied to investigate B cells and antibodies in the blood and CSF of NMOSD patients 79. Haematopoietic stem cell transplantation has been considered a possible option for treating patients with severe NMOSD 80. To reduce brain lesions and therapeutically treat patients with CSF1R-related leukoencephalopathy, haematopoietic stem cell transplantation could renew dysfunctional microglia 81. The effect and application of haematopoietic stem cell transplantation on microglia should be further investigated in patients with NMOSD. Although there are some limitations, such as immunogenic reactions and a lack of specificity of viral vectors, gene therapy has been applied with positive outcomes in neurological diseases, including MS 82. Insulin-like growth factor 1 (IGF1) gene therapy could target microglia, modify the inflammatory response and improve cognitive or motor deficits 83. Therefore, gene therapeutic approaches might be a promising choice to partially modulate the progression of NMOSD by targeting microglial activation. To identify new therapeutic and diagnostic approaches with safety and efficacy, these novel technologies should be utilized in future studies of microglial activation in NMOSD.
Conclusion
Although the functions and mechanisms of microglia remain under investigation, the activation of these immunomodulatory cells attracts the attention of researchers. Cytokines such as IL-6 and the IFN-I family, the complement system and PGRN are involved in the pathogenesis of NMOSD. M1 or M2 polarization might regulate microglial activation in NMOSD. Combined studies with ncRNAs, as well as novel technologies such as single-cell sequencing, stem cell therapy and gene therapy, are promising options for investigating the microglial activation in NMOSD.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81800855), Hunan Provincial Natural Scientific Foundation (No. 2019JJ50849) and Scientific Research Project of Hunan Provincial Health Commission (No. 202113050843).
References
- 1.Wingerchuk DM, Hogancamp WF, O'Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic's syndrome) Neurology. 1999;53:1107–14. doi: 10.1212/wnl.53.5.1107. [DOI] [PubMed] [Google Scholar]
- 2.Jarius S, Wildemann B. The history of neuromyelitis optica. J Neuroinflammation. 2013;10:8. doi: 10.1186/1742-2094-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao-Draayer Y, Thiel S, Mills EA, Chitnis T, Fabian M, Katz Sand I. et al. Neuromyelitis optica spectrum disorders and pregnancy: therapeutic considerations. Nat Rev Neurol. 2020;16:154–70. doi: 10.1038/s41582-020-0313-y. [DOI] [PubMed] [Google Scholar]
- 4.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–7. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG. The spectrum of neuromyelitis optica. Lancet Neurol. 2007;6:805–15. doi: 10.1016/S1474-4422(07)70216-8. [DOI] [PubMed] [Google Scholar]
- 6.Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T. et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–89. doi: 10.1212/WNL.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thoman ME, McKarns SC. Metabolomic Profiling in Neuromyelitis Optica Spectrum Disorder Biomarker Discovery. Metabolites. 2020. 10. [DOI] [PMC free article] [PubMed]
- 8.Hor JY, Asgari N, Nakashima I, Broadley SA, Leite MI, Kissani N. et al. Epidemiology of Neuromyelitis Optica Spectrum Disorder and Its Prevalence and Incidence Worldwide. Front Neurol. 2020;11:501. doi: 10.3389/fneur.2020.00501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papp V, Magyari M, Aktas O, Berger T, Broadley SA, Cabre P. et al. Worldwide Incidence and Prevalence of Neuromyelitis Optica: A Systematic Review. Neurology. 2021;96:59–77. doi: 10.1212/WNL.0000000000011153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciccarelli O, Cohen JA, Reingold SC, Weinshenker BG, International Conference on Spinal Cord I, Imaging in Multiple S. et al. Spinal cord involvement in multiple sclerosis and neuromyelitis optica spectrum disorders. Lancet Neurol. 2019;18:185–97. doi: 10.1016/S1474-4422(18)30460-5. [DOI] [PubMed] [Google Scholar]
