Abstract
Objective:
The evaluation of the effect of a mammography decision aid (DA) designed for older women at risk for lower health literacy (LHL) on their knowledge of mammography’s benefits and harms and decisional conflict.
Methods:
Using a pretest-posttest design, women > 75 years at risk for LHL reviewing a mammography DA before and after their [B] primary care provider visit. Women were recruited from an academic medical center and community health centers and clinics.
Results:
Of 147 eligible women approached, 43 participated. Receipt of the DA significantly affected knowledge of mammography’s benefits and harms [B] (pre-test (M = 3.75, SD = 1.05) to post-test (M = 4.42, SD = 1.19), p = .03). Receipt of the DA did not significantly affect decisional conflict (pre-test (M = 3.10, SD = .97) to post-test (M = 3.23, SD = 1.02), p = .71, higher scores = lower decisional conflict). The majority of the women (97%) indicated that the DA was helpful.
Conclusions:
Women found a mammography screening DA helpful and its use was associated with these women having increased knowledge of mammography’s benefits and harms.
Practice Implications:
With the shift toward shared decision-making for women > 75 years, there is a need to engage women of all literacy levels to participate in these decisions and have tools such as the one tested in this study.
Keywords: Mammography decision aid, Health literacy, Older women, Screening
1. Introduction
Women aged 75 and older are the fastest growing segment of the US population and breast cancer incidence increases with age [1]. Almost 14% of women > 75 years are diagnosed with breast cancer [2] Screening mammography is effective in detecting breast cancer when tumors are small and decreases breast cancer mortality in women 50–74 years [3,4]. However, the benefits may not outweigh the harms for women > 75 and particularly those women with short life expectancies (LE). Women need 5–10 years of LE to have a chance to benefit from mammography screening. Therefore, those with short LEs may only experience harms from being screened [5,6]. Harms of mammography screening include: pain and anxiety related to the test, complications from additional tests after a false positive mammogram, [P] complications from biopsies, and overdiagnosis, ([Q] diagnosis of breast cancers that otherwise would not have caused problems or symptoms in an older woman’s lifetime. [7]
Guidelines from organizations such as the US Preventive Services Task Force and the American Academy of Family Physicians indicate current evidence is insufficient to determine the balance of the benefits and harms of mammography in women > 75 years [4]. Guidelines state older women should be informed of the uncertainty of benefit and potential for harm. Guidelines further encourage clinicians to consider patient health and LE before offering screening [8,9]. However, Medicare covers annual mammograms for all women > 65 years [10] and many older women are screened regardless of their LE. Few older women are informed of mammography’s harms and most overestimate the benefits. [C] [11,12]
1.1. Decision aids
Decision aids (DAs) are decision support tools that are educational and designed to inform [R] individuals about available tests or treatments and their potential benefits and harms. DAs increase knowledge of the benefits and harms of tests and treatments, increase participation in decision-making, and improve decision quality [13]. A mammography screening DA, “Should I continue having mammograms? For women age 75–84 years,” was developed to help women > 75 years decide whether or not to continue with mammography [14]. The DA includes information on older women’s breast cancer risk, LE, outcomes of screening, competing mortality risks, breast cancer treatments, and a values clarification exercise.
The DA was recently tested in a large randomized controlled trial of women > 75 years and findings indicate the DA increased women’s knowledge of the benefits and harms of mammography screening and led to fewer older women choosing to be screened [15]. However, the DA was developed and tested with few women with LHL and data from the RCT suggests older women with lower educational attainment, a factor of LHL, were less likely to understand the DA. Therefore, in a prior qualitative study, women with LHL reviewed the DA and suggested edits to make it easier for them to understand [16]. Based on their suggestions and using health literacy principles (e.g, use of plain language, short sentences, pictures, a glossary, and avoidance of medical jargon), this paper-based mammography DA was modified for use with older women with lower health literacy. The modified DA is available in the appendix and on e-prognosis to print.
1.2. Importance of health literacy
Health literacy is “the ability to obtain, process, or understand basic health information needed to make appropriate health care decisions” [17]. Lower health literacy (LHL) is associated with adults over the age of 75, low educational attainment, minorities, or low-income populations [18] and is associated with a lack of medical knowledge, low self-efficacy, and less desire to participate in treatment decision-making [19-21]. Attention to low literacy principles when developing health materials is increasingly important and critical to [T] ensure all vulnerable populations, in particular older adults, are able to access information [22]. Despite this, few DAs are written for patients with LHL and further research is needed to ensure populations with LHL levels have access to tools to support their decision-making [23,24]. Thus, the objective of the study was to evaluate the effect of the LHL mammography screening DA for women >75 on older women’s knowledge of the benefits and harms and decisional conflict around mammography screening. We hypothesized use of the DA would increase women’s knowledge of mammography’s benefits and harms and decrease decisional conflict among older women.
2. Methods
2.1. Study design
We tested the efficacy of a mammography screening DA designed for women > 75 years at risk for LHL in a pretest-posttest trial. We recruited women for this study from three sites including a large Boston-based academic medical center, one community health center affiliated with the medical center, and from 9 community health clinics affiliated with a safety-net hospital in Cambridge, MA. Beth Israel Deaconess Medical Center’s Institutional Review Board approved this study.
