Abstract
Background
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is challenging health systems all over the world. Particularly high-risk groups show considerable mortality rates after infection. In 2020, a huge number of case reports, case series, and consecutively various systematic reviews have been published reporting on morbidity and mortality risk connected with SARS-CoV-2 in solid organ transplant (SOT) recipients. However, this vast array of publications resulted in an increasing complexity of the field, overwhelming even for the expert reader.
Methods
We performed a structured literature review comprising electronic databases, transplant journals, and literature from previous systematic reviews covering the entire year 2020. From 164 included articles, we identified 3451 cases of SARS-CoV-2–infected SOT recipients.
Results
Infections resulted in a hospitalization rate of 84% and 24% intensive care unit admissions in the included patients. Whereas 53.6% of patients were reported to have recovered, cross-sectional overall mortality reported after coronavirus disease 2019 (COVID-19) was at 21.1%. Synoptic data concerning immunosuppressive medication attested to the reduction or withdrawal of antimetabolites (81.9%) and calcineurin inhibitors (48.9%) as a frequent adjustment. In contrast, steroids were reported to be increased in 46.8% of SOT recipients.
Conclusions
COVID-19 in SOT recipients is associated with high morbidity and mortality worldwide. Conforming with current guidelines, modifications of immunosuppressive therapies mostly comprised a reduction or withdrawal of antimetabolites and calcineurin inhibitors, while frequently maintaining or even increasing steroids. Here, we provide an accessible overview to the topic and synoptic estimates of expectable outcomes regarding in-hospital mortality of SOT recipients with COVID-19.
Since the World Health Organization declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak starting in 2019 a pandemic, many countries have been severely affected by continuously rising infection rates. This unprecedented situation has challenged health systems on a global scale, straining patient treatment inter alia because of an altered risk assessment for a variety of patient cohorts. Based on rapidly emerging data, factors such as age, diabetes mellitus, chronic lung disease, and hypertension have been identified to increase disease-related mortality [1]. This is why close attention has been paid to vulnerable patient populations. For instance, in patients undergoing surgery, an international cohort study has established an excessive mortality risk when patients became infected with SARS-CoV-2 directly before or during the first month after surgery [2]. Although this risk profile is most probably modulated by a variety of factors, the scale of these effects is unparalleled and calls for cautionary and preventative measures in regions affected by SARS-CoV-2 propagation.
Against this background, patients who received a solid organ transplant (SOT) have been identified as another high-risk group. An analysis of more than 17 million electronic health care records from the United Kingdom, including >10,000 deaths related to coronavirus disease 2019 (COVID-19), suggests a 6-fold increased sex- and age-adjusted risk of death (95% confidence interval, 4.73-7.61) in SOT recipients [3]. This relates both to patients who recently underwent transplantation and long-term SOT recipients. In addition to immunosuppression, transplant recipients frequently have additional risk factors that may favor detrimental outcomes. Meanwhile, an array of case reports, case series as well as case-control studies has been published, predominantly confirming an increased mortality risk for SOT recipients when infected with SARS-CoV-2 and developing COVID-19.
Multiple systematic reviews on the topic have become available throughout 2020, with steadily increasing case numbers. However, the massive increment of publications on SARS-CoV-2 has resulted in an unprecedented complexity of the field, which is overwhelming even for the expert reader [4]. This situation has also fostered a surge of non-peer–reviewed research published as preprints [5]. Although the rapid distribution of latest research findings represents a valuable tool to combat the pandemic, it is also linked to inherent limitations. Furthermore, pandemic pressure and the urge to catch up with the flood of information and findings already supplied by news and social media as well as in preprints has resulted in more rapid review by many scientific journals and the publication of preliminary reports. Taken together, revisiting available empirical data systematically seems highly relevant. Here, comprehensive synoptic analyses are a gateway to access the available literature, for example, allowing a broad-ranging overview and risk assessment for SARS-CoV-2–infected SOT recipients, which may help with addressing the many urgent unanswered key questions arising in this context [6]. Thus, we performed a structured literature review, providing an overview that compiles all relevant scientific literature from January 1, 2020 until December 31, 2020, to produce a current synoptic assessment of mortality and clinical outcomes subsequent to infection and COVID-19 in SOT recipients, as well as a comprehensive summary of the relevant scientific literature that even a multitude of preceding systematic reviews falls short to provide so far [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19].
Materials and Methods
We performed a structured review searching for publications reporting on patients after SOT with confirmed SARS-CoV-2 infections and/or COVID-19. The search strategy conformed to applicable guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist [20] is available from the authors of this article on request). A total of 626 articles were identified by searching the electronic database MEDLINE through PubMed (https://pubmed.ncbi.nlm.nih.gov/) and the Cochrane library (https://www.cochranelibrary.com/). Respective search terms and search strings used to query electronic databases is available from the authors of this article on request. This search was complemented by screening reference lists as well as dedicated journals including the American Journal of Transplantation (Online ISSN: 1600-6143), Transplantation (Online ISSN: 1534-6080), and Liver Transplantation (Online ISSN: 1527-6473), identifying 160 additional articles through predefined search terms (including SARS-CoV-2, COVID-19, and transplantation). We searched for all articles published within the period from January 1, 2020, until December 31, 2020.
In addition, because of the high current interest in the topic, we also systematically searched PubMed for previously published systematic reviews relevant to the topic and identified 99 references from 13 systematic reviews (Table 1 ), totaling 728 references after duplicate removal to be screened.
Table 1.
Characteristics of Previously Published Systematic Reviews
| No. | Author | Period Until | Transplanted Organ(s) | Date Published | Included Articles, No. | Patients, No. | Mortality Rate, % |
|---|---|---|---|---|---|---|---|
| 1 | Gavriilidis et al. [9] | April 2020 | Liver | 06/25/2020 | 5 | 12 | 33.3 |
| 2 | Hage et al. [11] | 04/08/2020 | SOT | 05/07/2020 | 5 | 8 | n.d. |
| 3 | Nacif et al. [16] | 04/20/2020 | SOT | 06/03/2020 | 24 | 39 | 25.6 |
| 4 | Imam et al. [12] | 05/06/2020 | Kidney | 07/24/2020 | 21 | 58 | 15.5 |
| 5 | González et al. [10] | 05/15/2020 | Kidney | 06/05/2020 | 34 | 184 | n.d. |
| 6 | Moosavi et al. [15] | 05/22/2020 | SOT | 07/24/2020 | 50 | 337 | 22.8 |
| 7 | Oltean et al. [17] | 06/04/2020 | Kidney | 07/13/2020 | 12 | 204 | 21.2 |
| 8 | Aziz et al. [7] | 06/06/2020 | SOT | 09/15/2020 | 49 | 403 | 21 |
| 9 | Fraser et al. [8] | 06/15/2020 | Liver | 07/30/2020 | 15 | 223 | 19.3 |
| 10 | Marinaki et al. [14] | 07/07/2020 | Kidney | 09/16/2020 | 63 | 420 | 22.1 |
| 11 | Mahaling-asivam et al. [13] | 08/04/2020 | Kidney | 11/03/2020 | 20 | 1955 | n.d. |
| 12 | Raja et al. [19] | 10/09/2020 | SOT | 11/14/2020 | 60 | 2772 | 18.6 |
| 13 | Phanish et al. [18] | 10/15/2020 | Kidney | 12/19/2020 | 16 | 1494 | 24 |
n.d., no data; SOT, solid organ transplant.
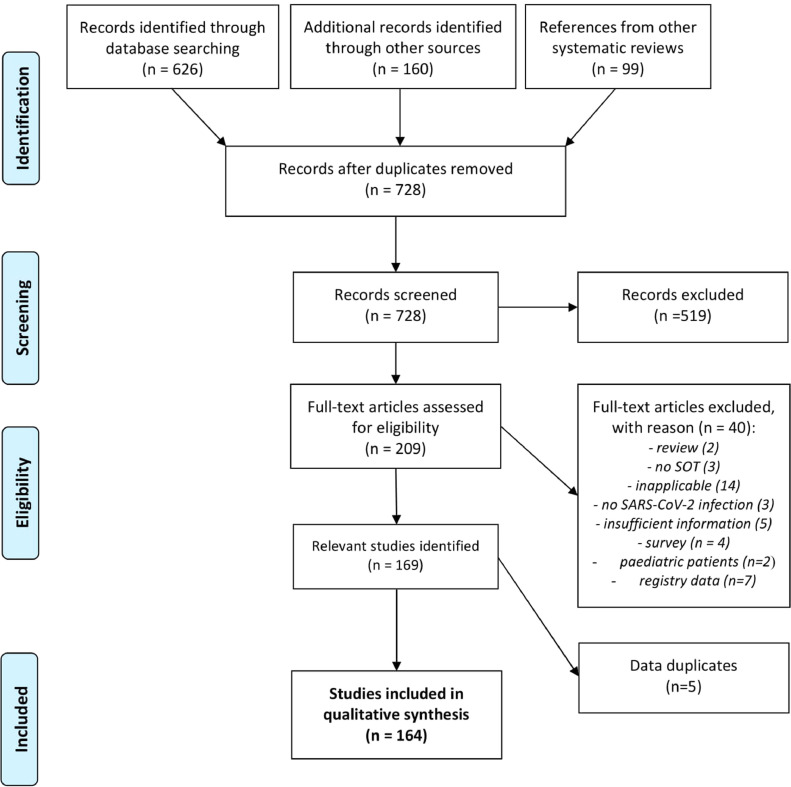
In a first screening step, 519 of these publications were excluded and the 209 remaining articles were individually assessed and screened in detail for the relevant minimum required information defined by us. Characteristics searched for were SOT recipients 10 years or older with confirmed SARS-CoV-2 infection and/ or COVID-19. Additional essential information required before article inclusion were the number of SARS-CoV-2/COVID-19–positive SOT recipients, transplanted organs, and clinical outcomes. Review articles, unassignable registry data, surveys and non–English-language articles were excluded. After excluding 40 full-text-publications with reasons, 169 suitable articles were identified and 164 were included in the review (Fig 1 ). Five articles were removed because they are potentially reporting on the same set of patients.
Fig 1.
Flow diagram outlining the literature search strategy and selection of articles. The diagram depicts the different stages of our structured review including identification, screening, and selection of suitable articles. Articles were identified through searching MEDLINE, PubMed, and Cochrane databases, as well as additional sources for articles reporting on SOT recipients with SARS-CoV-2 infection or COVID-19. The used search strategy conforms to PRISMA guidelines [6]. Precise search terms and a PRISMA checklist as well as extracted data are available from the authors of this article on request. COVID-19, coronavirus disease 2019; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SOT, solid organ transplant.
Data were compiled and tabulated using Microsoft Excel (Microsoft Corporation, Redmond, Washington, United States); data analysis and visualization were performed by using the free and open-source programming language GNU R [21] with the additional packages easyPubMed [22] as well as ggplot2 [23]. Figures were drawn using Inkscape (https://inkscape.org) and Biorender (https://biorender.com/).
