Abstract
Background
COVID-19 pandemic has remained one of the leading causes of death which claimed the lives of many well-trained and experienced healthcare professionals. Vaccination is the most effective way of controlling infectious diseases, while success is challenged by individuals and groups who choose to delay or refuse vaccines. The objective of the present study was to assess the intention of healthcare workers in Eastern Ethiopia to receive the second round of COVID-19 vaccine.
Methods
Institution-based cross-sectional survey research design was used to collect quantitative data from a representative sample of healthcare workers in Dire Dawa, Haramaya, and Harar towns of Eastern Ethiopia. The correctly filled questionnaires were selected and entered into SPSS software for further analysis, where frequency tables, percentages, mean, and multinomial logistic regression analysis were used in the process.
Results
The findings revealed that most (61.6%) of the research participants are willing to receive the second round of COVID-19 vaccine, and 10.3% reported that they have not decided yet. Moreover, the main reason for respondents’ lack of intention to receive the second round of COVID-19 vaccine is the belief that the first round of COVID-19 vaccine is sufficient to prevent infection (27.8%) followed by concern over the safety or side effects of the vaccine (26.6%). Above all, the healthcare workers’ intention of taking the second round of COVID-19 vaccine is significantly associated to having children (OR=0.362, P<0.05; 95% CI: 3.279–5465.189), previous interaction with someone infected by COVID-19 (OR=1.480, P<0.05; 95% CI: 3.949–0.055), the perception that COVID-19 causes a severe illness (OR=0.018, P<0.05, 95% CI: 13.489–196.391), and experience of receiving the first round of COVID-19 vaccine (OR=50431.104, P<0.01; 95% CI: 408.789–626.00).
Conclusion
The present study has shown that healthcare workers in Eastern Ethiopia have a good intention of receiving the second round of COVID-19 vaccine. Nevertheless, the findings have also made it clear that there are still issues to be addressed as far as both willingness to receive the second round of the vaccine and experience of taking the first round of the vaccine are concerned. It is, therefore, important that sufficient training should be given to the healthcare workers in the area in order to raise their level of awareness and enhance their willingness to receive the second round of the vaccine.
Keywords: COVID-19, healthcare workers, intention, second-round, vaccine
Introduction
Reports indicate that healthcare workers across the world are facing an increasing threat as a result of confronting severe and contagious diseases, including COVID-19.1,2 Furthermore, the COVID-19 pandemic has remained one of the leading causes of death which claimed the lives of many well-trained and experienced healthcare professionals, especially in Europe.3 Many healthcare workers have died after contracting the virus while treating the patients infected by COVID-19.4 The loss of such trained manpower has enormous economic and social consequences,5,6 the impact of which increases especially in developing countries such as Ethiopia where the cost of training medical personnel is relatively high. Some of the determinants of risk of disease transmission to the healthcare workers include working in close proximity to a patient, risks associated to the hospital environment, the lack of consistency with safety instructions and the frequently changing directives, the attitudes and actions of the management and the perceived importance of occupational health and safety, the absence of evidence-based and practical infection control policies, and the lack of communication about safety within healthcare organizations.7
Vaccine hesitancy is believed to be responsible for decreasing vaccine coverage and an increasing risk of vaccine-preventable disease outbreaks and epidemics.8 Previous researches are full of findings that show a mix of both high and low acceptability of COVID-19 vaccination among the healthcare workers in various parts of the world. For instance, a study conducted in Democratic Republic of Congo9 and Saudi Arabia10 found low acceptability of COVID-19 vaccination among healthcare workers. Moreover, Kukreti et al11 found that Taiwan’s healthcare workers' and outpatients’ willingness to receive vaccination was low for both healthcare workers (23.4%) and the outpatient sample (30.7%) due to the relatively safe status of COVID-19 infection in Taiwan, where risk perception, willingness to take rapid test, and preventive COVID-19 infection behaviors were significant factors explaining the healthcare workers’ willingness to receive vaccination. Paudel et al12 found that only one-third (38.3%) of healthcare workers in Nepal are willing to be vaccinated for COVID-19. On the other hand, a study conducted among the clinical staffs of Yale Medicine and Yale New Haven Health by Roy et al13 revealed that 85% of healthcare workers were extremely likely or somewhat likely to receive the COVID-19 vaccine. Moreover, Alvarado-Socarras et al14 found that between 77.0% and 90.7% of physicians in Colombia accept COVID-19 vaccination. According to a study undertaken by Vignier et al15 in French Guiana, 65.6% of respondents reported that they were willing or had already been vaccinated against COVID-19, while 24.3% of respondents reported that they did not want to get vaccinated against COVID-19, and 11.2% were unsure.
According to the health belief model, a person’s beliefs about health and health conditions play a significant role in determining his/her health-related behaviors.16 The key variables that determine an individual’s health behavior include perceived severity of an illness, whether the person thinks he is susceptible to certain ill-health conditions, perceived benefits that the person is likely to obtain as a result of engaging in a pro-health behavior, perceived barriers, information that prompts a desire to make a health change, and a person’s self-efficacy of bringing health-related change.17–19 For instance, Jones et al17 found a positive effect of increased exposure to vaccination campaign on adults’ vaccination behavior.