2.1.1. Inclusion criteria
Inclusion criteria for all women regardless of site included: women between 75 and 89 years and women who identified at risk for LHL with a response of “somewhat to not at all confident” to the validated health literacy question [D] [25], “How confident are you filling out medical forms by yourself?” and/or who had completed some college or less. Exclusion criteria included: women >90 years because on average, women >90 years have < 5-year LE [26]; may have dementia, which is common (36%) among this population and few are screened [27]; who had a history of breast cancer; whose medical records indicated [U] they did not have a mammogram in the past three years; and women who scored >9 on the Orientation-Memory-Concentration Test [28] indicating severe cognitive impairment. [V] We asked women to explain in their own words the purpose of the study and the benefits and harms to participating to ensure their ability to provide informed consent. Finally, to target women who may be contemplating screening, we excluded women who had been screened in the past 6 months, and women with documentation indicating they had declined future mammograms.
2.2. Participants
We identified participants using electronic medical records. Our electronic search identified women ages 75–89 who met the inclusion criteria. We first obtained approval from their primary care physicians (PCPs). After receiving approval from PCPs, we mailed eligible patients an [W] information letter about the study and a number to call if they wanted to opt-out of being contacted. We contacted women who did not opt-out of initial telephone contact to confirm eligibility and to assess willingness to participate. We obtained verbal informed consent from participants. A research assistant (RA) (A.J and M.K.) administered the pretest survey over the phone after obtaining consent. We then asked women to come to a routine appointment with their PCP early to read the DA. After reading the DA, which takes approximately 5–10 min, participants attended their scheduled visit. After the visit, the (RA) administered the posttest survey. The posttest survey was administered in person after the visit or over the phone (depending on the participant’s preference and access to a phone). We conducted reminder calls a week before and the day before their PCP appointment. Participants were offered $40 as incentive for participating in the study. See Fig. 1 for diagram of the screening, enrolling (and follow-up) of the participants.
Fig. 1.
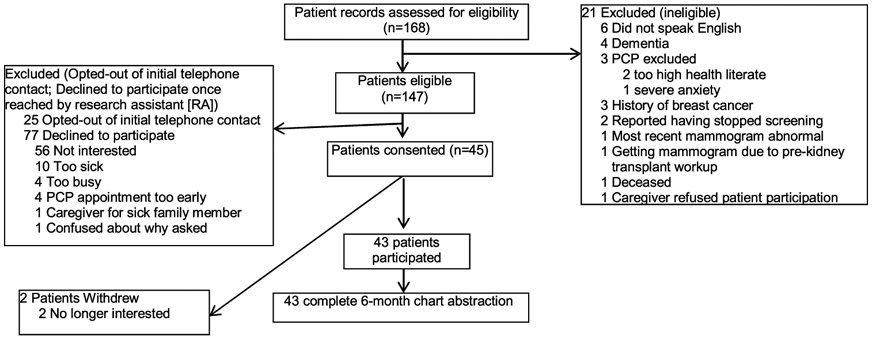
Mammography Screening Decision Aid, Enrollment, and Follow-up of Trial Participants.
2.3. Data collection
At baseline, we assessed participants’ socio-demographic characteristics, including race/ethnicity, educational attainment, health insurance, and LE (using a validated measure developed by [29] where a score of > 10 indicates LE of < 10 years. We also assessed knowledge of mammography’s benefits and harms and decisional conflict. Our posttest questionnaire re-assessed women’s decisional conflict and knowledge about mammography. It also asked about women’s decision-making role and their perceptions of the acceptability of the DA. We conducted chart abstractions of women at 6 months after reviewing the DA to determine if there was a note from their PCP documenting a discussion about mammography.
2.3.1. Outcomes
Knowledge about mammography was assessed with 7 questions (true or false); See Appendix. [K] Questions were adapted from other studies [30-33] and based on material in our DA. The questions were pilot tested among 18 women with LHL. We summed the number of correct responses.
Decisional Conflict. The Decisional Conflict Scale: SURE [X] (Sure of myself; Understand information; Risk-benefit ratio; Encouragement) test is a validated 4-item scale for clinical practice to measure whether patients feel sure about their treatment options, know the benefits and risks of their options, whether they feel clear about their personal values, and have enough support to make a choice [34]. Decisional conflict is the most commonly used outcome in decision aid trials [35]. To create an overall score, the 4 items were summed. Scores ranging from 0 [extremely high decisional conflict] to 4 [no decisional conflict]. A score of < 3 indicates decisional conflict. Individual items had scores of 0 (No) or 1(Yes) to the four items.
Decision-Making Role. In the posttest survey only, we evaluated older women’s preferred role in decision making about mammography. Answers from 5 statements from the Control Preference Scale were categorized as shared, passive (deferring to the physician), or active (the patient makes the final decision) [36,37].
Acceptability. In the posttest survey only, we asked about the DA’s length, clarity, balance, whether it is anxiety provoking, and whether participants would recommend it to a friend [38].