Data were processed to depict the relative number of cases up to each time point, both overall as well as separated by group (type of study as well as geographic area). Data are presented in total numbers and percentages. References to all included articles and extracted data used for evaluations with transparent and reproducible methodology are available from the authors on request.
Results
Included Literature
This structured literature review identified 164 publications overall within our defined scope, which report on 3451 patients in total. The literature search strategy for the selection of scientific articles is illustrated in Fig 1. Most included studies were case reports (n = 89) [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], followed by cohort studies (n = 38) [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], case series (n = 26) [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], multicenter cohort studies or case series (n = 8) [177], [178], [179], [180], [181], [182], [183], [184], and 3 case-control studies [185], [186], [187]. An overview on the largest patient cohorts is provided in Table 2 .
Table 2.
Overview of Cohort Studies and Largest Published Data Sets on Kidney, Liver, Heart, and Lung Transplant Recipients Infected With SARS-CoV-2
| Author | Study Design | Origin | Patients, No. | Transplanted Organ(s) | Mortality Rate, % |
|---|---|---|---|---|---|
| Coll et al. [177] | Multicenter cohort study | Europe | 665 | Kidney/liver/heart/lung/other | 23.5 |
| Kute et al. [179] | Multicenter cohort study | Asia | 250 | Kidney | 11.6 |
| Azzi et al. [118] | Cohort study | North America | 229 | Kidney | 20.5 |
| Webb et al. [184] | Multicenter cohort study | Other | 151 | Liver | 18.5 |
| Cravedi et al. [127] | Cohort study | North America | 144 | Kidney | 31.9 |
| Favà et al. [131] | Cohort study | Europe | 104 | Kidney | 26.9 |
| Molnar et al. [180] | Cohort study | North America | 98 | Kidney/liver/heart/lung/other | 39.8 |
| Ozturk et al. [181] | Multicenter cohort study | Asia | 81 | Kidney | 11.1 |
| Craig-Schapiro et al. [126] | Cohort study | North America | 80 | Kidney | 16.3 |
| Ali et al. [117] | Cohort study | Asia | 67 | Kidney/liver/lung | 3.0 |
SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Patient Demographics
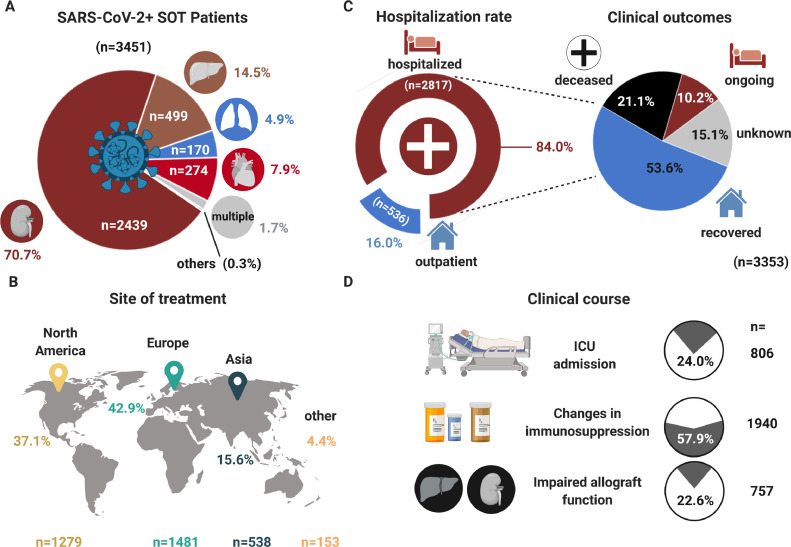
Most included patients had received a kidney allograft (n = 2439; 70.7%), followed by liver (n = 499; 14.5%), heart (n = 274; 7.9%), and lung (n = 170; 4.9%) transplants. Only a minor fraction had multiple organ (n = 59; 1.7%) transplants (Fig 2 A). An analysis of the global distribution revealed that the largest proportion of included patients were treated either in Europe (n = 1481; 42.9%) or North America (n = 1279; 37.1%), whereas a smaller number of patients was reported from countries located in Asia (538; 15.6%). Additionally, 153 patients (4.4%) were reported from other countries/regions or could not be allocated. Overall, only 2 patients were reported from South American countries (Fig 2B).
Fig 2.
Synthesis of structured review results assessing SARS-CoV-2 infections in solid organ transplant recipients. Our structured review comprises 3451 cases of SOT recipients with confirmed SARS-CoV-2 infection (SARS-CoV-2+) and/or COVID-19 presented as a synopsis (respective source data are available from the authors). (A) The pie chart depicts % fractions of infected SOT recipients (subdivided into liver, lung, heart, and multiple organs). (B) Assigns numbers and % fractions of infected SOT recipients according to the local origin of the reports/their site of treatment. (C) Presents respective SOT recipients according to treatment, categorized either as hospitalized or as outpatient, as well as outcomes at the time of reporting, categorized into deceased/recovered and ongoing treatment. (D) Clinical outcomes of SOT recipients are presented as % fractions and numbers of patients among all cases requiring ICU admission, changes in immunosuppression, and patients experiencing an impaired transplant function linked to infection. COVID-19, coronavirus disease 2019; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SOT, solid organ transplant.
Clinical Course and Outcome
Among 3451 patients reported with confirmed SARS-CoV-2 infection and/or COVID-19, data on the clinical course and outcome were available for 3353 patients (97.2%). According to this, 84% required hospitalization, whereas the remaining 536 patients were treated in an outpatient setting. For one study, respective data were unavailable [156] and hospitalization was assumed as the default option. Among all included 2817 hospitalized patients, 53.6% recovered from SARS-CoV-2 infection or could be discharged. Altogether 21.1% (n = 709) of patients were deceased at the time of data reporting and 10.2% of the patients remained affected by the disease, whereas 15.1% remained with an unknown outcome (Fig 2C). For 57.9% of the patients, changes in immunosuppressive medication were reported, and for at least 22.6% of SOT recipients disease progression involved an impaired allograft function (Fig 2D).
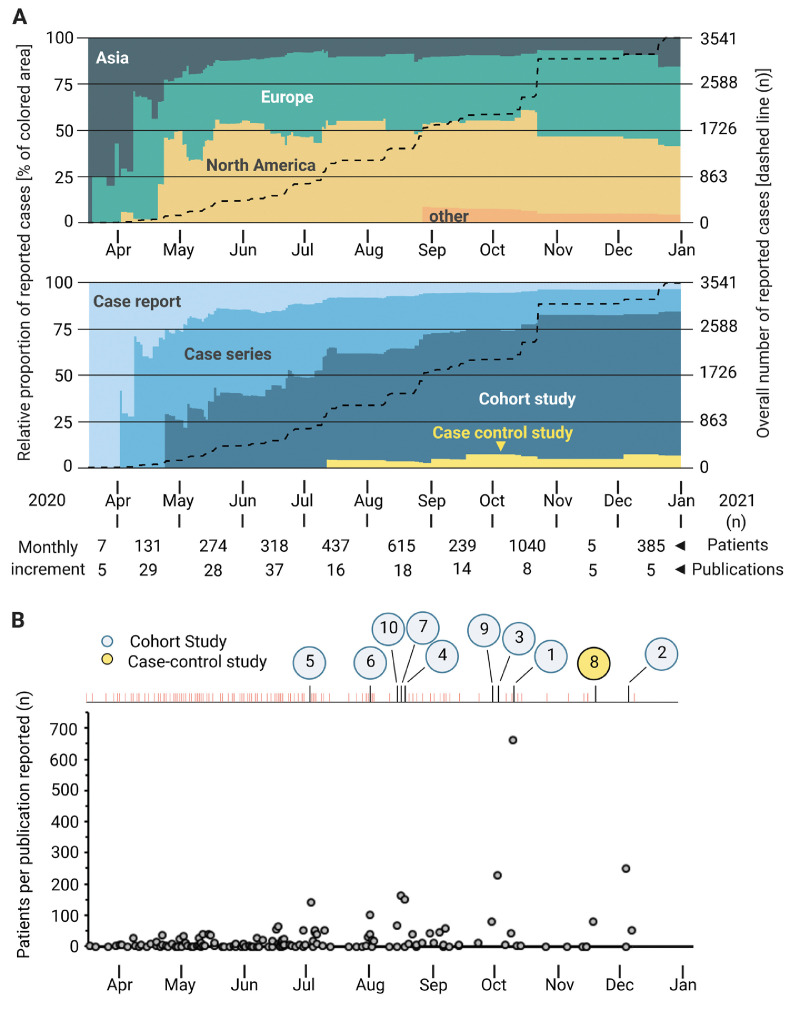
Development of Publications on COVID-19 and Transplantation Over Time
We further analyzed the types of publications and the geographical origin of the included studies throughout the year 2020, thereby revealing clear longitudinal trends for both origin and publication type. Starting with the SARS-CoV-2 outbreak, first reports on disease outcomes in SOT recipients became available from Asia. In spring 2020, when Europe was severely hit by a first SARS-CoV-2 wave, this resulted in increasing publication numbers reporting on SOT recipients. By mid-April 2020, also sizeable numbers of publications on SARS-CoV-2 and SOT recipients from North America were published. Relevant publications from other continents were only published late in 2020 and remained scarce compared with the publication output from Asia, Europe, and North America (Fig 3 A).
Fig 3.
Comparison of publications on COVID-19 and transplantation over time. (A) The diagram illustrates the course of scientific information about COVID-19 made available (dates of first publication). A distinction is made between the origin of the studies (graph above) the types of publication (graph below). The dashed line represents overall numbers of patients; the colored area represents the relative number of patients reported until that time. (B) The graph depicts the number of patients per publication reported over time. The numbers from 1 to 10 illustrate the 10 studies with the largest patient collective, as presented in Table 2. COVID-19, coronavirus disease 2019.
Similar longitudinal trends can also be shown when analyzing the type of data published. Although early in the pandemic data on SARS-CoV-2 in SOT recipients were derived mainly from case reports, this was later followed by case series, with steadily increasing patient numbers reported in each publication and then succeeded by publications of cohort studies starting in late April 2020. Ultimately, also case-control studies became available but only in the second half of the year. However, their number remained small, thus accounting only for a minor proportion of patients reported (Fig 3A, B).
Management of Immunosuppressive Therapy
Among a subgroup of 1192 transplant recipients from 5 large cohorts [119,132,164,177,179], we analyzed the available data on modification and management of the immunosuppressive therapies. Accordingly, the most frequent measure mentioned was the reduction or withdrawal of antimetabolites in 81.9% of SOT recipients with SARS-CoV-2 infection initially receiving this treatment. Reduction or withdrawal of calcineurin inhibitors was also reported frequently (48.9%). In contrast, steroids have been increased in 46.8% of respective patients, while reporting a reduction or withdrawal remained an exception (1.3%) (Table 3 ).
Table 3.