- 11.Gospe SM 3rd, Chen JJ, Bhatti MT. Neuromyelitis optica spectrum disorder and myelin oligodendrocyte glycoprotein associated disorder-optic neuritis: a comprehensive review of diagnosis and treatment. Eye (Lond) 2021;35:753–68. doi: 10.1038/s41433-020-01334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul F, Murphy O, Pardo S, Levy M. Investigational drugs in development to prevent neuromyelitis optica relapses. Expert Opin Investig Drugs. 2018;27:265–71. doi: 10.1080/13543784.2018.1443077. [DOI] [PubMed] [Google Scholar]
- 13.Nosadini M, Alper G, Riney CJ, Benson LA, Mohammad SS, Ramanathan S. et al. Rituximab monitoring and redosing in pediatric neuromyelitis optica spectrum disorder. Neurol Neuroimmunol Neuroinflamm. 2016;3:e188. doi: 10.1212/NXI.0000000000000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim SH, Hyun JW, Kim HJ. Individualized B cell-targeting therapy for neuromyelitis optica spectrum disorder. Neurochem Int. 2019;130:104347. doi: 10.1016/j.neuint.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 15.Graf J, Mares J, Barnett M, Aktas O, Albrecht P, Zamvil SS, Targeting B cells to modify MS, NMOSD, and MOGAD: Part 2. Neurol Neuroimmunol Neuroinflamm. 2021. 8. [DOI] [PMC free article] [PubMed]
- 16.Graf J, Mares J, Barnett M, Aktas O, Albrecht P, Zamvil SS, Targeting B Cells to Modify MS, NMOSD, and MOGAD: Part 1. Neurol Neuroimmunol Neuroinflamm. 2021. 8. [DOI] [PMC free article] [PubMed]
- 17.Xie Q, Sun M, Sun J, Zheng T, Wang M. New progress in the treatment of neuromyelitis optica spectrum disorder with monoclonal antibodies (Review) Exp Ther Med. 2021;21:148. doi: 10.3892/etm.2020.9579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levy M, Fujihara K, Palace J. New therapies for neuromyelitis optica spectrum disorder. Lancet Neurol. 2021;20:60–7. doi: 10.1016/S1474-4422(20)30392-6. [DOI] [PubMed] [Google Scholar]
- 19.Icoz S, Tuzun E, Kurtuncu M, Durmus H, Mutlu M, Eraksoy M. et al. Enhanced IL-6 production in aquaporin-4 antibody positive neuromyelitis optica patients. Int J Neurosci. 2010;120:71–5. doi: 10.3109/00207450903428970. [DOI] [PubMed] [Google Scholar]
- 20.Matsushita T, Tateishi T, Isobe N, Yonekawa T, Yamasaki R, Matsuse D. et al. Characteristic cerebrospinal fluid cytokine/chemokine profiles in neuromyelitis optica, relapsing remitting or primary progressive multiple sclerosis. PLoS One. 2013;8:e61835. doi: 10.1371/journal.pone.0061835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linhares UC, Schiavoni PB, Barros PO, Kasahara TM, Teixeira B, Ferreira TB. et al. The ex vivo production of IL-6 and IL-21 by CD4+ T cells is directly associated with neurological disability in neuromyelitis optica patients. J Clin Immunol. 2013;33:179–89. doi: 10.1007/s10875-012-9780-2. [DOI] [PubMed] [Google Scholar]
- 22.Ai N, Liu H, Zhou H, Lin D, Wang J, Yang M. et al. Cytokines and chemokines expression in serum of patients with neuromyelitis optica. Neuropsychiatr Dis Treat. 2019;15:303–10. doi: 10.2147/NDT.S185336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salter MW, Stevens B. Microglia emerge as central players in brain disease. Nat Med. 2017;23:1018–27. doi: 10.1038/nm.4397. [DOI] [PubMed] [Google Scholar]
