Abstract
Hazardous drinking by persons living with HIV (PLHIV) is a well-established determinant of sub-optimal HIV care and treatment outcomes. Despite this, to date, few interventions have sought to reduce hazardous drinking among PLHIV in sub-Saharan Africa (SSA). We describe an iterative cultural adaptation of an evidence-based multi-session alcohol reduction intervention for PLHIV in southwestern Uganda. The adaptation process included identifying core, theoretically informed, intervention elements, and conducting focus group discussions and cognitive interviews with community members, HIV clinic staff and patients to modify key intervention characteristics for cultural relevance and saliency. Adaptation of evidence-based alcohol reduction interventions can be strengthened by the inclusion of the target population and key stakeholders in shaping the content, while retaining fidelity to core intervention elements.
Keywords: cultural adaptation, alcohol reduction, evidence-based interventions, people living with HIV, Uganda, sub-Saharan Africa
Introduction
Sub-Saharan Africa (SSA) is home to the majority (53%) of persons living with HIV (PLHIV) globally [1]. An estimated 12–62% of PLHIV in SSA engage in hazardous drinking [2], defined as a quantity or pattern of alcohol consumption that increases risk for adverse health events [3]. In Uganda, HIV prevalence is 6.2% [4], with an estimated 21% of the population reporting heavy episodic drinking (i.e., more than 60 grams of alcohol on at least one occasion at least once a month) [5]. Alcohol use is a well-established determinant of sexual risk behavior and HIV transmission [6–8]. Moreover, hazardous drinking is associated with suboptimal HIV care outcomes, including reduced antiretroviral therapy (ART) adherence and viral suppression [8–10]. Sustained engagement in HIV care is critical to ensure the health and well-being of PLHIV and to prevent onward transmission [11, 12], making the reduction of hazardous drinking among PLHIV a public health priority.
To date, few interventions have sought to reduce hazardous drinking among PLHIV in SSA [8, 13, 14], with the most effective being interventions with 4 to 6 in-person sessions [14–17]. Yet, the scalability and cost-effectiveness of multi-session in-person interventions may be sub-optimal in many settings [18]. Evidence from the United States (US) suggests that in-person alcohol reduction interventions with telephone-based boosters may reduce hazardous drinking among PLHIV [19, 20]. The Healthy Women Healthy Living (HWHL) study, developed for women living with HIV in the US, included two in-person and two phone-based booster sessions, and was found to be efficacious in reducing heavy drinking days by 43% [19].
Given its efficacy for PLHIV in the U.S., and the brief multi-session format, HWHL holds promise as an effective strategy to reduce drinking among PLHIV in Uganda. Further, the growing ubiquity of mobile phone usage in SSA [21], and the acceptability of mobile phone-based HIV interventions in Uganda [22], indicates that HWHL could be feasibly implemented in this setting. We therefore adapted the HWHL intervention for the Ugandan context, in advance of a randomized controlled trial (RCT) to examine the efficacy, cost effectiveness, and acceptability of the adapted intervention.
Cultural adaptation rationale and approach
Behavioral norms related to alcohol use vary across cultures. For instance, cultures can vary in terms of whether they are perceived as “wet” (i.e. most people drink) or “dry” (i.e. most people abstain) [23–25], whether drinking occurs in private or public spaces [26], and by the perceived negative consequences of alcohol use [25]. Indeed, the context and consequences of hazardous drinking in Uganda vary from that of the U.S., suggesting the need to culturally adapt the HWHL intervention to the Ugandan context. For example, while Americans drink both in the home and in social spaces such as bars or night clubs, drinking is primarily a social activity that occurs outside the home in Uganda [27–29]. Further, alcohol use has been identified as a significant financial burden in Uganda, where resources are more limited than in the U.S. [27–29]. The financial strain of alcohol use has been identified as a strong motivating factor to reduce alcohol consumption in Uganda [28, 29]. Adapting evidence-based alcohol reduction interventions, such as HWHL, to account for the cultural context in which they are implemented is essential to ensure their relevance, acceptability, and sustainability in the new setting [30–32]. Failing to do so jeopardizes the potential efficacy of interventions that are designed to improve health outcomes [31].
Cultural adaptation frameworks [31–36] describe core elements and key characteristics of evidence-based interventions (EBIs) [31, 32, 34–36]. Core intervention elements are the theory-informed elements that are hypothesized to drive efficacy [34–36]. Key characteristics, while important, are non-essential and modifiable aspects of the intervention that reflect cultural contexts and populations (e.g., language, norms, and values) [34–36]. Some cultural adaptation frameworks focus on modifying key characteristics of EBIs for cultural relevance and acceptability [15, 33]. These include concepts (how a health problem is conceptualized and communicated to the participants), language (how people express meanings), metaphors (symbols used in a culture), and context (social, economic and political contexts) [33]. We describe the process of adapting the HWHL intervention for PLHIV in southwestern Uganda, organized by this prior framing, including iterative adaptation methods, and examples of the ways the material was adapted in response to our findings.
Methods
The HWHL intervention
The HWHL intervention [19] includes two 20-minute face-to-face counseling sessions conducted one month apart, each followed by a 5–10 minute live telephone-based booster session with a counselor. Sessions are led by a trained counselor, following a scripted workbook. In the first session, participants are encouraged to agree to a drinking limit with the counselor and are given the workbook, a drinking diary to track alcohol use between sessions, and take-home exercises. Participants receive a phone-based booster session two weeks later to assess recent drinking, discuss barriers and facilitators to complying with drinking limits, and reinforce individualized motivations [19]. In the second in-person session, participants review their drinking diary, drinking agreement, and take-home exercises with the counselor. They discuss barriers and facilitators to changing their alcohol use. Participants are also encouraged to bring a ‘helper’ to this session to support their behavior change. Two to three weeks after the second session, participants receive a final booster call [19].
Theoretical framework for HWHL
The theoretical framework underlying HWHL is the Information-Motivation-Behavioral Skills (IMB) model, which holds that well-informed and motivated individuals, equipped with the appropriate behavioral skills, can engage in health promoting behaviors such as alcohol reduction or medication adherence [37]. HWHL is also informed by Social Cognitive Theory [38], Social Norms Theory [39], Cognitive Dissonance [40], Value Expectancies [41] and Motivational Models of Alcohol Use [42]. In the intervention, information is provided about the negative effects of alcohol use, definitions of lower risk drinking, standard drink sizes, and drinking norms. Elements designed to improve motivation include discussing the negative consequences of drinking, risky situations, benefits of reducing or quitting, and guidance to set a specific drinking limit. Behavioral skills are cultivated via discussions of strategies to overcome drinking triggers. Booster sessions assess recent drinking and reinforce motivation towards meeting individualized drinking limits. The in-person follow-up sessions are designed to reinforce motivation and behavioral skills by reviewing the benefits of reducing alcohol use, discussing barriers and facilitators to reducing drinking, and identifying strategies to overcome barriers in the long term.
