Abstract
Objective:
To examine demographic and clinical characteristics associated with diagnostic delay in psoriatic arthritis (PsA).
Methods:
We characterized a retrospective, population-based cohort of incident adult (≥18 years) PsA patients from Olmsted County, MN from 2000–17. All patients met classification criteria. Diagnostic delay was defined as the time from any patient-reported PsA-related joint symptom to a physician diagnosis of PsA. Factors associated with delay in PsA diagnosis were identified through logistic regression models.
Results:
Of the 164 incident PsA cases from 2000–17, 162 had a physician or rheumatologist diagnosis. Mean (SD) age was 41.5 (12.6) and 46% were females. Median time from symptom onset to physician diagnosis was 2.5 years (interquartile range: 0.5 to 7.3). By six months, 38 (23%) received a diagnosis of PsA, 56 (35%) by one year and 73 (45%) by two years after symptom onset. No significant trend in diagnostic delay was observed over calendar time. Earlier age at onset of PsA symptoms, higher body mass index, and enthesitis were associated with a diagnostic delay of >2 years, while sebopsoriasis was associated with a lower likelihood of delay.
Conclusion:
In our study, more than half of PsA patients had a diagnostic delay of >2 years, and no significant improvement in time to diagnosis was noted between 2000–17. Patients with younger age at PsA symptom onset, higher BMI, or enthesitis before diagnosis were more likely to have a diagnostic delay of >2 year while patients with sebopsoriasis were less likely to have a diagnostic delay.
Keywords: Psoriatic arthritis, spondyloarthritis, diagnosis, delay
INTRODUCTION
Psoriatic arthritis (PsA) is a chronic musculoskeletal disease, which can lead to progressive joint pain, joint destruction, and loss of function. The impact on quality of life and functional status is similar to rheumatoid arthritis (RA) (1). There is also increasing evidence that early diagnosis and treatment of PsA leads to improved long term outcomes for patients in terms of disease severity, and radiographic damage (2,3). Delays in diagnosis of even 6 to 12 months have been shown to be associated with joint damage and poor functional outcomes (3–5). Similarly, treatment response may also be better in early PsA (4). Despite this, the majority of patients have significant delays in diagnosis of PsA; up to 40% have not been previously identified in screening studies (6). Several factors contribute to delay in diagnosis of PsA. While early diagnosis is important in PsA, awareness of PsA compared to RA is poor in community practice (7). The clinical presentation of PsA is heterogeneous, and there are no definitive, gold standard diagnostic tests. Similarly, psoriasis patients may not report joint symptoms or be aware of joint inflammation. Moreover, psoriasis patients can have joint pain due to other common etiologies such as osteoarthritis, gout, and fibromyalgia (6,8). Another issue is that approximately 10–15% of patients develop arthritis prior to psoriasis, posing additional difficulty with diagnosis (9).
Only a few studies have examined delay in diagnosis of PsA, most of which relied on patient surveys or administrative data for ascertainment of the date of PsA diagnosis, which may be misleading. A study from Europe showed improvement in time to diagnosis for PsA (10). However, the trends in diagnostic delay of PsA in the US and factors associated with delay in diagnosis have not been well studied. Lack of longitudinal, population-based PsA cohorts in the US has made this type of study difficult. The aims of our study were to 1) examine the diagnostic delay in PsA in residents of Olmsted County from 2000–17, and 2) identify demographic and clinical characteristics associated with diagnostic delay in PsA.
METHODS
Data source.
A retrospective inception cohort of Olmsted County, MN residents with PsA between 2000 and 2017 was assembled. The population of Olmsted County, Minnesota, in which resides the city of Rochester, is well suited for investigation of the epidemiology of PsA as comprehensive medical records for all residents seeking medical care for over five decades are available. A record linkage system allows ready access to the medical records from all health care providers for the local population, including the Mayo Clinic, the Olmsted Medical Center and affiliated hospitals, local nursing homes, and the few private practitioners (11,12). The population of Olmsted County in 2010 was 144,248 with 74.7% being adults of age ≥18 years. Patients who denied authorization to use their medical records for research were excluded. The study was approved by the Mayo Clinic (18–010851) and Olmsted Medical Center (051-OMC-18) institutional review boards.