Adjustments of Immunosuppressive Drug Regimen in Selected Cohort Studies/Case Series of Transplant Recipients Infected With SARS-CoV-2
| Antimetabolites, n/N (%)* |
Calcineurin Inhibitors, n/N (%)† |
Steroids, n/N (%)‡ |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Transplanted Organ(s) | Study Cohort, No. | ↔ | X | ↓ | ↑ | ↔ | X | ↓ | ↑ | ↔ | X | ↓ | ↑ |
| Coll et al. [177] | Kidney, HSCT, liver, lung, pancreas, multivisceral | 778 | 92/389 (23.7) | 273/389 (70.2) | 24/389 (6.2) | 0 | 175/495 (35.4) | 181/495 (36.6) | 134/495 (27.1) | 5/495 (1) | 197/460 (42.8) | 8/460 (1.7) | 2/460 (0.4) | 253/460 (55) |
| Kute et al. [179] | Kidney | 250 | 0 | 188/250 (75.2) | 62/250 (24.8) | 0 | 165/236 (69.9) | 21/236 (8.9) | 50/236 (21.2) | 0 | 150/250 (60) | 0 | 0 | 100/250 (40) |
| Bechetti et al. [119] | Liver | 57 | 15/26 (57.7) | 10/26 (38.5) | 1/26 (3.8) | 0 | 31/50 (62) | 7/50 (14) | 12/50 (24) | 0 | 10/10 (100) | 0 | 0 | 0 |
| Lubetzky et al. [164] | Kidney | 54 | 13/52‡ (25) | 24/52 (46.2) | 15/52 (28.8) | 0 | 35/52 (67.3) | 0 | 17/52 (32.7) | 0 | 22/27 (81.5) | 0 | 0 | 5/27 (18.5) |
| Felldin et al. [132] | Kidney, liver, heart, lung, liver-kidney, kidney-heart | 53 | 17/41 (41.5) | 19/41 (46.3) | 5/41 (12.2) | 0 | 42/53 (79.2) | 3/53 (5.7) | 8/53 (15.1) | 0 | 30/40 (75) | 0 | 0 | 10/40 (25) |
| Total | 1192 | 137/758 (18.1) | 514/758 (67.8) | 107/758 (14.1) | 0 | 448/886 (50.6) | 212/886 (23.9) | 221/886 (24.9) | 5/886 (0.6) | 409/787 (52) | 8/787 (1) | 2/787 (0.3) | 368/787 (46.8) | |
↔, no (substantial) change; ↓, dose reduction; ↑, dose increase; HSCT, hematopoietic stem cell transplant; n, quantity; N, patient population among study cohort that initially received the respective treatment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; X, withdrawal.
Azathioprine and/or mycophenolate mofetil.
Cyclosporine and/or tacrolimus.
No reduction/≤50% reduction.
To obtain a more conclusive picture, we additionally screened the most recent recommendations from national and international transplantation societies regarding the immunosuppressive management of SOT recipients with SARS-CoV-2 infection. We identified 6 clinical guidelines generally based on expert opinion and summarized their recommendations (Table 4 ) [188], [189], [190], [191], [192], [193]. A broad consensus prevails, suggesting a critical consideration of the overall level of immunosuppression in SARS-CoV-2–infected SOT recipients based on established principles for managing infections in those patients. In patients with low risk of allograft rejection, decreasing immunosuppressive medication should be considered, especially in patients with severe COVID-19 disease. Here, guidelines consistently recommend withdrawal or reduction of antimetabolites as a first step, followed by reduction of calcineurin inhibitors. Although no guideline recommends the reduction of steroids, some do recommend the administration of dexamethasone (6 mg daily) for up to 10 days in patients who require oxygen supplementation or are mechanically ventilated.
Table 4.
Recommendations From National and International Transplantation Societies
| Society/Reference | Origin | Date | Guideline | Recommendation |
|---|---|---|---|---|
| British Transplantation Society [188] | UK | January 2021 | Guidance on the management of transplant recipients diagnosed as having or suspected of having COVID-19 | Outpatients: - Stop antiproliferative agents (MMF/azathioprine) - Review total burden of immunosuppression and consider reduction of CNIs - High or increased dose steroid is NOT recommended at this stage Hospitalized patients: - Stop antiproliferative agents (MMF/azathioprine) Consider reducing or stopping CNIs - Dexamethasone 6 mg daily for 10 d Patients requiring ventilatory support: - Stop antiproliferative agents (MMF/azathioprine) - Dramatically reduce or stop CNIs - Consider dexamethasone, as above |
| International Society of Heart and Lung Transplantation [189] | International | February 2021 | Guidance from the International Society of Heart and Lung Transplantation regarding the SARS-CoV-2 pandemic | - For transplant recipients, consider holding MMF, mTOR inhibitors, or azathioprine while admitted with moderate/severe illness. |
| Transplantation Society [190] | International | March 2021 | Guidance on Coronavirus Disease 2019 (COVID-19 for Transplant Clinicians | - Dexamethasone 6 mg daily for up to 10 d can be considered in patients who require supplemental oxygen or are mechanically ventilated. - Attention should be paid to the potential drug interactions with current immunosuppression and the potential for increased risk of infectious complications when immunomodulatory agents are added to existing immunosuppressive therapy. |
| American Association for the Study of Liver Diseases [191] | US | March 2021 | Clinical Best Practice Advice for Hepatology and Liver transplant Providers During the COVID-19 Pandemic: AASLD Expert Panel Consensus Statement | - Consider lowering the overall level of immunosuppression, particularly antimetabolite dosages (eg, azathioprine or MMF) based on general principles for managing infections in transplant recipients and to decrease the risk of superinfection. - Monitor kidney function and CNI levels. - Adjust immunosuppressive medications based on severity of COVID-19 and risk of graft rejection and renal injury. |
| Canadian Society of Transplantation [192] | Canada | April 2021 | Consensus guidance and recommendations for organ donation and transplantation services during COVID-19 pandemic | - Based on current evidence, we suggest a temporary adjustment of maintenance immune suppression for hospitalized patients with severe COVID-19. - Data on optimal immune-suppression adjustment in patients with COVID-19 are lacking, may vary, and may not be required depending on disease severity and physician judgment. |
| American Society of Transplantation [193] | US | June 2021 | 2019-nCoV (Coronavirus): FAQs for Organ Transplantation | - The impact of immunosuppression on COVID-19 is not currently known but decreasing immunosuppression may be considered for infected recipients who have not had recent rejection episodes. - Many providers have decreased or discontinued cell cycle inhibitors or reduced CNI levels, but comparative data regarding these interventions are not yet available. - Whether adjunctive corticosteroid therapy for patients with severe ARDS may be beneficial is also unknown. |
AASLD, American Association for the Study of Liver Diseases; ARDS, acute respiratory distress syndrome; CNI, calcineurin inhibitor; COVID-19, coronavirus disease 2019; FAQs, frequently asked questions; MMF, mycophenolate mofetil; mTOR, mammalian target of rapamycin; UK, United Kingdom; US, United States of America; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Discussion
Based on data from other patient cohorts, it was reasonable to assume early on in the pandemic that SOT recipients do also exhibit a high-risk profile after infection with SARS-CoV-2 because of indispensable immunosuppressive medication and a high rate of additional medical risk factors. Data from first small cohort studies that had become available in kidney transplant recipients confirmed this notion, with reported mortality rates of up to 30% [168]. A case-control study with a more robust study design conducted in 151 liver transplant recipients and 627 hospitalized control patients who were not transplant recipients surprisingly concluded that SOT status by itself was not independently associated with higher mortality. Instead, multivariate analysis established that mortality was primarily associated with age and disease severity [184]. These two examples may demonstrate the broad range of published information on SARS-CoV-2 in SOT recipients, while at the same time calling for careful synoptic assessment of the available literature to support a better understanding of the overall risk involved for SARS-CoV-2–infected SOT recipients.
Here, our comprehensive evaluations confirm that during the course of 2020 better studies with a more robust scientific design have increasingly become available. However, the SARS-CoV-2 pandemic has also fundamentally impacted research publishing, as reflected by increasing submission numbers, preprint rush, expedited review, and in some cases retractions, even in high-profile peer-reviewed journals [5]. Therefore, our work may provide a robust overview and facilitate orientation within the tsunami of information linked to COVID-19.
Our synoptic review incorporates 3451 cases of SOT recipients with confirmed SARS-CoV-2 infection and/or COVID-19, predominantly from the Unites States and Europe, and therefore sheds additional light on key issues in SOT recipients exposed to SARS-CoV-2, facilitating an easy overview. In contrast, the largest patient cohort previously reported on in a systematic review were considerably smaller with 2772 SOT recipients [19] and 1955 and 223 for kidney [13] and liver [8] transplant recipients, respectively. About 70.7% of patients included by us were kidney transplant recipients, which is relevant since chronic kidney disease has been implicated in COVID-19–related mortality [194]. The overall mortality in our data set was 21.1%, which is well in line with previous work [7,8,14,15,17]. Compared with the status quo before the pandemic, these data are alarming, even when assuming the very low end of estimates concerning the COVID-19–related case fatality rate reported at only 8.1% and 4.6% in men and women, respectively [195]. However, a large observational study in more than 10,000 hospitalized patients in Germany found in-hospital mortality rates at 22% among the general population [196], which is in line with our review findings among SOT recipients.
Our compiled data suggest that SARS-CoV-2 infection and COVID-19 resulted in a hospitalization rate of 84% with 24% of patients requiring intensive care unit admission. We may speculate that the hospitalization rate derived from respective articles published in 2020 is most likely an overestimation resulting from reporting bias, which is inherent to this kind of evaluation. Nonetheless, our findings tend to concur with previous reports, for example, in 36 infected adult kidney transplant recipients from the United States, where the hospitalization rate was 78%, and 39% of patients required mechanical ventilation, with a resulting mortality rate of 28% [114]. Then again, a single-center report from Italy, which had been severely impacted early on in the pandemic, has reported unanimous hospitalization (100%), frequent occurrence of acute respiratory distress syndrome (55%), and 25% mortality among 20 SARS-CoV-2–infected renal allograft recipients [152], suggesting the local situation may likely have impacted reporting.
The management of immunosuppressive therapies in COVID-19–positive SOT recipients is crucial but has not been conclusively addressed until now. Here, balancing the risks of allograft rejection and viral infection is paramount for the affected patients, yet the available data are scarce and scattered so far. Therefore, current guidelines from transplantation societies are mainly based on expert opinion, consistently recommending the withdrawal or reduction of antimetabolites followed by a reduction in calcineurin inhibitor dosage, depending on disease severity. Those recommendations are in line with the summary results of our literature overview, considering available retrospective clinical evidence.
Along the same lines, tacrolimus could be linked with a positive independent effect on survival in liver transplant recipients [197], whereas baseline immunosuppression containing mycophenolate mofetil was an independent predictor of severe COVID-19 [198].