- 24.Qin C, Zhou LQ, Ma XT, Hu ZW, Yang S, Chen M. et al. Dual Functions of Microglia in Ischemic Stroke. Neurosci Bull. 2019;35:921–33. doi: 10.1007/s12264-019-00388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.West PK, Viengkhou B, Campbell IL, Hofer MJ. Microglia responses to interleukin-6 and type I interferons in neuroinflammatory disease. Glia. 2019;67:1821–41. doi: 10.1002/glia.23634. [DOI] [PubMed] [Google Scholar]
- 26.Moinfar Z, Zamvil SS. Microglia complement astrocytes in neuromyelitis optica. J Clin Invest. 2020;130:3961–4. doi: 10.1172/JCI138804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lucchinetti CF, Guo Y, Popescu BF, Fujihara K, Itoyama Y, Misu T. The pathology of an autoimmune astrocytopathy: lessons learned from neuromyelitis optica. Brain Pathol. 2014;24:83–97. doi: 10.1111/bpa.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen T, Bosco DB, Ying Y, Tian DS, Wu LJ. The Emerging Role of Microglia in Neuromyelitis Optica. Front Immunol. 2021;12:616301. doi: 10.3389/fimmu.2021.616301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramakrishnan P. Could Galectin-3 be a key player in the etiology of neuromyelitis optica spectrum disorder? Med Hypotheses. 2021;146:110450. doi: 10.1016/j.mehy.2020.110450. [DOI] [PubMed] [Google Scholar]
- 30.Chen T, Lennon VA, Liu YU, Bosco DB, Li Y, Yi MH. et al. Astrocyte-microglia interaction drives evolving neuromyelitis optica lesion. J Clin Invest. 2020;130:4025–38. doi: 10.1172/JCI134816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bradl M, Kanamori Y, Nakashima I, Misu T, Fujihara K, Lassmann H. et al. Pain in neuromyelitis optica-prevalence, pathogenesis and therapy. Nat Rev Neurol. 2014;10:529–36. doi: 10.1038/nrneurol.2014.129. [DOI] [PubMed] [Google Scholar]
- 32.Ishizu T, Osoegawa M, Mei FJ, Kikuchi H, Tanaka M, Takakura Y. et al. Intrathecal activation of the IL-17/IL-8 axis in opticospinal multiple sclerosis. Brain. 2005;128:988–1002. doi: 10.1093/brain/awh453. [DOI] [PubMed] [Google Scholar]
- 33.Wang KC, Tsai CP, Lee CL, Chen SY, Chin LT, Chen SJ. Elevated plasma high-mobility group box 1 protein is a potential marker for neuromyelitis optica. Neuroscience. 2012;226:510–6. doi: 10.1016/j.neuroscience.2012.08.041. [DOI] [PubMed] [Google Scholar]
- 34.Uzawa A, Mori M, Ito M, Uchida T, Hayakawa S, Masuda S. et al. Markedly increased CSF interleukin-6 levels in neuromyelitis optica, but not in multiple sclerosis. J Neurol. 2009;256:2082–4. doi: 10.1007/s00415-009-5274-4. [DOI] [PubMed] [Google Scholar]
- 35.Jones SA. Directing transition from innate to acquired immunity: defining a role for IL-6. J Immunol. 2005;175:3463–8. doi: 10.4049/jimmunol.175.6.3463. [DOI] [PubMed] [Google Scholar]
- 36.Hsu MP, Frausto R, Rose-John S, Campbell IL. Analysis of IL-6/gp130 family receptor expression reveals that in contrast to astroglia, microglia lack the oncostatin M receptor and functional responses to oncostatin M. Glia. 2015;63:132–41. doi: 10.1002/glia.22739. [DOI] [PubMed] [Google Scholar]
- 37.Hunter CA, Jones SA. IL-6 as a keystone cytokine in health and disease. Nat Immunol. 2015;16:448–57. doi: 10.1038/ni.3153. [DOI] [PubMed] [Google Scholar]
- 38.Rose-John S. IL-6 trans-signaling via the soluble IL-6 receptor: importance for the pro-inflammatory activities of IL-6. Int J Biol Sci. 2012;8:1237–47. doi: 10.7150/ijbs.4989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rose-John S. The soluble interleukin-6 receptor and related proteins. Best Pract Res Clin Endocrinol Metab. 2015;29:787–97. doi: 10.1016/j.beem.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Blank T, Prinz M. Type I interferon pathway in CNS homeostasis and neurological disorders. Glia. 2017;65:1397–406. doi: 10.1002/glia.23154. [DOI] [PubMed] [Google Scholar]
- 41.Owens T, Khorooshi R, Wlodarczyk A, Asgari N. Interferons in the central nervous system: a few instruments play many tunes. Glia. 2014;62:339–55. doi: 10.1002/glia.22608. [DOI] [PubMed] [Google Scholar]
