Abstract
Background
Erectile dysfunction (ED) is a prevalent health problem that seriously impacts men's quality of life. The potential treatment of ED by percutaneous approach has emerged with valid angiographic results and a significant improvement in symptoms and quality of life. In addition, cell-based regenerative therapies aiming at enhancing neovascularization have been successfully performed with peripheral blood mononuclear cells (PBMNCs) in diabetic patients affected by critical limb ischaemia.
Case summary
We report a case of a young insulin dependent (ID) diabetic patients who suffered of severe vasculogenic erectile dysfunction associated with a poor response for more than 1 year to oral phosphodiesterase-5 inhibitors (PDE5i) and intracavernous (IC) phosphodiesterase type 1 (PDE1) therapy. At selective angiography of the pelvic district, a severe atherosclerotic disease of the internal iliac and pudendal artery was evident with absence of distal vascularization of the cavernous bodies. The patient was treated by mechanical revascularization with drug-coated balloon and drug-eluting stent placement associated with IC injection of autologous PBMNCs. Immediate and 1-year clinical and angiographic follow-up are described.
Discussion
Percutaneous revascularization with drug-coated balloon and drug-eluting stent associated with IC autologous PBMNCs cells injection is a safe and effective procedure to restore normal erectile function in diabetic patients affected by severe vasculogenic ED not responding to conventional oral drug therapies.
Keywords: Erectile dysfunction, Sirolimus-eluting balloon, Autologous peripheral blood mononuclear cells, Case report
Learning points
Vasculogenic erectile dysfunction is a common complication of poor controlled type I diabetes mellitus. In particular, diabetic patients have dysfunction and reduction in endothelial cells, and cavernous smooth muscle cells content, associated to a severe inflammatory environment related to advanced glycate-end products production. In this setting, utilization of stem cells, which can differentiate into various cell types including endothelial cells (ECs), cavernous smooth muscle cells (CSMCs), Schwann cells, and neurons, has been proposed for erectile dysfunction treatment, based on the hypothesis that transplantation of stem cells into the penis might replenish depleted EC or CSMC content.
Peripheral blood mononuclear cells (PBMNCs) constituted by monocyte/macrophage and lymphocyte populations are known to act as a rich source of paracrine mediators and angiogenic factors, able to create trophic support for neo-endothelium. The role and the efficacy of a cellular therapy with PBMNCs have been documented in diabetic patients with chronic limb ischaemia that was not susceptible to revascularization, with decreased ischaemic pain and significative reduction of minor and major amputations.
It has been demonstrated that mechanical revascularization with drug-coated balloons (DCB) and drug-eluting stents (DES) can significantly improve erectile function in patients not responding anymore to oral phosphodiesterase inhibitors or intracavernous injection of prostaglandins. The first combined treatment (balloon angioplasty with DCB and DES together with intracavernous autologous PBMNCs injection by Hematrate® blood filtration system) is illustrated and described.
Introduction
Erectile dysfunction (ED) is defined as the recurrent inability to achieve and maintain an erection satisfactory for sexual intercourse. Erectile dysfunction is a prevalent health problem that seriously impacts men's quality of life and their partners.1 Although the majority of ED patients can be satisfactorily treated with phosphodiesterase type-5 inhibitors (PDE5i),2 these drugs can cause a variety of side effects that make them unsuitable for some patients. Moreover, particular patient subsets, such as those affected by diabetes, are poor responders to PDE5i treatment in more than 40% of cases.3
In this setting, diabetic patients are characterized by a multifactorial disease of sexual function characterized by endothelial cells (ECs) dysfunction, and reduction in cavernous nerves and cavernous smooth muscle cells (CVSMCs) content.4 In these patients, utilization of stem cells has been proposed for ED treatment, based on the hypothesis that these cells might replenish depleted endothelial cells or cavernous smooth muscle cells content and trigger the regeneration of the host's own ECs, restoring proper interactions between ECs and SMCs.5 Interestingly, cell-based regenerative therapies also aiming at enhancing neovascularization: peripheral blood mononuclear cells (PBMNCs) showed to be safe and effective in diabetic patients affected by critical limb ischaemia.6,7
Recently, the potential treatment of ED by percutaneous approach has emerged with valid angiographic results and a significant improvement in symptoms and quality of life. A Swiss group reported the 1-year outcomes in 50 consecutive patients affected by erectile dysfunction and internal pudendal artery (IPA) stenosis.8 Patients were treated employing standard balloon angioplasty (16%), drug-coated balloon (DCB, 27%), or drug-eluting stent (DES, 55%) implantation. Procedure success was achieved in 49 (98%) of 50 patients. At 12 months, 30 (65%) of 46 patients achieved a minimum of clinically relevant improvement in the International Index of Erectile Function Questionnaire score (IIEF).8
In this case report, we present to the best of our knowledge, the first combined treatment (balloon angioplasty with DCB and intra-cavernous autologous PBMNCs injection) in a patient affected by insulin-dependent diabetes mellitus and severe erectile dysfunction related to bilateral atherosclerotic disease. Clinical and angiographic long-term follow-up is described.