The ‘Extend’ intervention in Uganda
We conducted the Extend Study to adapt the HWHL intervention for men and women living with HIV in southwestern Uganda and test it in a 3-armed RCT ((NCT 03928418). Participants were recruited at the Immune Suppression Syndrome (ISS) HIV clinic in Mbarara, Uganda, which serves over 11,000 patients. As with HWHL, the Extend intervention includes two in-person counseling sessions guided by a workbook. To maximize feasibility of the intervention, the in-person sessions occur the same day as participants’ regular ISS clinic visits. Phone-based booster sessions occur between the two in-person sessions, delivered as either 1) live phone booster sessions with a trained counselor, covering similar material as the HWHL booster sessions, delivered three weeks apart; or 2) twice-weekly two-way automated mobile-phone short messaging system (SMS) or interactive voice response (IVR) sessions (according to participant preference), for a total of approximately 24 sessions. The SMS/IVR sessions deliver similar material as the live call but lack discussion of barriers and facilitators to adhering to drinking limits. A third control arm receives a wait-list standard-of-care, with in-person counseling and booster sessions offered following the RCT.
Cultural adaptation methodology
The iterative cultural adaptation process included data collection, analysis and intervention refinement at multiple time points. A phased approach was chosen for pragmatic purposes; to break up the intervention into smaller components to allow enough time to review each component within a 1–2-hour focus group/interview. All focus groups and cognitive interviews were designed to gain input on the key characteristics of the intervention to improve its relevance and acceptability. Previous qualitative work conducted by our team offered insight into the social context of alcohol use among PLHIV in Uganda [29] and informed the selection of the HWHL intervention. We also chose HWHL because of its efficacy among PLHIV, its brevity, which maximized potential feasibility in the setting, and the inclusion of multiple sessions, as recommended by the U.S. Preventive Services Task Force [43]. The six-phase adaptation process (Table I) included: 1) identification of core intervention elements to be retained, and “surface structure” adaptations [44] of the HWHL workbook and booster scripts; 2) one round of focus group discussions (FGDs) with key stakeholders and patients to gain initial input on the intervention; 3) cognitive interviews (CIs) with clinic patients to iteratively adapt the HWHL workbook and booster scripts; 4) FGDs with clinic patients to inform workbook and drinking diary adaptation and CIs with patient helpers to inform helper components and handouts; 5) FGDs with clinic patients to adapt automated booster scripts from the live booster scripts; and 6) CIs to test the booster scripts.
Table I.
Procedures for cultural adaptation of a brief alcohol reduction intervention for people living with HIV in Uganda
| Goals and activities | Participants |
|---|---|
| Phase 1. Initial intervention adaptation for the setting | |
| • Changes to local terminology, names, places and local statistics related to drinking frequencies etc. • Translate intervention materials into local language |
None |
| Phase 2. FGDs to gather initial intervention feedback | |
| • Obtain community, clinic and patient perspectives on the revised intervention content and structure and discuss mobile phone usage. Short skits by study staff presented parts of the intervention. | Group 1: Community Advisory Board (CAB) members (n=9, mixed gender) Group 2: Clinic staff (n=10, mixed gender) Group 3: Literate male hazardous drinkers (n=7) Group 4: Literate female hazardous drinkers (n=8) Group 5: Low-literacy male hazardous drinkers (n= 5) Group 6: Low-literacy female hazardous drinkers (n= 9) Total of 6 FGDs with 48 participants |
| Phase 3. Cognitive interviews (CIs) to adapt workbook and booster scripts | |
| • Provide opportunity for patients to describe their thoughts, understanding and reactions to the content of the revised in-person and live booster intervention components including the drinking diary and helper handout, as well as confidentiality concerns. | Literate hazardous drinkers (n=2 male and 2 female) Low-literacy hazardous drinkers (n=2 male and 2 female) Two rounds of cognitive interviews with the same 8 participants= 16 interviews |
| Phase 4. FGDs and CIs to adapt workbook and take-home materials | |
| • Elicit patient feedback on the clarity and relevance of the revised intervention workbook, drinking diary, and helper handout. Elicit responses of helpers (supporters of participants’ reduced drinking) in the session 2 scripts. |
First round FGDs: Group 1: Literate male hazardous drinkers (n=9) Group 2: Literate female hazardous drinkers (n=9) Group 3: Low-literacy female hazardous drinkers (n=6) Group 4: Low-literacy male hazardous drinkers (n=9) Second round: Group 1: Literate male hazardous drinkers (n=6) Group 2: Literate female hazardous drinkers (n=6) Group 3: Low-literacy female hazardous drinkers (n=6) Group 4: Low-literacy male hazardous drinkers (n=8) Total of 8 FGDs with 59 participants Helper CIs (n=9 participants) Helpers of literate hazardous drinkers (n=7) Helpers of low-literacy hazardous drinkers (n=2) |
| Phase 5. FGDs to adapt automated booster scripts | |
| • Obtain patient feedback on the clarity and content of the automated booster script, including tailoring, call frequency, and adapting live booster scripts for automated tech delivery. |
First round FGDs: Group 1: Literate male hazardous drinkers (n=9) Group 2: Literate female hazardous drinkers (n=11) Group 3: Mixed gender low-literacy hazardous drinkers (n=8) Second round (different participants than first round): Group 1: Literate male hazardous drinkers (n=4) Group 2: Literate female hazardous drinkers (n=5) Group 3: Mixed gender low-literacy hazardous drinkers (n=6) Total of 6 FGDs with 43 participants |
| Phase 6: CIs to test the adapted booster scripts | |
| • Provide opportunity for patients to describe their thoughts, understanding and reactions to the content of each automated booster script |
First round CIs: Low-literacy male hazardous drinker (n=1) Low-literacy female hazardous drinker (n=4) Literate male hazardous drinker (n=1) Literate female hazardous drinker (n=1) Second round CIs (different participants than first round): Low-literacy male hazardous drinker (n=1) Low-literacy female hazardous drinker (n=1) Literate male hazardous drinker (n=2) Literate female hazardous drinker (n=1) Total of 12 cognitive interviews |
FGDs and CIs were selected due to their different but complementary strengths. FGDs elicit a broad range of perceptions about intervention content and approach, and suggestions for improvement [45]. CIs systematically assess understanding of intervention components and provide insight into whether the adapted materials convey their desired meaning [46]. They also provide an opportunity to explore concerns that may not be easily discussed in a group.