A population-based cross-sectional e-survey conducted by Mesele20 found poor knowledge but a positive attitude held towards COVID-19 vaccine in Ethiopia. Another related study conducted in southern Ethiopia21 revealed low acceptance (46.1%) of COVID-19 vaccine among the population most at risk of infection in the area. Similarly, Belsti et al22 have also come up with the finding that there is low (31.4%) acceptance of COVID-19 vaccine in Ethiopia. On the other hand, Mose et al23 found a relatively high (70.7%) acceptance of the vaccine among pregnant women attending antenatal care clinic in Southwest Ethiopia. Other authors24,25 have also undertaken similar studies of knowledge, attitude, and acceptability of COVID-19 vaccine among the general population in Ethiopia and found a mix of both high and low acceptance levels of the vaccine. Recent public media sources revealed that about 1.9 million people in Ethiopia have received the first round of COVID-19 vaccine. The experiences of these groups of population with the first round of vaccine, including their emotional reactions and their willingness to receive the second round of the vaccine, have not been researched. The purpose of the present research was therefore to examine the intention of healthcare workers in Eastern Ethiopia to receive the second round of COVID-19 vaccine and the factors associated to their intention.
Materials and Methods
Research Design
Institutional-based cross sectional study design was used in which quantitative data were collected using a survey method from a representative sample of healthcare workers providing healthcare services in various healthcare facilities of Eastern Ethiopia.
Research Site and Selection of Participants
The present study was undertaken during the period in which the population “most at risk of infection with COVID-19” had taken the first round of COVID-19 vaccine and were waiting to take the remaining dose. Therefore, the target populations of the present research were all people in Eastern Ethiopia that had taken the first round of COVID-19 vaccine. Unfortunately, it was only the healthcare workers and a few elderly having chronic illnesses that had got the chance to be vaccinated, given the lesser amount of vaccines that the government could supply. With the poor client’s basic information archival experiences of healthcare facilities in the study area, tracing the addresses of the other groups who have taken the vaccine (the elderly with chronic illnesses) was hardly possible for the researchers. Consequently, the survey populations of the present study are all healthcare workers in Eastern Ethiopia that have taken the first round of COVID-19 vaccine. In order to determine the sample size, the researchers applied Cochran’s (1977) formula for calculating the sample size of an unknown population as:
 |
Where n is the sample size, z is the selected critical value of desired confidence level, p is the estimated proportion of an attribute that is present in the population. Then, the final sample units were chosen on the basis of probability proportionate to size sampling technique.
Research Method and Source of Data
Primary data were gathered mainly through the use of survey research method. A self-administered questionnaire was prepared in English, and then translated into local (Amharic) language. Then, data collectors, all of whom were instructors from the sociology department, were trained about the items in the questionnaire and all the things to be done in the process of data collection. Following this, a permission letter was secured from the concerned body of the Haramaya University. Next, a pilot test was undertaken to prove compatibility of the questionnaire on a 5% sample of respondents having similar characteristics with the actual survey population. On the basis of feedbacks and comments obtained from the baseline survey, slight improvements were made to the instrument of data collection. The same questionnaire, having similar items, was duplicated according to the already determined sample size after consideration of a 5% addition of questionnaire copies to substitute potential losses before distribution. Finally, the actual data collection activity was held in June 2021 under the supervision of the principal investigator. During data gathering, data collectors have been clearly instructing respondents about how to fill the questionnaire. A close follow-up was made by both data collectors and supervisors. Respondents were told to freely raise any question that is unclear to them. The reliability of the instrument was checked through internal consistency of the response items using Cronbach’s α, while both content and face validity measures were used to maintain its validity.
Instrument Design
The questionnaire that served as an instrument of data collection in our research was partly taken from the studies of Zewude et al21 and adapted to the purpose at hand, while most other questions were developed by the researchers. The questionnaire mainly consists of three sections: questions seeking socio-demographic background of respondents, their experiences with the first round of COVID-19 vaccine and their intention to receive the second round of vaccine, and questions seeking to assess the attitude of respondents towards COVID-19 vaccine. The first (background) section of the tool comprises variables such as sex, age, education, occupational status, marital status, and the presence of children. In addition, this part also includes questions that aim at measuring respondents’ perceptions of COVID-19 and their previous contact or experience with the disease. For instance, respondents were asked about their perception regarding whether COVID-19 causes severe illnesses, if they know someone who was infected by or died of COVID-19, and whether they believe that they can be infected by COVID-19, their belief about the likelihood of dying from COVID-19, all with response categories of “Yes“ and “No“.
The second section of the questionnaire which assesses respondents’ willingness to take the second round of COVID-19 vaccine comprises questions such as: 1) “Will you take the second round of COVID-19 vaccine if it is freely provided by the government?” with response categories of “Yes” and “No”, 2) a question that attempts to understand the reasons for respondents who may hesitate to take the vaccine with response categories of “I am concerned about the safety and/or the side effects”, “because I believe that I have adequate natural immunity”, “I am concerned because I don’t think the vaccine will be effective”, “I believe that I am not exposed to the disease”, “I believe that I can easily withstand the illness if infected by the disease”, “I don’t think I will need the vaccine due to previous infection, health status or age” among other alternatives. Furthermore, respondents who may respond “Yes” to take the vaccine were also asked when they would like to take the vaccine provided that it is freely available to them, with response categories of “as soon as possible” and “after the vaccine’s safety is confirmed”. Moreover, the section also includes questions that aim at assessing healthcare workers’ experiences and reactions with the first round of the vaccine, including the reasons that respondents did not receive the first round of COVID-19 vaccine.