Patient population and case ascertainment.
PsA cases were defined as patients fulfilling ClASsification of Psoriatic ARthritis (CASPAR) criteria for PsA (sensitivity of 91.4% and specificity of 98.7%) (13). ICD-9/10 diagnostic codes for arthralgias, arthritis, monoarthritis, oligoarthritis, polyarthritis, spondylitis, ankylosing spondylitis, arthropathy, psoriatic arthropathy, spondyloarthropathy, and seronegative spondyloarthropathy were used to screen for patients with PsA. Medical record chart review of all potential cases was performed to ascertain fulfillment of the CASPAR criteria. Questionable cases were resolved by mutual agreement between study investigators. Patients ≥18 years fulfilling CASPAR criteria between January 1, 2000 and December 31, 2017 were included in the PsA incidence cohort.
Outcomes.
The primary outcome of interest was delay in diagnosis of PsA >2 years (i.e., the time from symptom onset to establishment of PsA diagnosis). Secondary outcomes were delays in PsA diagnosis of >6 months or >1 year. Symptom onset was defined as the first PsA-related musculoskeletal symptom (not explained by other diagnoses) documented by a clinician in the medical records. PsA-related musculoskeletal symptoms were defined as joint- or enthesis-related symptoms documented in the medical records that did not have a clear alternative explanation besides PsA such as trauma/injury, gout, fibromyalgia, or degenerative joint disease (14). MSK symptoms included were arthralgia, AM joint stiffness, pain or stiffness at entheseal sites, and inflammatory back pain. The PsA diagnosis date was the date of establishment of PsA diagnosis by a rheumatologist. For patients meeting CASPAR criteria but never seen by a rheumatologist, confirmatory diagnosis of PsA by any physician was included. Time to diagnosis was defined as the time from onset of symptoms to establishment of PsA diagnosis. Radiographic damage was defined based on parameters of joint erosion, destruction and proliferation from hand/wrist and feet radiographs included in the Sharp-van der Heijde score modified for PsA (Table 1) (15).
Table 1.
Baseline characteristics of patients with psoriatic arthritis (PsA) with delay in diagnosis of 2 or less years compared to more than 2 years
| ≤2yr (n=73) | >2yr (n=89) | Total (n=162) | p value | |
|---|---|---|---|---|
| Years from PsA symptom onset to Physician/Rheumatologist diagnosis of PsA, median (IQR) | 0.5 (0.2–1.0) | 6.5 (3.5–10.1) | 2.5 (0.5–7.3) | -- |
| Age (yrs) at PsA symptom onset, mean (SD) | 44.0 (12.4) | 39.5 (12.4) | 41.5 (12.6) | 0.041 |
| Sex, female (%) | 36 (49%) | 39 (44%) | 75 (46%) | 0.48 |
| Education Level | 0.79 | |||
| High school or less | 16 (22%) | 16 (18%) | 32 (20%) | |
| Some college or 2yr degree | 27 (38%) | 36 (40%) | 63 (39%) | |
| ≥4 yr college degree | 29 (40%) | 37 (42%) | 66 (41%) | |
| Missing | 1 | 0 | 1 | |
| Race | 0.018 | |||
| Black | 2 (3%) | 2 (2%) | 4 (2%) | |
| Asian | 0 (0%) | 8 (9%) | 8 (5%) | |
| Hispanic | 6 (8%) | 3 (3%) | 9 (6%) | |
| Other/Mixed | 1 (1%) | 0 (0%) | 1 (1%) | |
| White | 64 (88%) | 75 (85%) | 139 (86%) | |
| Unknown | 0 | 1 | 1 | |