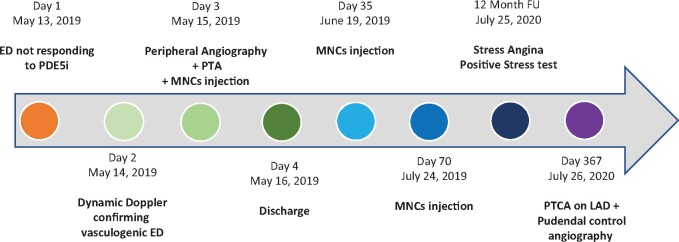
Timeline
Case presentation
A 57-year-old gentleman with a history of active smoking, insulin dependent diabetes mellito (IDDM), hypertension, dyslipidaemia, and chronic coronary artery disease (CAD), presented complaining of severe ED. He underwent percutaneous coronary intervention (PCI) in 2010 with implantation of three DES on left anterior descending artery, OM1, and right coronary artery. He was asymptomatic for chest pain, and echocardiography demonstrated normal cardiac function. He had normal external genitalia and secondary sexual characteristics. Sexual hormones analyses were in the reference range (total testosterone 7.34 ng/dL; free testosterone 17 pg/mL; sex hormone binding globulin 54 nmol/L; DHEA-S 394 g/dL). Ultrasound evaluation revealed normal prostate. Patient was taking 1 tablet of Bisoprolol 1.25 mg in the morning. He showed no response to increasing doses of different oral PDE5i drugs as well as no response to intra-cavernosal injections to prostaglandin E1 (IC-PDE1) over a 1-year period. Libido was normal. Dynamic Doppler Ultrasound with IC injection of PDE1 (Caverject® 10 mcg and after 10 min additional 10 mcg) showed a peak systolic velocity (PSV) of 12 cm/s on the left cavernosal artery and a PSV of 6 cm/s on the right cavernosal artery suggestive of a bilateral severe vasculogenic ED (normal response after Caverject > 25 cm/s). International Index of Erectile Dysfunction-5 questionnaire (IIEF) score was 3 points (normal 26–30; severe ED 6–10; moderate ED 11–16; mild ED 17–25). Selective angiography showed significant and diffuse atherosclerotic disease of the right mid and distal internal pudendal artery (IPA) associated with absence opacification of distal vascularization of the cavernous bodies and critical stenosis of the left internal iliac artery (IIA) (Figure 1A and D). By utilization of a 6 Fr. left internal mammary guiding catheter (Cordis, Milan, Italy), the left IIA was engaged, and a 0.014' BMW wire (Abbott, Milan, Italy) was utilized to cross the stenosis. After non-compliant 5 mm × 40 mm balloon pre-dilatation at 10 atm (Sequent Neo NC, B.Braun), a self-expandable 6 mm × 18 mm bare-metal stent (Vascuflex® – B.Braun,) was precisely placed at the ostium of the vessel with no residual stenosis (Figure 1B). Then, the IPA was engaged, and stenosis crossed by a Sion Blu 0.014' wire (Asahi Intecc Co. Japan) followed by semi-compliant balloon 2.0 mm × 20 mm (Sequent Neo, B. Braun) inflation at 10 atm in the proximal, mid, and distal segments and subsequently by sirolimus-eluting balloon 2.5 mm × 30 mm inflation (Magic Touch ED, Concept Medical) at proximal and middle segments followed by 2.0 mm × 20 mm sirolimus balloon inflation at the distal segment for 2 min at 8 atm, respectively. After waiting for 10 min to rule out elastic recoil, a 2 × 18 drug-eluting stent (DES; Supraflex Cruz, SMT) was implanted in the mid-segment of the IPA due to >30% residual stenosis with an optimal final acute result at control angiography (Figure 1E). Femoral access was closed by a 6 Fr Angioseal VIP closure device (Terumo Europe).
