Abstract
Objectives
This study explored differences in COVID-19 incidence, mortality, and timing among long-term care facility (LTCF) residents and staff with those living in the community in South Carolina (SC).
Design
Longitudinal secondary data analysis.
Setting and Participants
Adults age ≥18 in SC with confirmed COVID-19 diagnosis from 3/15/2020 and 1/2/2021 (n = 307,891).
Methods
COVID-19 data came from the SC Department of Health and Environmental Control (SCDHEC). We included all COVID-19 cases, hospitalizations, and deaths among adult residents. Residence and employment in LTCF were confirmed by SCDHEC. Descriptive statistics and trends for cases, hospitalizations, and deaths were calculated. We used Cox proportional hazards to compare COVID-19 mortality in LTCF residents and staff to community dwelling older adults and adults not employed in LTCF, respectively, controlling for age, gender, race, and pre-existing chronic health conditions.
Results
LTC residents experienced greater incidence of cases throughout the study period until the week ending on 1/2/21. LTCF residents with COVID-19 were more likely to be hospitalized compared to older adults in the community and 74% more likely to die (HR: 1.74, 95% CI: 1.59-1.90), after adjusting. LTC staff experienced greater incidence of cases compared to adults not employed in LTCF until the week ending on 12/26/2020, while experiencing similar incidence of death compared to the similar community members. After adjusting, LTC staff had 0.58 (HR = 0.58; CI: 0.39-0.88) times lower hazard of death compared to community members that did not work in a LTCF.
Conclusions and Implications
Narrowing of the gap between LTCF and community-wide infection and mortality rates over the study period suggests that early detection of COVID-19 in LTCFs could serve as a first indicator of disease spread in the greater community. Results also indicate that policies and regulations addressing staff testing and protection may help to slow or prevent spread within facilities.
Keywords: COVID-19, older adults, long-term care facilities, staff
The novel SARS-CoV-2 (COVID-19) virus was first detected in South Carolina (SC) on March 4th, 2020, and case numbers have grown in the state since. COVID-19 has disproportionately impacted vulnerable populations,1 namely those with pre-existing conditions,2 , 3 overweight/obese,4 , 5 dependency,6 dementia,7 frailty,8 and those age ≥ 60.2 , 9 Long-term care facilities (LTCF) tend to have more vulnerable populations, including older adults with pre-existing conditions.10 Consequently, LTCF residents are at greater risk of COVID-19 and adverse consequences such as hospitalization and death.11 Concerns regarding spread in LTCF populations are compounded by findings of asymptomatic and/or atypical manifestation among residents, as well as a negative impact on well-being and mental health of residents without COVID-19.12
State-and facility-level pandemic response may significantly impact the spread of COVID-19 in LTCF, especially through staff mitigation measures.13, 14, 15 Important facility-level factors include the availability of necessary protective equipment, staff cases, testing, and visitation policies.16 Facility factors are in-turn influenced by state and federal guidelines and policies such as stay-at-home orders and visitation recommendations.17 Mitigation efforts may also have negative impacts on resident well-being. For instance, restrictions implemented to slow COVID-19 have been found to decrease residents’ social encounters, leading to increased loneliness, anxiety, and depression.18 , 19 The balance of resident well-being and safety is an important consideration when implementing control strategies in LTCF.20
The disproportionate impact of COVID-19 on LTCFs highlights the need to understand and describe the spread of COVID-19 to help inform policies, preparedness, monitoring, and coordination of future pandemic response. Given wide variability of state and LTCF responses to the COVID-19 outbreak, describing how rates of disease have changed concurrently with mitigation measures over time may provide valuable information to future outbreak strategies. Likewise, given the likely bidirectional links between LTCF resident and staff infections, it is important to describe and compare the parallel spread of COVID-19 among LTCF employees and support staff. This study explored descriptive differences and associations in COVID-19 incidence and mortality among older adults living in the community and those living LTCFs in SC. We describe the timeline of spread among LTCF residents and staff, along with relevant state-specific and national changes in policy and guidance.