Chart abstraction. We reviewed the notes in participants’ medical records to determine if a discussion about mammography screening occurred.
2.4. Analyses
For continuous outcomes, knowledge and decisional conflict, we used paired t-tests to examine changes in scores before and after reading the DA. For individual items of the outcomes in each scale (e.g., each knowledge question, SURE test individual items), we used the McNemar’s test to examine differences from pre to posttest because the outcomes were categorical. We provide descriptive statistics for decision-making roles, acceptability of the DA and the chart abstraction review. We used SPSS25 to conduct all analyses.
3. Results
Of the 147 eligible patients approached for this study, 25 opted out, 77 refused and 45 agreed to participate. However, 2 withdrew leaving 43 participants. On average, participants were 78 years old and 57% identified as non-Hispanic Black. [E] Non-participants had similar demographic characteristics with an average age of 79 years and 42% who identified as non-Hispanic Black. More than half (52%) had [Y] completed and received a high school degree or obtained their [F] high school equivalency certificate (GED) and 43% (18) indicated they were somewhat confident or less in their ability to fill out medical forms. Finally, 63% (27) had an estimated LE < 10 years [29]. The mean score was 10. 1 + 3.5 with a range of 3–17. Participant characteristics are presented in Table 1.
Table 1.
Characteristics of 43 Patients (Median Age, 78 Years).
| Characteristica | Value No. % |
|---|---|
| Recruitment Site | |
| Academic Medical Center | 23 (53) |
| Community Health center | 5 (12) |
| Safety-net hospital community affiliates | 15 (35) |
| Race/Ethnicity | |
| Non-Hispanic White | 17 (40) |
| Non-Hispanic Black | 26 (60) |
| Educational Attainment | |
| Less than high school | 9 (21) |
| High school/GED | 24 (56) |
| Some college/Associate’s degree | 10 (23) |
| Age, mean (SD) | 78 + 3.74 |
| 75–79 years | 34 (79) |
| 80–84 years | 5 (12) |
| 85+ years | 4 (9) |
| Level of confidence in filling out medical forms | |
| Extremely confident | 18 (42) |
| Quite a bit confident | 6 (14) |
| Somewhat confident | 14 (33) |
| A little confident | 1 (2) |
| Not at all confident | 3 (7) |
| Missing | 1 (2) |
| Self-reported health status | |
| Excellent | 4 (9) |
| Very good | 6 (14) |
| Good | 18 (42) |
| Fair | 14 (33) |
| Poor | 1 (2) |
| Estimated Life Expectancya | |
| <10 years | 27 (63) |
| >10 years | 16 (37) |
Life expectancy was estimated using the Schonberg mortality index: Scores for participants ranged from 3 to 17. Scores >10 are associated with >50% chance of 10-year mortality. Thus, adults who score >10 are estimated to have <10- year life expectancy.
3.1. Pre-test post-test trial
There was a significant change in the overall score for knowledge about the benefits and harms of mammography screening [H] at pre-test (M = 3.75 correct on 7 item test, SD = 1.05) to post-test (M = 4.42, SD = 1.19), p = .03). Women tended to do better on [H] post-test versus pre-test questions related to understanding a mammogram would not prevent an older woman from getting breast cancer; most women who have abnormal mammograms do not have breast cancer; more women age 75 and older die of heart disease than breast cancer; and their health matters when considering whether or not to have a mammogram. [H] Scores were worse at post-test compared to pre-test for two of the questions: the benefit of having a mammogram is finding and treating a breast cancer when it is small and can be treated only with minor surgery and some breast cancers found by a mammogram would never have shown up or caused problems in a woman’s lifetime. See Table 2 for further details.
Table 2.
Decision Aid Pretest and Posttest Data Based on Participant-Reported Outcome.
| Outcome | Pretest | Posttest | p value |
|---|---|---|---|
| Decisional Conflict Scale mean (SD) | 3.10 (.97) | 3.23 (1.02) | .71 |
| a Response of “I don’t know:” 4 | |||
| Do you feel sure about the best choice for you in terms of whether or not to have a mammogram? | .97 (.16) | .89 (.32) | .22 |
| Do you know the benefits and risks or downsides of having a mammogram? | .59 (.50) | .74 (.44) | .23 |
| Are you clear about which benefits and risks of having a mammogram matter most to you? | .77 (.43) | .77 (.43) | 1.00 |
| Do you have enough support and advice to make a choice about when to stop having a mammogram? | .77 (.43) | .84 (.37) | .69 |
| Knowledge about mammography mean (SD) correct | 3.75 (1.05) | 4.42 (1.19) | .03 |
| a Response of “I don’t know:” 7 | |||
| The benefit of having a mammogram is finding and treating a breast cancer when it is small and can be treated with only minor surgery (Correct answer: true) (Response of “I don’t know:” 6) | .97 (.16) | .90 (.33) | .08 |
| Having a mammogram will prevent an older woman from getting breast cancer (Correct answer: false) (Response of “I don’t know:” 7) | .68 (.47) | .87 (.33) | .04 |
| Most women who have an abnormal mammogram have breast cancer (Correct answer: false) (Response of “I don’t know:” 7) | .81(.40) | .90 (.30) | .26 |
| More women aged 75 or older die of heart disease than breast cancer (Correct answer: true) (Response of “I don’t know:” 7) | .66 (.48) | .75 (.44) | .37 |
| Your other health problems should affect whether or not you have a mammogram (Correct answer: true) (Response of “I don’t know:” 6) | .26 (.44) | .31 (.47) | .59 |
| Some breast cancers found by a mammogram would never have shown up or caused problems in a woman's lifetime (Correct answer: true) (Response of “I don’t know:” 7) | .66 (.48) | .58 (.50) | .44 |
| Some breast cancers do not show up on a mammogram (Correct answer: true) (Response of “I don’t know:” 7) | .80 (.41) | .80 (.41) | 1.00 |
We did not categorize as an incorrect response if they did not know.