Participants included ISS clinic staff (clerks, counselors and medical staff), Community Advisory Board (CAB) members (community members and leaders), clinic patients who reported hazardous drinking (purposively selected based on drinking status, literacy level, and sex) and patient helpers (Table I). Patients who participated in prior studies at the ISS clinic [47, 48], and who reported hazardous drinking in those studies, operationalized as an Alcohol Use Disorders Identification Test–Consumption [AUDIT-C] [49] score ≥3 for women and ≥4 for men, were invited to participate. Literacy levels in those studies were assessed by asking participants to read a sentence on a card. Where possible, FGDs with clinic patients were conducted in sex- and literacy-disaggregated groups; CIs were conducted with a patient sample selected to include all purposive sampling categories.
Across all phases, 100 unique participants took part in the CIs and FGDs; 57 participated in more than one data collection stage. Participants provided written informed consent and were given transport reimbursements and refreshments. Discussions and interviews were conducted in the preferred language (Runyankole or English) by trained qualitative interviewers. FGDs were audio recorded, transcribed, and translated into English. CIs were conducted using conversational interviewing techniques, with responses captured by interviewers using a form comprised of both close-ended and open text note fields. Interviewers wrote reports after each FGD and CI to reflect upon the main themes that emerged, the tone of the interviews, and any content that participants found unclear.
Phase 1: Initial workbook and booster script adaptation
First, the research team identified core intervention elements and made “surface structure” adaptations to include local terminology, names, places, and statistics related to alcohol use [44]. The research team referred to the theory underlying the HWHL intervention noted above (IMB model, social cognitive theory etc.), to identify core intervention elements. Intervention materials were then translated to Runyankole. Counselors were trained in Motivational Interviewing-informed counseling by a licensed clinical psychologist and study co-investigator (SWK), to facilitate the description of the intervention during the FGDs and for the intervention delivery.
Phase 2: FGDs to elicit initial intervention feedback
CAB members, clinic staff and patients participated in six FGDs, with 5–10 participants in each group, for a total of 48 participants (Table I). FGDs were conducted at this stage to assess a broad range of perspectives on the cultural relevance of the key characteristics of the intervention and suggestions for improvement. A semi-structured discussion guide elicited perspectives on the intervention content and suggestions for improvement. FGD with the CAB elicited community feedback on the relevance of the counseling messages to the Ugandan context and preferences for the intervention. The FGD with clinic staff focused on provider challenges and strategies for counseling clients about alcohol use, as well as barriers and facilitators to implementing the intervention. Patient FGDs explored barriers and facilitators to reducing alcohol use, preferences for automated boosters, mobile phone usage, desired timing, frequency, and length of the booster messages, as well as confidentiality issues.
Phase 3: CIs to adapt workbook and booster script
Following revisions based on phase 2 FGD findings, CIs were conducted with eight clinic patients with low and high literacy levels (n=4 male and n=4 female). CI participants were different than those who participated in the FGDs in the prior stage to gain feedback on the relevance and understanding of the materials from a broader patient population. In the first round of CIs, interviewers and participants reviewed the revised workbook and live booster scripts for the first in-person counseling visit and reviewed the drinking diary. Participants were asked to comment on their understanding of every aspect of each component. After revisions in response to the first round of CIs, the same group of patients were invited back for a second round of CIs to review the revised materials from the first stage and asked to comment on whether the revisions improved the relevance and understanding of the materials. Participants also reviewed the workbook content for the second in-person counseling session and offered feedback on their understanding of each aspect of these materials as well as their thoughts on timing and confidentiality issues related to the booster script.
Phase 4: FGDs and CIs to adapt workbook and take-home materials
Two rounds of four FGDs each were then conducted with clinic patients to gain feedback and group consensus on the revised intervention materials. The first round included 6–9 participants in each group for a total of 33 participants. All participants were invited back to the second round, and 6–8 of the same participants took part in each FGD for a total of 26 participants. In the first FGD, participants reviewed the adapted workbook for the first counseling visit and the drinking diary. In the second FGD, participants reviewed the revised materials based on their first FGD feedback, as well as the workbook for the second counseling visit and handout for patient helpers. Finally, we conducted CIs with nine patient-helpers to review and assess their understanding of the patient-helper handout and explore how they could better support patients.
Phase 5: FGDs to adapt automated booster scripts
We then conducted two rounds of patient FGDs to gain a broad range of feedback on the relevance of the automated booster scripts. These FGDs were conducted with participants engaged in the previous data collection phases since they were already familiar with the other intervention materials that the booster scripts were meant to supplement. Each round of data collection included three FGDs, for a total of six groups. The first FGDs included 8–11 participants in each group for a total of 28 participants. Different participants, who were involved in the previous phases of data collection, participated in the second round of FGDs, which consisted of 4–6 in each, for a total of 15 participants. The decision to include different participants in the second round of FGDs was made to ensure that the booster scripts were relevant and understandable to a broader patient population. In the first round, participants reviewed the booster scripts, and provided suggestions for how to improve them. In the second round, participants reviewed the adapted automated booster scripts based on the feedback from the first round of FGDs in this phase.
Phase 6: CIs to test the booster scripts
Finally, we conducted two rounds of CIs with patients who participated in earlier steps of the adaptation process, again due to their familiarity with the other intervention components. The first round of CIs included 7 participants and the second round included 5 different participants. Different participants were included in the two stages to gain detailed feedback on the understanding of each booster script from a broader range of participants. In these final CIs, the interviewers and participants role-played receiving the automated booster or the live booster sessions in real time. For example, for the live booster session, the interviewer called the participant (in the same room) and read through the booster script and participants commented on their understanding of each message.
Research Ethics
This study received ethical approval from the University of California, San Francisco Institutional Review Board (IRB), the Mbarara University of Science and Technology Research and Ethics Committee, and the Uganda National Council on Science and Technology.
Analysis
The research team, including local Ugandan researchers as well as US-based researchers with experience in intervention development in the Ugandan context, engaged in a rapid group analytic process [50, 51]. This analytic process was chosen due to the pragmatic and non-exploratory nature of the research objectives, the multi-phased data collection procedures, and time constraints involved in preparing the adapted intervention for testing in the clinical trial. All team members participated in the analysis and interpretation of the data. The first set of FGDs in phase 2 were analyzed in Dedoose software using an inductive and deductive approach, guided by a collaboratively developed coding framework [52]. Data from FGDs and CIs conducted in phases 3 and beyond, involved a group review and discussion of transcripts and interview reports, followed by collaborative development of analytical matrices and memos. Matrices were pre-populated, and themes organized by core elements of the intervention, while allowing unanticipated themes to emerge from the data.