The third section of the questionnaire, with the objective of assessing respondents’ overall attitude towards the vaccine, consisted of questions with answers on a four-point Likert scale ranging from “1=strongly agree” to “4=strongly disagree”. The section comprised questions such as: “I will not be taking COVID-19 vaccine until it becomes compulsory by law”, “Taking other protective measures is much better than taking COVID-19 vaccine”, and “COVID-19 is not such a serious disease that it doesn’t require vaccine”, among other statements.
Method of Data Analysis
The questionnaires returned from the field were first checked for completeness. The correctly completed ones were then inserted into Statistical Package for Social Sciences software. Data generated from the software were presented using both descriptive and inferential statistical tools. Data analysis was conducted using statistical techniques, including percentages, frequency distributions, and logistic regression analysis. The descriptive statistical techniques were mainly used to present data regarding the frequency and percentage distribution of responses pertaining to respondents’ socio-demographic characteristics, intention to receive the second round of the vaccine, previous experiences and reflections with the first round of COVID-19 vaccine, and reasons for not taking the vaccine. The multinomial logistic regression test was used to examine the association between the socio-demographic characteristics of respondents and their intention to receive the second round of COVID-19 vaccine.
Results
Data presented in Table 1 show the frequency and percentage distribution of respondents’ socio-demographic characteristics. The mean age of respondents is 31.97 (SD=8.0), and females constitute the majority (60.8%) of the research participants; 55.6% of respondents are married, while the widowed hold the least (3%) share in the distribution. Moreover, 53.4% of the survey participants reported to have children. The educational status of the respondents reveal that most (53%) of them are BA/BSc degree holders, followed by college diploma holders (26.7%). Furthermore, nurses constituted 39.7% of the occupational group, followed by other categories of healthcare professionals (22.3%). In addition, 75.4% of respondents currently work in the public healthcare organizations, and 21.1% of them belong to the private healthcare facilities. Above all, 80.6% of research participants disclosed that they know someone who has been infected by COVID-19, and 73.7% know someone who died from COVID-19. The data also show that 59.1% of respondents think that they can be infected by COVID-19, while 87.9% of them believe that COVID-19 causes a severe illness. It is also revealed that 50.4% of the research participants perceive that they are not likely to die if infected by COVID-19.
Table 1.
Socio-Demographic Characteristics of Respondents
| Variables | Categories | Frequency (%) |
|---|---|---|
| Sex | Male | 91 (39.2%) |
| Female | 141 (60.8%) | |
| Marital status | Never married | 82 (35.3%) |
| Married | 129 (55.6%) | |
| Divorced | 14 (6%) | |
| Widowed | 7 (3%) | |
| Having children | Yes | 124 (53.4%) |
| No | 108 (46.6%) | |
| Educational status | Never attended school | 1 (0.4%) |
| Primary school (1–8) | 9 (3.9%) | |
| Secondary school (9–12) | 24 (10.3%) | |
| College diploma | 62 (26.7%) | |
| BA/BSc Degree | 123 (53%) | |
| MA/MSc Degree and above | 13 (5.6%) | |
| Occupational status | Medical doctor | 9 (3.9%) |
| Health officer | 8 (3.4%) | |
| Administrative staff | 26 (11.2%) | |
| Nurse | 92 (39.7%) | |
| Medical laboratory technician | 18 (7.8%) | |
| Pharmacist | 17 (7.3%) | |
| Security | 3 (1.3%) | |
| Janitor | 6 (2.6%) | |
| Others | 53 (22.3%) | |
| Type of organization in which respondents are currently working | Public | 175 (75.4%) |
| Private | 49 (21.1%) | |
| Charity | 6 (2.6%) | |
| Others | 2 (0.9%) | |
| Do you know someone ever infected by COVID-19? | Yes | 187 (80.6%) |
| No | 45 (19.4%) | |
| Do you know someone who died of COVID-19? | Yes | 171 (73.7%) |
| No | 61 (26.3%) | |
| Do you think you can be infected by COVID-19? | Yes | 137 (59.1%) |
| No | 95 (40.9%) | |
| Do you think COVID-19 causes a severe illness? | Yes | 204 (87.9%) |
| No | 28 (12.1%) | |
| Do you think you are likely to die if infected by COVID-19? | Yes | 115 (49.6%) |
| No | 117 (50.4%) | |
| Total | 232 (100%) |
Intention to Receive the Second Round of COVID-19 Vaccine Among the Healthcare Workers
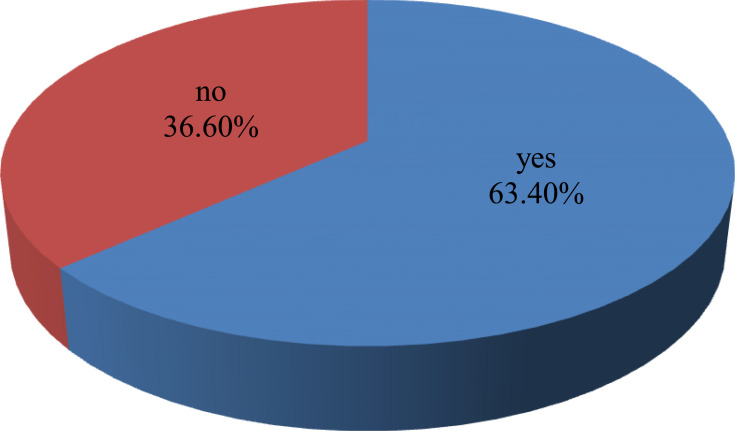
According to the data presented in Figure 1, 63.4% of respondents disclosed that they have received the first round of COVID-19 vaccine, while 36.6% reported that they did not take the vaccine. Moreover, the main reason for respondents for not receiving the vaccine is concerns about the safety or side effects of the vaccine (41.9%), followed by doubts pertaining to the effectiveness of the vaccine (40.7%), reasons related to religion (14%), the belief that other non-vaccine preventive mechanisms are sufficient to prevent infection (9.3%), and belief of possessing adequate natural immunity (9.3%), as presented in Table 2.