There was no significant change in overall score on the decisional conflict SURE test; however participants did tend to report being more likely to know the benefits and downsides of mammography (pretest: M = 0.59, SD = .50; posttest: M = .74, SD = .44, p = .23) and more likely to feel supported in their mammography decision (pretest: M = .77, SD=.43; posttest: M = .84, SD = .37, p = .69). However, overall women tended to be less sure in their decision (pretest: M = .97, SD = .16; posttest: M = .89; SD = .32, p = .69). See Table 2 for further details.
In terms of preferred role in decision-making around mammography screening, 42% (18) indicated they wanted to make the decision on their own and 35% (15) indicated they wanted to share the decision with their physician. Only 23% (10) wanted their PCP to make the final screening decision after reading the DA. In addition, women had a mean score of 3.60 (+.93) on the preparation for decision making scale of 1–5, suggesting that participants felt the DA would prepare them quite a bit for decision-making. Of note, women were most likely to report using this scale the DA helped them recognize a decision needs to be made about whether or not to have a mammogram. See Table 3 for further details.
Table 3.
Role and preparation in decision making regarding mammography screening.
| Preferred role in mammography screening No (%) | |
| Active, patient makes decision | 18 (42) |
| Shared with physician | 15 (35) |
| Passive, physician makes decisions | 10 (23) |
| Missing | 0 |
| Preparation for Decision-Making mean (SD)b (Missing: 2) Help you | 3.60 (.93) |
| 1. recognize that a decision needs to be made about whether or not to have a mammogram (M = 3.88, SD = 1.20) | |
| 2. make a better decision about whether or not to have a mammogram (M = 3.63, SD = 1.45) | |
| 3. think about the benefits and risks of having a mammogram (M = 3.65, SD = 1.23) | |
| 4. think about which benefits and risks about having a mammogram most important to you (M = 3.51, SD = 1.24) | |
| 5. know that the decision whether or not to have a mammogram depends on what matters to you most (M = 3.67, SD = 1.26) | |
| 6. organize your own thoughts about the decision about whether or not to have a mammogram (M = 3.58, SD = 1.58) | |
| 7. think about how involved you want to be involved in the decision (M = 3.63, SD = 1.45) | |
| 8. identify questions you want to ask your doctor about mammography (M = 3.49, SD = 1.45) | |
| 9. prepare you to talk to your doctor about what matters most to you about whether or not to have a mammogram (M = 3.57, SD = 1.31) | |
| 10. prepare you for a visit with your doctor (M = 3.35, SD = 1.63) | |
| Documented note from PCP about mammography screening | |
| No documented note about discussion | 25 (58) |
| Documented note from PCP | 18 (42) |
| Will continue | 12 (67) |
| Will not continue | 4 (22) |
| Undecided | 2 (11) |
Preferred role in mammography screening = 5 item index to assess patients’ preferred involvement in decision-making. We categorized responses as active (patient made the final decision) versus passive too or shared with doctor to learn women’s roles.
Preparation for Decision Making = 10 item index (each item scored 1[not at all] to 5 [a great deal] points) to see if the DA prepared them to communicate with their clinician.
Chart reviews of each participants occurred at 6 months after the follow-up visit. Of the 43 participants, 18 or 42% had a note in their medical records documenting a discussion with their PCP about whether or not to continue mammography screening. Of the 18 who had a discussion, 4/18 (22%) indicated discontinuing mammography screening and 2 (5%) were unsure. [J] For the women with a documented discussion about stopping screening, the LE scores were 6, 7, 10 and 12. Thus half had a LE < 10 years and the other half had a LE > 10 years. See Table 3 for further details.
Regarding acceptability of the DA, the majority of women felt the length was just right 83% (14); the amount of information was just right 91% (39) and the information was clear 93% (40). Further, 93% reported understanding most or all of the information in the DA. The majority of the women (97%) indicated the DA was helpful to them in making a mammography screening decision. Most (65%) women did not feel the DA made them anxious. Of note, 58% percent (7/12) of women with a high school education or less reported some anxiety reading the DA whereas only 10% of women with some college education reported feeling this way. In addition, 91% (37) would recommend the DA; 91% (39) prefer DAs to be on paper and 68% (27) would like DAs mailed (or emailed) before a visit rather than receiving the DA at the visit. See Table 4 for further details.
Table 4.