| BMI (kg/m2) at PsA diagnosis, mean (SD) | 29.5 (6.1) | 32.2 (7.7) | 31.0 (7.1) | 0.028 |
| Missing | 4 | 5 | 9 | |
| Smoking at PsA diagnosis | 0.53 | |||
| Current smoker | 12 (16%) | 15 (17%) | 27 (17%) | |
| Past smoker | 23 (32%) | 35 (39%) | 58 (36%) | |
| Never smoker | 38 (52%) | 39 (44%) | 77 (48%) | |
| Alcohol intake at PsA dx | 56 (77%) | 65 (73%) | 121 (75%) | 0.59 |
| Psoriasis (Current or personal history) | 0.15 | |||
| No psoriasis | 2 (3%) | 5 (6%) | 7 (4%) | |
| Current psoriasis | 70 (96%) | 78 (88%) | 148 (91%) | |
| Personal history of psoriasis | 1 (1%) | 6 (7%) | 7 (4%) | |
| Family history of psoriasis | 24 (40%) | 35 (49%) | 59 (45%) | 0.32 |
| Missing | 13 | 17 | 30 | |
| Estmated age (yrs) at onset of psoriasis symptom, mean (SD) | 34 (14) | 34 (15) | 34 (14) | 0.85 |
| Missing | 2 | 5 | 7 | |
| Psoriasis Severity at first diagnosis | 0.25 | |||
| Mild (< 2% BSA) | 38 (54%) | 34 (41%) | 72 (47%) | |
| Moderate (2–10% BSA) | 20 (28%) | 33 (40%) | 53 (34%) | |
| Severe (>10% BSA) | 13 (18%) | 16 (19%) | 29 (19%) | |
| No Documentation/Missing | 2 | 6 | 8 | |
| Type of psoriasis at first dx | 0.033 | |||
| Chronic plaque psoriasis | 56 (80%) | 74 (88%) | 130 (84%) | |
| Guttate psoriasis | 3 (4%) | 1 (1%) | 4 (3%) | |
| Pustular psoriasis- Generalized | 1 (1%) | 0 (0%) | 1 (1%) | |
| Pustular psoriasis- palms/soles | 2 (3%) | 4 (5%) | 6 (4%) | |
| Sebo-psoriasis | 5 (7%) | 0 (0%) | 5 (3%) | |
| Chronic plaque psoriasis & Guttate psoriasis | 0 (0%) | 3 (4%) | 3 (2%) | |
| Chronic plaque & Pustular psoriasis-palms/soles | 1 (1%) | 0 (0%) | 1 (1%) | |
| Chronic plaque & Sebo-psoriasis | 2 (3%) | 2 (2%) | 4 (3%) | |
| No Documentation/Missing | 3 | 5 | 8 | |
| Site of psoriatic lesions at first diagnosis of psoriasis | 0.65 | |||
| Palms and/or soles | 1 (5%) | 3 (15%) | 4 (10%) | |
| Elbows and/or knees | 3 (14%) | 4 (20%) | 7 (17%) | |
| Limbs arms and/or legs | 5 (23%) | 5 (25%) | 10 (24%) | |
| Trunk | 0 (0%) | 1 (5%) | 1 (2%) | |
| Face | 1 (5%) | 0 (0%) | 1 (2%) | |
| Scalp | 9 (41%) | 7 (35%) | 16 (38%) | |
| Intergluteal/Perianal | 2 (9%) | 0 (0%) | 2 (5%) | |
| Genital | 1 (5%) | 0 (0%) | 1 (2%) | |
| Missing | 51 | 69 | 120 | |
| Nail involvement at first diagnosis of psoriasis | 24 (42%) | 23 (35%) | 47 (38%) | 0.41 |
| No documentation | 16 | 23 | 39 | |
| Family history of PsA | 6 (12%) | 6 (11%) | 12 (11%) | 0.84 |
| Missing | 22 | 32 | 54 | |
| Enthesitis at or prior to PsA diagnosis | 16 (22%) | 35 (39%) | 51 (31%) | 0.018 |
| Dactylitis at or prior to PsA diagnosis | 35 (48%) | 35 (39%) | 70 (43%) | 0.27 |
| Inflammatory back pain at or prior to PsA diagnosis | 4 (5%) | 13 (15%) | 17 (10%) | 0.059 |
| Uveitis | 4 (5%) | 3 (3%) | 7 (4%) | 0.70 |
| Inflammatory bowel disease | 0 (0%) | 0 (0%) | 0 (0%) | -- |
| ESR (mm/hr) at PsA diagnosis, mean (SD) | 18.9 (18.3) | 18.2 (15.3) | 18.5 (16.8) | 0.95 |
| Missing | 4 | 17 | 21 | |
| CRP (mg/L) at PsA diagnosis, mean (SD) | 16.5 (32.4) | 13.6 (19.0) | 14.9 (26.0) | 0.87 |
| Missing | 22 | 29 | 51 | |
| Radiographic damage | 17 (24%) | 31 (35%) | 48 (30%) | 0.12 |
| Missing | 1 | 0 | 1 |
Covariates of interest.
