Abstract
Background
Sepsis is the leading cause of death in critically ill patients, and the prevention of which requires precise outcome prediction and early intervention. We evaluated the prognostic prediction value of serum thioredoxin-1 (Trx-1) as an anti-inflammatory factor in patients with sepsis.
Methods
As a prospective study, patients with sepsis admitted to the intensive care unit (ICU) of our hospital during 2020 were recruited. Medical history collection, sequential organ failure assessment (ΔSOFA), and laboratory tests were performed within 24 h of admission. Serum levels of Trx-1 and other inflammatory biomarkers were detected with samples dynamically collected before, during, and after septic shock. Patients were categorized as survivors and non-survivors according to survival status on day 28. Correlation between Trx-1 and other sepsis-associated parameters as well as the correlation of Trx-1 and other sepsis-associated parameters with 28-day mortality were evaluated. Prognostic factors were identified by Cox regression analyses.
Results
A total of 187 patients were recruited. Serum Trx-1 level was positively correlated with inflammatory factors (interleukin-6, C-reactive protein, procalcitonin) and index of sepsis severity (ΔSOFA score, partial pressure of oxygen/fraction of inspired oxygen), all of which were significantly higher in non-survivors than survivors. While Trx-1 level at different timepoints and its evolution over time significantly differed between survivors and non-survivors, the initial Trx-1 level outperformed the other parameters in predicting 28-day survival. With 38.27 ng/mL as the cutoff value, serum Trx-1 predicted 28-day survival with optimal sensitivity and specificity.
Conclusion
Early increases in serum levels of Trx-1 can predict 28-day mortality in sepsis patients in the ICU.
Keywords: thioredoxin-1, prognosis, sepsis, mortality
Introduction
Sepsis is defined as a systematically dysregulated inflammatory response triggered by microbial infection. Characterized by acute onset and rapid progression, multiple organ damage and septic shock can rapidly develop in patients with sepsis when infection and the inflammatory response get out of control.1,2 As a major cause of intensive care unit (ICU) admission and the leading cause of death worldwide,1 sepsis remains a serious threat to human health and imposes a heavy burden on the health care system. According to global data, the mortality rate is up to 10% in patients with sepsis, and is even as high as 40% when septic shock develops.2 A cross-sectional study in China reported a mortality rate of 20.6% in patients hospitalized with sepsis.3
Early intervention and appropriate therapeutic strategies such as empirical antibiotic administration and fluid management are of paramount importance in reducing sepsis mortality, which requires early recognition of the disease and precise prediction of progression.4 Thus, there is a need to identify biomarkers that can accurately predict the trajectory of disease progression even at the very beginning of disease onset. Multiple biomarkers have been evaluated or applied to clinical practice for sepsis as diagnostic or prognostic markers. Characterized by an overwhelming inflammatory response, biomarkers of the inflammatory response such as interleukin-6 (IL-6), IL-1β, tumor-necrosis factor-α (TNF-α), procalcitonin (PCT), and C-reactive protein (CRP) were first evaluated in sepsis for the purpose of diagnosis or prognostic prediction.5,6 All of these biomarkers are significantly increased in patients, although their prognostic prediction value is not satisfactory.7 Both CRP and PCT are widely applied in the clinic to identify patients with infection and sepsis, but they are less desirable for predicting the outcome of sepsis patients.8–11 To facilitate real-time monitoring and optimize the management of sepsis, biomarkers that convey prognostic information with their dynamic changes are also urgently needed.
As a feedback response to the overwhelming inflammation during sepsis, anti-inflammatory factors are also elevated and play an equally important role especially during the early onset of sepsis.12 The dynamic interaction between pro-inflammatory and anti-inflammatory effects ultimately decides the trajectory of sepsis progression, indicating that anti-inflammatory biomarkers may also be promising for predicting the outcome of sepsis.13,14 Studies on the prognostic value of other anti-inflammatory cytokines for sepsis remain scarce. Thioredoxin-1 (Trx-1) was first identified as an antioxidant that serves as an electron donor for enzymes such as ribonucleotide reductase.15 Further studies have revealed its role in a variety of biological processes including the control of cell growth or apoptosis and inflammation regulation.16–18 The extracellular level of Trx-1 is markedly increased in response to the inflammatory response or oxidative stress.14,19 Both inflammation and oxidative stress are the major pathophysiological players of sepsis during its evolution,20 which signifies the potential of Trx-1 as a prognostic marker in sepsis. Leaver et al21 first reported that serum levels of Trx-1 are significantly increased in sepsis patients and play a role in inhibiting the inflammatory response. Utilizing a mouse model of sepsis caused by colon perforation, Chen22 demonstrated that Trx-1 can improve the survival of septic mice by decreasing the release of inflammatory cytokines such as IL-1β and TNF-α.22 However, no study has evaluated the prognostic role of Trx-1 in patients with sepsis.
To determine whether Trx-1 can serve as a prognostic biomarker of sepsis and if the dynamic changes in Trx-1 level correlate with disease severity or change in disease progression, we conducted this single-center prospective study in patients who were diagnosed with sepsis and hospitalized in our hospital.
Patients and Methods
Patients
This was a prospective single-center study, which recruited 187 consecutive cases diagnosed with sepsis and hospitalized in the Department of Critical Care Medicine of the Changsha Traditional Chinese Medicine Hospital (Hunan, China) between January and December 2020. All patients met the diagnostic criteria for sepsis (version 3), which defines sepsis as organ dysfunction caused by a dysregulated response to microbial infection, with sequential organ failure assessment (ΔSOFA) score ≥2 considered to be organ dysfunction.2 Patients with the following conditions were excluded from the study: malignant disease, antibiotic administration within 2 weeks before admission, and readmission to the ICU during the same hospitalization period. Medical history collection, measurement of vital signs, ΔSOFA, routine blood tests, arterial blood gas analyses, and blood chemistry tests were performed within 24 h of admission. All of the enrolled patients received standard treatment during their stay in the ICU. All eligible patients were categorized into two groups according to their survival status within 28 days of diagnosis: the survivor group included patients who survived 28 days after initial diagnosis, and the non-survivor group included patients who died within 28 days after diagnosis. This study was conducted in accordance with Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Changsha Traditional Chinese Medicine Hospital (No.2018003). Informed written consent was obtained from the patients or their relatives.