Methods
Data and Sample
Data come from the South Carolina Infectious Disease and Outbreak Network (SCION), a division of the South Carolina Department of Health and Environmental Control (DHEC) that collects information on infectious disease occurrence in the state. SC law requires reporting of all COVID-19 test results to SCION. For all positive tests, DHEC staff contact the positive individual to complete a case report with demographic, health, employment, and additional information. All data for this study were obtained through a data use agreement with DHEC and the analysis was approved by the DHEC Institutional Review Board.
We included all COVID-19 cases among SC residents age 18 or older reported between 3/15/2020 and 1/2/2021. For the comparison of LTC residents to community-dwelling older adults, only individuals 65 and older were included; however, for analyses of LTCF staff, we included all adults while excluding those in LTCFs. In SC, LTCFs included nursing homes and community residential care facilities. Cases were confirmed by detection of severe acute respiratory syndrome coronavirus 2 ribonucleic acid (SARS-CoV-2 RNA) in a clinical specimen using a molecular amplification detection test. Probable cases met one of the following criteria: clinical criteria AND epidemiologic linkage with no confirmatory laboratory testing performed for SARS-CoV-2; presumptive laboratory evidence (detection of SARS-CoV-2 by antigen test in a respiratory specimen); or vital records criteria with no confirmatory laboratory evidence for SARS-CoV-2. Detailed information on case determination is available from the CDC.21 State LTC resident population size was determined from reporting by all certified LTC facilities to DHEC. Mandatory LTC resident population reporting began on 5/17/2020; analyses using LTC resident population size before mandated reporting assumed the same resident population size as reported on 5/17/2020.
Individuals were classified as a resident or employee of an LTCF based on response to DHEC case reports, which was then verified with DHEC for each LTCF. Individuals who did not report residence in an LTCF were considered community-dwelling. Demographic and health-related information including age, gender, race, pre-existing conditions, death, and hospitalization were collected by SCION as part of mandatory COVID reporting.
Data were expressed as mean ± SD, median, or percentages, as appropriate. COVID-19 incidence rates and case fatality rates were plotted over time. Mean values and percentages were compared between those in the community, LTC residents, and staff. A Kaplan-Meier survival plot was used to estimate the survival function of COVID-19; a log-rank test was used to test for significance. COVID-19 case fatality rates were estimated adjusting for age, gender, race, neurological disease/neurodevelopmental disorder, diabetes, stroke, cardiovascular, COPD, asthma, chronic liver disease, and immunosuppressive condition using Cox proportional hazards models. Statistical analyses were performed using SAS (Statistical Analysis System) software version 9.4 (SAS Institute, Cary, NC, USA). P values < 0.05 were considered statistically significant.
Results
Between 3/15/2020 and 1/2/2021, 54,514 cases of COVID-19 were identified among older adults in SC (Table 1 ). Of these, 86.5% (n = 47,148) were in the community, while 13.5% (n = 7366) resided in a LTCF. Compared to older adults in the community, LTCF residents were older, more likely to be female, white, and report more of pre-existing conditions. LTCF residents with COVID-19 were significantly more likely to be hospitalized (26.5% vs. 14.9%) compared to older adults living in the community. Table 2 displays descriptive statistics for LTCF staff and adults in the general population (ie, not employed by LTCF). Between 3/15/2020 and 1/2/2021, 6877 cases of COVID-19 were identified among LTCF staff and 301,036 among adults in the general population. LTCF staff were more likely to be female, black, and to have fewer chronic health conditions compared to the general population.
Table 1.