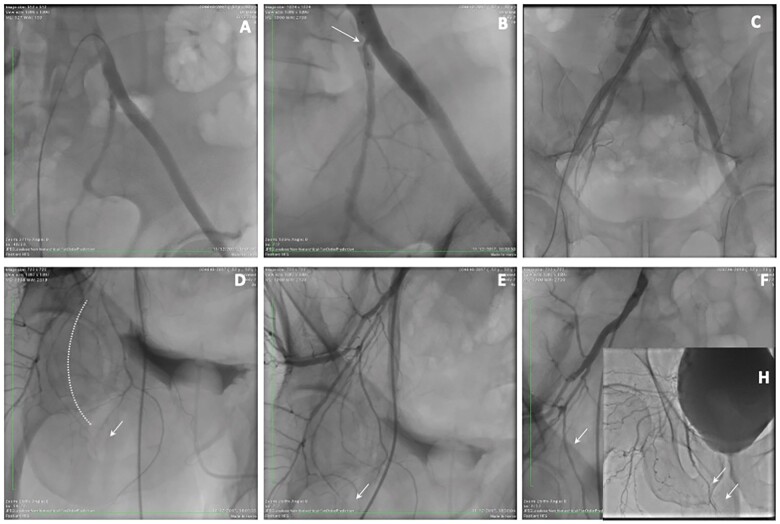
Figure 1.
Composite panel of basal angiography, acute result, and 1-year follow-up angiography. (A) Basal angiography showing critical stenosis of the left internal iliac ostial segment. (B) Balloon pre-dilatation. (C) Final result after stenting. (D) Basal right pudendal angiography demonstrating severe diffuse atherosclerotic disease of the proximal, middle, and distal segments (dotted line) with a complete absence of the distal pudendal artery and common penile artery (arrow). (E) Final angiography after treatment of drug-coated balloon and drug-eluting stent placement. (F) One-year follow-up demonstrating excellent patency of the entire pudendal artery and visualization (inset H) of the common penile and cavernous body small vessels (arrows).
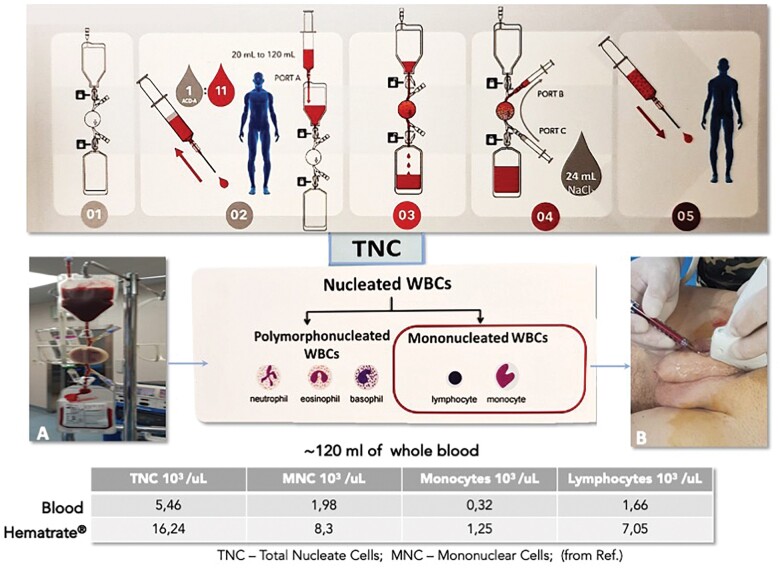
One hundred and twenty millilitre volume of peripheral blood was utilized to concentrate 12 mL of autologous mononuclear cells by point-of-care device (Hematrate® Blood Filtration System, Cook Regentec), designed to obtain an autologous concentration of mononuclear cells (MNCs) utilizing whole-blood selective filtration (Figure 2A). Mononuclear cells were immediately injected into the cavernous bodies under echo-guidance (Figure 2B). This procedure was repeated at 35 and 70 days after the index procedure, following the same protocol used for critical limb ischaemia non-option patients.6
Figure 2.