Dynamic Evaluation of Biomarkers and ΔSOFA Score
Blood samples were dynamically collected during the entire disease course and stored at −80°C. Specifically, samples were collected at three different timepoints: 1) within 24 h of admission in ICU 2) during septic shock (for patients who did not develop septic shock, the second timepoint was defined as 5–7 days after admission instead); 3) during the convalescence of septic shock (survival group) or 1–3 days before death caused by sepsis (non-survival group). Trx-1 and IL-6 were detected by the enzyme-linked immunosorbent assay (ELISA), with an intra-assay coefficient <10% and 2.1%, and the inter-assay coefficient of variation <12% and 2.4%. PCT, CRP were detected by chemiluminescent immunoassay, and lactate was detected by spectrophotometry. ΔSOFA was also performed at the time point in alignment with that of blood sampling. We also quantified the index of changes for the abovementioned makers according to the following algorithm: first change index = level obtained at the second timepoint minus level obtained at the first timepoint divided by level obtained at the first timepoint; second change index = level obtained at the third timepoint minus level obtained at second timepoint divided by level obtained at the second timepoint; third change index = level obtained at the third timepoint minus level obtained at the first timepoint divided by level obtained at the first timepoint.
Statistical Analyses
SPSS Statistics version 24.0 for Windows (SPSS Inc., Chicago, IL, USA) and MedCalc statistical software version 19.0 (MedCalc Software Ltd, Belgium) were used for the statistical analyses. Normally distributed continuous variables are presented as the mean ± standard deviation, and between–group differences were assessed using the independent t-test. Non-normally distributed data are expressed as the median and interquartile range, and between–group differences were assessed by the Mann–Whitney U-test. Pearson’s correlation analyses were used to assess the correlation of serum Trx-1 level with other conventional markers associated with sepsis such as IL-6, lactate, CRP, PCT, ΔSOFA score, and ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FIO2). Cox multivariate models were used to establish the independent prognostic value of circulating biomarkers and ΔSOFA detected at different timepoints and their changes during the disease course. Receiver operating characteristic curve analysis was performed to evaluate the sensitivity and specificity of Trx-1 detected at admission as a predictor for 28-day survival. The optimal cut-off value of Trx-1 was derived from Youden’s index. Patients were categorized as high Trx-1 group and low Trx-1 group based on the Trx-1 level detected within 24 h of admission and the optimal cut-off value. Kaplan–Meier curves were constructed by using Trx-1 groups as strata and compared by the Log rank test. ROCs analyses were performed to analyze other parameters (ΔSOFA, CRP, PCT and IL-6) detected within 24 h of admission with 28-day mortality. Pairwise comparisons of ROC results were performed to compare the predicting power of different parameters. P < 0.05 was considered statistically significant.
Results
Comparison of Biomarkers Derived from Different Timepoints Between Survivors and Non-Survivors
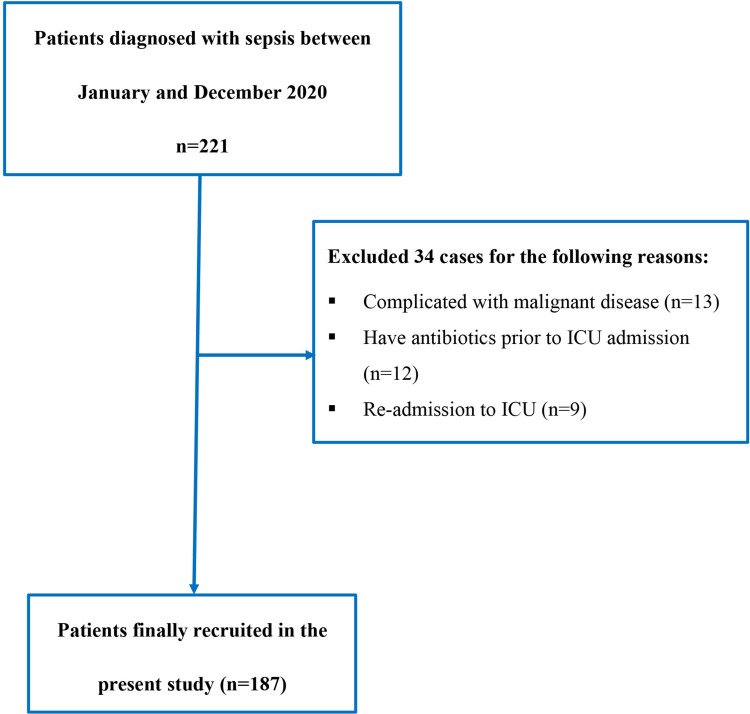
A total 221 patients with sepsis were identified during the primary screening. We further excluded 34 cases for the following reasons: complications of malignant diseases (n=13), taken antibiotics prior to ICU admission (n=12), and re-admitted to the ICU (n=9) (Figure 1). Among the 187 cases that were finally recruited, 144 patients survived more than 28 days after admission and thus were categorized as the survivor group, whereas 43 patients died of sepsis complications within 28 days of diagnosis and thus were categorized as non-survivors. Baseline characteristics obtained within 24 h of admission were compared between survivors and non-survivors (Table 1). Non-survivors differed from survivors by having significantly higher serum levels of Trx-1 (P < 0.001), lactate (P < 0.001), PCT (P < 0.001), CRP (P < 0.001), IL-6 (P < 0.001), creatine (Scr) (P=0.002), and total bilirubin (TBIL) (P=0.029); and lower median arterial pressure (MAP) (P < 0.001), heart rate (HR) (P=0.033), respiratory rate (RR) (P=0.048), ΔSOFA score (P < 0.001), and platelet (PLT) (P=0.025), PaO2/FIO2 (P=0.001), and Glasgow Coma Score (GCS) (P < 0.001). No difference was observed for white blood cells (WBCs) and hematocrit (HCT %) (P > 0.05). We further evaluated the between–group difference of Trx-1 and conventional sepsis biomarkers (eg, lactate, PCT, CRP, IL6 and ΔSOFA detected at later timepoints; Tables 2 and 3). All of them were significantly higher in non-survivors compared to survivors (P < 0.001), whether they were detected during septic shock or after the peak onset of sepsis (during the convalescence of septic shock for survivors or 1–3 days before death for non-survivors).