Descriptive Statistics by Residential Status (LTCF and Community Dwelling)
| Variable | LTCF (n = 7366) | Community Dwelling (n = 47,148) | P-value | |
|---|---|---|---|---|
| Gender | Female | 64.8% (4640) | 54.1% (24,444) | P < .001 |
| Age | 81.8 (9.1) | 73.8 (7.2) | P < .001 | |
| Race | P < .001 | |||
| White | 58.1% (3838) | 62.2% (25,831) | ||
| Black | 26.0% (1718) | 22.6% (9374) | ||
| Asian, American Indian Alaskan Native, Native Hawaiian Pacific Islander | 0.3% (18) | 0.6% (265) | ||
| Other | 5.7% (379) | 7.2% (3006) | ||
| Unknown | 9.9% (657) | 7.4% (3066) | ||
| Neurologic, Neurodevelopmental/intellectual disability | P < .001 | |||
| Yes | 49.5% (1933) | 7.1% (1275) | ||
| Cardiovascular disease | P < .001 | |||
| Yes | 69.2% (2862) | 49.6% (9449) | ||
| Congestive heart failure | P < .001 | |||
| Yes | 12.7% (358) | 7.2% (1244) | ||
| COPD, Bronchitis, or Emphysema | P < .001 | |||
| Yes | 23.6% (853) | 15.5% (2867) | ||
| History of Kidney Disease | P < .001 | |||
| Yes | 21.0% (739) | 7.0% (1249) | ||
| Chronic Renal Failure | P < .001 | |||
| Yes | 14.9% (519) | 4.7% (859) | ||
| Chronic Liver Disease | P < .001 | |||
| Yes | 3.3% (123) | 1.8% (325) | ||
| Stroke | P < .001 | |||
| Yes | 16.3% (454) | 6.5% (1070) | ||
| Died | P < .001 | |||
| Yes | 23.9% (1760) | 6.0% (2839) | ||
| Hospitalization | P < .001 | |||
| Yes | 26.5% (1953) | 14.9% (7007) | ||
| Median Time from Illness Onset to Death | 13 | 16 | P < .001 | |
Note: Unknown responses were removed from calculations.
Table 2.
Descriptive Statistics by Employment Status (LTCF Staff and Non-LTCF Staff-general Population)
| Variable | Staff (n = 6877) | General Population (n = 301,036) | P-value | |
|---|---|---|---|---|
| Gender | Female | 82.1% (5451) | 54.3% (158,120) | P < .001 |
| Age | 42.5 (14.2) | 45.2 (18.3) | P < .001 | |
| Race | P < .001 | |||
| White | 36.2% (2385) | 54.2% (125,065) | ||
| Black | 51.6% (3401) | 23.8% (55,001) | ||
| Asian, American Indian Alaskan Native, Native Hawaiian Pacific Islander | 0.8% (54) | 1.1% (2612) | ||
| Other | 5.9% (388) | 11.2% (25,814) | ||
| Unknown | 5.4% (358) | 9.7% (22,482) | ||
| Neurologic, Neurodevelopmental/intellectual disability | P < .001 | |||
| Yes | 2.4% (60) | 4.5% (2633) | ||
| Cardiovascular disease | P < .001 | |||
| Yes | 31.2% (795) | 32.5% (19,969) | ||
| Congestive heart failure | P < .001 | |||
| Yes | 1.5% (33) | 3.6% (1988) | ||
| COPD, Bronchitis, or Emphysema | P < .001 | |||
| Yes | 7.3% (180) | 9.2% (5516) | ||
| History of Kidney Disease | P < .001 | |||
| Yes | 1.7% (41) | 3.7% (2164) | ||
| Chronic Renal Failure | P < .001 | |||
| Yes | 0.8% (21) | 2.5% (1515) | ||
| Chronic Liver Disease | P < .001 | |||
| Yes | 0.8% (21) | 1.4% (827) | ||
| Stroke | P < .001 | |||
| Yes | 1.0% (22) | 3.3% (1799) | ||
| Died | P < .001 | |||
| Yes | 0.6% (39) | 1.3% (3662) | ||
| Hospitalization | P < .001 | |||
| Yes | 3.1% (214) | 4.6% (12,437) | ||
| Mean Time from Illness Onset to Death | 19.3 | 18.8 | P = .429 | |
Note: Unknown responses were removed from calculations.