(Upper panel) Preparation of the Hematrate® blood filtration kit. (Number 1) Kit opening; (Number 2) 120 mL of whole blood is withdrawn from a peripheral vein of the patient and inserted in the upper bag; (Number 3) Blood is filling the lower bag after being selectively filtrated by gravity in approximately 30 min; (Number 4) After dilution with NaCl, filtrated blood is collected and re-injected into the patient (Number 5). (Middle panel) Total nucleated cells composed of polymorphonucleated white blood cells and mononucleated white blood cells are separated through the kit (inset A) and injected into the patient (inset B). (Lower panel) Total nucleated cell is concentrated three times, while mononuclear cells four times more than reference total nucleated cell values contained in the whole blood (from reference #15).
The patient's hospital course was without complications. He was discharged with aspirin 100 mg lifelong, clopidogrel 75 mg for 1 year (choice related to the presence of multiple risk factors, previous coronary revascularization and multiple stents placement in the pudendal arteries usually considered a low flow district), rosuvastatin 20 mg, and fenofibrate 200 mg, Tadalafil 5 mg/daily, and vitamin E supplementation. After 3-months from the procedure, the patient reported an excellent response to PDE5i. At 6-month, the patient underwent Dynamic Doppler ultrasound with 10 mcg of IC-PDE1, which showed peak systolic velocity of 27 cm/s on the left and 32 cm/s on the right cavernosal arteries. IEF-5 score was 16 (delta IEF 13), suggestive of an excellent mid-term result. No complication was observed at the site of MNCs injection at the time of out-patient visit. At 1-year follow-up, the patient reported stable improvement in sexual function with an IEF-5 score of 18. He underwent control angiography demonstrating complete stent patency of the left IIA (Figure 1C) and excellent result on the right IPA with a marked increase in vascularization of the distal IPA and common penile artery (Figure 1F and H—arrows).
Discussion
Given the high prevalence of erectile dysfunction in the diabetic male population and the significant psychological impact this symptom has on affected patients, different therapeutic approaches have been proposed. Albeit the mainstay of all therapies is represented by oral PDE5i in this setting, almost half of patients affected by diabetes do not respond to PDE5i treatment.3 Therefore, mechanical revascularization of the internal pudendal and dorsalis penis arteries has been proposed in patients who are not responsive to oral PDE5i.8–12
In addition, the need to develop a curative treatment for ED that could provide spontaneous unassisted intercourse has stimulated interest in utilizing adjunctive therapeutic modalities.3,5 The most futuristic treatment option in the vasculogenic ED is represented by autologous stem cell therapy.3 The regenerative effects of stem cells is mediated by the secretion of growth factors and cytokines, the paracrine effect, together their ability to migrate to the injury site along with cell contact and cellular differentiation.3