Some guidelines even recommend dexamethasone administration for up to 10 days in patients who require supplemental oxygen or are mechanically ventilated, thus conforming with the Randomised Evaluation of COVID-19 Therapy Trial (RECOVERY) results [199] and treatment guidelines for the general population. The only review of guidelines addressing the use of immunosuppressants during the coronavirus pandemic for diverse indications also concluded that steroid use should not be stopped and emphasized the role of an individualized risk-benefit assessment, weighing the risk of COVID-19 infection and drug-induced immunosuppression for each patient [200].
Another critical aspect in COVID-19–diseased SOT recipients is the preservation of transplant function. Graft impairment or failure has been reported for about 22.6% of the cases we have compiled. Such complications were frequently reported for kidney and liver transplant recipients. Corresponding data for acute kidney injury have been reported to range between 25% and 57% in COVID-19–diseased kidney transplant recipients [41,65,152,154,185], linking it with a particularly poor prognosis [201].
We believe that the presented overview should be fairly comprehensive because of the amount of data compiled, while at the same time providing a representative number regarding clinical outcomes and in-hospital mortality rates that may be expectable in COVID-19–diseased SOT patients. Our data are unfortunately not suitable for a general assessment because of inherent study limitations. Here, especially asymptomatic SARS-CoV-2–infected SOT recipients may not be reflected by our evaluations, and any deductive conclusions should therefore be avoided.
As a potential limitation of our aggregate findings, a relevant selection bias is probable because of the design of our work. In detail, we assume, for example, mortality rates may be overestimated and most probably apply only to the in-hospital setting. Another limitation is that follow-up duration was inhomogeneous and ranged widely, with many included cases having ongoing disease at time of reporting or unknown outcomes, which may render results premature. Nevertheless, most patients had a sufficiently long follow-up period in our view, considering mortality in infected SOT recipients is mainly observed within the first 15 days after hospitalization [185]. We intentionally refrained from any meta-analyses of data or reporting estimates of uncertainty, which was deliberately not within the scope of our work. We believe that preceding publications have proven this attempt to be most likely futile, while at the same time lacking significant added value [19]. Hence, the aggregated data presented here come with limitations that are defined by the nature of the available data and should therefore be considered as rough ballpark estimates rather than detailed outcomes.
Conclusions
In conclusion, we provide a topical, comprehensive overview of the literature on SARS-CoV-2 and/or COVID-19 comprising more than 3400 SOT recipients, aggregating their clinical outcomes, setting the available findings into a larger context, and providing entry points to a vast body of results published over one year.
Therefore, this overview adds substantially to the hitherto available studies and comparable previous work. Because the data support the notion that clinical outcomes after SARS-CoV-2 infections in SOT recipients are poor, maintaining adequate precautionary measures seems reasonable.
References
- 1.Lu L, Zhong W, Bian Z, Li Z, Zhang K, Liang B, et al. A comparison of mortality-related risk factors of COVID-19, SARS, and MERS: a systematic review and meta-analysis. J Infect. 2020;81:e18–e25. doi: 10.1016/j.jinf.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Q, Allot A, Lu Z. Keep up with the latest coronavirus research. Nature. 2020;579:193. doi: 10.1038/d41586-020-00694-1. [DOI] [PubMed] [Google Scholar]
- 5.Else H. How a torrent of COVID science changed research publishing - in seven charts. Nature. 2020;588:553. doi: 10.1038/d41586-020-03564-y. [DOI] [PubMed] [Google Scholar]
- 6.Ritschl PV, Nevermann N, Wiering L, Wu HH, Moroder P, Brandl A, et al. Solid organ transplantation programs facing lack of empiric evidence in the COVID-19 pandemic: a by-proxy society recommendation consensus approach. Am J Transplant. 2020;20:1826–1836. doi: 10.1111/ajt.15933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aziz H, Lashkari N, Yoon YC, Kim J, Sher LS, Genyk Y, et al. Effects of coronavirus disease 2019 on solid organ transplantation. Transplant Proc. 2020;52:2642–2653. doi: 10.1016/j.transproceed.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fraser J, Mousley J, Testro A, Smibert OC, Koshy AN. Clinical presentation, treatment, and mortality rate in liver transplant recipients with coronavirus disease 2019: a systematic review and quantitative analysis. Transplant Proc. 2020;52:2676–2683. doi: 10.1016/j.transproceed.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gavriilidis P, Pai M. The impact of COVID-19 global pandemic on morbidity and mortality of liver transplant recipients children and adults: a systematic review of case series. J Clin Med Res. 2020;12:404–408. doi: 10.14740/jocmr4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez J, Ciancio G. Early experience with COVID-19 in kidney transplantation recipients: update and review. Int Braz J Urol. 2020;46:145–155. doi: 10.1590/S1677-5538.IBJU.2020.S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hage R, Steinack C, Benden C, Schuurmans MM. COVID-19 in patients with solid organ transplantation: a systematic review. Transplantology. 2020;1:1–15. [Google Scholar]
- 12.Imam A, Abukhalaf SA, Imam R, Abu-Gazala S, Merhav H, Khalaileh A. Kidney transplantation in the times of COVID-19 - a literature review. Ann Transplant. 2020;25 doi: 10.12659/AOT.925755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahalingasivam V, Craik A, Tomlinson LA, Ge L, Hou L, Wang Q, et al. A systematic review of COVID-19 and kidney transplantation. Kidney Int Rep. 2021;6:24–45. doi: 10.1016/j.ekir.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marinaki S, Tsiakas S, Korogiannou M, Grigorakos K, Papalois V, Boletis I. A systematic review of COVID-19 infection in kidney transplant recipients: a universal effort to preserve patients’ lives and allografts. J Clin Med. 2020;9:2986. doi: 10.3390/jcm9092986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moosavi SA, Mashhadiagha A, Motazedian N, Hashemazar A, Hoveidaei AH, Bolignano D. COVID-19 clinical manifestations and treatment strategies among solid-organ recipients: a systematic review of cases. Transpl Infect Dis. 2020;22:e13427. doi: 10.1111/tid.13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nacif LS, Zanini LY, Waisberg DR, Pinheiro RS, Galvao F, Andraus W, et al. COVID-19 in solid organ transplantation patients: a systematic review. Clinics (Sao Paulo) 2020;75:e1983. doi: 10.6061/clinics/2020/e1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oltean M, Softeland JM, Bagge J, Ekelund J, Felldin M, Schult A, et al. COVID-19 in kidney transplant recipients: a systematic review of the case series available three months into the pandemic. Infect Dis (Lond) 2020;52:830–837. doi: 10.1080/23744235.2020.1792977. [DOI] [PubMed] [Google Scholar]
- 18.Phanish M, Ster IC, Ghazanfar A, Cole N, Quan V, Hull R, et al. Systematic review and meta-analysis of COVID-19 and kidney transplant recipients, the South West London Kidney Transplant Network experience. Kidney Int Rep. 2021;6:574–585. doi: 10.1016/j.ekir.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raja MA, Mendoza MA, Villavicencio A, Anjan S, Reynolds JM, Kittipibul V, et al. COVID-19 in solid organ transplant recipients: a systematic review and meta-analysis of current literature. Transplant Rev (Orlando) 2021;35 doi: 10.1016/j.trre.2020.100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 21.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2018. R: a language and environment for statistical computing. [Google Scholar]
- 22.Fantini D. EasyPubMed: search and retrieve scientific publication records from PubMed. 2019.
- 23.Wickham H. Springer-Verlag; New York, NY: 2016. ggplot2: elegant graphics for data analysis. [Google Scholar]
- 24.Abuzeineh M, Desai N, Brennan DC, Alasfar S. COVID-19 early after a deceased donor kidney transplant surgery. Transplantation. 2020;104 doi: 10.1097/TP.0000000000003439. e354-5. [DOI] [PubMed] [Google Scholar]
- 25.Abuzeineh M, Muzaale AD, Crews DC, Avery RK, Brotman DJ, Brennan DC, et al. Telemedicine in the care of kidney transplant recipients with coronavirus disease 2019: case reports. Transplant Proc. 2020;52:2620–2625. doi: 10.1016/j.transproceed.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adapa S, Konala VM, Naramala S, Daggubati SR, Koduri NM, Gayam V, et al. COVID-19 in renal transplant patient presenting with active typical symptoms and resolved atypical symptoms. J Investig Med High Impact Case Rep. 2020;8 doi: 10.1177/2324709620949307. 2324709620949307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adrogue AH, Mithani F, Ibrahim HN, Schwartz MR, Gaber L, Hebert SA, et al. A kidney transplant recipient with coronavirus disease 2019: utility of a prognostication score. Transplant Proc. 2020;52:2688–2692. doi: 10.1016/j.transproceed.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmad SH, Smith R, Camilleri B. Belatacept, kidney transplantation and COVID-19: successful management of the first reported case within the United Kingdom. Clin Transplant. 2020;34:e14026. doi: 10.1111/ctr.14026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aigner C, Dittmer U, Kamler M, Collaud S, Taube C. COVID-19 in a lung transplant recipient. J Heart Lung Transplant. 2020;39:610–611. doi: 10.1016/j.healun.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allam SR, Dao A, Madhrira MM, Antiporta PB, Nair RR, Guiteau JJ, et al. Interleukin-6 receptor antagonist therapy to treat SARS-CoV-2 driven inflammatory syndrome in a kidney transplant recipient. Transpl Infect Dis. 2020;22:e13326. doi: 10.1111/tid.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Antony SJ, Singh J, de Jesus M, Lance J. Early use of tocilizumab in respiratory failure associated with acute COVID-19 pneumonia in recipients with solid organ transplantation. IDCases. 2020;21:e00888. doi: 10.1016/j.idcr.2020.e00888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arpali E, Akyollu B, Yelken B, Tekin S, Turkmen A, Kocak B. Case report: a kidney transplant patient with mild COVID-19. Transpl Infect Dis. 2020;22:e13296. doi: 10.1111/tid.13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Athanazio RA, Costa AN, Carraro RM, Gonzalez D, Rached SZ, Samano MN, et al. Early COVID-19 infection after lung transplantation in a patient with cystic fibrosis. Clinics (Sao Paulo) 2020;75:e2274. doi: 10.6061/clinics/2020/e2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bartiromo M, Borchi B, Botta A, Bagala A, Lugli G, Tilli M, et al. Threatening drug-drug interaction in a kidney transplant patient with coronavirus disease 2019 (COVID-19) Transpl Infect Dis. 2020;22:e13286. doi: 10.1111/tid.