Acceptability of Decision Aid.
| Acceptability variable | n = 43 |
|---|---|
| Length of decision aid (n = 41 respondents) | |
| A little too short | 4/41 |
| Just right | 34/41 |
| A little too long | 3/41 |
| Amount of information (n = 41 respondents) | |
| Much more than needed | 1/41 |
| A little more than needed | 1/41 |
| Just right | 39/41 |
| Clarity of the information (n = 41 respondents) | |
| Information was clear | 40/41 |
| Information was unclear | 1/41 |
| Information Slant (n = 41 respondents) | |
| Slanted towards not having a mammogram | 7/41 |
| Completely balanced | 16/41 |
| Slanted towards having a mammogram | 18/41 |
| Understanding of the information (n = 41 respondents) | |
| I understood a little of the information | 3/41 |
| I understood most of the information | 21/41 |
| I fully understood all of the information | 17/41 |
| DA helpful in making a decision about mammography (n = 41 respondents) | |
| Not helpful | 1/41 |
| Helpful | 40/41 |
| Reading the decision aid made me feel:(n = 40 respondents) Anxious | |
| Very anxious | 3/40 |
| A little anxious | 9/40 |
| Not anxious at all | 28/40 |
| Recommend use of the DA (n = 42 respondents) | |
| Not recommend | 3/42 |
| Recommend | 39/42 |
| Preferred format (n = 43 respondents) | |
| Paper format | 39/43 |
| Web-based or mobile application | 1/43 |
| No preference | 3/43 |
| Preference on when to receive DA (n = 41 respondents) | |
| Mailed before a visit | 27/41 |
| Emailed before a visit | 2/41 |
| In waiting room before a visit | 4/41 |
| From doctor at visit | 7/41 |
| From doctor’s staff after visit | 1/41 |
4. Discussion and conclusion
4.1. Discussion
Results from this study suggested the DA increased knowledge about the benefits and harms of mammography screen which is consistent with the literature [13]. Results also indicated older women at risk for LHL found the DA to be helpful and acceptable. The DA may help women at risk for LHL realize it is a decision whether or not to keep having mammograms after age 75 and as a result, more older women with < 10 year LE and little chance to benefit may choose to stop being screened.
The mammography DA increased older women’s knowledge about the benefits and harms of mammography screening. This is important because many studies have shown most older women are screened with little knowledge of the benefits and harms [39-41]. While knowledge scores improved overall, there were 2 questions where women’s knowledge did not improve. The two questions were about understanding the benefit of a mammogram is early detection and minor treatment and understanding overdiagnosis that can occur with mammography screening. There are several possible reasons why women’s knowledge did not improve for these questions. First, these two questions were longer and/or double-barreled. Future research will include designing knowledge surveys for populations with lower health literacy and will focus on learning how to explain overdiagnosis to older women with or at risk for LHL since scores did not improve on this question. [K] Overdiagnosis is a difficult concept to explain to patients because the idea of finding a small, slow- growing breast cancer as a result of mammography screening may be harmful rather than beneficial is counterintuitive. We define overdiagnosis as overdetection in the DA as “13 women out of 1000 who continue having mammograms are told that they have breast cancer but their breast cancers are growing so slowly that they would never have caused problems.” [42]. Prior research [42-44] suggest shared-decision-making discussions consider using DA’s as a strategy to communicate overdiagnosis. Further, findings from a prior qualitative study [16] suggested that women at risk for LHL wanted earlier knowledge about diagnosis to get treated. This finding may be applicable to this study because the women were set in their thoughts about these two questions. Thus, the combination of the long questions and their personal understanding of the benefits contributed to worsening scores. It is also possible the women in this study needed more time to review the DA even though they read it in 5–10 min and in fact 66% noted they would prefer to receive the DA in the mail before the visit rather than at the time of the visit likely because they would then have more time to review it and [K] share with family or friends.
Although overall changes in decisional conflict did not significantly improve, they did improve for perceiving greater knowledge about the benefits and downsides of mammography and feeling supported in their decision, but got slightly worse for being sure in their decision. Many of the women were very enthusiastic about screening. The DA may have made these women more aware about the harms of screening and as a result, these women became more conflicted. A score of less than 4 on the SURE test indicates clinically significant decisional conflict [45]. Previous research [46] indicates that while the goals of DAs are to reduce decisional conflict, there is evidence that having decisional conflict can promote appropriate deliberations about outcomes, personal goals and engagement in the decision-making process. Thus, decisional conflict can increase as a result of being more aware of the risks of an intervention [29]. This concept may explain the dichotomy for the women in this study who were very enthusiastic about screening but possibly became more uncertain of their screening decision as they became more aware screening’s harms. Interestingly, 78% of the women in this study indicated they wanted an active or shared role with their physician in deciding about mammography suggesting that when recognizing there are harms to screening, women want to be involved in screening decisions. Despite the lack of significance, findings from this study suggest women shifted their views from simply accepting getting a mammography to thinking about whether a mammography is right for them based on the benefits and harms. This is consistent with findings from Schonberg et al. [15] that indicated women > 75 made more informed decisions when receiving a DA before a PCP visit.