Figure 1.
Diagram of patient selection.
Table 1.
Comparison of Baseline Clinical Characteristics Between Survivors and Non-Survivors
| Survivors | Non-Survivors | P value | |
|---|---|---|---|
| Age (years) | 68±13 | 65±16 | 0.172 |
| Gender (male/female) | 24/19 | 109/35 | 0.012 |
| Coronary heart disease | 13 (30.2%) | 45 (31.3%) | 0.899 |
| Hypertension | 11 (25.6%) | 38 (26.4%) | 0.916 |
| Type 2 diabetes | 5 (11.6%) | 15 (10.4%) | 0.822 |
| Chronic renal failure | 4 (9.3%) | 11 (7.8%) | 0.725 |
| COPD | 8 (18.1%) | 23 (16.0%) | 0.684 |
| Length of ICU stay (days) | 6 (2~22) | 8 (3~21) | 0.025 |
| Survival days | 10 (2~22) | 28 | 0.000 |
| Trx-1 (ng/mL) | 15.2 (2.3–789.5) | 382.5 (7.5–1732.5) | 0.000 |
| Lac (mmol/L) | 2.2 (0.5–11.0) | 3.2 (0.9–18) | 0.000 |
| PCT (ng/mL) | 4.10 (0.40–200.00) | 13.9 (0.4–200.0) | 0.000 |
| CRP (mg/mL) | 99.40 (7.48–200.0) | 127.6 (18.6–468.0) | 0.000 |
| IL-6 (pg/mL) | 74.6 (2.9–754.3) | 376.3 (13.4–912.1) | 0.000 |
| ΔSOFA | 6 (2–18) | 11 (3–15) | 0.000 |
| HR (beats/min) | 101±22 | 110±33 | 0.033 |
| RR (beats/min) | 24±6 | 24 (12–40) | 0.048 |
| MAP (mmHg) | 84±18 | 70±17 | 0.000 |
| Temperature | 37.5±1.0 | 37.8±1.3 | 0.000 |
| WBCs (109) | 15.1±8.0 | 13.5±6.4 | 0.222 |
| HCT% | 32.7±9.1 | 31.1±7.0 | 0.295 |
| PLT (109) | 172 (21.0–527.0) | 130.0 (17.0–364.0) | 0.025 |
| Scr (umol/L) | 96.4 (33.7–507.6) | 144.0 (44.9–1477.9) | 0.002 |
| TBIL (mmol/L) | 17 (3.1–122.0) | 19.6 (4.6–124.7) | 0.029 |
| PaO2/FIO2 (mmHg) | 187.8 (44.8–675.0) | 150.2 (63.3–417.1) | 0.001 |
| GCS | 12 (3–15) | 9 (3–15) | 0.000 |
Abbreviations: Trx-1, thioredoxin; Lac, lactate; PCT, procalcitonin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score; HR, heart rate; RR, respiratory rate; MAP, mean artery pressure; WBC, white blood cells; PLT, platelet; HCT, hematocrit; TBIL, total bilirubin; GCS, Glasgow Coma Score.
Table 2.
Comparison of Biomarkers Detected at the Second Timepoint (During Septic Shock or 5–7 Days After ICU Admission) Between Survivors and Non-Survivors
| Survivors | Non-Survivors | P value | |
|---|---|---|---|
| Trx-1 (ng/mL) | 10.6 (1.8–235.7) | 684.4 (15.0–1896.7) | 0.000 |
| Lac (mmol/L) | 1.6 (0.4–7.6) | 5.4 (0.8–19.2) | 0.000 |
| PCT (ng/mL) | 2.17 (0.03–128.00) | 18.7 (1.2–232.3) | 0.000 |
| CRP (mg/mL) | 61.0 (5.6–216.5) | 139.6 (28.3–496.5) | 0.000 |
| IL-6 (pg/mL) | 43.6 (1.5–562.3) | 427.4 (13.4–912.1) | 0.000 |
| ΔSOFA | 4 (1–12) | 16 (4–23) | 0.000 |
Abbreviations: Trx-1, thioredoxin; Lac, lactate; PCT, procalcitonin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score.
Table 3.
Comparison of Biomarkers Detected at the Third Timepoint (During the Convalescence of Septic Shock or 1–3 Days Before Death) Between Survivors and Non-Survivors
| Survivors | Non-Survivors | P value | |
|---|---|---|---|
| Trx-1 (ng/mL) | 6.8 (1.2~32.2) | 864.1 (21.2–1987.7) | 0.000 |
| Lac (mmol/L) | 1.2 (0.2~4.0) | 6.5 (1.9–22.2) | 0.000 |
| PCT (ng/mL) | 1.11 (0.01~78.40) | 20.5 (1.1–242.3) | 0.000 |
| CRP (mg/mL) | 22.2 (3.3~126.3) | 152.5 (21.2–312.5) | 0.000 |
| IL-6 (pg/mL) | 22.8 (1.3–276.2) | 443.2 (28.1–1342.5) | 0.000 |
| ΔSOFA | 2 (0~9) | 18 (3–24) | 0.000 |
Abbreviations: Trx-1, thioredoxin; Lac, lactate; PCT, procalcitonin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score.
Correlation Between Trx-1 and Other Biomarkers
Pearson’s correlation analysis was performed, which showed that serum level of Trx-1 was significantly and positively correlated with CRP, PCT, IL-6, lactate, ΔSOFA score, and PaO2/FIO2 (P < 0.01) (Table 4).
Table 4.
Correlation Between Trx-1 and Other Biomarkers
| R (Correlation Coefficient) | P | |
|---|---|---|
| CRP | 0.182 | 0.000 |
| PCT | 0.215 | 0.000 |
| IL-6 | 0.359 | 0.000 |
| LAC | 0.268 | 0.000 |
| ΔSOFA | 0.293 | 0.000 |
| PaO2/FIO2 | 0.141 | 0.005 |
Abbreviations: PCT, procalcitonin; CRP, C-reactive protein; IL-6, interleukin-6; LAC, lactate; ΔSOFA, sequential organ failure assessment score.