- 42.Asgari N, Voss A, Steenstrup T, Kyvik KO, Stenager E, Lillevang ST. Interferon alpha association with neuromyelitis optica. Clin Dev Immunol. 2013;2013:713519. doi: 10.1155/2013/713519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wlodarczyk A, Khorooshi R, Marczynska J, Holtman IR, Burton M, Jensen KN. et al. Type I interferon-activated microglia are critical for neuromyelitis optica pathology. Glia. 2021;69:943–53. doi: 10.1002/glia.23938. [DOI] [PubMed] [Google Scholar]
- 44.Li W, Viengkhou B, Denyer G, West PK, Campbell IL, Hofer MJ. Microglia have a more extensive and divergent response to interferon-alpha compared with astrocytes. Glia. 2018;66:2058–78. doi: 10.1002/glia.23460. [DOI] [PubMed] [Google Scholar]
- 45.Varrin-Doyer M, Spencer CM, Schulze-Topphoff U, Nelson PA, Stroud RM, Cree BA. et al. Aquaporin 4-specific T cells in neuromyelitis optica exhibit a Th17 bias and recognize Clostridium ABC transporter. Ann Neurol. 2012;72:53–64. doi: 10.1002/ana.23651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howe CL, Kaptzan T, Magana SM, Ayers-Ringler JR, LaFrance-Corey RG, Lucchinetti CF. Neuromyelitis optica IgG stimulates an immunological response in rat astrocyte cultures. Glia. 2014;62:692–708. doi: 10.1002/glia.22635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davoust N, Jones J, Stahel PF, Ames RS, Barnum SR. Receptor for the C3a anaphylatoxin is expressed by neurons and glial cells. Glia. 1999;26:201–11. doi: 10.1002/(sici)1098-1136(199905)26:3<201::aid-glia2>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 48.Vainchtein ID, Molofsky AV. Astrocytes and Microglia: In Sickness and in Health. Trends Neurosci. 2020;43:144–54. doi: 10.1016/j.tins.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu Y, Given KS, Harlow DE, Matschulat AM, Macklin WB, Bennett JL. et al. Myelin-specific multiple sclerosis antibodies cause complement-dependent oligodendrocyte loss and demyelination. Acta Neuropathol Commun. 2017;5:25. doi: 10.1186/s40478-017-0428-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu Y, Given KS, Owens GP, Macklin WB, Bennett JL. Distinct patterns of glia repair and remyelination in antibody-mediated demyelination models of multiple sclerosis and neuromyelitis optica. Glia. 2018;66:2575–88. doi: 10.1002/glia.23512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Subhramanyam CS, Wang C, Hu Q, Dheen ST. Microglia-mediated neuroinflammation in neurodegenerative diseases. Semin Cell Dev Biol. 2019;94:112–20. doi: 10.1016/j.semcdb.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Orihuela R, McPherson CA, Harry GJ. Microglial M1/M2 polarization and metabolic states. Br J Pharmacol. 2016;173:649–65. doi: 10.1111/bph.13139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pan J, Jin JL, Ge HM, Yin KL, Chen X, Han LJ. et al. Malibatol A regulates microglia M1/M2 polarization in experimental stroke in a PPARgamma-dependent manner. J Neuroinflammation. 2015;12:51. doi: 10.1186/s12974-015-0270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu LR, Liu JC, Bao JS, Bai QQ, Wang GQ. Interaction of Microglia and Astrocytes in the Neurovascular Unit. Front Immunol. 2020;11:1024. doi: 10.3389/fimmu.2020.01024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jin X, Liu MY, Zhang DF, Zhong X, Du K, Qian P. et al. Natural products as a potential modulator of microglial polarization in neurodegenerative diseases. Pharmacol Res. 2019;145:104253. doi: 10.1016/j.phrs.2019.104253. [DOI] [PubMed] [Google Scholar]
- 56.Ransohoff RM. A polarizing question: do M1 and M2 microglia exist? Nat Neurosci. 2016;19:987–91. doi: 10.1038/nn.4338. [DOI] [PubMed] [Google Scholar]