Residents
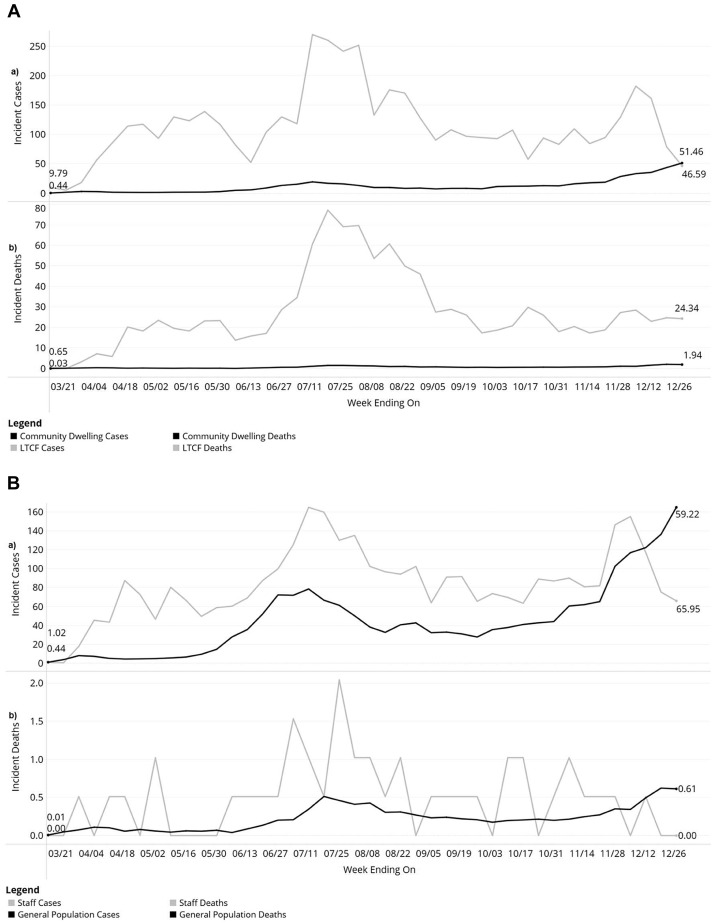
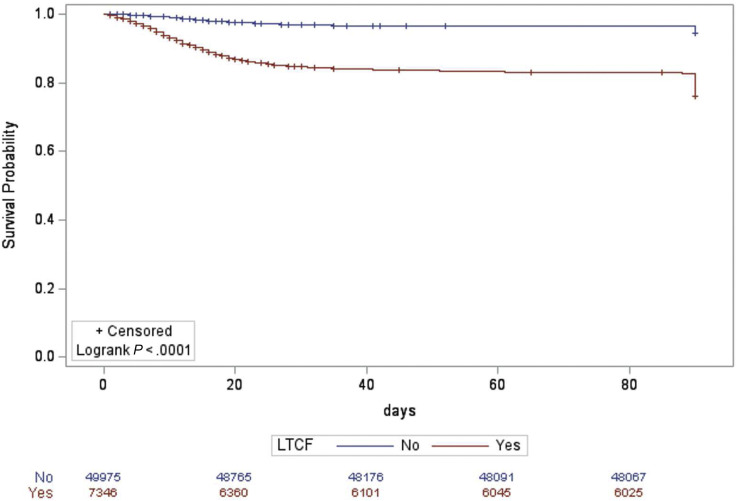
Figure 1A.a displays the weekly incidence of COVID-19 per 10,000 individuals, by LTCF status. From 3/15/2020 to 1/2/2021, the incidence per 10,000 was 51.0 for community-dwelling older adults and 484.7 for LTC residents. Throughout the study period, LTCF residents experienced greater incidence, but this difference diminished over time. Of all community-dwelling adults with COVID-19, 6.0% died, while 23.9% of those living in a LTCF died. Figure 1b displays deaths from COVID-19 per 10,000 individuals over time for community-dwellers and LTCF residents. From 3/15/2020 to 1/2/2021, 3.0 and 115.6 per 10,000 community-dwellers and LTCF residents, respectively, died from COVID-19. Supplemental Figure 1 shows that LTCF residents had a significantly lower probability of survival from COVID-19 compared to community-dwellers over the study period (log-rank: P < .001). After adjusting for age, gender, race, neurological disease/neurodevelopmental disorder, diabetes, stroke, cardiovascular, COPD, asthma, chronic liver disease, and immunosuppressive condition, LTCF residents with COVID-19 had 1.74 (HR = 1.74; CI: 1.59-1.90) times greater hazard of death.