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Billah M, Santeusanio A, Delaney V, Cravedi P, Farouk SS. A catabolic state in a kidney transplant recipient with COVID-19. Transpl Int. 2020;33:1140–1141. doi: 10.1111/tri.13635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bussalino E, De Maria A, Russo R, Paoletti E. Immunosuppressive therapy maintenance in a kidney transplant recipient with SARS-CoV-2 pneumonia: a case report. Am J Transplant. 2020;20:1922–1924. doi: 10.1111/ajt.15920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen D, Yang B, Zhang Y, Chen L, Wei L, Zhang W, et al. Withdrawing mycophenolate mofetil in treating a young kidney transplant recipient with COVID-19: a case report. Medicine (Baltimore) 2020;99:e20481. doi: 10.1097/MD.0000000000020481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen S, Yin Q, Shi H, Du D, Chang S, Ni L, et al. A familial cluster, including a kidney transplant recipient, of coronavirus disease 2019 (COVID-19) in Wuhan, China. Am J Transplant. 2020;20:1869–1874. doi: 10.1111/ajt.15903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheng D, Wen J, Liu Z, Lv T, Chen JS. Coronavirus disease 2019 in renal transplant recipients: report of two cases. Transpl Infect Dis. 2020;22:e13329. doi: 10.1111/tid.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chenna A, Konala VM, Gayam V, Naramala S, Adapa S. Coronavirus disease 2019 (COVID-19) in a renal transplant patient. Cureus. 2020;12:e8038. doi: 10.7759/cureus.8038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Columbia University Kidney Transplant Program Early description of coronavirus 2019 disease in kidney transplant recipients in New York. J Am Soc Nephrol. 2020;31:1150–1156. doi: 10.1681/ASN.2020030375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cozzi E, Faccioli E, Marinello S, Loy M, Congedi S, Calabrese F, et al. COVID-19 pneumonia in lung transplant recipients: report of 2 cases. Am J Transplant. 2020;20:2933–2937. doi: 10.1111/ajt.15993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dahl Mathiasen V, Jensen-Fangel S, Skov K, Leth S. Uneventful case of COVID-19 in a kidney transplant recipient. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Gottardi A, Fratila C, Bertoli R, Cerny A, Magenta L, Gianella P, et al. Clinical characteristics and management of a liver transplanted patient admitted with SARS-CoV-2 infection. Clin Res Hepatol Gastroenterol. 2020;44:e141–e144. doi: 10.1016/j.clinre.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Souza L, Nwanji V, Kaur G. An auspicious triumph of recovery from dialysis-requiring acute kidney injury in COVID-19 in a patient with chronic kidney disease, alpha-1 antitrypsin deficiency, and liver transplant: a case report. Clin Nephrol. 2020;94:297–306. doi: 10.5414/CN110294. [DOI] [PubMed] [Google Scholar]
- 46.Decker A, Welzel M, Laubner K, Grundmann S, Kochs G, Panning M, et al. Prolonged SARS-CoV-2 shedding and mild course of COVID-19 in a patient after recent heart transplantation. Am J Transplant. 2020;20:3239–3245. doi: 10.1111/ajt.16133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dirim AB, Demir E, Ucar AR, Garayeva N, Safak S, Oto OA, et al. Fatal SARS-CoV-2 infection in a renal transplant recipient. CEN Case Rep. 2020;9:409–412. doi: 10.1007/s13730-020-00496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farfour E, Picard C, Beaumont L, Lesprit P, Ballester MC, Ackermann F, et al. SARS-CoV-2 Foch Hospital study, COVID-19 in lung-transplanted and cystic fibrosis patients: be careful. J Cyst Fibros. 2020;19:e16–e17. doi: 10.1016/j.jcf.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fontana F, Alfano G, Mori G, Amurri A, Tei L, Ballestri M, et al. COVID-19 pneumonia in a kidney transplant recipient successfully treated with tocilizumab and hydroxychloroquine. Am J Transplant. 2020;20:1902–1906. doi: 10.1111/ajt.15935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141:1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gandolfini I, Delsante M, Fiaccadori E, Zaza G, Manenti L, Degli Antoni A, et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20:1941–1943. doi: 10.1111/ajt.15891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gao F, Zheng KI, Gu JY, George J, Zheng MH. COVID-19 and liver transplantation: lessons learned from three reported cases. Transpl Infect Dis. 2020;22:e13335. doi: 10.1111/tid.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gautier-Vargas G, Baldacini C, Benotmane I, Keller N, Perrin P, Moulin B, et al. Rapid resolution of cytokine release syndrome and favorable clinical course of severe COVID-19 in a kidney transplant recipient treated with tocilizumab. Kidney Int. 2020;98:508–509. doi: 10.1016/j.kint.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guillen E, Pineiro GJ, Revuelta I, Rodriguez D, Bodro M, Moreno A, et al. Case report of COVID-19 in a kidney transplant recipient: does immunosuppression alter the clinical presentation? Am J Transplant. 2020;20:1875–1878. doi: 10.1111/ajt.15874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hammami MB, Garibaldi B, Shah P, Liu G, Jain T, Chen PH, et al. Clinical course of COVID-19 in a liver transplant recipient on hemodialysis and response to tocilizumab therapy: a case report. Am J Transplant. 2020;20:2254–2259. doi: 10.1111/ajt.15985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holzhauser L, Lourenco L, Sarswat N, Kim G, Chung B, Nguyen AB. Early experience of COVID-19 in 2 heart transplant recipients: case reports and review of treatment options. Am J Transplant. 2020;20:2916–2922. doi: 10.1111/ajt.15982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hsu JJ, Gaynor P, Kamath M, Fan A, Al-Saffar F, Cruz D, et al. COVID-19 in a high-risk dual heart and kidney transplant recipient. Am J Transplant. 2020;20:1911–1915. doi: 10.1111/ajt.15936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang J, Lin H, Wu Y, Fang Y, Kumar R, Chen G, et al. COVID-19 in posttransplant patients-report of 2 cases. Am J Transplant. 2020;20:1879–1881. doi: 10.1111/ajt.15896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang JF, Zheng KI, George J, Gao HN, Wei RN, Yan HD, et al. Fatal outcome in a liver transplant recipient with COVID-19. Am J Transplant. 2020;20:1907–1910. doi: 10.1111/ajt.15909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Italiano J, Bush R, Acharya R, Upadhyay K. Persistent viral shedding despite seroconversion in a kidney transplant recipient with severe extrapulmonary COVID-19. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-239612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jang K, Khatri A, Majure DT. COVID-19 leading to acute encephalopathy in a patient with heart transplant. J Heart Lung Transplant. 2020;39:853–855. doi: 10.1016/j.healun.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jiang J, Miao Y, Zhao Y, Lu X, Zhou P, Zhou X, et al. Convalescent plasma therapy: helpful treatment of COVID-19 in a kidney transplant recipient presenting with severe clinical manifestations and complex complications. Clin Transplant. 2020;34:e14025. doi: 10.1111/ctr.14025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnson KM, Belfer JJ, Peterson GR, Boelkins MR, Dumkow LE. Managing COVID-19 in renal transplant recipients: a review of recent literature and case supporting corticosteroid-sparing immunosuppression. Pharmacotherapy. 2020;40:517–524. doi: 10.1002/phar.2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kadosh BS, Pavone J, Wu M, Reyentovich A, Gidea C. Collapsing glomerulopathy associated with COVID-19 infection in a heart transplant recipient. J Heart Lung Transplant. 2020;39:855–857. doi: 10.1016/j.healun.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kates OS, Fisher CE, Stankiewicz-Karita HC, Shepherd AK, Church EC, Kapnadak SG, et al. Earliest cases of coronavirus disease 2019 (COVID-19) identified in solid organ transplant recipients in the United States. Am J Transplant. 2020;20:1885–1890. doi: 10.1111/ajt.15944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Keller BC, Le A, Sobhanie M, Colburn N, Burcham P, Rosenheck J, et al. Early COVID-19 infection after lung transplantation. Am J Transplant. 2020;20:2923–2927. doi: 10.1111/ajt.16097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim Y, Kwon O, Paek JH, Park WY, Jin K, Hyun M, et al. Two distinct cases with COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20:2269–2275. doi: 10.1111/ajt.15947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kocak B, Arpali E, Akyollu B, Yelken B, Tekin S, Kanbay M, et al. Oligosymptomatic kidney transplant patients with COVID-19: do they pose a risk to other recipients? Transplant Proc. 2020;52:2663–2666. doi: 10.1016/j.transproceed.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koczulla RA, Sczepanski B, Koteczki A, Kuhnert S, Hecker M, Askevold I, et al. SARS-CoV-2 infection in two patients following recent lung transplantation. Am J Transplant. 2020;20:2928–2932. doi: 10.1111/ajt.15998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kumar RN, Tanna SD, Shetty AA, Stosor V. COVID-19 in an HIV-positive kidney transplant recipient. Transpl Infect Dis. 2020;22:e13338. doi: 10.1111/tid.13338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lauterio A, Valsecchi M, Santambrogio S, De Carlis R, Merli M, Calini A, et al. Successful recovery from severe COVID-19 pneumonia after kidney transplantation: the interplay between immunosuppression and novel therapy including tocilizumab. Transpl Infect Dis. 2020;22:e13334. doi: 10.1111/tid.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lazareth H, Pere H, Binois Y, Chabannes M, Schurder J, Bruneau T, et al. COVID-19-related collapsing glomerulopathy in a kidney transplant recipient. Am J Kidney Dis. 2020;76:590–594. doi: 10.1053/j.ajkd.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li F, Cai J, Dong N. First cases of COVID-19 in heart transplantation from. China. J Heart Lung Transplant. 2020;39:496–497. doi: 10.1016/j.healun.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li J, Chen G, Zhang M, Tu S, Chen C. Different clinical presentations of two renal transplant recipients with coronavirus disease 2019: a case report. BMC Infect Dis. 2020;20:707. doi: 10.1186/s12879-020-05434-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li Q, Cheng Q, Zhao Z, Dai N, Zeng L, Zhu L, et al. Novel coronavirus infection and acute kidney injury in two renal transplant recipients: a case report. J Int Med Res. 2020;48 doi: 10.1177/0300060520964009. 300060520964009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu B, Wang Y, Zhao Y, Shi H, Zeng F, Chen Z. Successful treatment of severe COVID-19 pneumonia in a liver transplant recipient. Am J Transplant. 