- 57.Tradtrantip L, Asavapanumas N, Verkman AS. Emerging therapeutic targets for neuromyelitis optica spectrum disorder. Expert Opin Ther Targets. 2020;24:219–29. doi: 10.1080/14728222.2020.1732927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kitic M, Hochmeister S, Wimmer I, Bauer J, Misu T, Mader S. et al. Intrastriatal injection of interleukin-1 beta triggers the formation of neuromyelitis optica-like lesions in NMO-IgG seropositive rats. Acta Neuropathol Commun. 2013;1:5. doi: 10.1186/2051-5960-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kao AW, McKay A, Singh PP, Brunet A, Huang EJ. Progranulin, lysosomal regulation and neurodegenerative disease. Nat Rev Neurosci. 2017;18:325–33. doi: 10.1038/nrn.2017.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yin F, Banerjee R, Thomas B, Zhou P, Qian L, Jia T. et al. Exaggerated inflammation, impaired host defense, and neuropathology in progranulin-deficient mice. J Exp Med. 2010;207:117–28. doi: 10.1084/jem.20091568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kimura A, Takemura M, Saito K, Serrero G, Yoshikura N, Hayashi Y. et al. Increased cerebrospinal fluid progranulin correlates with interleukin-6 in the acute phase of neuromyelitis optica spectrum disorder. J Neuroimmunol. 2017;305:175–81. doi: 10.1016/j.jneuroim.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Liu F, Zhang W, Yang F, Feng T, Zhou M, Yu Y. et al. Interleukin-6-stimulated progranulin expression contributes to the malignancy of hepatocellular carcinoma cells by activating mTOR signaling. Sci Rep. 2016;6:21260. doi: 10.1038/srep21260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Frampton G, Invernizzi P, Bernuzzi F, Pae HY, Quinn M, Horvat D. et al. Interleukin-6-driven progranulin expression increases cholangiocarcinoma growth by an Akt-dependent mechanism. Gut. 2012;61:268–77. doi: 10.1136/gutjnl-2011-300643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matsubara T, Mita A, Minami K, Hosooka T, Kitazawa S, Takahashi K. et al. PGRN is a key adipokine mediating high fat diet-induced insulin resistance and obesity through IL-6 in adipose tissue. Cell Metab. 2012;15:38–50. doi: 10.1016/j.cmet.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 65.Wang C, Zhang L, Ndong JC, Hettinghouse A, Sun G, Chen C. et al. Progranulin deficiency exacerbates spinal cord injury by promoting neuroinflammation and cell apoptosis in mice. J Neuroinflammation. 2019;16:238. doi: 10.1186/s12974-019-1630-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Filiano AJ, Martens LH, Young AH, Warmus BA, Zhou P, Diaz-Ramirez G. et al. Dissociation of frontotemporal dementia-related deficits and neuroinflammation in progranulin haploinsufficient mice. J Neurosci. 2013;33:5352–61. doi: 10.1523/JNEUROSCI.6103-11.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Menzel L, Kleber L, Friedrich C, Hummel R, Dangel L, Winter J. et al. Progranulin protects against exaggerated axonal injury and astrogliosis following traumatic brain injury. Glia. 2017;65:278–92. doi: 10.1002/glia.23091. [DOI] [PubMed] [Google Scholar]
- 68.Salta E, De Strooper B. Non-coding RNAs with essential roles in neurodegenerative disorders. Lancet Neurol. 2012;11:189–200. doi: 10.1016/S1474-4422(11)70286-1. [DOI] [PubMed] [Google Scholar]