Figure 1.
Long-Term Care Residents (A) and Long-Term Care Staff (B) trends over time for incident COVID-19 cases (a) and deaths (b) per 100,000 compared to the general population. Note: LTCF = Long-term care facility.
Supplemental Fig. 1.
Kaplan-Meier survival curve comparing survival probabilty of Long-Term Care Residents and Community-Dwelling older adults.
Staff
LTCF staff experienced more cases per 10,000 throughout the study period compared to the general SC population until the week ending on 12/26 (Figure 1B a.). Similar to COVID-19 incidence, the difference in the proportion of COVID deaths between LTCF and community-dwelling older adults decreased over time. LTCF staff had a similar proportion of deaths from COVID-19 compared with the community throughout the study period (Figure 1B b.). After adjusting for age, gender, race, neurological disease/neurodevelopmental disorder, diabetes, stroke, cardiovascular, COPD, asthma, chronic liver disease, and immunosuppressive condition, staff had 0.58 (HR = 0.58; CI: 0.39-0.88) times lower hazard of death compared to adults not working in LTCF.
Discussion
This is one of the first studies to compare longitudinal characteristics and outcomes of older adults with COVID-19 living in LTCF and LTCF staff to those in the community at the state level. LTCF residents in SC were almost twice as likely to be hospitalized and 1.74 times as likely to die from COVID-19 compared to those living in the community. The rates of COVID-19 infections and deaths for LTC residents decreased from the initial peak at the beginning of the pandemic. The opposite pattern was found for older adults in the community. Similarly, LTCF staff experienced greater rates of cases and death at the beginning of the pandemic compared to the general population but lower rates at the end of the study period. These results suggest that infection and death rates in LTCF are a key bellwether for the impact of COVID-19 among older adults in the general community, and that rates in these settings may be impacted by state and facility responses such as visitation policies and mask mandates.13 , 22
This study contributes to recent research on COVID-19, providing further evidence that older adults residing in LTCF are particularly vulnerable to COVID-19 due to increased spread and prevalence of pre-existing conditions. For instance, Machado et al. (2020) found that a majority (61.9%) of older adult deaths due to COVID-19 in Brazil happened in LTCFs.23 This result is consistent with the elevated hazard and proportion of death among LTCF residents in our study. LTCF residents made up approximately 38% (1760/4599) of COVID-related deaths among older adults, despite representing a small percentage of the total older adult population. Although our results are consistent with this previous study, it is unclear whether any differences are due to international variability in testing availability, policies, and recording of cases and deaths.24 This study extends these previous findings by tracking longitudinal changes in cases and mortality rates of LTC residents compared to those in the community. Differences between LTCF and community cases and deaths diminished over the study period, potentially reflecting implementation of more testing in LTCF or mitigation measures within LTCF settings, such as availability of personal protective equipment and quarantining. However, many state-and national-level policies and recommendations related to LTCF occurred months after the pandemic began,25 so the influence of broad policies on LTCF is unclear.