In the case reported herein, we have shown the significant clinical impact of a double strategy of percutaneous revascularization of IPA and IC injection of PBMNCs. Peripheral blood mononuclear cells constituted by monocyte/macrophage and lymphocyte populations (Figure 2) are known to act as a rich source of paracrine mediators and angiogenic factors, able to create trophic support for neo-endothelium.13,14 The Hematrate® Blood Filtration System is a point-of-care device for use in human cell therapy, that permits to produce MNCs which have in vivo and in vitro pro-angiogenic potential in a quick, safe, cost-effective way.15 Peripheral blood mononuclear cells allow repeatable implants avoiding local pain, haematomas, and anaemia that can follow bone marrow harvesting3 showing a high safety profile, as reported in meta-analysis in critical limb ischemia (CLI) patients.6 Furthermore, no complications or bleeding have been reported for other cell therapies injected into the corpora cavernosa.3,16
Peripheral blood mononuclear cells concentrated by Hematrate® releases angiogenic cytokines including fibroblast growth factor, vascular endothelial growth factor, hepatocyte growth factor, and granulocyte-colony stimulating factor and contains CD34+ endothelial progenitors cells and CD34+KDR+15 producing therapeutic angiogenesis in ischaemic tissue.6,14 Noteworthy, both PB-MNCs and shockwaves therapy, also used in non-responder patients, showed a common mechanism of action which is the ability to polarize inflammatory macrophage (M1) into anti-inflammatory and angiogenic macrophages M2.17,18
Conclusion
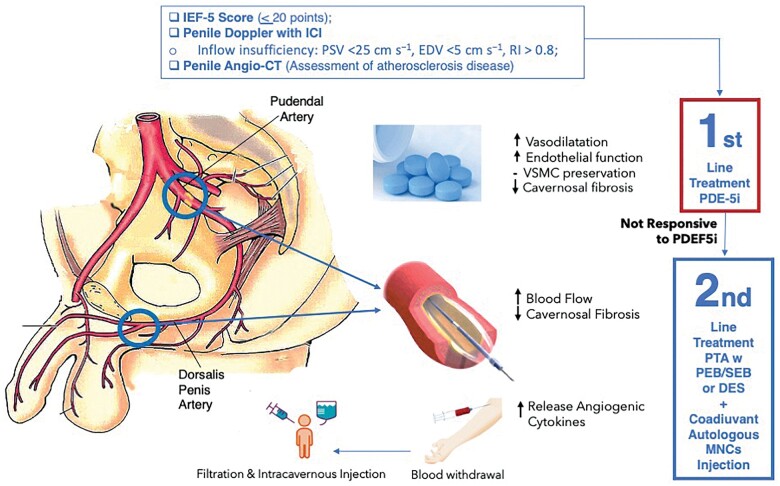
Revascularization with DCB and DES associated with IC autologous PBMNC injection is a safe and effective procedure to restore normal erectile function in diabetic patients affected by severe vasculogenic ED not responding to PDE5i therapy. The idea of the PBMNC cell therapy used as adjuvant therapy to revascularization (Figure 3), is based on the focus of trying to solve both the macro-vascular problem and the damaged microcirculation, well described in the diabetic patients. Larger series and future RCT are needed to confirm this preliminary experience.
Figure 3.
Proposed pathway for patient selection and treatment in patients presenting with erectile dysfunction. Patients with IIEF-5 score less than 20 points showing a PSV < 25 cm/s at Dynamic Doppler Examination should be submitted to pelvic Angio-CT to evaluate presence of atherosclerotic disease of the pudendal district. The first line treatment should always be PDE5i administration for at least 6 mos and only in case of no response patients can be submitted to selective angiography followed by PTA with -B and/or drug-eluting stent placement. In diabetic patients an adjunctive therapy may be represented by autologous mononuclear cells intracavernous injection to increase the release of angiogenic cytokines within the corpora cavernosa and stimulate neovascularization, as outlined in this case report. DCB, drug-coated balloon; DES, drug-eluting stent; IIEF, International Index of Erectile Function; PSV, peak systolic velocity.
Lead author biography
Dr Sangiorgi was born in Florence on October 4th 1965. He graduated at the University of Rome Tor Vergata in 1990. He is Board Certified in Cardiology (1994) and in Surgical Pathology (1999). He served as a Fellow in Cardiovascular Disease at the Mayo Clinic and Foundation, Rochester, USA from 1991 to 1998. He is currently the Chief of Cardiac Cath Lab of the University of Rome Tor Vergata. He is member of the ESC, SICI-GISE and SCAI. He served as board of Directors in the Italian Society of Interventional Cardiology (GISE). He is also a member of the Working Group on Interventional Cardiology and Coronary Circulation of the ESC. Dr. Sangiorgi is author of 380 medical papers in major international peer reviewed journals.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing these cases and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: n one declared.
Funding: None declared.