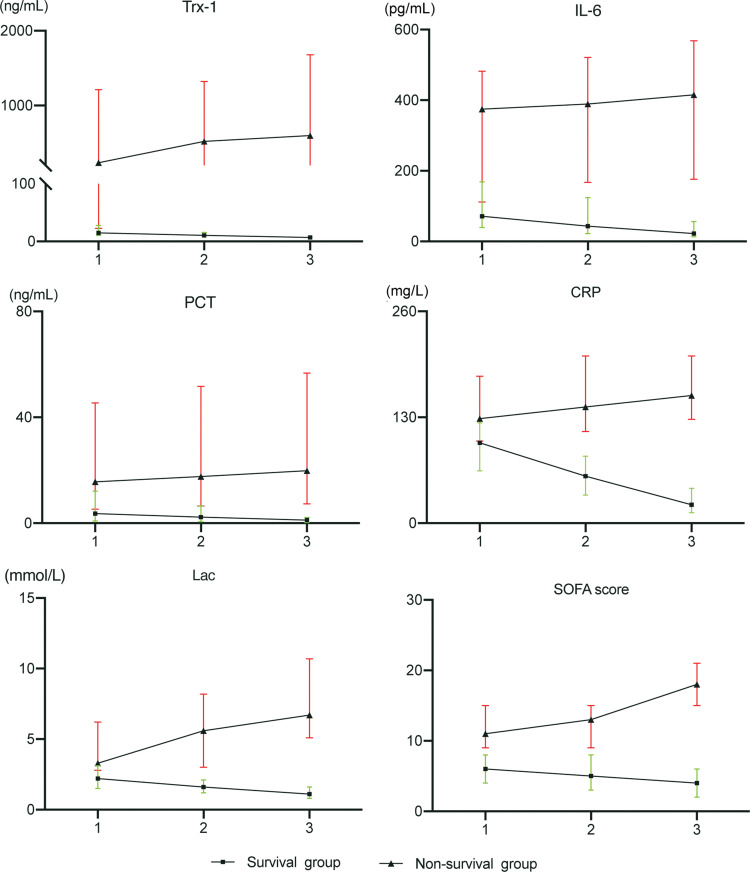
Evolution of Trx-1 During Hospitalization Differs Between Survivors and Non-Survivors
As shown above, the serum level of Trx-1 was significantly higher in non-survivors than in survivors, regardless of the detection timepoints. Next, we further evaluated how serum level of Trx-1 changes with time among survivors and non-survivors. As shown in Figure 2, Trx-1 level in survivors and non-survivors had the opposite evolving trend, with Trx-1 gradually decreasing in survivors but increasing in non-survivors.
Figure 2.
Line plot presenting changes in the levels of different parameters at three different time points among survivors or non-survivors. The definition of different time points: 1, within 24 h of admission in ICU; 2, during septic shock (for patients who did not develop septic shock, the second timepoint was defined as 5–7 days after admission instead); 3, during the convalescence of septic shock (survival group) or 1–3 days before death caused by sepsis (non-survival group).
Identification of Independent Predictors of 28-Day Survival for Sepsis
To identify biomarkers with independent prognostic value in predicting the 28-day mortality for sepsis, multivariate Cox regression analyses were performed for potential markers detected at different timepoints, as well as the index for their changes during hospitalization. We first included the markers that were available within 24 h of admission such as the serum level of Trx-1, CRP, PCT, IL-6, lactate, and ΔSOFA score in the multivariate analyses, which showed that Trx-1 (P < 0.001), ΔSOFA score (P < 0.001), CRP (P < 0.001), and IL-6 (P=0.047) had independent prognostic value (Table 5). Similar multivariate analyses were performed with analyzed variates extended to markers available at the second timepoint (during septic shock), which included biomarkers detected at the first and second timepoints, as well as the index of their first change. The identified independent predictors included Trx-1 detected at the first timepoint (P < 0.001), ΔSOFA score at the second timepoint (P < 0.001), CRP detected at the second timepoint (P < 0.001), first change of index of IL-6 (P=0.001), and first change of index of LAC (P=0.007) (more details are shown in Table 6). Similarly, we performed Cox regression multivariate analyses again and integrated all of the parameters available at the third timepoint, which included biomarkers detected at the first/second/third timepoints and the index of their first/second/third changes. As shown in Table 7, parameters conveying an independent prediction value included Trx-1 level at the first timepoint (P=0.003), ΔSOFA score at the third timepoint (P < 0.001), first change index of IL-6 (P=0.006), and second change index of ΔSOFA score (P=0.001).
Table 5.
Prognostic Significance of Parameters Detected at Baseline
| Parameters | P | EXP(β) | 95% CI |
|---|---|---|---|
| Trx-1 | 0.000 | 1.002 | 1.001–1.002 |
| ΔSOFA | 0.000 | 1.201 | 1.102–1.308 |
| CRP | 0.000 | 1.008 | 1.003–1.012 |
| IL-6 | 0.047 | 1.001 | 1.000–1.003 |
| PCT | 0.324 | _ | _ |
Abbreviations: Trx-1, thioredoxin; CRP, C-reactive protein; IL-6, interleukin-6; PCT, procalcitonin; ΔSOFA, sequential organ failure assessment score.
Table 6.
Parameters Available at the Second Timepoint with Independent Prognostic Value
| Parameters | P | EXP(β) | 95% CI |
|---|---|---|---|
| Trx-1 at first timepoint | 0.000 | 1.001 | 1.001–1.002 |
| ΔSOFA at second timepoint | 0.000 | 1.237 | 1.153–1.327 |
| CRP at second timepoint | 0.000 | 1.008 | 1.004–1.013 |
| First change of IL-6 | 0.001 | 1.279 | 1.111–1.471 |
| First change of LAC | 0.007 | 1.829 | 1.181–2.831 |
Note: First change index = level obtained at the second timepoint minus level obtained at the first timepoint divided by level obtained at the first timepoint.
Abbreviations: Trx-1, thioredoxin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score.