Complete medical records from all healthcare providers were identified and reviewed for each patient by PK using a standardized, pre-tested data abstraction form in the Research Electronic Data Capture (REDCap) system for consistency. Information regarding demographics, clinical characteristics, laboratory data, and radiographic features were collected. Psoriasis was confirmed by documentation of diagnosis in the medical record by either a dermatologist, rheumatologist, or positive skin biopsy. Severity of psoriasis was defined based on body surface area involvement, distribution of involved sites, and requirement for phototherapy or systemic therapy as documented in the medical records.
Statistical analysis.
Descriptive statistics (medians, percentages, etc.) were used to summarize the data. Chi-square, Fisher’s exact, or rank sum tests were used to compare characteristics between groups. Logistic regression models adjusted for age and sex were performed to identify factors associated with delay in PsA diagnosis. Trends in time from symptom onset to diagnosis of PsA were examined using linear regression models adjusted for age and sex with and without log transformation of the delay to address skewness. Model diagnostics were examined. Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and R 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
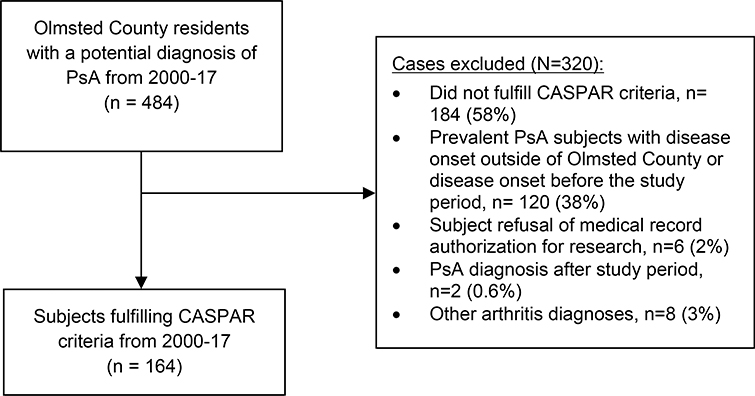
A total of 164 patients aged ≥18 years of age were identified who fulfilled CASPAR criteria between January 1, 2000 and December 31, 2017 (Figure 1). Two patients who did not have a physician diagnosis of PsA were excluded. The remaining 162 patients with incident PsA were included in this study. A rheumatologist made the diagnosis of PsA for 160 patients, and the remaining two patients received a confirmatory diagnosis of PsA by internal medicine physicians. Both of them clearly met CASPAR criteria and had characteristic DIP erosions on radiographs. The mean (SD) age at PsA symptom onset in the cohort was 41.5 (12.6) years, and 46% were females.
Figure 1.