Results
We describe adaptations of the HWHL intervention for the Ugandan context that were made with the intent to retain core intervention elements and their theoretical underpinnings (Table II). We frame these cultural adaptations using three broad thematic categories informed both by findings from inductive analyses and prior theoretical approaches to cultural adaptation [33]: 1) social and economic contexts; 2) concepts and metaphors; and 3) language and communication styles.
Table II.
Summary examples of cultural adaptation
| Theoretical component | Workbook Section/Core Element | Cultural Adaptation Examples |
|---|---|---|
| Motivation | Empathetic approach | • Added prompt for counselor to ask participant how they are feeling today and to tell the counselor a bit about themselves (e.g., if they are married, have children) |
| Information & motivation | Learn about the harmful effects of alcohol use | • Added examples of culturally salient harmful effects of alcohol use on individuals and their families, including the financial costs of alcohol use which could prevent people from providing for their family, risk of violence, keeping one from having close relationships, or starting a family. • Described depression and anxiety using culturally relevant terms. • Added additional relevant harmful effects of alcohol use on body including nausea and vomiting. Described delirium tremens in lay language understood locally. • Added context-specific images of the harmful effects of alcohol use highlighted by participants. |
| Information, Social norms theory, and cognitive dissonance | Learn about low-risk drinking, a standard drink, elicit self-comparison with levels of drinking in the context | • Replaced drawing of standard drinks from the US with pictures/drawings of standard drinks in Uganda. • Replaced statistics about women’s drinking in Baltimore with statistics about women’s and men’s drinking in western Uganda. • Added where the participant falls in comparison to these statistics based on their AUDIT-C score |
| Motivation | Decisional balance: Reasons to quit or cut down alcohol | • Added culturally salient reasons to reduce or quit drinking, in the categories of 1) family (e.g., ‘take better care of my family’, to ‘be better respected by others in family/community’); 2) health and sex life (e.g. ‘to have more energy’, ‘to avoid sexual assault’); 3) Finances (e.g. ‘to not destroy my work/to keep my job’, ‘to have more money for food & school fees’, to ‘avoid being robbed or cheated’) |
| Behavioral skills, social norms theory, value expectancies | Identify situations that make you want to take alcohol | • Added examples of culturally salient ‘risky situations’ including when people offer to buy me drinks’, ‘when working in bar, with alcohol present’, ‘when living close to a bar’, when ‘having money problems’ or ‘no food at home’ |
| Behavioral skills, and social cognitive theory | Self-efficacy: How do handle risky situations | • Added examples of culturally salient strategies including taking tea, reading the bible, calculating how much money you can save by not buying alcohol, remembering that you want to be respected by your family and others in your community. • Added culturally relevant photos of strategies to reduce/avoid alcohol use. |
| Motivation | Accountability: Make an agreement about drinking | • Enhanced discussion regarding whether the participant thinks it is realistic to quit drinking right now, with inclusion of examples of what reducing drinking can mean. • Added language to discuss parameters of drink reduction before moving to the agreement. |
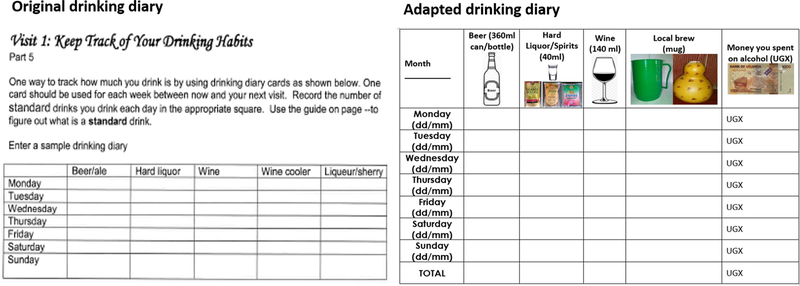
| Behavioral skills & motivation | Self-monitoring: keep track of your drinking habits in a drinking diary | • Inclusion of locally relevant images of standard drinks in drinking diary • Added a column to tally the amount of money spent on alcohol each day • Inclusion of detailed instructions about how to fill out the drinking diary, including how much money spent on alcohol over the week. • Included guidance on identifying a time in the day to fill out the drinking diary |
| Motivation | Social support: identify a support person | • Included guidance on identifying a trusted person who could support the participant in filling out the drinking diary and adding more explicit guidelines for inviting the support person to join the second counseling session. • Included guidance in the second counseling session for inviting the support person into the room and discussing tips to support the participant. |
| Motivation | Individualized feedback on drinking diary | • Enhanced feedback discussion in second counseling visit to have counselor ask how drinking agreement went for the participant and discuss most difficult and easiest aspects of usage. • Enhanced guidance for counselors on helping participants to identify patterns in their drinking. |
| Behavioral skills and social cognitive theory | Self-efficacy: create a self-help action plan | • Removed discussion of most people finding it easier to change drinking habits if they don’t keep alcohol in the house • Added “I’m cutting down on taking alcohol to save money” to the list of ways to say no to drinking alcohol. • Added culturally relevant ways to relax instead of drinking alcohol including “read your holy book and/or pray” • Provided an option to create a new drinking agreement in the second session if the original one wasn’t working. |
Social and economic contexts of alcohol use
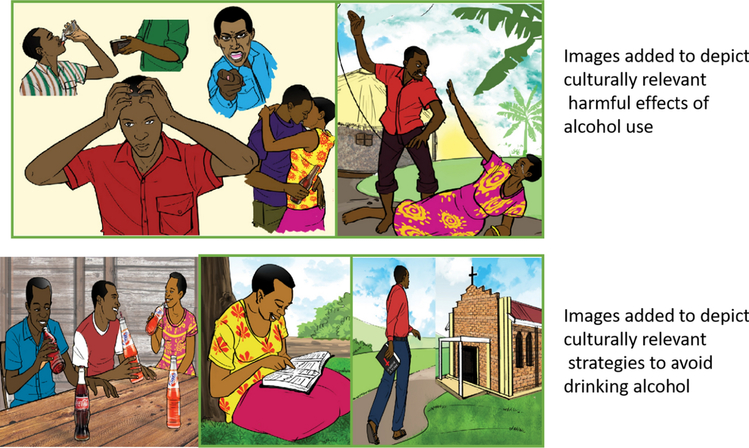
We found that drinking is largely conceptualized as a social activity and primarily occurs in local bars with friends, during public celebrations and gatherings, and rarely at home. As one man (age 30) noted “if it is not for friends, I don’t drink. I only drink when I go with friends to a bar or when I go for a party.” As a result, we replaced references in the original workbook about refraining from keeping alcohol in the home, with information on the social contexts of drinking. Because of the social nature of drinking, some participants described feeling pressured to drink by their peers and during social events. The pressure to drink was especially salient for people who worked in bars. One female bar owner (age 37) noted, “when I give a customer a drink, he will also buy for me, then I also drink. If I don’t drink, he will think that I have given him poison.” Accordingly, suggestions for how to manage working in a bar and peer pressure, such as drinking soda instead of alcohol (Figure 1), were added to the section of the workbook that addressed strategies to handle risky situations for drinking.