Table 7.
Parameters Available at the Third Timepoint with an Independent Prognostic Value
| Parameters | P | EXP(β) | 95% CI |
|---|---|---|---|
| Trx-1 at first timepoint | 0.003 | 1.001 | 1.001–1.002 |
| ΔSOFA at third timepoint | 0.000 | 1.159 | 1.092–1.230 |
| CRP at second timepoint | 0.000 | 1.008 | 1.004–1.013 |
| First change of IL-6 | 0.006 | 1.203 | 1.054–1.373 |
| Second change of ΔSOFA | 0.001 | 4.994 | 2.000–12.469 |
Notes: First change index = level obtained at the second timepoint minus level obtained at the first timepoint divided by level obtained at the first timepoint; second change index = level obtained at the third timepoint minus level obtained at second timepoint divided by level obtained at the second timepoint.
Abbreviations: Trx-1, thioredoxin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score.
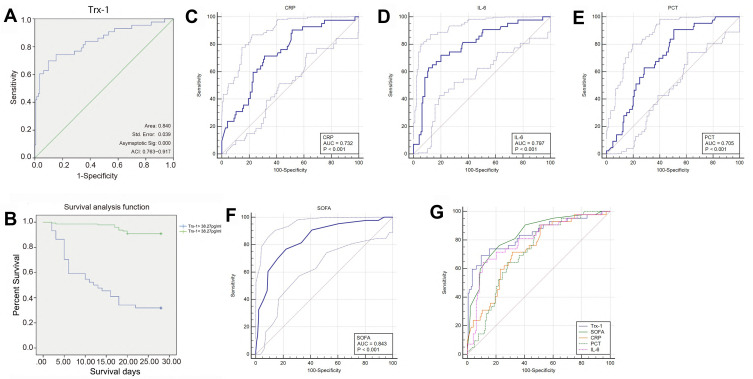
Explore the Early Optimal Serum Levels of Trx-1 to Predict 28-Day Mortality in Septic Patients
As aforementioned, Trx-1 level detected at admission was an independent prognostic predictor and outperformed Trx-1 level detected at later timepoints as well as its changing indexes in predicting 28-day mortality for sepsis. To further evaluate the prediction power of Trx-1 and other parameters (ΔSOFA, CRP, PCT and IL-6) detected within 24 h of admission, ROC analyses were performed to analyze their relationship with 28-day mortality (Figure 3). The area under the ROC curve for the ability of Trx-1, ΔSOFA, CRP, PCT, and IL-6 to predict 28-day mortality for sepsis was 0.837, 0.84, 0.731, 0.713, and 0.795, respectively (Table 8). Pairwise comparison of the ROC results was performed to compare the predicting power of different parameters. As shown in Table 9, Trx-1 significantly outperformed PCT and CRP in predicting the 28-day mortality of sepsis patients (P=0.046 for Trx-1~ CRP; P=0.007 for Trx-1 ~ PCT), and so was ΔSOFA (P=0.041 for ΔSOFA ~ CRP; P=0.0031 for ΔSOFA ~ PCT). However, the predicting power of Trx-1, ΔSOFA, and IL-6 was comparable with one another, with P > 0.05 for all pairwise comparisons (Table 9). The optimal cutoff was 38.27 ng/mL for Trx-1 to better discriminate survivors from non-survivors, with a sensitivity and specificity of 70.0% and 90.2%, respectively, a positive and negative predictive value of 68.2% and 90.8%, and a Youden index of 0.60. The Kaplan–Meier curve showed that the survival rate in patients with Trx-1 level <38.27 ng/mL was significantly higher than that in those with levels >38.27 ng/mL (P < 0.001) by Log rank test (Figure 3B).
Figure 3.
ROC analyses of different biomarkers. (A, C-F) ROC curve and corresponding parameters of TRx-1 (A), CRP (C), IL-6 (D), PCT (E), SOFA (F); (B) Kaplan-Meier survival curve of patients with Trx-1 level > 38.27 ng/mL (green line) and those with Trx-1 level < 38.27 ng/mL (blue line); (G) combined ROC curves of all biomarkers.
Abbreviations: ACI, area confidence interval; Asymptotic Sig, statistical significance (P value).
Table 8.
Summary of ROC Analysis for Each Parameter
| Trx-1 | ΔSOFA | CRP | PCT | IL-6 | |
|---|---|---|---|---|---|
| AUC | 0.837 | 0.840 | 0.731 | 0.713 | 0.795 |
| SE | 0.040 | 0.035 | 0.042 | 0.040 | 0.041 |
| 95% CI | 0.776~0.887 | 0.779~0.890 | 0.661~0.793 | 0.642~0.777 | 0.730~0.851 |
| Cut-off value | 38.27ng/mL | 8 scores | 107.6mg/L | 3.70ng/mL | 198.5pg/mL |
| Sensitivity | 70.00% | 76.70% | 71.40% | 90.70% | 72.10% |
| Specificity | 90.20% | 77.80% | 68.90% | 49.30% | 80.00% |
| Positive predictive value | 68.20% | 50.80% | 40.00% | 34.80% | 51.70% |
| Negative predictive value | 90.80% | 91.80% | 89.20% | 94.70% | 90.60% |
| Youden index | 0.60 | 0.55 | 0.40 | 0.40 | 0.52 |
Abbreviations: Trx-1, thioredoxin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score; AUC, area under curve; SE, standard error; 95% CI, 95% confidence interval.
Table 9.