Figure 1.
Experiences of receiving the first round of COVID-19 vaccine?.
Table 2.
Frequency Distribution of Respondents’ Reasons for Not Taking the First Round of COVID-19 Vaccine
| Reasons for Not Taking the First Round of COVID-19 Vaccine | Responses | Percent of Cases | |
|---|---|---|---|
| N | Percent | ||
| I am concerned about the safety and/or the side effects | 36 | 26.5% | 41.9% |
| I believe that I have adequate natural immunity | 8 | 5.9% | 9.3% |
| I am concerned because I do not think the vaccine will be effective | 35 | 25.7% | 40.7% |
| I believe that I am not exposed to the disease | 2 | 1.5% | 2.3% |
| I believe that I can easily withstand the illness if infected by the disease | 2 | 1.5% | 2.3% |
| I do not think I will need the vaccine due to previous infection, health status or age | 5 | 3.7% | 5.8% |
| I am against vaccines in general | 5 | 3.7% | 5.8% |
| Lack of adequate information | 6 | 4.4% | 7.0% |
| Reasons related to belief or religion | 12 | 8.8% | 14.0% |
| I believe that other non-vaccine preventive mechanisms are sufficient | 8 | 5.9% | 9.3% |
| COVID-19 is not that serious a concern in my work or residential area | 1 | 0.7% | 1.2% |
| Other reasons | 16 | 11.8% | 18.6% |
| Total | 136 | 100.0% | 158.1% |
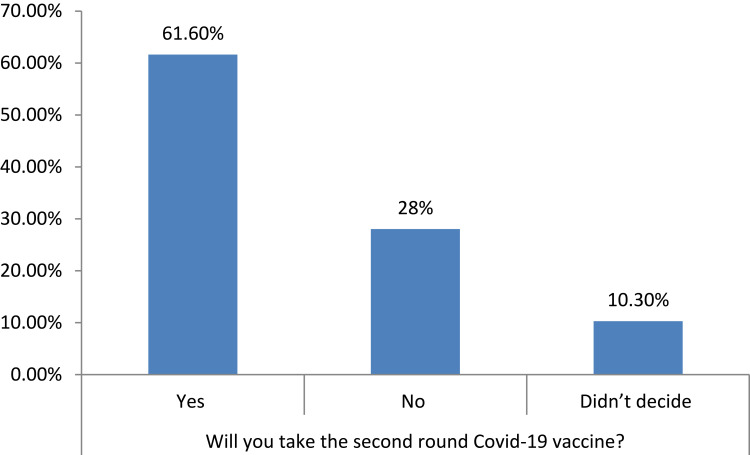
Figure 2 shows data regarding the distribution of respondents in terms of intention to receive the second round of COVID-19 vaccine. Accordingly, most (61.6%) of the research participants are willing to receive the second round of COVID-19 vaccine, followed by 28% of respondents who disclosed that they are not willing to take the second round of COVID-19 vaccine, and 10.3% reported that they have not decided yet. In addition, data presented in Table 3 reveal that the main reason for respondents’ lack of intention to receive the second round of COVID-19 vaccine is the belief that the first round of COVID-19 vaccine is sufficient to prevent infection (27.8%), followed by concern over the safety or side effects of the vaccine (26.6%), doubts about the effectiveness of the vaccine in preventing infection (22.8%), and experiences of discomfort during receiving the first round of the vaccine (20.3%).
Figure 2.
Intention to receive the second round of COVID-19 vaccine.
Table 3.