Results of the present study highlight the parallel, but commonly overlooked, spread of COVID-19 among LTCF staff. Like residents, COVID-19 incidence rates and case-fatality rates were higher than in the general community from early in the pandemic until December 2020. In contrast to LTCF residents, staff had significantly lower risk of death compared to those in the general population. This finding may be explained by better general health or access to healthcare among healthcare workers compared to the general population.26 Taken together, high infection suggest that the prevalence of COVID-19 in LTCF staff may play a role in driving resident infection rates.27 As staff may serve as a link for infection between LTCF residents and the community, these findings highlight the importance of clearly defining staff testing, quarantine, and protection policies. Furthermore, one explanation of the lower mortality risk among staff compared to comparable community-dwellers is the recommended increased screening of COVID-19 that LTC staff experience as a part of their occupation.28
This study has notable strengths, including use of the most comprehensive source of data on COVID-19 infection, symptoms, and mortality in the state of SC. Further, DHEC staff collected data on health and employment characteristics of cases, allowing comparisons of resident and staff rates. There are also limitations that should be considered when interpreting results. First, DHEC data may not contain all relevant characteristics that may influence differences in mortality and infection between LTCF residents. Case reports lacked information, for instance, on clinical manifestation of COVID-19 or from comprehensive geriatric assessments. Second, reporting of state LTCF resident populations was not mandated until May 17, 2020. Thus, calculations of infection and mortality rates before mandatory reporting assume a constant resident population over the first few months of the pandemic. Third, while the pattern of resident infection rates over time closely paralleled those of staff, it is unclear whether staff and resident cases were causally related or whether other factors such as regional fluctuations in infections led to this correlation.
Conclusion and Implications
These results have implications for LTCF policies and future pandemic planning. First, the narrowing of the gap between LTCF and community-wide infection and mortality rates over the study period suggests that early detection of COVID-19 in LTCFs could serve as a first indicator of disease spread in the greater community. Early identification and response to LTCF outbreaks may thus serve to slow broader spread of the disease. However, while LTCF residents were among the first to become eligible to receive vaccines, there are still notable barriers to vaccination even within LTCFs.29 Our results also indicate that policies and regulations addressing staff testing and protection may help to slow or prevent spread within facilities. Although many individual facilities have updated these practices during the pandemic, high rates of LTCF staff infections early in the pandemic suggest that establishing coordinated policies at the state and national level may help to stem future outbreaks. For example, by having mitigation measures, such as masks and social distance policies, in place for different types of viruses and ability to test individuals more quickly and frequently could help to identify cases early to provide medical attention earlier.
Acknowledgments
N/A.
Footnotes
The authors declare no conflicts of interest.
Supplementary Data
References
- 1.Kuy S., Tsai R., Bhatt J. Focusing on vulnerable populations during COVID-19. Acad Med. 2020;95(11):e2–e3. doi: 10.1097/ACM.0000000000003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanyaolu A., Okorie C., Marinkovic A. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020:1–8. doi: 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ssentongo P., Ssentongo A.E., Heilbrunn E.S. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS One. 2020;15(8):e0238215. doi: 10.1371/journal.pone.0238215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters S.A.E., MacMahon S., Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the UK biobank: Comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab. 2021;23(1):258–262. doi: 10.1111/dom.14199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain A., Mahawar K., Xia Z. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020 doi: 10.1016/j.orcp.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Rivera-Izquierdo M., del Carmen Valero-Ubierna M., R-delAmo J.L. Sociodemographic, clinical and laboratory factors on admission associated with COVID-19 mortality in hospitalized patients: A retrospective observational study. PLoS One. 2020;15(6):e0235107. doi: 10.1371/journal.pone.0235107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saragih I.D., Saragih I.S., Batubara S.O., Lin C.