Pairwise Comparison of ROC Curves Between Different Parameters
| Pairwise comparison | DBA | SE | 95% CI | P value |
|---|---|---|---|---|
| Trx-1 ~ ΔSOFA | 0.003 | 0.039 | −0.074–0.081 | 0.933 |
| Trx-1 ~ CRP | 0.106 | 0.053 | 0.001–0.210 | 0.046 |
| Trx-1 ~ PCT | 0.124 | 0.046 | 0.034–0.214 | 0.007 |
| Trx-1 ~ IL-6 | 0.042 | 0.046 | −0.049–0.132 | 0.368 |
| ΔSOFA ~ CRP | 0.109 | 0.053 | 0.0044–0.214 | 0.041 |
| ΔSOFA ~ PCT | 0.128 | 0.043 | 0.0429–0.212 | 0.003 |
| ΔSOFA ~ IL-6 | 0.045 | 0.042 | −0.038–0.129 | 0.292 |
| CRP ~ PCT | 0.018 | 0.049 | −0.078–0.115 | 0.711 |
| CRP ~ IL-6 | 0.064 | 0.046 | −0.027–0.156 | 0.170 |
| PCT ~ IL-6 | 0.003 | 0.039 | −0.075–0.081 | 0.933 |
Abbreviations: Trx-1, thioredoxin; CRP, C-reactive protein; IL-6, interleukin-6; ΔSOFA, sequential organ failure assessment score; DBA, difference between areas; SE, standard error; 95% CI, 95% confidence interval.
Discussion
In this study, we found that Trx-1 level was positively correlated with conventional markers such as CRP, PCT, IL6, lactate, and ΔSOFA score, all of which were significantly higher in non-survivors compared to survivors. Specifically, non-survivors demonstrated a significantly higher Trx-1 level compared to survivors at any timepoint, with Trx-1 level rising among non-survivors but gradually declining in survivors. Trx-1 level detected at admission was an independent prognostic predictor and outperformed many conventional biomarkers as well as Trx-1 level detected at later timepoints and its changing indexes in predicting 28-day mortality. The optimal cut-off value for early Trx-1 was 38.27ng/mL in predicting 28-day survival for patients with sepsis. To our knowledge, this is the first study to evaluate the prognostic significance of Trx-1 in patients with sepsis.
Trx-1 is well studied for its role in antioxidation, anti-inflammation, and anti-apoptosis and is associated with cardiovascular disease, inflammatory diseases, viral infection, and cancer.23–25 A previous study also reported its evaluation in sepsis patients, although its correlation with the outcome of sepsis has yet to be clarified. To the best of our knowledge, we first demonstrated that Trx-1 level was significantly elevated in non-survivors compared to survivors, regardless of whether detection at an early timepoint or at a later stage of sepsis.
Trx-1 is an anti-inflammatory factor, whose function is to inhibit the overwhelming inflammatory response during sepsis development and bring the immune response back to balance. Theoretically increased levels of serum Trx-1 should be associated with a favorable prognosis in sepsis. However, our study found that increased levels of serum Trx-1 predicted a poor outcome for sepsis patients, which could be explained by the following perspectives. Trx-1 level is positively correlated with inflammation, as shown by the positive correlation between Trx-1 and inflammatory biomarkers such as IL-6, CRP, and PCT as was shown in our study. As the interdependent force for the immune system, anti-inflammatory effects are initiated in response to and also in proportion to the effects of inflammation.26 One reason is that elevation of Trx-1 is an indicator of an uncontrolled inflammatory response, and thus is also an indicator of unfavorable disease outcome. Another reason is that the control of sepsis progression relies on the eradication of invaded pathogens, which in turn requires well-functioning immune response.4 Both overwhelming immune suppression and dysregulation of the immune response are unhelpful for the battle against infection,27 which is why overexpression of Trx-1 as an immune suppressant is a predictor of an unfavorable prognosis. Furthermore, Trx-1 plays a key role in redox regulation.28 Its elevation is also an indicator of the oxidant–antioxidant imbalance,29 which has been associated with the progression of sepsis.30,31
One of the highlights in the present study was the evaluation of the prognostic significance of the dynamic changes in the biomarkers. We found that Trx-1 level had the opposite trend of change during disease evolution, with Trx-1 level rising in non-survivors but gradually declining in survivors. The escalation of Trx-1 in non-survivors could be due to the imbalance between the anti-inflammatory and pro-inflammatory response, which kept exacerbating and went out of control. By contrast, Trx-1 level in survivors gradually returned to the physiological level as the inflammatory response was well controlled in the survivors. These findings indicate that the balance of anti-inflammatory and pro-inflammatory reactions is key to controlling the progression of sepsis.
To investigate the prognostic significance of Trx-1 in patients with sepsis, we evaluated its correlation with 28-day mortality in-terms of its serum level at different time points as well as its dynamic change during the disease course. We found that the evaluation of Trx-1 at any timepoint had predictive value with regard to 28-day mortality. Of note, Trx-1 level at each timepoint outperformed PCT in prognostic prediction as PCT was not involved in the COX equation as an independent predictor at any timepoint. The outstanding prognostic significance of Trx-1 could be attributed to its multiple biological roles as an anti-inflammatory factor and antioxidant among others.23,32 It was expected that the dynamic change in Trx-1 level is a better parameter in predicting outcome. However, the result was quite the opposite, with Trx-1 level at early timepoints demonstrating the optimal prognostic value. Trx-1 was not constitutively expressed unless in response to inflammation or an oxidant reaction.23 For sepsis patients with an unfavorable prognosis, the inflammatory response was overwhelming even at the early stage, accompanied by the significant evaluation of Trx-1. Trx-1 in non-survivors at an early stage was 25 times that of survivors. Although its level kept increased with disease progression in non-survivors, the changes were not as dramatic as the elevation at early stage. Also, its decline in survivors was even less conspicuous, with the level changing from 15.2 ng/mL to 10.6 ng/mL and to 6.8 ng/mL at the recovery stage. That might be the reason that Trx-1 at the early stage outperformed its dynamic change in predicting 28-day mortality.
Consistent with previous findings, conventional biomarkers such as PCT, CRP, IL-6, and ΔSOFA score also had significant prognostic value in our study. PCT has been proposed as a reliable diagnostic marker33 as well as indicator for therapeutic efficacy34 in patients with bacterial infection and sepsis. CRP is another biomarker for sepsis diagnosis and severity evaluation that is widely used in the clinic.35,36 Our study showed that both PCT and CRP were significantly elevated in non-survivors compared to survivors, although only CRP but not PCT was capable of being an independent predictor of 28-day survival. IL-6 is an inflammatory cytokine with excellent diagnostic and prognostic value for sepsis, especially in differentiating sepsis from non-infectious systemic inflammatory response syndrome.37,38 Consistently, we found that serum level of IL-6 detected at admission could independently predict the 28-day mortality of sepsis patients, indicating that it could be a promising early predictor of prognosis. ΔSOFA score is a widely used parameter for organ failure evaluation, the evaluation of which has been associated with the unfavorable outcome of sepsis patients.39,40 ΔSOFA score was also found to be an independent prognostic predictor for sepsis in our study, and its prediction was more reliable at the later stage. Lactate level as a widely recognized biomarker for sepsis development and progression41,42 was found to be associated with 28-day survival, with the dynamic elevation of lactate predicting an unfavorable outcome.