Case-finding strategy for psoriatic arthritis (PsA) from the medical records
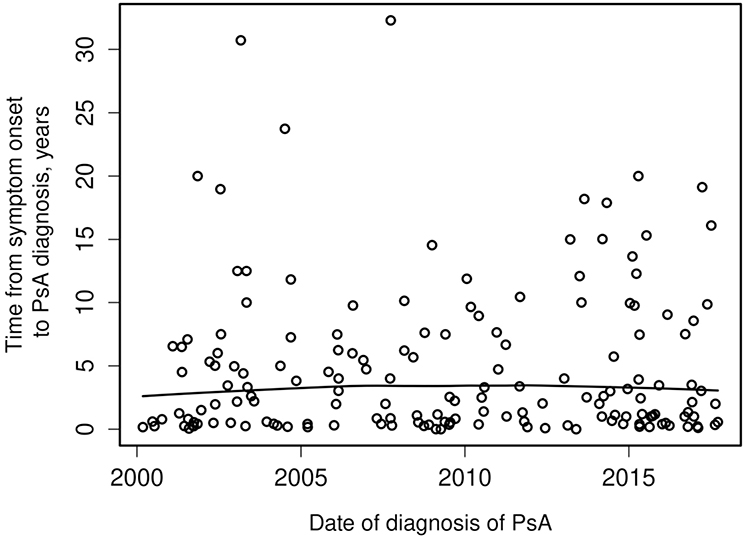
Median time to diagnosis from first PsA-related joint symptom was 2.5 years (interquartile range [IQR]: 0.5 to 7.3). By six months after symptom onset, 38 patients (23%) received an established diagnosis of PsA, 56 (35%) by one year, and 73 (45%) by two years. No significant trend in time to diagnosis was observed during the study period of 2000–2017 (p=0.84; Figure 2). There were no significant differences between those with and without diagnostic delay in terms of sex, education level, smoking status, alcohol intake, psoriasis severity or location, nail involvement, family history of psoriasis or PsA, history of extra-articular manifestations (i.e., uveitis, inflammatory bowel disease), or high inflammatory markers at the time of diagnosis (Table 1).
Figure 2.
Trend over time (2000–2017) in diagnostic delay from symptom onset to diagnosis of psoriatic arthritis (PsA).
PsA patients with younger age at PsA symptom onset (OR per 10 year decrease = 1.34, 95% CI 1.04–1.74), higher body mass index (BMI) (OR per 10 kg/m2 increase = 1.89, 95% CI 1.15–3.10) and enthesitis at or before diagnosis (OR = 2.20, 95% CI 1.08–4.46) were associated with a diagnostic delay of longer than 2 years (Table 2). Sebo-psoriasis at diagnosis was associated with a lower likelihood of delay of more than 2 years (OR=0.19, 95% CI 0.04–0.97). Radiographic damage at PsA diagnosis showed a possible association with a delay in diagnosis of longer than 2 years (OR=1.63, 95% CI 0.78–3.41), but this was not statistically significant. Results were similar for diagnostic delays of 6 months or 1 year.
Table 2.
Logistic regression models for delay in psoriatic arthritis (PsA) diagnosis adjusted for age at symptom onset and sex
| Clinical Features | >2 yr, OR (95% CI) | >1 yr, OR (95% CI) | >6 mo, OR (95% CI) |
|---|---|---|---|
| Age at PsA symptom onset per 10 year decrease* | 1.34 (1.04–1.74) | 1.26 (0.97–1.65) | 1.35 (1.00–1.82) |
| BMI at PsA dx per 10 kg/m2 increase | 1.89 (1.15–3.10) | 1.73 (1.03–2.92) | 1.58 (0.89–2.81) |
| Enthesitis prior to PsA | 2.20 (1.08–4.46) | 1.75 (0.83–3.68) | 2.27 (0.91–5.63) |
| ESR at PsA diagnosis per 10 mm/hr increase | 1.00 (0.82–1.23) | 0.96 (0.78–1.18) | 0.82 (0.66–1.02) |
| Type of psoriasis at first diagnosis (sebopsoriasis) | 0.19 (0.04–0.97) | 0.21 (0.05–0.89) | 0.10 (0.02–0.45) |
| Radiographic damage | 1.72 (0.83–3.53) | 1.80 (0.83–3.91) | 2.19 (0.87–5.52) |
Adjusted for sex only
DISCUSSION
In this population-based study, more than half of PsA patients were diagnosed at least two years after symptom onset. Younger age at PsA symptom onset, obesity, and enthesitis were associated with a delay in diagnosis of longer than 2 years. The importance of diagnosing PsA early has been outlined in several studies, and delay in diagnosis has been shown to be associated with poor outcomes in PsA. Studies from UK and Canada show that diagnostic delay of greater than 1 year and 2 years respectively were associated with worse functional outcomes (2,3). Observational studies have reported improved outcomes in PsA patients receiving early treatment; these improved outcomes may be long lasting (2–5). While PsA can sometimes be mild, requiring minimal pharmacological therapy, high risk patients may benefit from earlier diagnosis. Therefore, additional efforts are needed to shorten the time from symptom onset to diagnosis.