Supplementary Material
References
- 1.Gandaglia G, Briganti A, Jackson G, Kloner RA, Montorsi F, Montorsi P. et al. A systematic review of the association between erectile dysfun ction and cardiovascular disease. Eur Urol 2014;65:968–978. [DOI] [PubMed] [Google Scholar]
- 2.Lue TF.Erectile dysfunction. N Engl J Med 2000;342:1802–1813. [DOI] [PubMed] [Google Scholar]
- 3.Protogerou V, Chrysikos D, Karampelias V, Spanidis Y, El Bisari S, Troupis T.. Erectile dysfunction treatment using stem cells: a review. Medicines 2021;8:2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hidalgo-Tamola J, Chitaley K.. Type 2 diabetes mellitus and erectile dysfunction. J Sex Med 2009;6:916–926. [DOI] [PubMed] [Google Scholar]
- 5.Soebadi MA, Moris L, Castiglione F, Weyne E, Albersen M.. Advances in stem cell research for the treatment of male sexual dysfunctions. Curr Opin Urol 2016;5:222–235. [DOI] [PubMed] [Google Scholar]
- 6.Persiani F, Paolini A, Camilli D, Mascellari L, Platone A, Magenta A. et al. Peripheral blood mononuclear cells therapy for treatment of lower limb ischemia in diabetic patients: a single-center experience. Ann Vasc Surg 2018;53:190–196. [DOI] [PubMed] [Google Scholar]
- 7.Rigato M, Monami M, Fadini GP.. Autologous cell therapy for peripheral arterial disease: systematic review and meta-analysis of randomized, nonrandomized, and noncontrolled studies. Circ Res 2017;120:1326–1340. [DOI] [PubMed] [Google Scholar]
- 8.Diehm N, Marggi S, Ueki Y, Schumacher D, Keo HH, Regli C. et al. Endovascular therapy for erectile dysfunction—who benefits most? Insights from a single-center experience. J Endovasc Ther 2019; 2019;26:181–190. [DOI] [PubMed] [Google Scholar]
- 9.Sangiorgi G, Pizzuto A, Diehm N, Greco F, Fusco F, Chiricolo G. et al. Endovascular therapy for erectile dysfunction: a state of the art review. Minerva Cardioangiol 2020; doi: 10.23736/S0026-4725.20.05136-1. [DOI] [PubMed] [Google Scholar]
- 10.Rogers JH, Goldstein I, Kandzari DE.. Zotarolimus-eluting peripheral stents for the treatment of erectile dysfunction in subjects with suboptimal response to phosphodiesterase-5 inhibitors. J Am Coll Cardiol 2012;60:2618–2627. [DOI] [PubMed] [Google Scholar]
- 11.Wang T-D, Lee W-J, Yang S-C, Lin P-C, Tai H-C, Hsieh J-T. et al. Safety and six-month durability of angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: a first-in-man study. EuroIntervention 2014;10:147–156. [DOI] [PubMed] [Google Scholar]
- 12.Wang TD, Lee WJ, Yang SC.. Clinical and imaging outcomes up to 1 year following balloon angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: The PERFECT-2 study. J Endovasc Ther 2016;23:867–877. [DOI] [PubMed] [Google Scholar]
- 13.Krishnasamy K, Limbourg A, Kapanadze T, Gamrekelashvili J, Beger C, Häger C. et al. Blood vessel control of macrophage maturation promotes arteriogenesis in ischemia. Nat Commun 2017;8:952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel AS, Smith A, Nucera S, Biziato D, Saha P, Attia RQ. et al. TIE2-expressing monocytes/macrophages regulate revascularization of the ischemic limb. EMBO Mol Med 2013;5:858–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spaltro G, Straino S, Gambini E, Bassetti B, Persico L, Zoli S. et al. Characterization of the Pall Celeris system as a point-of-care device for therapeutic angiogenesis. Cytotherapy 2015;17:1302–1313. Elsevier Inc; [DOI] [PubMed] [Google Scholar]
- 16.Lokeshwar SD, Patel P, Shah SM, Ramasamy R.. A systematic review of human trials using stem cell therapy for erectile dysfunction. Sex Med Rev 2020;8:122–130. [DOI] [PubMed] [Google Scholar]
- 17.Arnold L, Henry A, Poron F, Baba-Amer Y, Van Rooijen N, Plonquet A. et al. Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory macrophages to support myogenesis. J Exp Med 2007;204:1057–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sukubo NG, Tibalt E, Respizzi S, Locati M, d’Agostino MC.. Effect of shock waves on macrophages: a possible role in tissue regeneration and remodeling. Int J Surg 2015;24:124–130. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.