Years of previous and current public health messaging encourage women to get screened for mammography regardless of age. However, nearly all guidelines recommend not screening older women with < 10-year LE [8,9] and our data indicates more than half of the women had LEs <10 years. Similar to previous research [16], findings suggest the DA may help older women prepare for a conversation with their PCP, especially because the majority found the DA helpful and because 42% had a documented note about a discussion about mammography in their charts. Again, evidence [47] suggests that populations with LHL do not feel comfortable having conversations and some of the women in this study did so. Specifically, findings [47] indicate that patients with adequate health literacy were almost two times more likely than those with LHL to prefer patient-involved decision-making confirming previous evidence indicating that patients with LHL lack the self-efficacy to be actively involved in their care [48,49]. Possible reasons for the findings may be the DA had information to suggest the decision is theirs to make or to share with their physicians. A benefit of this finding is that having women feel prepared to have a conversation with their providers may alleviate some of the fears providers may have about having conversations with older women about continuing or discontinuing cancer screening [49]. Interestingly, it may be even more important that providers reduce their concerns about having conversations given findings from this study that suggest women with high school degrees or less did report more anxiety reading the DA than women with some college. While all women found the DA helpful, it may be that for older women with the lowest health literacy, use of a DA with a health education counselor to help them may be the most effective [50]. It is possible the combination of a DA in combination with non-medical staff (health educator, social worker, community health worker) would also be more effective in helping older women such as the ones in this study, understand the concept of overdiagnosis.
In the previous investigation [16] to modify the DA for older women at risk for LHL, there was an explicit intent to explain that mammography screening was a personal decision. Results from this study indicated that the majority of the women thought the DA would prepare them quite a bit for decision-making. Specifically, they thought the DA helped them recognize that a decision needs to be made about whether or not to have a mammogram. Previous evidence suggests more interventions are needed to support populations with LHL in their decision-making [13]. Because 39/42 would recommend the use of the DA, it is possible women in this study are interested in learning and understanding complexities related to health care decisions. This finding may be due to the fact that overall women perceived the DA acceptable – meaning they understood the information, felt it was clear and did not feel anxious while reading and thinking about it.
Finally, it is important to note that findings indicate 56% of women indicated that they were extremely confident or quite a bit confident in their response to the question, “How confident are you filling out medical forms by yourself?” We began the study identifying women at risk for LHL based on this validated question. Given the uneasiness we discovered about older women admitting their discomfort with medical forms and the recognition that using this question as our only criteria for defining a woman’s literacy level led us to initially exclude women for whom the DA may have been useful. Therefore, we added educational level for defining older women’s health literacy. Further, evidence indicates there is a stigma regarding lower health literacy. Thus, it may be difficult for individuals at risk for LHL to share concerns about understanding and using health information [51].
4.1.1. Limitations
There are several limitations to this study including a small sample size from one geographical area, which limits the ability to generalize to the greater older adult women with lower health literacy population. [M] Further, we were unable to account for screening intentions for the majority of women because we did not ask about their screening intentions halfway through the study. Finally, we could not assess if the DA affected individual’s preferred role in mammography screening because we did not assess at baseline.
4.2. Conclusion
We tested the effects of a modified DA to help older women at risk for LHL to understand decision making about mammography screening. While evidence indicates poor health literacy influences decision-making, findings from this study suggest a focus on developing and testing a DA can have positive effects, including increased knowledge about the benefits and harms of mammography screening.
4.3. Practice implications
With the shift toward shared decision-making for women > 75 years, there is a need to engage women of all literacy levels to make these decisions and tools to help them weigh the benefits and risks of mammography screening. Failing to account for health literacy in design of DAs and the design of the knowledge surveys to determine increases or decreases in knowledge, could inadvertently exacerbate existing inequalities in health. It is critically needed to provide older women with LHL [N] to help them decide with clear and understandable information about whether or not to get a mammogram. The DA is available at ePrognosis (https://eprognosis.ucsf.edu/decision_aids/Manmography_-LOW_LIT_75-84.pdf) for use. Results from this investigation will contribute to improving the quality of life for this vulnerable population.
Acknowledgments
Funding
This work was supported by the National Cancer Institute, United States, 3R01CA181357-03S1.