Frequency Distribution of Respondents’ Reasons for the Lack of Willingness to Take the Second Round of COVID-19 Vaccine
| Reasons for the Lack of Willingness to Receive the Second Round of COVID-19 Vaccine | Responses | Percent of Cases | |
|---|---|---|---|
| N | Percent | ||
| I believe that the first round of COVID-19 vaccine is sufficient to prevent infection | 22 | 18.5% | 27.8% |
| I was not comfortable with the first dose of COVID-19 vaccine | 16 | 13.4% | 20.3% |
| I am concerned about the safety and/or the side effects | 21 | 17.6% | 26.6% |
| I believe that I have adequate natural immunity | 6 | 5.0% | 7.6% |
| I am concerned because I do not think the vaccine will be effective | 18 | 15.1% | 22.8% |
| I believe that I am not exposed to the disease | 1 | 0.8% | 1.3% |
| I believe that I can easily withstand the illness if infected by the disease | 1 | 0.8% | 1.3% |
| I do not think I will need the vaccine due to previous infection, health status or age | 4 | 3.4% | 5.1% |
| I am against vaccines in general | 3 | 2.5% | 3.8% |
| Lack of adequate information | 6 | 5.0% | 7.6% |
| Reasons related to belief or religion | 5 | 4.2% | 6.3% |
| I believe that other non-vaccine preventive mechanisms are sufficient | 2 | 1.7% | 2.5% |
| COVID-19 is not that serious a concern in my work or residential area | 1 | 0.8% | 1.3% |
| Other reasons | 13 | 10.9% | 16.5% |
| Total | 119 | 100.0% | 150.6% |
As shown in Table 4, the majority (72%) of respondents disclosed that they would like to take the second round of COVID-19 vaccine as soon as they get it, while 28% replied that they would like to receive the vaccine after its safety is confirmed. Furthermore, respondents were asked about their feelings if they fail to get the chance of receiving the second round of COVID-19 vaccine. Accordingly, 39.2% of respondents reported that they will be highly concerned, 37.5% not concerned at all, and 23.3% of respondents report being moderately concerned if they do not get the opportunity of receiving the second round of COVID-19 vaccine.
Table 4.
Respondents’ Concerns Over Receiving the Second Round of COVID-19 Vaccine
| Variables | Categories | Frequency (%) |
|---|---|---|
| When would you like to take the second round of COVID-19 vaccine? | As soon as I get it | 167 (72%) |
| After its safety is confirmed | 65 (28%) | |
| How concerned will you be if you do not get the opportunity of receiving the second round of COVID-19 vaccine? | Highly concerned | 91 (39.2%) |
| Moderately concerned | 54 (23.3%) | |
| Not concerned at all | 87 (37.5%) | |
| Total | 232 (100%) |
Data presented in Table 5 show the attitude of healthcare workers towards COVID-19 vaccine. It is shown that 171 (73.7%) of respondents agree and strongly agree that they will not be taking COVID-19 vaccine unless they are compelled by law (M=2.06, SD=1.02). In addition, 60.7% of the healthcare workers who participated in the study agree that taking other protective measures (such as wearing a mask, frequent washing of hands, etc) is much better than taking COVID-19 vaccine (M=2.3, SD=1.0). Moreover, 85.7% of the research participants agree that it is better to be infected by COVID-19 than taking the vaccine (M=1.7, SD=0.85). Accordingly, the findings imply that healthcare workers who participated in the survey generally have negative attitude towards COVID-19 vaccine.
Table 5.
Healthcare Workers’ Attitude Towards COVID-19 Vaccine
| Statements | SA | A | D | SD | Mean | St.Dev. |
|---|---|---|---|---|---|---|
| I will not be taking COVID-19 vaccine unless I am compelled by law | 80 (34.5%) | 91 (39.2%) | 26 (11.2%) | 35 (15.1%) | 2.0690 | 1.02964 |
| Taking other protective measures is much better than taking COVID-19 vaccine | 56 (24.1%) | 85 (36.6%) | 54 (23.3%) | 37 (15.9%) | 2.3103 | 1.01003 |
| COVID-19 is not such a serious diease that it does not require vaccine | 90 (38.8%) | 99 (42.7%) | 26 (11.2%) | 17 (7.3%) | 1.8615 | 0.87369 |
| I believe that the side effects of COVID-19 vaccine outweigh its immunizing advantages | 62 (26.7%) | 110 (47.4%) | 31 (13.4%) | 29 (12.5%) | 2.1164 | 0.94401 |
| It is better to be infected by COVID-19 than taking the vaccine | 114 (49.1%) | 85 (36.6%) | 19 (8.2%) | 14 (6%) | 1.7112 | 0.85698 |
| N=232 | ||||||
Abbreviations: SA, strongly agree; A, agree; D, disagree; SD, strongly disagree; St.Dev, standard deviation.
Factors Associated with Intention to Receive the Second Round of COVID-19 Vaccine
Table 6 presents the results of multinomial logistic regression analysis regarding the association between respondents’ socio-demographic characteristics and their intention to receive the second round of COVID-19 vaccine. According to the data, the healthcare workers’ intention of taking the second round of COVID-19 vaccine is significantly associated to having children (OR=0.362, P<0.05; 95% CI: 3.279–5465.189), previous interaction with someone infected by COVID-19 (OR=1.480, P<0.05; 95% CI:3.949–0.055), the perception that COVID-19 causes a severe illness (OR=0.018, P<0.05, 95% CI: 13.489–196.391), and experience of receiving the first round of COVID-19 vaccine (OR=50431.104, P<0.01; 95% CI: 408.789–626.00). For instance, healthcare workers having children are 10.65 times more willing to receive the second round of COVID-19 vaccine; those who know someone who was infected by COVID-19 are −18 times more likely to receive the second round of COVID-19 vaccine.
Table 6.