-J. Dementia as a mortality predictor among older adults with COVID-19: A systematic review and meta-analysis of observational study. Geriatr Nurs (Minneap) 2021 Mar 14. doi: 10.1016/j.gerinurse.2021.03.007. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aw D., Woodrow L., Ogliari G., Harwood R. Association of frailty with mortality in older inpatients with covid-19: A cohort study. Age Ageing. 2020;49(6):915–922. doi: 10.1093/ageing/afaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonanad C., Garcia-Blas S., Tarazona-Santabalbina F. The effect of age on mortality in patients with COVID-19: A meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020;21(7):915–918. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore K.L., Boscardin W.J., Steinman M.A., Schwartz J.B. Patterns of chronic co-morbid medical conditions in older residents of U.S. Nursing homes: Differences between the sexes and across the agespan. J Nutr Health Aging. 2014;18(4):429–436. doi: 10.1007/s12603-014-0001-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sepulveda E.R., Stall N.M., Sinha S.K. A comparison of COVID-19 mortality rates among long-term care residents in 12 OECD Countries. J Am Med Dir Assoc. 2020;21(11):1572–1574.e3. doi: 10.1016/j.jamda.2020.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollock A.M., Lancaster J. Asymptomatic transmission of covid-19. BMJ. 2020 371;m4851. [Google Scholar]
- 13.Bedford J., Enria D., Giesecke J. COVID-19: Towards controlling of a pandemic. Lancet (London, England) 2020;395(10229):1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson D.-C., Barbu M.-G., Beiu C. The Impact of COVID-19 Pandemic on Long-Term Care Facilities Worldwide: An Overview on International Issues. Biomed Res Int. 2020;2020:8870249. doi: 10.1155/2020/8870249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pillemer K., Subramanian L., Hupert N. The importance of long-term care populations in Models of COVID-19. JAMA. 2020;324(1):25–26. doi: 10.1001/jama.2020.9540. [DOI] [PubMed] [Google Scholar]
- 16.Ouslander J.G., Grabowski D.C. COVID-19 in nursing homes: Calming the Perfect Storm. J Am Geriatr Soc. 2020;68(10):2153–2162. doi: 10.1111/jgs.16784. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Infection control for nursing homes. Published 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html. Accessed April 22, 2021.
- 18.Lee R.M., Draper M., Lee S. Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. J Couns Psychol. 2001;48(3):310–318. [Google Scholar]
- 19.Quan N.G., Lohman M.C., Resciniti N.V., Friedman D.B. A systematic review of interventions for loneliness among older adults living in long-term care facilities. Aging Ment Heal. 2020;24:1945–1955. doi: 10.1080/13607863.2019.1673311. [DOI] [PubMed] [Google Scholar]
- 20.Lan C.-C., Tsai S.-J., Huang C.-C. Functional Connectivity Density Mapping of depressive symptoms and loneliness in non-Demented elderly Male. Front Aging Neurosci. 2016;7:251. doi: 10.3389/fnagi.2015.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) 2020 interim case definition. Available at: https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/08/05/. Published 2020. Accessed April 22, 2021.
- 22.Douglas M., Katikireddi S.V., Taulbut M. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Machado C.J., Pereira C.C. de A., Viana B. de M. Estimates of the impact of COVID-19 on mortality of institutionalized elderly in Brazil. Cien Saude Colet. 2020;25(9):3437–3444. doi: 10.1590/1413-81232020259.14552020. [DOI] [PubMed] [Google Scholar]
- 24.Comas-Herrera A., Zalakaín J., Lemmon E. Mortality associated with COVID-19 in care homes: International evidence. Artic LTCcovid org, Int long-term care policy Network. CPEC-LSE. June 26, 2020 [Google Scholar]
- 25.Chen A.T., Ryskina K.L., Jung H.-Y. Long-term care, residential facilities, and COVID-19: An Overview of federal and state policy responses. J Am Med Dir Assoc. 2020;21(9):1186–1190. doi: 10.1016/j.jamda.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helfand B.K.I., Mukamal K.J. Healthcare and Lifestyle practices of healthcare workers: Do healthcare workers practice what They Preach? JAMA Intern Med. 2013;173(3):242–244. doi: 10.1001/2013.jamainternmed.1039. [DOI] [PubMed] [Google Scholar]
- 27.Shi S.M., Bakaev I., Chen H. Risk factors, Presentation, and Course of coronavirus disease 2019 in a Large, Academic long-term care facility. J Am Med Dir Assoc. 2020;21(10):1378–1383.e1. doi: 10.1016/j.jamda.2020.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Society A.G. American geriatrics Society policy Brief: COVID-19 and nursing homes. J Am Geriatr Soc. 2020;68(5):908–911. doi: 10.1111/jgs.16477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jain V., Schwarz L., Lorgelly P. A Rapid review of COVID-19 vaccine Prioritization in the U.S.: Alignment between federal guidance and state practice. Int J Environ Res Public Heal. 2021;18:3483. doi: 10.3390/ijerph18073483. [DOI] [PMC free article] [PubMed] [Google Scholar]