Appendix A
Knowledge questions (True or False)
The benefit of having a mammogram is finding and treating a breast cancer when it is small and can be treated with only minor surgery
Having a mammogram will prevent an older woman from getting breast cancer
Most women who have an abnormal mammogram have breast cancer
More women aged 75 or older die of heart disease than breast cancer
Your other health problems should affect whether or not you have a mammogram
Some breast cancers found by a mammogram would never have shown up or caused problems in a woman's lifetime
Some breast cancers do not show up on a mammogram
References
- [1].Ortman JM, Velkoff VA, Hogan H, An aging nation: the older population in the United States. Washington, DC: United States Census Bureau, Economics and Statistics Administration, US Department of Commerce. [Google Scholar]
- [2].Howlader N, Noone AM, Krapcho M, Garshell J, Neyman N, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975–2010, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/archive/csr/1975_2010/. [Google Scholar]
- [3].Independent UK Panel on Breast Cancer Screening, The benefits and harms of breast cancer screening: an independent review, Lancet 380 (9855) (2012) 1778–1786, doi: 10.1016/S0140-6736(12)61611-0. [DOI] [PubMed] [Google Scholar]
- [4].Siu AL, Screening for breast cancer: US Preventive Services Task Force recommendation statement, Ann. Intern. Med 164 (2016) 279–296. [DOI] [PubMed] [Google Scholar]
- [5].Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC, Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark, Br. Med. J. Clin. Res. Ed 8 (2013) 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Warner E, Breast-cancer screening, NEJM 365 (2011) 1025–1032. [DOI] [PubMed] [Google Scholar]
- [7].Schonberg MA, Decision-making regarding mammography screening for older women, J. Am. Geriatr. Soc 64 (12) (2016) 2413–2418, doi: 10.1111/jgs.14503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Breast cancer screening in older women. American Geriatrics Society Clinical Practice Committee, J. Am. Geriatr. Soc 48 (2000) 842–844. [PubMed] [Google Scholar]
- [9].U.S. Preventive Services Task Force. Final recommendation statement: Breast Cancer: Screening; 2019https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1.
- [10].Balanced Budget Act of 1997. Retrieved from https://www.govinfo.gov/content/pkg/PLAW-105publ33/pdf/PLAW-105publ33.pdf.
- [11].Schonberg MA, Breslau ES, McCarthy EP, Targeting of mammography screening according to life expectancy in women aged 75 and older, J. Am. Geriatr. Soc 61 (3) (2013) 388–395, doi: 10.1111/jgs.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Walter LC, Schonberg MA, Screening mammography in older women: a review, JAMA 311 (13)(2014) 1336–1347, doi: 10.1001/jama.2014.2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L, Decision aids for people facing health treatment or screening decisions, Cochrane Database Syst. Rev (4) (2017), doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Schonberg MA, Hamel MB, Davis RB, et al. , Development and evaluation of a decision aid on mammography screening for women 75 years and older, JAMA Intern. Med 174 (3) (2014) 417–424, doi: 10.1001/jamainternmed.2013.13639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schonberg MA, Kistler CE, Pinheiro A, et al. , Effect of a mammography screening decision aid for women 75 years and older: a cluster randomized clinical trial, JAMA Intern. Med 180 (6) (2020) 831–842, doi: 10.1001/jamainternmed.2020.0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Siska M, Schonberg MA, Modifying a mammography decision aid for older adult women with risk factors for low health literacy, HLRP: Health Lit. Res. Pract 5 (2) (2021) e78–e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Office of Disease Prevention and Health Promotion US Department of Health and Human Services, National Action Plan to Improve Health Literacy Health, US Department of Health & Human Services, 2010. https://health.gov/our-work/health-literacy/national-action-plan-improve-health-literacy. [Google Scholar]
- [18].Healthy People 2020. (n.d.). Health Literacy. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/health-literacy.
- [19].DeWalt DA, Boone RS, Pignone MP, Literacy and its relationship with self-efficacy, trust, and participation in medical decision making, Am. J. Health Behav 31 (2007) S27–35. [DOI] [PubMed] [Google Scholar]
- [20].Lyttle DJ, Ryan A, Factors influencing older patients’ participation in care: a review of the literature, Int. J. Older People Nurs 5 (2010) 274–282. [DOI] [PubMed] [Google Scholar]
- [21].Von Wagner C, Semmler C, Good A, Wardle J, Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ Couns;75:352–357. [DOI] [PubMed] [Google Scholar]
- [22].Rudd R, Implications of Health Literacy for Public Health: Workshop Summary, National Acaddemies Press, 2014. [PubMed] [Google Scholar]
- [23].Koops van ‘t Jagt R, Hoeks JC, Jansen CJ, de Winter AF, Reijneveld SA, Comprehensibility of health-related documents for older adults with different levels of health literacy: a systematic review, J. Health Commun 21 (2016) 159–177. [DOI] [PubMed] [Google Scholar]
- [24].McCaffery Kj, Holmes-Rovner M, Smith Sk, Rovner D, Nutbeam D, Clayman Ml, Kelly-Blake K, Wolf Ms, Sheridan Sl, Addressing health literacy in patient decision aids, BMC Med. Inform. Decis. Mak 13 (2013) S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Chew LD, Griffin JM, Partin MR, et al. , Validation of screening questions for limited health literacy in a large VA outpatient population, J. Gen. Intern. Med 23 (5) (2008) 561–566, doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Arias E, United States Life Tables, 2008. National Vital Statistics Reports, 61,15 (Table 3). [PubMed] [Google Scholar]