Coefficients of Multinomial Logistic Regression Analysis
| Will You Take the Second Round of COVID-19 Vaccine if It Is Freely Provided to You? | B | P-value | OR | 95% CI | |
|---|---|---|---|---|---|
| Yes | Sex | −1.016 | 0.663 | 0.362 | 0.004–34.844 |
| Marital status | 5.189 | 0.985 | 179.269 | 6.27–5.125 | |
| Children | 10.653 | 0.027* | 42337.124 | 3.279–5465.189 | |
| Educational status | −3.673 | 0.990 | 0.025 | 2.751–2.347 | |
| Occupational status | 48.885 | 0.856 | 1,700,441 | 8.198–3.527 | |
| Know someone infected by COVID-19 | −18.028 | 0.020* | 1.480 | 3.949–0.055 | |
| Know someone died of COVID-19 | 6.036 | 0.215 | 418.106 | 0.030–5847.941 | |
| Perceived susceptibility to COVID-19 | −3.025 | 0.261 | 0.049 | 0.000–9.522 | |
| Perceive COVID-19 causes severe illness | 15.454 | 0.018* | 5148819.228 | 13.489–196.391 | |
| Belief about the likelihood dying of COVID-19 | −1.678 | 0.462 | 0.187 | 0.002–16.281 | |
| Received the first round of COVID-19 vaccine | 29.249 | 0.002** | 50431.104 | 408.789–626.00 | |
| No | Sex | −1.902 | 0.466 | 0.149 | 0.001–24.850 |
| Marital status | −2.605 | 0.993 | 0.074 | 2.072–2.634 | |
| Children | 21.735 | 0.009** | 27514.643 | 246.882–3066.00 | |
| Occupational status | 9.265 | 0.033* | 10566.263 | 2.144–528.82 | |
| Know someone infected by COVID-19 | −22.512 | 0.010* | 1.672 | 6.632–0.004 | |
| Know someone died of COVID-19 | 14.486 | 0.026* | 19561.785 | 5.550–6882.915 | |
| Perceived susceptibility to COVID-19 | −0.077 | 0.969 | 0.926 | 0.018–46.640 | |
| Perceive COVID-19 causes severe illness | 3.328 | 0.485 | 27.871 | 0.002–3160.57 | |
| Belief about the likelihood dying of COVID-19 | 0.973 | 0.644 | 2.647 | 0.042–165.117 | |
| Received the first round of COVID-19 vaccine | 7.073 | 0.123 | 1179.426 | 0.147–9482.52 | |
Notes: The reference category is: did not decide. **P<0.01, *P<0.05.
Abbreviations: OR, odds ratio; CI, confidence interval.
Discussion
The COVID-19 pandemic has remained one of the leading causes of death for health professionals worldwide, which claimed the lives of many well-trained and experienced healthcare professionals, especially in Europe.3 Many healthcare workers have died after contracting the virus while treating the patients infected by COVID-19.4 Vaccination is the most effective way of controlling infectious diseases, while success is challenged by individuals and groups who choose to delay or refuse vaccines.26 Vaccine hesitancy is believed to be responsible for decreasing vaccine coverage and an increasing risk of vaccine-preventable disease outbreaks and epidemics.8 According to the health belief model, a person’s beliefs about health and health conditions play a significant role in determining his/her health related behaviors.16 The objective of the present study was to assess the intention of healthcare workers in Eastern Ethiopia to receive the second round of COVID-19 vaccine.
The results of the research indicated that 63.4% of respondents disclosed that they have received the first round of COVID-19 vaccine, while 36.6% reported that they did not take the vaccine. Moreover, most (61.6%) of the research participants are willing to receive the second round of COVID-19 vaccine, followed by 28% of respondents who disclosed that they are not willing to take the second round of vaccine, and 10.3% reported that they have not decided yet. The findings of the present study are consistent with the results of most other previous researches conducted outside of Ethiopia regarding the willingness of healthcare workers to receive COVID-19 vaccine. For instance, a study conducted by Roy et al13 revealed that 85% of healthcare workers were extremely likely or somewhat likely to receive the COVID-19 vaccine. In addition, Alvarado-Socarraset al14 found that between 77.0% and 90.7% of physicians in Colombia accept COVID-19 vaccination. According to a study undertaken by Vignier et al,15 65.6% of respondents reported that they were willing or had already been vaccinated against COVID-19, while 24.3% of respondents reported that they did not want to get vaccinated against COVID-19, and 11.2% were unsure. On the other hand, a study conducted in Chile by Cerda et al26 indicated that 49% of respondents are willing to be vaccinated, while 28% were undecided.
From those who expressed willingness to receive the second round of vaccine, the majority (72%) of respondents disclosed that they would like to take the second round of COVID-19 vaccine as soon as they get it, while 28% replied that they would like to receive the vaccine after its safety is confirmed. In a study undertaken in the United States of America,28 36% of healthcare workers were willing to take the vaccine as soon as it became available, while 56% were not sure or would wait to review more data. According to the findings of Roy et al,13 87% sought the vaccine as soon as it was available to them, while 12% expressed mild hesitancy by stating that they would get it in the next 6 months.