Several patient and system related factors may contribute to delay of diagnosis: 1) patient factors; 2) practitioner delay in recognition or referral; and 3) system delays (i.e., time to rheumatology visit) (16,17). Our study found that patients with younger age at PsA symptom onset, higher BMI, or enthesitis before diagnosis were more likely to have a diagnostic delay of two or more years. It is possible that patients with younger age may dismiss their symptoms. Similarly, patients may not report joint pain symptoms or may not be aware of joint inflammation (6). Symptoms such as enthesitis may be attributed to overuse and trauma. Obese patients may attribute joint symptoms to more commonly associated diseases such as osteoarthritis or gout. Longer time to diagnosis (5.7 vs. 2.8 years) was also noted in obese patients compared to patients with normal BMI in the University of Toronto PsA cohort (18).
Similarly, delay could be related to provider misattribution of PsA signs or symptoms to more common conditions, such as trauma, overuse, degenerative disease, fibromyalgia, or gout. In a US patient survey, less recognized symptoms of PsA, such as enthesitis and back pain, were also associated with diagnostic delay (19). Inflammatory back pain symptoms were not different between patients with and without diagnostic delay in our study. An important and novel finding of our study is the association of obesity with diagnostic delay. BMI is accurately captured in the REP database with height and weight captured at each visit. Obesity could make the joint examination difficult; other concurrent joint pathologies, such as degenerative disease and gout, are also more common in obesity. In the absence of apparent psoriasis or other extra-articular manifestations of SpA, manifestations of enthesitis and joint symptoms in obese patients may not be diagnosed until late after the development of objective clinical or radiologic findings. In our study, patients with sebo-psoriasis were less likely to have a diagnostic delay. While it is debatable whether this is a true psoriasis variant, early diagnosis of sebo-psoriasis by a dermatologist could aid rheumatologists in diagnosing a patient with PsA in the right setting.
Previous studies have examined time to PsA diagnosis, and the results have been variable. In a study from Denmark, the average time from initial symptoms to diagnosis was 3.42 years (SD = 4.75) (10). Another study from an older referral cohort (University of Toronto) using CASPAR criteria reported that 60% of patients had >2 years of symptoms (median 11 years in this group) before PsA diagnosis (2). The reported times to diagnosis in other studies are slightly better. A study from the UK using CASPAR criteria showed that only one-third of patients had a symptom duration of ≥1 year before diagnosis (3). Similarly, another study from a rheumatology clinic in Dublin reported the median time from symptom onset to first rheumatologic assessment was 1 year (IQR 0.5–2) (5). The outcome in this study was first rheumatologic assessment rather than an established diagnosis of PsA, which could explain the lower median delay in the study compared to ours. Finally, in a cross-sectional web-based survey from the US, one-third of PsA patients sought medical attention after 1 year of symptom onset; up to one-third of the patients had ≥5 years between seeking medical attention and receiving a diagnosis (19). However, the results of this survey study should be interpreted in the context of the limitations of surveys, including potential recall, participation, or ascertainment bias with regard to PsA diagnosis (e.g., self-reported diagnosis).
Secular trends in diagnostic delay have not been robustly studied. The study from Denmark showed improvement in time to diagnosis of PsA from 2000 to 2011 (42 months in 2000–02 to 7 months in 2009–11) (10). This study was conducted within the DANBIO registry where patient eligibility was restricted to patients on biologic therapy (i.e., only patients with severe PsA) and included before 2005. Similarly, recall bias was a potential concern in this study, especially in patients with longer symptom duration because symptom onset was collected at study registration. In our study, we did not find a change in time to diagnosis between 2000 and 2017.