2020;20:1891–1895. doi: 10.1111/ajt.15901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ma BA, Hung IFN, Chan GCW, Tam AR, Chan SSK, Wong BCK, et al. Case of “relapsing” COVID-19 in a kidney transplant recipient. Nephrology (Carlton) 2020;25:933–936. doi: 10.1111/nep.13786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Machado DJB, Ianhez LE. COVID-19 pneumonia in kidney transplant recipients-where we are? Transpl Infect Dis. 2020;22:e13306. doi: 10.1111/tid.13306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maggi U, De Carlis L, Yiu D, Colledan M, Regalia E, Rossi G, et al. The impact of the COVID-19 outbreak on liver transplantation programs in Northern Italy. Am J Transplant. 2020;20:1840–1848. doi: 10.1111/ajt.15948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Man Z, Jing Z, Huibo S, Bin L, Fanjun Z. Viral shedding prolongation in a kidney transplant patient with COVID-19 pneumonia. Am J Transplant. 2020;20:2626–2627. doi: 10.1111/ajt.15996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marx D, Moulin B, Fafi-Kremer S, Benotmane I, Gautier G, Perrin P, et al. First case of COVID-19 in a kidney transplant recipient treated with belatacept. Am J Transplant. 2020;20:1944–1946. doi: 10.1111/ajt.15919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Massoumi H, Rocca J, Frager S, Kinkhabwala M. Changes in liver transplant center practice in response to coronavirus disease 2019: unmasking dramatic center-level variability. Liver Transpl. 2020;26:1198–1199. doi: 10.1002/lt.25811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mathiasen VD, Oversoe SK, Ott P, Jensen-Fangel S, Leth S. Recovery of moderate coronavirus disease 2019 in a liver transplant recipient on continued immunosuppression: a case report. Transplant Proc. 2020;52:2703–2706. doi: 10.1016/j.transproceed.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mathies D, Rauschning D, Wagner U, Mueller F, Maibaum M, Binnemann C, et al. A case of SARS-CoV-2 pneumonia with successful antiviral therapy in a 77-year-old man with a heart transplant. Am J Transplant. 2020;20:1925–1929. doi: 10.1111/ajt.15932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Meziyerh S, Zwart TC, van Etten RW, Janson JA, van Gelder T, Alwayn IPJ, et al. Severe COVID-19 in a renal transplant recipient: a focus on pharmacokinetics. Am J Transplant. 2020;20:1896–1901. doi: 10.1111/ajt.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Modi AR, Koval CE, Taege AJ, Modaresi Esfeh J, Eghtesad B, Narayanan Menon KV, et al. Coronavirus disease 2019 in an orthotopic liver transplant recipient living with human immunodeficiency virus. Transpl Infect Dis. 2020;22:e13351. doi: 10.1111/tid.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mohamed MA, Kaur J, Wani F, Kichloo A, Bhanot R. Renal transplant recipient with concurrent COVID-19 and Stenotrophomonas maltophilia pneumonia treated with trimethoprim/sulfamethoxazole leading to acute kidney injury: a therapeutic dilemma. Am J Case Rep. 2020;21 doi: 10.12659/AJCR.926464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Monne M, Asproni R, Fancello T, Piras G, Sulis V, Floris AR, et al. SARS-CoV-2 systemic infection in a kidney transplant recipient: sequence analysis in clinical specimens. Eur Rev Med Pharmacol Sci. 2020;24:11914–11918. doi: 10.26355/eurrev_202011_23850. [DOI] [PubMed] [Google Scholar]
- 89.Namazee N, Mahmoudi H, Afzal P, Ghaffari S. Novel coronavirus 2019 pneumonia in a kidney transplant recipient. Am J Transplant. 2020;20:2599–2601. doi: 10.1111/ajt.15999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nikoupour H, Arasteh P, Gholami S, Nikeghbalian S. Liver transplantation and COVID-19: a case report and cross comparison between two identical twins with COVID-19. BMC Surg. 2020;20:181. doi: 10.1186/s12893-020-00837-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ning L, Liu L, Li W, Liu H, Wang J, Yao Z, et al. Novel coronavirus (SARS-CoV-2) infection in a renal transplant recipient: case report. Am J Transplant. 2020;20:1864–1868. doi: 10.1111/ajt.15897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Qin J, Wang H, Qin X, Zhang P, Zhu L, Cai J, et al. Perioperative presentation of COVID-19 disease in a liver transplant recipient. Hepatology. 2020;72:1491–1493. doi: 10.1002/hep.31257. [DOI] [PubMed] [Google Scholar]
- 93.Renaud-Picard B, Gallais F, Ohana M, Zeyons F, Kretz B, Andre J, et al. Bilateral acute cardioembolic limb ischemia after coronavirus disease 2019 pneumonia in a lung transplant recipient: a case report. Transplant Proc. 2020;52:2715–2718. doi: 10.1016/j.transproceed.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sakulkonkij P, Bruminhent J, Pankongngam C, Chalermphunchai N. A family cluster of diagnosed coronavirus disease 2019 (COVID-19) kidney transplant recipient in Thailand. Immun Inflamm Dis. 2020;8:534–543. doi: 10.1002/iid3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Seminari E, Colaneri M, Sambo M, Gallazzi I, Di Matteo A, Roda S, et al. SARS CoV-2 infection in a renal-transplanted patient: a case report. Am J Transplant. 2020;20:1882–1884. doi: 10.1111/ajt.15902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Serrano OK, Kutzler HL, Rochon C, Radojevic JA, Lawlor MT, Hammond JA, et al. Incidental COVID-19 in a heart-kidney transplant recipient with malnutrition and recurrent infections: implications for the SARS-CoV-2 immune response. Transpl Infect Dis. 2020;22:e13367. doi: 10.1111/tid.13367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sessa A, Mazzola A, Lim C, Atif M, Pappatella J, Pourcher V, et al. COVID-19 in a liver transplant recipient: could iatrogenic immunosuppression have prevented severe pneumonia? A case report. World J Gastroenterol. 2020;26:7076–7084. doi: 10.3748/wjg.v26.i44.7076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shingare A, Bahadur MM, Raina S. COVID-19 in recent kidney transplant recipients. Am J Transplant. 2020;20:3206–3209. doi: 10.1111/ajt.16120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Soquet J, Rousse N, Moussa M, Goeminne C, Deblauwe D, Vuotto F, et al. Heart retransplantation following COVID-19 illness in a heart transplant recipient. J Heart Lung Transplant. 2020;39:983–985. doi: 10.1016/j.healun.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sperry BW, Khumri TM, Kao AC. Donor-derived cell-free DNA in a heart transplant patient with COVID-19. Clin Transplant. 2020;34:e14070. doi: 10.1111/ctr.14070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Suwanwongse K, Shabarek N. Fatal outcome in a kidney-pancreas transplant recipient with COVID-19. Cureus. 2020;12:e8691. doi: 10.7759/cureus.8691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Taha M, Sharma A, Taha M, Samavati L. Coronavirus disease 2019 in immunocompromised organ transplant recipients: a case report and review of the literature. Transplant Proc. 2020;52:2698–2702. doi: 10.1016/j.transproceed.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tantisattamo E, Reddy UG, Duong DK, Ferrey AJ, Ichii H, Dafoe DC, et al. Hyponatremia: a possible immuno-neuroendocrine interface with COVID-19 in a kidney transplant recipient. Transpl Infect Dis. 2020;22:e13355. doi: 10.1111/tid.13355. [DOI] [PubMed] [Google Scholar]
- 104.Tatar E, Karatas M, Bozaci I, Ari A, Acar T, Simsek C, et al. Intravenous immunoglobulin and favipiravir treatment for a kidney transplant patient with severe COVID-19 pneumonia. Transfus Apher Sci. 2020;59 doi: 10.1016/j.transci.2020.102904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Thammathiwat T, Tungsanga S, Tiankanon K, Torvorapanit P, Chumpangern W, Udomkarnjananun S, et al. A case of successful treatment of severe COVID-19 pneumonia with favipiravir and tocilizumab in post-kidney transplant recipient. Transpl Infect Dis. 2021;23:e13388. doi: 10.1111/tid.13388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Velioglu A, Tuglular S. Care of asymptomatic SARS-CoV-2 positive kidney transplant recipients. Transpl Int. 2020;33:1331–1332. doi: 10.1111/tri.13691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang J, Li X, Cao G, Wu X, Wang Z, Yan T. COVID-19 in a kidney transplant patient. Eur Urol. 2020;77:769–770. doi: 10.1016/j.eururo.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Westhoff TH, Seibert FS, Bauer F, Stervbo U, Anft M, Doevelaar AAN, et al. Allograft infiltration and meningoencephalitis by SARS-CoV-2 in a pancreas-kidney transplant recipient. Am J Transplant. 2020;20:3216–3220. doi: 10.1111/ajt.16223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu JJ, Samaha D, Mondhe S, Massicotte-Azarniouch D, Knoll G, Ruzicka M. Renal infarct in a COVID-19-positive kidney-pancreas transplant recipient. Am J Transplant. 2020;20:3221–3224. doi: 10.1111/ajt.16089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yamada M, Rastogi P, Ince D, Thayyil A, Adela Mansilla M, Smith RJH, et al. Minimal change disease with nephrotic syndrome associated with coronavirus disease 2019 after apolipoprotein L1 risk variant kidney transplant: a case report. Transplant Proc. 2020;52:2693–2697. doi: 10.1016/j.transproceed.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhong Z, Zhang Q, Xia H, Wang W, Liang W, Zhou W, et al. Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients. Am J Transplant. 2020;20:1916–1921. doi: 10.1111/ajt.15928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhu L, Xu X, Ma K, Yang J, Guan H, Chen S, et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant. 2020;20:1859–1863. doi: 10.1111/ajt.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ahluwalia M, Givertz MM, Mehra MM. A proposed strategy for management of immunosuppression in heart transplant patients with COVID-19. Clin Transplant. 2020;34:e14032. doi: 10.1111/ctr.14032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Akalin E, Azzi Y, Bartash R, Seethamraju H, Parides M, Hemmige V, et al. COVID-19 and kidney transplantation. N Engl J Med. 2020;382:2475–2477. doi: 10.1056/NEJMc2011117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Akdur A, Karakaya E, Ayvazoglu Soy EH, Alshalabi O, Kirnap M, Arslan H, et al. Coronavirus disease (COVID-19) in kidney and liver transplant patients: a single-center experience. Exp Clin Transplant. 2020;18:270–274. doi: 10.6002/ect.2020.0193. [DOI] [PubMed] [Google Scholar]
- 116.Al-Darzi W, Aurora L, Michaels A, Cowger J, Grafton G, Selektor Y, et al. Heart transplant recipients with confirmed 2019 novel coronavirus infection: the Detroit experience. Clin Transplant. 2020;34:e14091. doi: 10.1111/ctr.14091. [DOI] [PubMed] [Google Scholar]
- 117.Ali T, Al-Ali A, Fajji L, Hammad E, Nazmi A, Alahmadi I, et al. Coronavirus disease-19: disease severity and outcomes of solid organ transplant recipients: different spectrums of disease in different populations? Transplantation. 2021;105:121–127. doi: 10.1097/TP.0000000000003433. [DOI] [PubMed] [Google Scholar]