The findings of the present research also revealed that the main reason respondents gave for not receiving the vaccine is concern about the safety or side effects of the vaccine (41.9%), followed by doubts pertaining to the effectiveness of the vaccine (40.7%), reasons related to religion (14%), the belief that other non-vaccine preventive mechanisms are sufficient to prevent infection (9.3%), and belief of possessing adequate natural immunity (9.3%). In addition, the main reason for respondents’ lack of intention to receive the second round of COVID-19 vaccine is the belief that the first round of COVID-19 vaccine is sufficient to prevent infection (27.8%), followed by concern over the safety or side effects of the vaccine (26.6%), doubts about the effectiveness of the vaccine in preventing infection (22.8%), and experiences of discomfort during receiving the first round of the vaccine (20.3%). Similar to the findings of the present study, Roy et al13 found that the top reasons for reluctance were long- and medium-term safety concerns and concerns over the clinical trial’s exclusion of specific groups. Furthermore, Pataka et al29 found that the rate of acceptance of COVID-19 vaccine was higher in healthcare professionals working with COVID-19 patients and also among physicians (76.5%) compared with nurses (48.3%) and other healthcare professionals. According to Unroe et al,30 concern about side effects was the primary reason for vaccine hesitancy (70%). Above all, Zewude et al21 found that the main reason for most respondents’ hesitancy to take the vaccine is the concern over the safety and/or the side effects of the vaccine, followed by doubt about the vaccine’s effectiveness, and lack of adequate information. Safety (69%), effectiveness (69%), and speed of development/approval (74%) were noted as the most common concerns regarding COVID-19 vaccination.27 Cerda et al26 revealed that individuals preferred less risky vaccines in terms of fewer side effects rather than effectiveness.
The findings of our study imply that healthcare workers who participated in the survey generally have negative attitudes towards COVID-19 vaccine. For instance, 171 (73.7%) of respondents agree and strongly agree that they will not be taking COVID-19 vaccine unless they are compelled by law (M=2.06, SD=1.02). In addition, 60.7% of the healthcare workers who participated in the study agree that taking other protective measures (such as wearing a mask, frequent washing of hands, etc) is much better than taking COVID-19 vaccine (M=2.3, SD=1.0). Moreover, 85.7% of the research participants agree that it is better to be infected by COVID-19 than taking the vaccine (M=1.7, SD=0.85). Our finding is inconsistent with the results of Mesele20 who found a poor knowledge but a positive attitude held towards COVID-19 vaccine in Ethiopia where access to the media, residential background, and educational status influence level of awareness.
The results of binary logistic regression analysis in our survey show that the healthcare workers’ intention of taking the second round of COVID-19 vaccine is significantly associated with having children (OR=0.362, P<0.05; 95% CI: 3.279–5465.189), previous interaction with someone infected by COVID-19 (OR=1.480, P<0.05; 95% CI:3.949–0.055), the perception that COVID-19 causes a severe illness (OR=0.018, P<0.05, 95% CI: 13.489–196.391), and experience of receiving the first round of COVID-19 vaccine (OR=50431.104, P<0.01; 95% CI: 408.789–626.00). According to the findings of Shekhar et al,28 vaccine acceptance increased with increasing age, education, and income level. A smaller percentage of female (31%), Black (19%), Lantinx (30%), and rural (26%) healthcare workers were willing to take the vaccine as soon as it became available than the overall study population. Moreover, Alvarado-Socarras et al14 found that medical specialty, having never paid for a vaccine, recommending the administration of the vaccine to their parents or people over 70 years, and dispensing the vaccine to their children were the factors to consider to be vaccinated for free. A study by Akibu et al31 found that only one-fourth of health professionals received the recommended full dose of the vaccine, where attending infection-prevention training, history of exposure to risky behavior, and long years of work experience have positively affected vaccination status.
Conclusion
The present study has shown that healthcare workers in Eastern Ethiopia have a good intention of receiving the second round of COVID-19 vaccine. Nevertheless, the findings have also made it clear that there are still issues to be addressed as far as both willingness to receive the second round of the vaccine and experience of taking the first round of the vaccine is concerned. With the government's very limited capacity of satisfying the vaccination demands of the population, the few doses obtained through international aid have been allocated to the healthcare workers, given their risky professional engagements. When that is done, it was with expectation that they will have all the required awareness about the vaccine and hence will be willing to receive it. The results of the present study, however, made it clear that healthcare workers hold negative attitude towards the vaccine, and more than one-third of them not only did not receive the first round of the vaccine but also do not have the intention to receive the second round of COVID-19 vaccine. Furthermore, we have also found that some of the healthcare professionals believe that the first round of the COVID-19 vaccine is sufficient to prevent infection, while there are others that are still concerned about the safety or side effects of the vaccine. It is, therefore, important that sufficient training should be given to the healthcare workers in the area in order to raise their level of awareness and enhance their willingness to receive the second round of the vaccine.
Acknowledgments
We would like to extend our gratitude to duplication unit staffs of Haramaya University for their unreserved help in the process of duplicating the questionnaires. Finally, all respondents who have willfully devoted their time in filling the questionnaires also deserve appreciation.