Figure 1.
Images added to intervention workbook as a result of the cultural adaptation process in Uganda
While drinking in public was described as the norm, it was described as being more acceptable for men than women. Some attributed this difference to gendered expectations that women prioritize caring for their children over drinking. Such expectations were described to manifest within the household, with some noting that a woman drinking at the bar instead of staying at home or caring for the children could result in domestic conflict. One man (age 52) stated, “Most women would like to leave bars late because they also are stressed, but many times, they fear […] their husbands’ rules. […] However, as for the men, they do not experience such fears.”
While drinking in public was more socially acceptable for men, participants noted the negative social consequences for both men and women. Specifically, the financial cost of drinking emerged as a salient theme across multiple FGDs. Some participants noted that they used the money needed for school fees, food, and household supplies to buy alcohol. This was especially salient for men, given the gendered expectation that men should provide for their family. As one man described:
If you counted the amount of money spent on alcohol, money meant for the family and the people you live with, after becoming sober, you get so disappointed with yourself […] You just go to a hide-out, and by the time you realize the intensity of the harm, you will have cheated your family so much. (Male, 52 years)
The influence of alcohol on the ability to fulfill gendered expectations related to caretaking and providing for one’s family was not included in the original intervention and was thus added to the workbook section on harmful effects of alcohol and reasons to stop drinking. Further, participants suggested that seeing the money they saved by reducing alcohol use would motivate them to reduce drinking. Accordingly, they requested that a column be added to the drinking diary to keep track of the money they spent/saved on alcohol each week (Figure 2). Calculating the amount of money saved by reducing or quitting drinking and thinking about the ways that money could be spent, were also added to the workbook section on strategies to reduce drinking.
Figure 2.
Adaptations made to the intervention ‘Drinking Diary’
A related theme concerned the loss of social standing and reputation associated with alcohol use. One man described the loss of respect associated with hazardous alcohol use in the following way:
Another thing that can motivate you to stop [drinking] is the respect you have in your home and amongst your friends. When you get home sober, you are respected. However, when you come home drunk, no one will respect you; even your children will leave you in the sitting room because you are drunk. Again, when you see how ugly other drunkard people are, you feel you should leave alcohol. When you see a sober man coming out of the restaurant, you are touched, and you want to be like him. If you also see another one who comes out of the bar crawling, you feel so bad, you want to stop. (Male, 50 years) As a result, being respected by others was added to the sections focusing on reasons to reduce or quit drinking and the harmful effects of alcohol.
Another salient theme that emerged was that alcohol increased risk for theft, fights, sexual assault and intimate partner violence (IPV). The threat of sexual assault and IPV, and their interplay with health risks such as sexually transmitted infections (STIs) and ART non-adherence, was especially salient for women, as illustrated in the following quotes:
There are instances where you find a drunk woman being dragged outside [the bar] and men rape her one after the other, yet she is HIV positive. You find even the men are also infected and the woman ends up contracting multiple diseases because of being drunk. (Female, 35 years)
Another thing that causes one to want to cut down on drinking, like us who have husbands, after drinking, a fight ensues. He will come when he is high [drunk], and you too are high, and you will exchange blows, then you will spend a week away without even taking your drugs [ART]. By the time you fought in the bar, there was no opportunity to go back home to pick your bag containing the drugs [ART]. (Female, 28 years)
In response to these findings, images of IPV were included in pictorial displays and discussed in the workbook section on risks of alcohol consumption (Figure 1).
Concepts and metaphors
Concepts
Concepts refer to the local understanding of alcohol use and how individuals conceptualize reducing drinking in this context. Participants, particularly men, discussed the important role alcohol played in social and peer bonding, and feared losing these bonds if they stopped drinking. One participant shared the following:
Your friend can call you for a drink, and when you say that you gave up on those things, he will tell you, ‘what kind of man are you, a man that can’t go and mix with his fellow men.’ When he tells you that, you become so disheartened and you decide to go. (Male, 30 years)
To maintain these bonds, participants identified other social activities that did not include alcohol such as drinking soda or tea, joining a club, playing cards, or watching TV (Figure 1). Some suggested reading holy books or attending church to avoid drinking. Further, given the potentially negative economic consequences of drinking and the cultural emphasis on providing for one’s family, participants expressed a desire to learn a new trade or start a business as an alternative to drinking alcohol. All of these suggestions were included in the workbook section on strategies to reduce drinking.
Metaphors
Another important consideration in the adaptation process was the varying literacy levels in the setting. As a result, the team incorporated images into the workbook to help convey messages to participants with lower levels of literacy. A local artist created culturally relevant images to depict the messages discussed throughout the workbook including the harmful effects of alcohol (an image of a man holding an empty wallet and an image of a man beating his wife; Figure 1) and how to handle risky situations (an image of a man drinking soda instead of beer with his friends; Figure 1). The HWHL workbook included pie charts showing the proportion of men and women who frequently consume alcohol. However, the Ugandan research team had difficulty translating these to the local context in a way that would be accessible for the expected range of participant education levels. Following discussions, the pie charts were replaced with a discussion about norms of alcohol use in the Ugandan context.
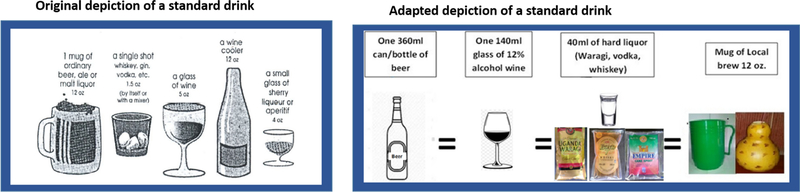
The HWHL workbook included drawings to help participants visualize a standard drink. However, participants in the present study noted the standard drinks pictured in the original workbook (a mug of beer/ale, a shot of hard alcohol, a glass of wine etc.) were less common in Uganda. Thus, we added images of locally-salient standard drinks including a bottle of beer, a glass of “alcohol wine,” local brew and Ugandan hard liquor – ‘waragi’ (Figure 3). Participants also suggested including the pictures of the standard drinks in the drinking diary to help people more accurately document their intake.