- 118.Azzi Y, Parides M, Alani O, Loarte-Campos P, Bartash R, Forest S, et al. COVID-19 infection in kidney transplant recipients at the epicenter of pandemics. Kidney Int. 2020;98:1559–1567. doi: 10.1016/j.kint.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Becchetti C, Zambelli MF, Pasulo L, Donato MF, Invernizzi F, Detry O, et al. COVID-19 in an international European liver transplant recipient cohort. Gut. 2020;69:1832–1840. doi: 10.1136/gutjnl-2020-321923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bosch F, Borner N, Kemmner S, Lampert C, Jacob S, Koliogiannis D, et al. Attenuated early inflammatory response in solid organ recipients with COVID-19. Clin Transplant. 2020;34:e14027. doi: 10.1111/ctr.14027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bossini N, Alberici F, Delbarba E, Valerio F, Manenti C, Possenti S, et al. Kidney transplant patients with SARS-CoV-2 infection: the Brescia Renal COVID task force experience. Am J Transplant. 2020;20:3019–3029. doi: 10.1111/ajt.16176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Caraffa R, Bagozzi L, Fiocco A, Bifulco O, Nadali M, Ponzoni M, et al. Coronavirus disease 2019 (COVID-19) in the heart transplant population: a single-centre experience. Eur J Cardiothorac Surg. 2020;58:899–906. doi: 10.1093/ejcts/ezaa323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Carey SA, Afzal A, Jamil A, Williams S, Gottlieb RL. Outpatient COVID-19 surveillance testing in orthotopic heart transplant recipients. Clin Transplant. 2020;34:e14105. doi: 10.1111/ctr.14105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen TY, Farghaly S, Cham S, Tatem LL, Sin JH, Rauda R, et al. COVID-19 pneumonia in kidney transplant recipients: focus on immunosuppression management. Transpl Infect Dis. 2020;22:e13378. doi: 10.1111/tid.13378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Christensen J, Kumar D, Moinuddin I, Bryson A, Kashi Z, Kimball P, et al. Coronavirus disease 2019 viremia, serologies, and clinical course in a case series of transplant recipients. Transplant Proc. 2020;52:2637–2641. doi: 10.1016/j.transproceed.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Craig-Schapiro R, Salinas T, Lubetzky M, Abel BT, Sultan S, Lee JR, et al. COVID-19 outcomes in patients waitlisted for kidney transplantation and kidney transplant recipients. Am J Transplant. 2021;21:1576–1585. doi: 10.1111/ajt.16351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cravedi P, Mothi SS, Azzi Y, Haverly M, Farouk SS, Perez-Saez MJ, et al. COVID-19 and kidney transplantation: results from the TANGO International Transplant Consortium. Am J Transplant. 2020;20:3140–3148. doi: 10.1111/ajt.16185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Demir E, Uyar M, Parmaksiz E, Sinangil A, Yelken B, Dirim AB, et al. COVID-19 in kidney transplant recipients: a multicenter experience in Istanbul. Transpl Infect Dis. 2020;22:e13371. doi: 10.1111/tid.13371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Devresse A, Belkhir L, Vo B, Ghaye B, Scohy A, Kabamba B, et al. COVID-19 infection in kidney transplant recipients: a single-center case series of 22 cases from Belgium. Kidney Med. 2020;2:459–466. doi: 10.1016/j.xkme.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Elias M, Pievani D, Randoux C, Louis K, Denis B, Delion A, et al. COVID-19 infection in kidney transplant recipients: disease incidence and clinical outcomes. J Am Soc Nephrol. 2020;31:2413–2423. doi: 10.1681/ASN.2020050639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fava A, Cucchiari D, Montero N, Toapanta N, Centellas FJ, Vila-Santandreu A, et al. Clinical characteristics and risk factors for severe COVID-19 in hospitalized kidney transplant recipients: a multicentric cohort study. Am J Transplant. 2020;20:3030–3041. doi: 10.1111/ajt.16246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Felldin M, Softeland JM, Magnusson J, Ekberg J, Karason K, Schult A, et al. Initial report from a Swedish high-volume transplant center after the first wave of the COVID-19 pandemic. Transplantation. 2021;105:108–114. doi: 10.1097/TP.0000000000003436. [DOI] [PubMed] [Google Scholar]
- 133.Garcia-Cosio MD, Flores Hernan M, Caravaca Perez P, Lopez-Medrano F, Arribas F, Delgado Jimenez J. Heart transplantation during the COVID-19 pandemic: follow-up organization and characteristics of infected patients. Rev Esp Cardiol (Engl Ed) 2020;73:1077–1080. doi: 10.1016/j.rec.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ghaffari Rahbar M, Nafar M, Khoshdel A, Dalili N, Abrishami A, Firouzan A, et al. Low rate of COVID-19 pneumonia in kidney transplant recipients-a battle between infection and immune response? Transpl Infect Dis. 2020;22:e13406. doi: 10.1111/tid.13406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hartzell S, Bin S, Benedetti C, Haverly M, Gallon L, Zaza G, et al. Evidence of potent humoral immune activity in COVID-19-infected kidney transplant recipients. Am J Transplant. 2020;20:3149–3161. doi: 10.1111/ajt.16261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Husain SA, Dube G, Morris H, Fernandez H, Chang JH, Paget K, et al. Early outcomes of outpatient management of kidney transplant recipients with coronavirus disease 2019. Clin J Am Soc Nephrol. 2020;15:1174–1178. doi: 10.2215/CJN.05170420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lum E, Bunnapradist S, Multani A, Beaird OE, Carlson M, Gaynor P, et al. Spectrum of coronavirus disease 2019 outcomes in kidney transplant recipients: a single-center experience. Transplant Proc. 2020;52:2654–2658. doi: 10.1016/j.transproceed.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Mehta SA, Leonard J, Labella P, Cartiera K, Soomro I, Neumann H, et al. Outpatient management of kidney transplant recipients with suspected COVID-19-single-center experience during the New York City surge. Transpl Infect Dis. 2020;22:e13383. doi: 10.1111/tid.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miarons M, Larrosa-Garcia M, Garcia-Garcia S, Los-Arcos I, Moreso F, Berastegui C, et al. COVID-19 in solid organ transplantation: a matched retrospective cohort study and evaluation of immunosuppression management. Transplantation. 2021;105:138–150. doi: 10.1097/TP.0000000000003460. [DOI] [PubMed] [Google Scholar]
- 140.Mocchegiani F, Baroni GS, Vivarelli M. Mild impact of SARS-CoV-2 infection on the entire population of liver transplant recipients: the experience of an Italian centre based in a high-risk area. Updates Surg. 2020;72:1291–1293. doi: 10.1007/s13304-020-00881-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Montagud-Marrahi E, Cofan F, Torregrosa JV, Cucchiari D, Ventura-Aguiar P, Revuelta I, et al. Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single center cohort of kidney recipients. Am J Transplant. 2020;20:2958–2959. doi: 10.1111/ajt.15970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Patrono D, Lupo F, Canta F, Mazza E, Mirabella S, Corcione S, et al. Outcome of COVID-19 in liver transplant recipients: a preliminary report from Northwestern Italy. Transpl Infect Dis. 2020;22:e13353. doi: 10.1111/tid.13353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rivinius R, Kaya Z, Schramm R, Boeken U, Provaznik Z, Heim C, et al. COVID-19 among heart transplant recipients in Germany: a multicenter survey. Clin Res Cardiol. 2020;109:1531–1539. doi: 10.1007/s00392-020-01722-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Roberts MB, Izzy S, Tahir Z, Al Jarrah A, Fishman JA, El Khoury J. COVID-19 in solid organ transplant recipients: dynamics of disease progression and inflammatory markers in ICU and non-ICU admitted patients. Transpl Infect Dis. 2020;22:e13407. doi: 10.1111/tid.13407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rodriguez-Cubillo B, de la Higuera MAM, Lucena R, Franci EV, Hurtado M, Romero NC, et al. Should cyclosporine be useful in renal transplant recipients affected by SARS-CoV-2? Am J Transplant. 2020;20:3173–3181. doi: 10.1111/ajt.16141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Travi G, Rossotti R, Merli M, Sacco A, Perricone G, Lauterio A, et al. Clinical outcome in solid organ transplant recipients with COVID-19: a single-center experience. Am J Transplant. 2020;20:2628–2629. doi: 10.1111/ajt.16069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Trujillo H, Caravaca-Fontan F, Sevillano A, Gutierrez E, Fernandez-Ruiz M, Lopez-Medrano F, et al. Tocilizumab use in kidney transplant patients with COVID-19. Clin Transplant. 2020;34:e14072. doi: 10.1111/ctr.14072. [DOI] [PubMed] [Google Scholar]
- 148.Tschopp J, L'Huillier AG, Mombelli M, Mueller NJ, Khanna N, Garzoni C, et al. First experience of SARS-CoV-2 infections in solid organ transplant recipients in the Swiss Transplant Cohort Study. Am J Transplant. 2020;20:2876–2882. doi: 10.1111/ajt.16062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Varghese J, Malleeswaran S, Patcha RV, Appusamy E, Karnan P, Kapoor D, et al. A multicentric experience on living donor liver transplantation in coronavirus disease 2019 hotspots in India. Liver Transpl. 2021;27:1334–1338. doi: 10.1002/lt.25957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yi SG, Rogers AW, Saharia A, Aoun M, Faour R, Abdelrahim M, et al. Early experience with COVID-19 and solid organ transplantation at a US high-volume transplant center. Transplantation. 2020;104:2208–2214. doi: 10.1097/TP.0000000000003339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abrishami A, Samavat S, Behnam B, Arab-Ahmadi M, Nafar M, Sanei Taheri M. Clinical course, imaging features, and outcomes of COVID-19 in kidney transplant recipients. Eur Urol. 2020;78:281–286. doi: 10.1016/j.eururo.2020.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, Pola A, et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97:1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Aversa M, Benvenuto L, Anderson M, Shah L, Robbins H, Pereira M, et al. COVID-19 in lung transplant recipients: a single center case series from New York City. Am J Transplant. 2020;20:3072–3080. doi: 10.1111/ajt.16241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Banerjee D, Popoola J, Shah S, Ster IC, Quan V, Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97:1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Benotmane I, Gautier-Vargas G, Wendling MJ, Perrin P, Velay A, Bassand X, et al. In-depth virological assessment of kidney transplant recipients with COVID-19. Am J Transplant. 2020;20:3162–3172. doi: 10.1111/ajt.16251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Dhampalwar S, Saigal S, Choudhary N, Saraf N, Bhangui P, Rastogi A, et al. Outcomes of coronavirus disease 2019 in living donor liver transplant recipients. Liver Transpl. 2020;26:1665–1666. doi: 10.1002/lt.25909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Fung M, Chiu CY, DeVoe C, Doernberg SB, Schwartz BS, Langelier C, et al. Clinical outcomes and serologic response in solid organ transplant recipients with COVID-19: a case series from the United States. Am J Transplant. 2020;20:3225–3233. doi: 10.1111/ajt.16079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ketcham SW, Adie SK, Malliett A, Abdul-Aziz AA, Bitar A, et al. Coronavirus disease-2019 in heart transplant recipients in southeastern Michigan: a case series. J Card Fail. 2020;26:457–461. doi: 10.1016/j.cardfail.