Even with these promising findings, the limitations of this study should be addressed. First, this was a single-center study with a relatively small sample size that precluded us from performing subgroup analyses according to infection organism, source of sepsis, etc. Also, we did not have long-term follow-up information on the patients and thus could not evaluate the prediction value of the biomarker in terms of long-term prognosis. Third, mechanistic analyses were not conducted in this study and the exact mechanism by which Trx-1 correlates with prognosis has yet to be evaluated. Further studies are needed to clarify whether the elevation in Trx-1 is just a consequence of an overwhelming inflammatory response, or if it also plays a role in exacerbating the process.
In conclusion, our study shows that Trx-1 is an early marker for predicting sepsis-associated mortality within 28 days. Our findings provided some basis for the applicability of Trx-1 as a biomarker for risk stratification and treatment guidance in clinical practice. Further study is needed to confirmed clinical indications for Trx-1 in large-scale, independent cohorts.
Funding Statement
This study was sponsored by the Natural Science Foundation of Hunan Province, China (No.2019JJ80051 and No.2019JJ80061).
Data Sharing Statement
Data will not be shared with a reason.
Ethics Approval and Consent to Participate
This study was conducted in accordance with Declaration of Helsinki. The study was approved by the Ethics Committee of Changsha of Traditional Chinese Medicine Hospital (No.2018003).
Consent for Publication
An informed consent form was obtained from all the patients or their guardians.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent JL. Sepsis and septic shock. Nat Rev Dis Primers. 2016;2:16045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou J, Tian H, Du X, et al. Population-based epidemiology of sepsis in a subdistrict of Beijing. Crit Care Med. 2017;45(7):1168–1176. doi: 10.1097/CCM.0000000000002414 [DOI] [PubMed] [Google Scholar]
- 4.Del Pozo JL. Stewardship in sepsis. Rev Esp Quimioter. 2019;32 Suppl 2(Suppl2):42–46. [PMC free article] [PubMed] [Google Scholar]
- 5.van Engelen TSR, Wiersinga WJ, Scicluna BP, van der Poll T. Biomarkers in sepsis. Crit Care Clin. 2018;34(1):139–152. doi: 10.1016/j.ccc.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 6.Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Critical Care. 2010;14(1):R15. doi: 10.1186/cc8872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ulusoy H, Kangalgil M, Küçük AO, et al. Effects of different lipid emulsions on serum adipokines, inflammatory markers and mortality in critically ill patients with sepsis: A prospective observational cohort study. Clin Nutr. 2021;40(7):4569-4578. doi: 10.1016/j.clnu.2021.05.037 [DOI] [PubMed] [Google Scholar]
- 8.Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(5):426–435. doi: 10.1016/S1473-3099(12)70323-7 [DOI] [PubMed] [Google Scholar]
- 9.Rowland T, Hilliard H, Barlow G. Procalcitonin: potential role in diagnosis and management of sepsis. Adv Clin Chem. 2015;68:71–86. [DOI] [PubMed] [Google Scholar]
- 10.Samraj RS, Zingarelli B, Wong HR. Role of biomarkers in sepsis care. Shock. 2013;40(5):358–365. doi: 10.1097/SHK.0b013e3182a66bd6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charles PE, Gibot S. Predicting outcome in patients with sepsis: new biomarkers for old expectations. Critical Care. 2014;18(1):108. doi: 10.1186/cc13723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamayo E, Fernández A, Almansa R, et al. Pro- and anti-inflammatory responses are regulated simultaneously from the first moments of septic shock. Eur Cytokine Netw. 2011;22(2):82–87. doi: 10.1684/ecn.2011.0281 [DOI] [PubMed] [Google Scholar]
- 13.Marchant A, Alegre ML, Hakim A, et al. Clinical and biological significance of interleukin-10 plasma levels in patients with septic shock. J Clin Immunol. 1995;15(5):266–273. doi: 10.1007/BF01540884 [DOI] [PubMed] [Google Scholar]
- 14.Gromer S, Urig S, Becker K. The thioredoxin system – from science to clinic. Med Res Rev. 2004;24(1):40–89. [DOI] [PubMed] [Google Scholar]
- 15.Arnér ES, Holmgren A. Physiological functions of thioredoxin and thioredoxin reductase. Eur J Biochem. 2000;267(20):6102–6109. doi: 10.1046/j.1432-1327.2000.01701.x [DOI] [PubMed] [Google Scholar]
- 16.Callister ME, Burke-Gaffney A, Quinlan GJ, et al. Extracellular thioredoxin levels are increased in patients with acute lung injury. Thorax. 2006;61(6):521–527. doi: 10.1136/thx.2005.053041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai J, Nakamura H, Kwon YW, et al. Critical roles of thioredoxin in nerve growth factor-mediated signal transduction and neurite outgrowth in PC12 cells. J Neurosci. 2003;23(2):503–509. doi: 10.1523/JNEUROSCI.23-02-00503.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmgren A. Antioxidant function of thioredoxin and glutaredoxin systems. Antioxid Redox Signal. 2000;2(4):811–820. doi: 10.1089/ars.2000.2.4-811 [DOI] [PubMed] [Google Scholar]
- 19.Nakamura H. Thioredoxin as a key molecule in redox signaling. Antioxid Redox Signal. 2004;6(1):15–17. doi: 10.1089/152308604771978309 [DOI] [PubMed] [Google Scholar]
- 20.Uhle F, Lichtenstern C, Brenner T, Weigand MA. [Pathophysiology of sepsis]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2015;50(2):114–122. [German] [DOI] [PubMed] [Google Scholar]