Figure 3.
Adaptations made to the depiction of the standard drink
Language and communication styles
The intervention materials were translated into the local language, Runyankole, and the local research team flagged words and concepts not easily translated. For example, in the original version of the intervention, alcohol use was discussed as a risk factor for depression and anxiety. In discussions with participants, the concept of depression was not easily translated or understood. The most closely related concept was stress. While ‘stress’ is a word in both English and Runyankole, it is a term that includes a number of symptoms, which are now included in the workbook.
Considerations also had to be made for the communication styles in the context. Participants noted the importance of greetings and suggested that more time be spent at the beginning of each session to formally greet participants. They also emphasized that we should not prioritize brevity, because participants did not want to feel rushed through the sessions. Further, congratulating individuals for their effort and their achievement was important. As a result, a portion of the first session was spent on introductions and participants were congratulated on their hard work throughout the workbook, particularly at the end.
Finally, while some felt it was important to congratulate those who met or made progress towards their drinking goals, others voiced a preference for an authoritarian approach from counselors including directives to quit drinking entirely and chastising those who did not. Such participants were concerned that messages to reduce, but not quit drinking, would lead to more drinking in the long term. As one participant shared:
There is nothing like low-risk drinking; every drink is harmful because it distorts one’s memory. You start with the intention of taking one drink, but you end up consuming more and more. That if you are to take two drinks, you will without a doubt take four and/or more. (Male, 36 years)
Another man (age 55) said, “We know that alcohol is bad, so why do you give them the liberty to drink a little? Let us just tell them that it is bad to drink.” The research team chose not to incorporate these suggestions given the evidence underlying IMB theory and prior empirical evidence supporting the use of positive reinforcement as a more effective means to facilitate behavior change [37]. Punitive language is also at odds with the motivational interviewing approach, which advocates for a collaborative, affirming, harm reduction orientation in behavior change interventions. Supporting this choice, participants described that drinkers often face stigma in health care settings and called for more non-judgmental care in relation to their alcohol use. Further, many participants felt that booster messages of positive reinforcement were personally encouraging and made them feel cared for. As one participant said,
I will say to myself, ‘this person seems to care about my health more than me, why not stick to his advice?’ Then I do that. I feel so good because he is following me so much, he cares about my health. (Male, 55 years)
Discussion
We describe the adaptation of a brief alcohol reduction intervention, largely informed by the IMB model, for the Ugandan context. We identified important cultural facets of the drinking context and culture of Uganda, which needed to be accounted for in the adaptation. Among them were adaptations to varying literacy levels in this setting; adaptations intended for lower literacy participants were also favored by more literate participants. Key adaptations were made to the motivations for reducing alcohol consumption to include salient concepts such as retaining the respect of family and community members and saving money. We also adapted key characteristics of the original intervention to reflect the social nature of drinking in Uganda. For example, we removed content focused on alcohol use in one’s home, and added content related to the risks of theft, fights, IPV, sexual assault, and peer pressure to drink. Adaptions to behavioral skills included identifying culturally relevant strategies to reduce alcohol use, such as taking tea or calculating how much money one will save through reducing or quitting alcohol.
Research from Uganda has highlighted similar social and economic contexts of alcohol use, confirming our findings and supporting our rationale for making these adaptations. As noted previously, studies have documented the social nature of alcohol use [27–29] and its financial burden in this setting [27–29]. Research has also documented the association between alcohol use and violence and victimization in Uganda [53, 54]. In agreement with prior research, we found that drinking was seen as threat to one’s social standing and reputation. Indeed, achieving the respect of one’s peers and community members is particularly important in SSA, where ties of dependence (whether mutual and inter-dependent or patron-client ties) work to strengthen social and financial stability [55]. Social standing and respectability, which is largely shaped by one’s ability to fulfill gendered expectations of providing for or caring for one’s family, is an important component of both masculine and feminine gender normativity in similar settings [56, 57]. Men with families in this setting are also motivated to reduce drinking to maintain the respect of their families and communities allowing for better fulfillment of their gendered role as fathers and providers [28, 53].
Our cultural adaptation is consistent in some respects with prior adaptation frameworks in that we conducted formative qualitative research to understand the local cultural context of alcohol consumption, and reviewed alcohol reduction EBIs for PLHIV to inform the selection of the HWHL intervention [15, 31, 32, 34–36]. We identified and retained the core elements of the HWHL intervention [32, 34–36], and conducted FGDs to assess which key characteristics of the intervention were salient and needed to be adapted [32, 34–36]. We also conducted role-plays of intervention components with patients, which is similar to the “theater test” in the ADAPT-ITT model [36], whereby facilitators implement modules of the EBI that capture the core elements of the intervention with the target population. After the theater testing, the audience provides feedback about the appropriateness of each module and identifies additional activities that should be included to enhance the intervention’s relevance and impact.
Several aspects of the adaptation approach for this study are to our knowledge unique: the adaptation process was highly iterative, involving four rounds of FGDs and three rounds of CIs with patients and stakeholders. Intervention content was revised after each data collection point, yielding ten phases of revision. Previous cultural adaptation approaches typically only include two to three phases of review and revision [15, 32, 34, 36]. This iterative approach permitted multiple opportunities for the target population to provide input. Previous cultural adaptation approaches allow for limited input from the target population, with many relying primarily on key stakeholders or experts [15, 32, 36]. For example, while ADAPT-ITT allows for the target population to provide input about the relevance and acceptability of the original intervention at the beginning of the adaptation, this framework does not re-engage the target population in reviewing the adapted intervention, and instead, relies on topical experts [36]. By allowing the target population ample opportunity to provide feedback, our approach potentially increases the saliency of concepts, and addresses the unique needs of the target population.
The inclusion of CIs as a method appears to be particularly novel. In our review of existing cultural adaptation approaches for EBIs, none mentioned using CIs as a method. This approach is particularly relevant for cultural adaptations as it provides insight into how participants understand the context of the intervention, and in turn, allows researchers to ensure that adapted materials convey their desired meanings.
While the process described above was conducted to culturally adapt an EBI to reduce alcohol use and improve health outcomes of PLHIV, a similar process could also be beneficial for researchers conducting cross-cultural alcohol-related HIV prevention research. As noted previously, research has documented that the norms and context of alcohol use varies across cultures and countries [23, 24, 58]. It is critical for interventions seeking to reduce alcohol and its negative effects on HIV risk behaviors, to consider how the dynamics of alcohol use (e.g., norms, values, customs, and contexts of alcohol use) might differ across cultures, and tailor their interventions accordingly. Failing to account for these cross-cultural differences could limit intervention relevance and, ultimately, its efficacy and effectiveness [31].