Improvement in identification and subsequent referral of patients with inflammatory arthritis will require a concerted effort. The Psoriatic Arthritis Forum consensus had recommended identification of cases in the community, public awareness programs, patient education, self-administered surveys, referral guidelines for community practitioners, and integrated multidisciplinary clinics with dermatologists and rheumatologists (7). Use of some of these approaches have been shown to improve diagnostic delays (20). Additionally, some validated screening tools in psoriasis could help capture PsA features such as enthesitis and back pain (21). Advanced imaging techniques, such as ultrasound in clinical practice, could improve detection of enthesitis and joint inflammation in the obese. Moreover, our results emphasize the complicated relationship between comorbidities such as obesity and PsA. Delay in diagnosis could be another possible mechanism associated with worse outcomes in obesity, in addition to lower response to therapy.
Strengths of our study include the unique record linkage system of the REP, allowing near complete ascertainment of all clinically recognizable PsA cases in a well-defined population (12). Furthermore, case ascertainment was done using the validated CASPAR criteria. Unlike administrative coding in most studies, all variables were collected via manual review of the paper and electronic records.
However, our study also has several limitations. While few PsA cases not fulfilling CASPAR criteria may have been missed, the sensitivity and specificity of the CASPAR criteria were close to 99% when adapted for retrospective use to identify PsA cohort (22). Due to the extended study period and availability of near-complete medical history in this population, we expect that most PsA cases would have been correctly ascertained. Second, being a retrospective study, the usual limitations regarding completeness of medical record documentation apply. Only those symptoms recorded in the medical records would be ascertained, and the precision/accuracy of exact symptom onset is uncertain. While our study did not examine patient reported or functional outcomes, a possible association of diagnostic delay with radiographic damage was seen. However, this association did not reach statistical significance, perhaps due to the limited sample size of the cohort and temporality could not be ascertained due to lack of radiographs before PsA diagnosis in most cases. Although the radiology reports were thoroughly reviewed, formal scoring by a radiologist was not performed. Lastly, the population of Olmsted County, Minnesota is predominantly white (90%), which may limit the generalizability of study results to other racial or ethnic groups.
In conclusion, more than half of PsA patients in our study had a diagnostic delay of >2 years, and no significant improvement in time to diagnosis was noted from 2000–17. Patients with younger age at PsA symptom onset, higher BMI, or enthesitis before diagnosis were more likely to have a diagnostic delay of >2 years. Better understanding of factors associated with diagnostic delay may help in earlier diagnosis and management to improve outcomes in high risk PsA patients. As not all patients have severe or progressive disease, identifying high risk patient subgroup will be important to stratify those that will benefit from early, aggressive treatment.
Acknowledgments
Financial support: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676, and Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Karmacharya is supported by T32 AR56950 grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program, and Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) pilot research grant. Dr. Duarte-García is supported by the Centers for Disease Control and Prevention, Rheumatology Research Foundation Scientist Development Award, the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, the Women’s Health Career Enhancement Award, and the Eaton Family Career Development Award.
Conflict of interest: Dr. Ogdie has served as a consultant for AbbVie, Amgen, BMS, Celgene, Corrona, Gilead, Janssen, Lilly, Novartis, Pfizer, and UCB (less than 10,000 each) and has received grants from Novartis and Pfizer to Penn and from Amgen to Forward (grants more than 10,000). Dr. Davis has received consulting fees and/or honoraria from AbbVie and Sanofi-Genzyme (less than $10,000 each) and research support from Pfizer. Dr. Ernste has received research support from Octapharma and Genentech (less than $10,000 each). No other disclosures relevant to this article.