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kolonko A, Dudzicz S, Wiecek A, Krol R. COVID-19 infection in solid organ transplant recipients: a single-center experience with patients immediately after transplantation. Transpl Infect Dis. 2021;23:e13381. doi: 10.1111/tid.13381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Latif F, Farr MA, Clerkin KJ, Habal MV, Takeda K, Naka Y, et al. Characteristics and outcomes of recipients of heart transplant with coronavirus disease 2019. JAMA Cardiol. 2020;5:1165–1169. doi: 10.1001/jamacardio.2020.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lee BT, Perumalswami PV, Im GY, Florman S, Schiano TD, Study Group COBE. COVID-19 in liver transplant recipients: an initial experience from the US epicenter. Gastroenterology. 2020;159:1176–1178. doi: 10.1053/j.gastro.2020.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lima B, Gibson GT, Vullaganti S, Malhame K, Maybaum S, Hussain ST, et al. COVID-19 in recent heart transplant recipients: clinicopathologic features and early outcomes. Transpl Infect Dis. 2020;22:e13382. doi: 10.1111/tid.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Loinaz C, Marcacuzco A, Fernandez-Ruiz M, Caso O, Cambra F, San Juan R, et al. Varied clinical presentation and outcome of SARS-CoV-2 infection in liver transplant recipients: initial experience at a single center in Madrid, Spain. Transpl Infect Dis. 2020;22:e13372. doi: 10.1111/tid.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lubetzky M, Aull MJ, Craig-Schapiro R, Lee JR, Marku-Podvorica J, Salinas T, et al. Kidney allograft recipients, immunosuppression, and coronavirus disease-2019: a report of consecutive cases from a New York City transplant center. Nephrol Dial Transplant. 2020;35:1250–1261. doi: 10.1093/ndt/gfaa154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Maritati F, Cerutti E, Zuccatosta L, Fiorentini A, Finale C, Ficosecco M, et al. SARS-CoV-2 infection in kidney transplant recipients: experience of the Italian Marche region. Transpl Infect Dis. 2020;22:e13377. doi: 10.1111/tid.13377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mella A, Mingozzi S, Gallo E, Lavacca A, Rossetti M, Clari R, et al. Case series of six kidney transplanted patients with COVID-19 pneumonia treated with tocilizumab. Transpl Infect Dis. 2020;22:e13348. doi: 10.1111/tid.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Morillas JA, Marco Canosa F, Srinivas P, Asadi T, Calabrese C, Rajendram P, et al. Tocilizumab therapy in 5 solid and composite tissue transplant recipients with early ARDS due to SARS-CoV-2. Am J Transplant. 2020;20:3191–3197. doi: 10.1111/ajt.16080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Nair V, Jandovitz N, Hirsch JS, Nair G, Abate M, Bhaskaran M, et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20:1819–1825. doi: 10.1111/ajt.15967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rahman F, Liu STH, Taimur S, Jacobs S, Sullivan T, Dunn D, et al. Treatment with convalescent plasma in solid organ transplant recipients with COVID-19: experience at large transplant center in New York City. Clin Transplant. 2020;34:e14089. doi: 10.1111/ctr.14089. [DOI] [PubMed] [Google Scholar]
- 170.Silva F, Cipriano A, Cruz H, Tavares J, Fragoso J, Malheiro J, et al. SARS-CoV-2 infection in kidney transplant recipients: early report of five cases. Transpl Infect Dis. 2021;23:e13394. doi: 10.1111/tid.13394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Singhvi A, Barghash M, Lala A, Mitter SS, Parikh A, Oliveros E, et al. Challenges in heart transplantation during COVID-19: a single-center experience. J Heart Lung Transplant. 2020;39:894–903. doi: 10.1016/j.healun.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Trujillo H, Caravaca-Fontan F, Sevillano A, Gutierrez E, Caro J, Gutierrez E, et al. SARS-CoV-2 infection in hospitalized patients with kidney disease. Kidney Int Rep. 2020;5:905–909. doi: 10.1016/j.ekir.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tzukert K, Abel R, Mor Yosef Levi I, Gork I, Yosha Orpaz L, Azmanov H, et al. The challenge of treating kidney transplant recipients infected with COVID-19: report of the first cases in Israel. Isr Med Assoc J. 2020;22:602–604. [PubMed] [Google Scholar]
- 174.Verleden GM, Godinas L, Lorent N, Van Bleyenbergh P, Dupont L, Delcroix M, et al. COVID-19 in lung transplant patients: a case series. Am J Transplant. 2020;20:3234–3238. doi: 10.1111/ajt.16212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang H, Chen Y, Yuan Q, Xia QX, Zeng XP, Peng JT, et al. Identification of kidney transplant recipients with coronavirus disease 2019. Eur Urol. 2020;77:742–747. doi: 10.1016/j.eururo.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zhu L, Gong N, Liu B, Lu X, Chen D, Chen S, et al. Coronavirus disease 2019 pneumonia in immunosuppressed renal transplant recipients: a summary of 10 confirmed cases in Wuhan, China. Eur Urol. 2020;77:748–754. doi: 10.1016/j.eururo.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Coll E, Fernandez-Ruiz M, Sanchez-Alvarez JE, Martinez-Fernandez JR, Crespo M, Gayoso J, et al. COVID-19 in transplant recipients: the Spanish experience. Am J Transplant. 2020;21:1825–1837. doi: 10.1111/ajt.16369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Iacovoni A, Boffini M, Pidello S, Simonato E, Barbero C, Sebastiani R, et al. A case series of novel coronavirus infection in heart transplantation from 2 centers in the pandemic area in the North of Italy. J Heart Lung Transplant. 2020;39:1081–1088. doi: 10.1016/j.healun.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kute VB, Bhalla AK, Guleria S, Ray DS, Bahadur MM, Shingare A, et al. Clinical profile and outcome of COVID-19 in 250 kidney transplant recipients: a multicenter cohort study from India. Transplantation. 2021;105:851–860. doi: 10.1097/TP.0000000000003593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Molnar MA, Bhalla A, Azhar A, Tsujita M, Talwar M, Balaraman V, et al. Outcomes of critically ill solid organ transplant patients with COVID-19 in the United States. Am J Transplant. 2020;20:3061–3071. doi: 10.1111/ajt.16280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ozturk S, Turgutalp K, Arici M, Odabas AR, Altiparmak MR, Aydin Z, et al. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrol Dial Transplant. 2020;35:2083–2095. doi: 10.1093/ndt/gfaa271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Passamonti SM, Cannavo A, Trunzo V, Caporale V, Buonocore R, DeFeo TM. Solid organ transplantation in the coronavirus disease 2019 era: “The Great Bet” in the North Italy Transplant Program area. Transplant Proc. 2020;52:2631–2636. doi: 10.1016/j.transproceed.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Saez-Gimenez B, Berastegui C, Barrecheguren M, Revilla-Lopez E, Los Arcos I, Alonso R, et al. COVID-19 in lung transplant recipients: a multicenter study. Am J Transplant. 2020;21:1816–1824. doi: 10.1111/ajt.16364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Webb GJ, Marjot T, Cook JA, Aloman C, Armstrong MJ, Brenner EJ, et al. Outcomes following SARS-CoV-2 infection in liver transplant recipients: an international registry study. Lancet Gastroenterol Hepatol. 2020;5:1008–1016. doi: 10.1016/S2468-1253(20)30271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Chaudhry ZS, Williams JD, Vahia A, Fadel R, Parraga Acosta T, Prashar R, et al. Clinical characteristics and outcomes of COVID-19 in solid organ transplant recipients: a cohort study. Am J Transplant. 2020;20:3051–3060. doi: 10.1111/ajt.16188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Pereira MR, Aversa MM, Farr MA, Miko BA, Aaron JG, Mohan S, et al. Tocilizumab for severe COVID-19 in solid organ transplant recipients: a matched cohort study. Am J Transplant. 2020;20:3198–3205. doi: 10.1111/ajt.16314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Sharma P, Chen V, Fung CM, Troost JP, Patel VN, Combs M, et al. COVID-19 outcomes among solid organ transplant recipients: a case-control study. Transplantation. 2021;105:128–137. doi: 10.1097/TP.0000000000003447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.British Transplantation Society . 2021. Guidance on the management of transplant recipients diagnosed with or suspected of having COVID19.https://bts.org.uk/wp-content/uploads/2021/01/Clinical-management-of-transplants-and-immunosuppression-22nd-January-2021-FINAL.pdf [accessed 07.01.21] [Google Scholar]
- 189.International Society of Heart and Lung Transplantation . 2021. Guidance from the International Society of Heart and Lung Transplantation regarding the SARS CoV-2 pandemic.https://ishlt.org/ishlt/media/documents/SARS-CoV-2_-Guidance-for-Cardiothoracic-Transplant-and-VAD-centers.pdf [accessed 07.01.21] [Google Scholar]
- 190.Transplantation Society . 2021. Guidance on coronavirus disease 2019 (COVID-19) for transplant clinicians.https://tts.org/23-tid/tid-news/657-tid-update-and-guidance-on-2019-novel-coronavirus-2019-ncov-for-transplant-id-clinicians [accessed 07.01.21] [Google Scholar]
- 191.American Association for the Study of Liver Diseases . 2021. Clinical best practice advice for hepatology and liver transplant providers during the COVID-19 pandemic: AASLD Expert Panel Consensus Statement.https://www.aasld.org/sites/default/files/2021-03/AASLD-COVID19-ExpertPanelConsensusStatement-March92021.pdf [accessed 07.01.21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Canadian Society of Transplantation . 2021. Consensus guidance and recommendations for organ donation and transplantation services during COVID-19 pandemic.https://professionaleducation.blood.ca/sites/msi/files/20210406_covid-19_consensus_guidance.pdf [accessed 07.01.21] [Google Scholar]
- 193.American Society of Transplantation . 2021. 2019-nCoV (coronavirus): FAQs for organ transplantation.https://www.myast.org/sites/default/files/COVID19%20FAQ%20Tx%20Centers%2004.12.2021.pdf [accessed 07.01.21] [Google Scholar]
- 194.Fang X, Li S, Yu H, Wang P, Zhang Y, Chen Z, et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging (Albany NY) 2020;12:12493–12503. doi: 10.18632/aging.103579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Mayo Clin Proc. 2020;95:1613–1620. doi: 10.1016/j.mayocp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Karagiannidis C, Mostert C, Hentschker C, Voshaar T, Malzahn J, Schillinger G, et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:853–862. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Belli LS, Fondevila C, Cortesi PA, Conti S, Karam V, Adam R, et al. Protective role of tacrolimus, deleterious role of age and comorbidities in liver transplant recipients with COVID-19: results from the ELITA/ELTR multi-center European study. Gastroenterology. 2021;160:1151–1163. doi: 10.1053/j.gastro.2020.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Colmenero J, Rodríguez-Perálvarez M, Salcedo M, Arias-Milla A, Muñoz-Serrano A, Graus J, et al. Epidemiological pattern, incidence, and outcomes of COVID-19 in liver transplant patients. J Hepatol. 2021;74:148–155. doi: 10.1016/j.jhep.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Barlow-Pay F, Htut TW, Khezrian M, Myint PK. Systematic review of immunosuppressant guidelines in the COVID-19 pandemic. Ther Adv Drug Saf. 2021;12 doi: 10.1177/2042098620985687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]