Despite the strengths of this adaptation method, there are some limitations. Specifically, although the multiple iterations of data collection and intervention refinement likely improved the saliency of the intervention for the Ugandan context, the process may be too time-consuming for researchers in other settings. However, we believe that engaging the target population in the process of adaptation, including checking to ensure adaptations successfully reflected their input, may facilitate the success of an adapted intervention. The study team was not able to incorporate every adaptation recommended by participants (for example, as mentioned, we refrained from reprimanding people for not achieving goals); there are instances where the intervention design ran counter to what some participants would have preferred, in order to retain fidelity to the theoretical underpinning of the intervention.
Conclusions
Our approach towards cultural adaptation of a brief alcohol reduction intervention for PLHIV in Uganda involved identifying core theoretically informed elements, and iteratively modifying content following multiple rounds of data collection and analysis. This approach offered the target population multiple opportunities to provide input and ensured that their voices shaped the product even as fidelity to key intervention characteristics was retained. The intervention is currently being tested for efficacy.
Acknowledgements
We would like to thank the participants who engaged in this study. We gratefully acknowledge the Uganda Ministry of Health, Mbarara University of Science and Technology (MUST), Mbarara Regional Referral Hospital, the staff of the Mbarara Immune Suppression Syndrome Clinic, our research and administrative teams at MUST and UCSF. We would also like to acknowledge the study counselors David Mugumya and Frances Musinguzi.
Funding: This research was supported by the National Institutes of Health (NIH) through the National Institute on Alcohol Abuse and Alcoholism (NIAAA) with grants R01AA024990 (PI: Hahn) and K24022586 (PI: Hahn). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health
Footnotes
Conflicts of interest statement: The authors have nothing to disclose.
Declarations:
Ethical approval: This study received ethical approval from the University of California San Francisco Institutional Review Board (IRB), the Mbarara University of Science and Technology Research and Ethics Committee, and the Uganda National Council on Science and Technology.
Consent to participate: All participants provided informed consent.
Consent for publication: Not applicable
Availability of data and material: Data will be made available upon request to the investigators Hahn, Camlin, and Muyindike
Code availability: Not applicable
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.UNAIDS. Global AIDS Update: Miles to go- closing gaps breaking barriers righting injustices. Geneva, Switzerland, 2018. [Google Scholar]
- 2.Duko B, Ayalew M, Ayano G. The prevalence of alcohol use disorders among people living with HIV/AIDS: a systematic review and meta-analysis. Subst Abuse Treat Prev Policy 2019; 14(1): 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reid MC, Fiellin DA, O’Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med 1999; 159(15): 1681–9. [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health, Uganda. Uganda Population-based HIV Impact Assessment (UPHIA) 2016–2017: Final Report. Kampala, Uganda, 2019. [Google Scholar]
- 5.World Health Organization. Global status on alcohol and health 2018. Geneva, Switzerland, 2018. [Google Scholar]
- 6.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci 2007; 8(2): 141–51. [DOI] [PubMed] [Google Scholar]
- 7.Woolf-King SE, Fatch R, Cheng DM, et al. Alcohol Use and Unprotected Sex Among HIV-Infected Ugandan Adults: Findings from an Event-Level Study. Arch Sex Behav 2018; 47(7): 1937–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol Use and Human Immunodeficiency Virus (HIV) Infection: Current Knowledge, Implications, and Future Directions. Alcohol Clin Exp Res 2016; 40(10): 2056–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. The Impact of Alcohol Use and Related Disorders on the HIV Continuum of Care: a Systematic Review : Alcohol and the HIV Continuum of Care. Curr HIV/AIDS Rep 2015; 12(4): 421–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Velloza J, Kemp CG, Aunon FM, Ramaiya MK, Creegan E, Simoni JM. Alcohol Use and Antiretroviral Therapy Non-Adherence Among Adults Living with HIV/AIDS in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. AIDS Behav 2020; 24: 1727–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N Engl J Med 2016; 375(9): 830–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva, Switzerland, 2016. [PubMed] [Google Scholar]
- 13.Carrasco MA, Esser MB, Sparks A, Kaufman MR. HIV-Alcohol Risk Reduction Interventions in Sub-Saharan Africa: A Systematic Review of the Literature and Recommendations for a Way Forward. AIDS Behav 2016; 20(3): 484–503. [DOI] [PubMed] [Google Scholar]
- 14.Papas RK, Gakinya BN, Mwaniki MM, et al. A randomized clinical trial of a group cognitive-behavioral therapy to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction 2021; 116(2): 305–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papas RK, Sidle JE, Gakinya BN, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction 2011; 106(12): 2156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.L’Engle KL, Mwarogo P, Kingola N, Sinkele W, Weiner DH. A randomized controlled trial of a brief intervention to reduce alcohol use among female sex workers in Mombasa, Kenya. J Acquir Immune Defic Syndr 2014; 67(4): 446–53. [DOI] [PubMed] [Google Scholar]
- 17.Zule W, Myers B, Carney T, Novak SP, McCormick K, Wechsberg WM. Alcohol and drug use outcomes among vulnerable women living with HIV: results from the Western Cape Women’s Health CoOp. AIDS Care 2014; 26(12): 1494–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braithwaite RS, Nucifora KA, Kessler J, et al. How inexpensive does an alcohol intervention in Kenya need to be in order to deliver favorable value by reducing HIV-related morbidity and mortality? J Acquir Immune Defic Syndr 2014; 66(2): e54–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chander G, Hutton HE, Lau B, Xu X, McCaul ME. Brief Intervention Decreases Drinking Frequency in HIV-Infected, Heavy Drinking Women: Results of a Randomized Controlled Trial. J Acquir Immune Defic Syndr 2015; 70(2): 137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasin DS, Aharonovich E, O’Leary A, et al. Reducing heavy drinking in HIV primary care: a randomized trial of brief intervention, with and without technological enhancement. Addiction 2013; 108(7): 1230–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pew Research Center. Cell phones in Africa: Communication Lifeline, 2015.