REFERENCES
- 1.Sokoll KB, Helliwell PS. Comparison of disability and quality of life in rheumatoid and psoriatic arthritis. J Rheumatol 2001;28:1842–6. [PubMed] [Google Scholar]
- 2.Gladman DD, Thavaneswaran A, Chandran V, Cook RJ. Do patients with psoriatic arthritis who present early fare better than those presenting later in the disease? Ann Rheum Dis 2011;70:2152–4. [DOI] [PubMed] [Google Scholar]
- 3.Tillett W, Jadon D, Shaddick G, Cavill C, Korendowych E, de Vries CS, et al. Smoking and delay to diagnosis are associated with poorer functional outcome in psoriatic arthritis. Ann Rheum Dis 2013;72:1358–61. [DOI] [PubMed] [Google Scholar]
- 4.Theander E, Husmark T, Alenius G-M, Larsson PT, Teleman A, Geijer M, et al. Early psoriatic arthritis: short symptom duration, male gender and preserved physical functioning at presentation predict favourable outcome at 5-year follow-up. Results from the Swedish Early Psoriatic Arthritis Register (SwePsA). Annals of the Rheumatic Diseases BMJ Publishing Group Ltd; 2014;73:407–13. [DOI] [PubMed] [Google Scholar]
- 5.Haroon M, Gallagher P, FitzGerald O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis 2015;74:1045–50. [DOI] [PubMed] [Google Scholar]
- 6.Ogdie A, Weiss P. The Epidemiology of Psoriatic Arthritis. Rheum Dis Clin North Am 2015;41:545–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helliwell P, Coates L, Chandran V, Gladman D, de Wit M, FitzGerald O, et al. Qualifying Unmet Needs and Improving Standards of Care in Psoriatic Arthritis. Arthritis Care Res (Hoboken) 2014;66:1759–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ritchlin CT, Colbert RA, Gladman DD. Psoriatic Arthritis. N Engl J Med 2017;376:957–70. [DOI] [PubMed] [Google Scholar]
- 9.Coates LC, Helliwell PS. Psoriatic arthritis: state of the art review. Clin Med (Lond) 2017;17:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sørensen J, Hetland ML, all departments of rheumatology in Denmark. Diagnostic delay in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis: results from the Danish nationwide DANBIO registry. Ann Rheum Dis 2015;74:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc 2012;87:1202–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, Pankratz JJ, Brue SM, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol 2012;41:1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 2006;54:2665–73. [DOI] [PubMed] [Google Scholar]
- 14.A Delphi Consensus Study to Standardize Terminology for the Pre-clinical Phase of Psoriatic Arthritis [Internet]. ACR Meeting Abstracts [cited 2020 Nov 19]. Available from: https://acrabstracts.org/abstract/a-delphi-consensus-study-to-standardize-terminology-for-the-pre-clinical-phase-of-psoriatic-arthritis/ [Google Scholar]
- 15.van der Heijde D, Gladman DD, Kavanaugh A, Mease PJ. Assessing structural damage progression in psoriatic arthritis and its role as an outcome in research. Arthritis Research & Therapy 2020;22:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hansen RP, Olesen F, Sørensen HT, Sokolowski I, Søndergaard J. Socioeconomic patient characteristics predict delay in cancer diagnosis: a Danish cohort study. BMC Health Serv Res 2008;8:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansen RP, Vedsted P, Sokolowski I, Søndergaard J, Olesen F. General practitioner characteristics and delay in cancer diagnosis. a population-based cohort study. BMC Fam Pract 2011;12:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eder L, Abji F, Rosen CF, Chandran V, Gladman DD. The Association Between Obesity and Clinical Features of Psoriatic Arthritis: A Case-control Study. J Rheumatol 2017;44:437–43. [DOI] [PubMed] [Google Scholar]
- 19.Ogdie A, Nowell WB, Applegate E, Gavigan K, Venkatachalam S, de la Cruz M, et al. Patient perspectives on the pathway to psoriatic arthritis diagnosis: results from a web-based survey of patients in the United States. BMC Rheumatol 2020;4:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Onna M, Gorter S, Maiburg B, Waagenaar G, van Tubergen A. Education improves referral of patients suspected of having spondyloarthritis by general practitioners: a study with unannounced standardised patients in daily practice. RMD Open 2015;1:e000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iragorri N, Hazlewood G, Manns B, Danthurebandara V, Spackman E. Psoriatic arthritis screening: a systematic review and meta-analysis. Rheumatology (Oxford) 2019;58:692–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tillett W, Costa L, Jadon D, Wallis D, Cavill C, McHUGH J, et al. The ClASsification for Psoriatic ARthritis (CASPAR) Criteria – A Retrospective Feasibility, Sensitivity, and Specificity Study. The Journal of Rheumatology The Journal of Rheumatology; 2012;39:154–6. [DOI] [PubMed] [Google Scholar]