- 21.Leaver SK, MacCallum NS, Pingle V, et al. Increased plasma thioredoxin levels in patients with sepsis: positive association with macrophage migtation inhibitory factor. ntensive Care Med. 2010. 36(2);336–341. doi: 10.1007/s00134-009-1640-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen G, Li X, Huang M, et al. Thioredoxin-1 increases survival in sepsis by inflammatory response through suppressing endoplasmic reticulum stress. Shock. 2016;46(1):67–74. doi: 10.1097/SHK.0000000000000570 [DOI] [PubMed] [Google Scholar]
- 23.Yodoi J, Matsuo Y, Tian H, Masutani H, Inamoto T. Anti-inflammatory thioredoxin family proteins for medicare, healthcare and aging care. Nutrients. 2017;9(10):10. doi: 10.3390/nu9101081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nasoohi S, Ismael S, Ishrat T. Thioredoxin-interacting protein (TXNIP) in cerebrovascular and neurodegenerative diseases: regulation and implication. Mol Neurobiol. 2018;55(10):7900–7920. doi: 10.1007/s12035-018-0917-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathys L, Balzarini J. The role of cellular oxidoreductases in viral entry and virus infection-associated oxidative stress: potential therapeutic applications. Expert Opin Ther Targets. 2016;20(1):123–143. doi: 10.1517/14728222.2015.1068760 [DOI] [PubMed] [Google Scholar]
- 26.Adib-Conquy M, Cavaillon JM. [Host inflammatory and anti-inflammatory response during sepsis]. Pathologie-Biologie. 2012;60(5):306–313. doi: 10.1016/j.patbio.2012.03.011. [Dutch] [DOI] [PubMed] [Google Scholar]
- 27.Salomão R, Ferreira BL, Salomão MC, Santos SS, Azevedo LCP, Brunialti MKC. Sepsis: evolving concepts and challenges. Braz J Med Biol Res. 2019;52(4):e8595. doi: 10.1590/1414-431x20198595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakamura T, Nakamura H, Hoshino T, Ueda S, Wada H, Yodoi J. Redox regulation of lung inflammation by thioredoxin. Antioxid Redox Signal. 2005;7(1–2):60–71. doi: 10.1089/ars.2005.7.60 [DOI] [PubMed] [Google Scholar]
- 29.Nadeem A, Masood A, Siddiqui N. Oxidant–antioxidant imbalance in asthma: scientific evidence, epidemiological data and possible therapeutic options. Ther Adv Respir Dis. 2008;2(4):215–235. doi: 10.1177/1753465808094971 [DOI] [PubMed] [Google Scholar]
- 30.Mantzarlis K, Tsolaki V, Zakynthinos E. Role of oxidative stress and mitochondrial dysfunction in sepsis and potential therapies. Oxid Med Cell Longev. 2017;2017:5985209. doi: 10.1155/2017/5985209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brigham KL. Oxygen radicals – an important mediator of sepsis and septic shock. Klin Wochenschr. 1991;69(21–23):1004–1008. doi: 10.1007/BF01645147 [DOI] [PubMed] [Google Scholar]
- 32.Watanabe R, Nakamura H, Masutani H, Yodoi J. Anti-oxidative, anti-cancer and anti-inflammatory actions by thioredoxin 1 and thioredoxin-binding protein-2. Pharmacol Ther. 2010;127(3):261–270. doi: 10.1016/j.pharmthera.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 33.Nakamura A, Wada H, Ikejiri M, et al. Efficacy of procalcitonin in the early diagnosis of bacterial infections in a critical care unit. Shock. 2009;31(6):586–591. doi: 10.1097/SHK.0b013e31819716fa [DOI] [PubMed] [Google Scholar]
- 34.Kopterides P, Siempos II, Tsangaris I, Tsantes A, Armaganidis A. Procalcitonin-guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(11):2229–2241. doi: 10.1097/CCM.0b013e3181f17bf9 [DOI] [PubMed] [Google Scholar]
- 35.Janković B, Veljković D, Pasić S, Rakonjac Z, Jevtić D, Martić J. [C-reactive protein and cytokines in the diagnosis of neonatal sepsis]. Med Pregl. 2006;59(11–12):545–549. doi: 10.2298/MPNS0612545J. [Slovenian] [DOI] [PubMed] [Google Scholar]
- 36.Hofer N, Zacharias E, Müller W, Resch B. An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology. 2012;102(1):25–36. doi: 10.1159/000336629 [DOI] [PubMed] [Google Scholar]
- 37.Ma L, Zhang H, Yin YL, et al. Role of interleukin-6 to differentiate sepsis from non-infectious systemic inflammatory response syndrome. Cytokine. 2016;88:126–135. doi: 10.1016/j.cyto.2016.08.033 [DOI] [PubMed] [Google Scholar]
- 38.Patel RT, Deen KI, Youngs D, Warwick J, Keighley MR. Interleukin 6 is a prognostic indicator of outcome in severe intra-abdominal sepsis. Br J Surg. 1994;81(9):1306–1308. doi: 10.1002/bjs.1800810914 [DOI] [PubMed] [Google Scholar]
- 39.Herwanto V, Shetty A, Nalos M, et al. Accuracy of quick sequential organ failure assessment score to predict sepsis mortality in 121 studies including 1,716,017 individuals: a systematic review and meta-analysis. Crit Care Explor. 2019;1(9):e0043. doi: 10.1097/CCE.0000000000000043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caraballo C, Jaimes F. Organ dysfunction in sepsis: an ominous trajectory from infection to death. Yale J Biol Med. 2019;92(4):629–640. [PMC free article] [PubMed] [Google Scholar]
- 41.Vincent JL, Quintairos ESA, Couto L Jr., Taccone FS. The value of blood lactate kinetics in critically ill patients: a systematic review. Critical Care. 2016;20(1):257. doi: 10.1186/s13054-016-1403-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chertoff J, Chisum M, Garcia B, Lascano J. Lactate kinetics in sepsis and septic shock: a review of the literature and rationale for further research. J Intensive Care. 2015;3(1):39. doi: 10.1186/s40560-015-0105-4 [DOI] [PMC free article] [PubMed] [Google Scholar]