- [27].Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, Burke JR, Hurd MD, Potter GG, Rodgers WL, Steffens DC, Prevalence of dementia in the United States: the aging, demographics, and memory study, Neuroepidemiology 29 (2007) 125–132, doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H, Validation of a short Orientation-Memory-Concentration Test of cognitive impairment, Am. J. Psychiatry (1983), doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- [29].Schonberg MA, Hamel MB, Davis RB, et al. , Development and evaluation of a decision aid on mammography screening for women 75 years and older, JAMA Intern. Med 174 (3) (2014) 417–424, doi: 10.1001/jamainternmed.2013.13639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Mathieu E, Barratt A, Davey HM, McGeechan K, Howard K, Houssami N, Informed choice in mammography screening: a randomized trial of a decision aid for 70-year-old women, Arch. Intern. Med 167 (2007) 2039–2046. [DOI] [PubMed] [Google Scholar]
- [31].Stager JL, The comprehensive breast cancer knowledge test: validity and reliability, J. Adv. Nurs 18 (1993) 1133–1140. [DOI] [PubMed] [Google Scholar]
- [32].v van Agt H, Fracheboud J, van der Steen A, de Koning H, Do women make an informed choice about participating in breast cancer screening? A survey among women invited for a first mammography screening examination, Patient Educ. Couns 89 (2012) 353–359. [DOI] [PubMed] [Google Scholar]
- [33].Wilcox S, Stefanick ML, Knowledge and perceived risk of major diseases in middle-aged and older women, Health Psychol. 18 (346) (1999). [DOI] [PubMed] [Google Scholar]
- [34].Ferron Parayre A, Labrecque M, Rousseau M, Turcotte S, Legare F, Validation of SURE, a four-item clinical checklist for detecting decisional conflict in patients, Med. Decis. Making 34 (2014) 54–62. [DOI] [PubMed] [Google Scholar]
- [35].O’Connor AM, Validation of a decisional conflict scale, Med. Decis. Making 15 (1995) 25–30. [DOI] [PubMed] [Google Scholar]
- [36].Degner LF, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, O’neil J, Bilodeau B, Watson P, Mueller B, Information needs and decisional preferences in women with breast cancer, J. Am. Med. Assoc 277 (1997) 1485–1492. [PubMed] [Google Scholar]
- [37].Kryworuchko J, Stacey D, Bennett C, Graham Id., Appraisal of primary outcome measures used in trials of patient decision support, Patient Educ. Couns 73 (2008) 497–503. [DOI] [PubMed] [Google Scholar]
- [38].O’Connor A, Cranney A, User Manual—Acceptability, Ottawa Hospital Research Institute, 2002. [Google Scholar]
- [39].Hoffmann TC, Del Mar C, Clinicians’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review, J. Am. Med. Assoc 177 (2017) 407–419. [DOI] [PubMed] [Google Scholar]
- [40].Hoover DS, Pappadis MR, Housten AJ, Krishnan S, Weller SC, Giordano SH, Bevers TB, Goodwin JS, Volk RJ, Preferences for communicating about breast cancer screening among racially/ethnically diverse older women, J. Health Commun 34 (2019) 702–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Seaman K, Dzidic PL, Castell E, Saunders C, Breen LJ, A systematic review of women’s knowledge of screening mammography, Breast 42 (2018) 81–93. [DOI] [PubMed] [Google Scholar]
- [42].Davies L, Petitti DB, Martin L, et al. , Defining, estimating, and communicating overdiagnosis in cancer screening, Ann. Intern. Med 169 (July 3(1)) (2018) 36–43, doi: 10.7326/M18-0694. [DOI] [PubMed] [Google Scholar]
- [43].Hersch J, Jansen J, Barratt A, et al. , Women’s views on overdiagnosis in breast cancer screening: a qualitative study, BMJ 346 (2013) f158, doi: 10.1136/bmj.f158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].McCaffery KJ, Jansen J, Scherer LD, Thornton H, Hersch J, Carter SM, Barratt A, Sheridan S, Moynihan R, Waller J, Brodersen J, Walking the tightrope: communicating overdiagnosis in modern healthcare, BMJ (February 5) (2016) 352. [DOI] [PubMed] [Google Scholar]
- [45].Légaré F, Kearing S, Clay K, Gagnon S, D’Amours D, Rousseau M, O’Connor A, Are you SURE?: assessing patient decisional conflict with a 4-item screening test, Can. Fam. Phys 56 (2010) e308–314. [PMC free article] [PubMed] [Google Scholar]
- [46].Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA, Rethinking the objectives of decision aids: a call for conceptual clarity, Med. Decis. Making 27 (2007) 609–618. [DOI] [PubMed] [Google Scholar]
- [47].Seo J, Goodman MS, Politi M, Blanchard M, Kaphingst KA, Effect of health literacy on decision-making preferences among medically underserved patients, Med. Decis. Making 36 (2016) 550–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Mancuso CA, Rincon M, Asthma patients’ assessments of health care and medical decision making: the role of health literacy, J. Asthma 43 (2006) 41–44. [DOI] [PubMed] [Google Scholar]
- [49].Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH, Barriers and facilitators to shared decision-making among African-Americans with diabetes, J. Gen. Intern. Med 24 (1135) (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Schoenborn NL, Boyd CM, Lee SJ, Cayea D, Pollack CE, Communicating about stopping cancer screening: comparing clinicians’ and older adults’ perspectives, Gerontologist 17 (59) (2019) S67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Miller Km, Brenner A, Griffith Jm, Pignone Mp, Lewis Cl., Promoting decision aid use in primary care using a staff member for delivery, Patient Educ. Couns 86 (2012) 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]