- 22.Campbell JI, Haberer JE. Cell Phone-Based and Adherence Device Technologies for HIV Care and Treatment in Resource-Limited Settings: Recent Advances. Curr HIV/AIDS Rep 2015; 12(4): 523–31. [DOI] [PubMed] [Google Scholar]
- 23.Savic M, Room R, Mugavin J, Pennay A, Livingston M. Editor’s Choice: Defining “drinking culture”: A critical review of its meaning and connotation in social research on alcohol problems. Drug-Educ Prev Polic 2016; 23(4): 270–82. [Google Scholar]
- 24.Room R, Makela K. Typologies of the cultural position of drinking. Journal of Studies on Alcohol 2000; 61(3): 475–83. [DOI] [PubMed] [Google Scholar]
- 25.Graham K, Bernards S, Knibbe R, et al. Alcohol-related negative consequences among drinkers around the world. Addiction 2011; 106(8): 1391–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bond JC, Roberts SCM, Greenfield TK, Korcha R, Ye Y, Nayak MB. Gender Differences in Public and Private Drinking Contexts: A Multi-Level GENACIS Analysis. International Journal of Environmental Research and Public Health 2010; 7(5): 2136–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breuer C, Bloom B, Miller AP, et al. “The Bottle Is My Wife”: Exploring Reasons Why Men Drink Alcohol in Ugandan Fishing Communities. Soc Work Public Health 2019; 34(8): 657–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sileo KM, Kizito W, Wanyenze RK, et al. A qualitative study on alcohol consumption and HIV treatment adherence among men living with HIV in Ugandan fishing communities. AIDS Care 2019; 31(1): 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sundararajan R, Wyatt MA, Woolf-King S, et al. Qualitative study of changes in alcohol use among HIV-infected adults entering care and treatment for HIV/AIDS in rural southwest Uganda. AIDS Behav 2015; 19(4): 732–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Castro FG, Barrera M, Martinez CR The cultural adaptation of prevention interventions: Resolving tensions between fidelity and fit. Prevention Science 2004; 5(1): 41–5. [DOI] [PubMed] [Google Scholar]
- 31.Castro FG, Barrera M Jr., Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol 2010; 6: 213–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barrera M Jr., Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol 2013; 81(2): 196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J Abnorm Child Psychol 1995; 23(1): 67–82. [DOI] [PubMed] [Google Scholar]
- 34.Hutton HE, Lancaster KE, Zuskov D, et al. Cultural Adaptation of 2 Evidence-Based Alcohol Interventions for Antiretroviral Treatment Clinic Patients in Vietnam. J Int Assoc Provid AIDS Care 2019; 18: 2325958219854368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKelroy VSG JS; Cummings B; Jones P; Harshbarger C; Collings C; Gelaude D; Carey JW; ADAPT Team. Adapting Evidence-Based Behavioral Interventions for New Settings and Target Populations. AIDS Education and Prevention 2006; 18(Supplement A): 59–73. [DOI] [PubMed] [Google Scholar]
- 36.Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. J Acquir Immune Defic Syndr 2008; 47 Suppl 1: S40–6. [DOI] [PubMed] [Google Scholar]
- 37.Fisher JDF, W.A.. Changing AIDS-risk behavior. . Psychological bulletin 1992; 111(3). [DOI] [PubMed] [Google Scholar]
- 38.Bandura A Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall, 1986. [Google Scholar]
- 39.Borsari B, Carey KB. Descriptive and injunctive norms in college drinking: a meta-analytic integration. J Stud Alcohol 2003; 64(3): 331–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Festinger L Cognitive dissonance. Sci Am 1962; 207: 93–102. [DOI] [PubMed] [Google Scholar]
- 41.Wigfield A, Eccles JS. Expectancy-Value Theory of Achievement Motivation. Contemp Educ Psychol 2000; 25(1): 68–81. [DOI] [PubMed] [Google Scholar]
- 42.Cox WM, Klinger E. A motivational model of alcohol use. J Abnorm Psychol 1988; 97(2): 168–80. [DOI] [PubMed] [Google Scholar]
- 43.Jonas DE, Garbutt JC, Amick HR, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2012; 157(9): 645–54. [DOI] [PubMed] [Google Scholar]
- 44.Resnicow KS R; Braithwaite RL; Ahluwalia JS; Butler J Cultural sensitivity in substance use prevention. Journal of Community Psychology 2000; 28(3): 271–90. [Google Scholar]
- 45.Green J, Thorogood N. Qualitative methods for health research. 2 ed. Thousand Oaks, CA: Sage, 2006. [Google Scholar]
- 46.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications, 2005. [Google Scholar]
- 47.Hahn JA, Cheng DM, Emenyonu NI, et al. Alcohol Use and HIV Disease Progression in an Antiretroviral Naive Cohort. J Acquir Immune Defic Syndr 2018; 77(5): 492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hahn JA, Emenyonu NI, Fatch R, et al. Declining and rebounding unhealthy alcohol consumption during the first year of HIV care in rural Uganda, using phosphatidylethanol to augment self-report. Addiction 2016; 111(2): 272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007; 31(7): 1208–17. [DOI] [PubMed] [Google Scholar]
- 50.Watkins DC. Rapid and Rigorous Qualitative Data Analysis: The “RADaR” Technique for Applied Research. International Journal of Qualitative Methods 2017; 16: 1–9. [Google Scholar]
- 51.Beebe J Rapid qualitative inquiry : a field guide to team-based assessment. Second edition. ed. Lanham: Rowman & Littlefield, 2014. [Google Scholar]
- 52.Dedoose. Dedoose. 7.0.23 ed. Los Angeles, CA: SocioCultural Research Consultants, LLC, 2016. [Google Scholar]
- 53.Sileo KM, Kintu M, Chanes-Mora P, Kiene SM. “Such Behaviors Are Not in My Home Village, I Got Them Here”: A Qualitative Study of the Influence of Contextual Factors on Alcohol and HIV Risk Behaviors in a Fishing Community on Lake Victoria, Uganda. AIDS Behav 2016; 20(3): 537–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wolff B, Busza J, Bufumbo L, Whitworth J. Women who fall by the roadside: gender, sexual risk and alcohol in rural Uganda. Addiction 2006; 101(9): 1277–84. [DOI] [PubMed] [Google Scholar]
- 55.Swidler A, Watkins SC. Ties of dependence: AIDS and transactional sex in rural Malawi. Stud Fam Plann 2007; 38(3): 147–62. [DOI] [PubMed] [Google Scholar]
- 56.Siu GE, Seeley J, Wight D. Dividuality, masculine respectability and reputation: how masculinity affects men’s uptake of HIV treatment in rural eastern Uganda. Social science & medicine (1982) 2013; 89: 45–52. [DOI] [PubMed] [Google Scholar]
- 57.Chantelois-Kashal H, Apenem Dagadu N, Gardsbane D. Contested femininity: strategies of resistance and reproduction across adolescence in northern Uganda. Cult Health Sex 2019: 1–16. [DOI] [PubMed] [Google Scholar]
- 58.Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and Cultural Contexts of Alcohol Use Influences in a Social-Ecological Framework. Alcohol Res-Curr Rev 2016; 38(1): 35–45. [PMC free article] [PubMed] [Google Scholar]