- 69.Chen J, Zhu J, Wang Z, Yao X, Wu X, Liu F. et al. MicroRNAs Correlate with Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder in a Chinese Population. Med Sci Monit. 2017;23:2565–83. doi: 10.12659/MSM.904642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keller A, Leidinger P, Meese E, Haas J, Backes C, Rasche L. et al. Next-generation sequencing identifies altered whole blood microRNAs in neuromyelitis optica spectrum disorder which may permit discrimination from multiple sclerosis. J Neuroinflammation. 2015;12:196. doi: 10.1186/s12974-015-0418-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xu J, Zhang F, Gao C, Ma X, Peng X, Kong D. et al. Microarray Analysis of lncRNA and mRNA Expression Profiles in Patients with Neuromyelitis Optica. Mol Neurobiol. 2017;54:2201–8. doi: 10.1007/s12035-016-9754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vaknin-Dembinsky A, Charbit H, Brill L, Abramsky O, Gur-Wahnon D, Ben-Dov IZ. et al. Circulating microRNAs as biomarkers for rituximab therapy, in neuromyelitis optica (NMO) J Neuroinflammation. 2016;13:179. doi: 10.1186/s12974-016-0648-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen C, Wu Y, Li M, Cui C, Zhao Y, Sun X. et al. Different Exosomal microRNA Profile in Aquaporin-4 Antibody Positive Neuromyelitis Optica Spectrum Disorders. Front Immunol. 2020;11:1064. doi: 10.3389/fimmu.2020.01064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sharaf-Eldin W, Kishk N, Sakr B, El-Hariri H, Refeat M, ElBagoury N. et al. Potential Value of miR-23a for Discriminating Neuromyelitis Optica Spectrum Disorder from Multiple Sclerosis. Arch Iran Med. 2020;23:678–87. doi: 10.34172/aim.2020.86. [DOI] [PubMed] [Google Scholar]
- 75.Sharaf-Eldin WE, Kishk NA, Gad YZ, Hassan H, Ali MAM, Zaki MS. et al. Extracellular miR-145, miR-223 and miR-326 expression signature allow for differential diagnosis of immune-mediated neuroinflammatory diseases. J Neurol Sci. 2017;383:188–98. doi: 10.1016/j.jns.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 76.Walsh AD, Nguyen LT, Binder MD. miRNAs in Microglia: Important Players in Multiple Sclerosis Pathology. ASN Neuro. 2021;13:1759091420981182. doi: 10.1177/1759091420981182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sun D, Yu Z, Fang X, Liu M, Pu Y, Shao Q. et al. LncRNA GAS5 inhibits microglial M2 polarization and exacerbates demyelination. EMBO Rep. 2017;18:1801–16. doi: 10.15252/embr.201643668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xiaoying G, Guo M, Jie L, Yanmei Z, Ying C, Shengjie S. et al. CircHivep2 contributes to microglia activation and inflammation via miR-181a-5p/SOCS2 signalling in mice with kainic acid-induced epileptic seizures. J Cell Mol Med. 2020;24:12980–93. doi: 10.1111/jcmm.15894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zou A, Ramanathan S, Dale RC, Brilot F. Single-cell approaches to investigate B cells and antibodies in autoimmune neurological disorders. Cell Mol Immunol. 2021;18:294–306. doi: 10.1038/s41423-020-0510-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ceglie G, Papetti L, Valeriani M, Merli P. Hematopoietic Stem Cell Transplantation in Neuromyelitis Optica-Spectrum Disorders (NMO-SD): State-of-the-Art and Future Perspectives. Int J Mol Sci. 2020. 21. [DOI] [PMC free article] [PubMed]
- 81.Han J, Sarlus H, Wszolek ZK, Karrenbauer VD, Harris RA. Microglial replacement therapy: a potential therapeutic strategy for incurable CSF1R-related leukoencephalopathy. Acta Neuropathol Commun. 2020;8:217. doi: 10.1186/s40478-020-01093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Iqubal A, Iqubal MK, Khan A, Ali J, Baboota S, Haque SE. Gene Therapy, A Novel Therapeutic Tool for Neurological Disorders: Current Progress, Challenges and Future Prospective. Curr Gene Ther. 2020;20:184–94. doi: 10.2174/1566523220999200716111502. [DOI] [PubMed] [Google Scholar]
- 83.Falomir-Lockhart E, Dolcetti FJC, Garcia-Segura LM, Herenu CB, Bellini MJ. IGF1 Gene Therapy Modifies Microglia in the Striatum of Senile Rats. Front Aging Neurosci. 2019;11:48. doi: 10.3389/fnagi.2019.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]