Funding Statement
There are no funding resources to declare.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Approval Committee of Haramaya University. Furthermore, prior to completing the questionnaires, written informed consent forms were signed by all research participants. In addition, a formal letter was secured from the Department of Sociology, Haramaya University. An informed both verbal and written consent was obtained by informing the research participants about the objectives and rationale of undertaking the research. Furthermore, upon collecting data, the names of the research participants were not written on the interviewer-administered questionnaire in order to keep their personal identity anonymous. Moreover, research participants were informed ahead about the possibility of withdrawing from the study in case the need arises at any time. This study was conducted in accordance with the Declaration of Helsinki.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Woyessa AH, Oluma A, Palanichamy T, et al. Predictors of health-care workers’ unwillingness to continue working during the peak of COVID-19 in western ethiopia: an extended parallel-process model study. Risk Manag Healthc Policy. 2021;14:1165–1173. doi: 10.2147/RMHP.S288003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brouwer M, Coelho E, Dores Mosse C, et al. Healthcare workers’ challenges in the implementation of tuberculosis infection prevention and control measures in mozambique. PLoS One. 2014;9(12):e114364. doi: 10.1371/journal.pone.0114364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hailu D, Benayew M, Liknaw T, et al. Occupational health safety of health professionals and associated factors during COVID-19 pandemics at north showa zone, oromia regional state, ethiopia. Risk Manag Healthc Policy. 2021;14:1299–1310. doi: 10.2147/RMHP.S292830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dorman P. The economics of safety, health, and well-being at work: an overview, in focus program on safe work, international labor organization the evergreen state college; 2020.
- 6.Health and Safety Authority. Workplace safety and health management: practical guidelines on the implementation and maintenance of an occupational safety, health and welfare management system. Dublin: Health and Safety Authority; 2006. Available from: https://www.hsa.ie/eng/Publications_and_Forms/Publications/Safety_and_Health_Management/Workplace_Safety_and_Health_Management.pdf. [Google Scholar]
- 7.Yassi A, Bryce E, Moore D, et al. Protecting the faces of health care workers: knowledge gaps and research priorities for effective protection against occupationally acquired respiratory infectious diseases. Occupational Health and Safety Agency for Healthcare in BC; 2004. Available from: https://open.library.ubc.ca/soa/cIRcle/collections/facultyresearchandpublications/52383/items/1.0048214. [Google Scholar]
- 8.Papagiannis D. The lack of vaccine in the recent COVID-19 pandemic and the silence of anti-vaccination activists. Hellenic J Nursing. 2020;59(4):348–352. [Google Scholar]
- 9.Nzaji KM, Ngombe KL, Mwamba NG, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic republic of the congo. Pragmatic Observational Res. 2020;11:103–109. doi: 10.2147/POR.S271096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8:644300. doi: 10.3389/fmed.2021.644300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kukreti S, Lu M-Y, Lin Y-H, et al. Willingness of Taiwan’s healthcare workers and outpatients to vaccinate against COVID-19 during a period without community outbreaks. Vaccines. 2021;9:246. doi: 10.3390/vaccines9030246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paudel S, Palaian S, Shankur PR, Subedi N. Risk perception and hesitancy toward COVID-19 vaccination among healthcare workers and staff At a medical college in nepal. Risk Manag Healthc Policy. 2021;14:2253–2261. doi: 10.2147/RMHP.S310289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy B, Kumar V, Venkatesh A. Health care workers’ reluctance to take the COVID-19 vaccine: a consumermarketing approach to identifying and overcoming hesitancy. NEJM Catalyst Innovations Care Delivery. 2020;1. [Google Scholar]
- 14.Alvarado-Socarras JL, Vesga-Varela AL, Quintero-Lesmes DC, et al. Perception of COVID-19 vaccination amongst physicians in Colombia. Vaccines. 2021;9:287. doi: 10.3390/vaccines9030287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vignier N, Brureau K, Granier S, et al. Attitudes towards the COVID-19 vaccine and willingness to get vaccinated among healthcare workers in french guiana: the influence of geographical origin. Vaccines. 2021;9:682. doi: 10.3390/vaccines9060682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boskey E. Health belief model; 2020. Available from:https://www.verywellmind.com/health-belief-model-3132721. Accessed July27, 2021.
- 17.Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30:566–576. doi: 10.1080/10410236.2013.873363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hermann A, Hall A, Proietto A. Using the health belief model to explore why women decide for or against the removal of their ovaries to reduce their risk of developing cancer. BMC Women’s Health. 2018;18:184. doi: 10.1186/s12905-018-0673-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frankenfield KM. Health belief model of breast cancer screening for female college students. Master’s Theses and Doctoral Dissertations. 258; 2009. [Google Scholar]
- 20.Mesele M. Awareness and attitude towards COVID-19 vaccination and associated factors in ethiopia: cross-sectional study. Infect Drug Resist. 2021;14:2193–2199. doi: 10.2147/IDR.S316461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zewude B, Habtegiorgis T. Willingness to take COVID-19 vaccine among people most at risk of exposure in Southern Ethiopia. Pragmatic Observ Res. 2021;12:37–47. doi: 10.2147/POR.S313991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Belsti Y, Gela YY, Akalu Y, et al. Willingness of ethiopian population to receive COVID-19 vaccine. J Multidis Healthcare. 2021;14:1233–1243. doi: 10.2147/JMDH.S312637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mose A, Yeshaneh A. COVID-19 vaccine acceptance and its associated factors among pregnant women attending antenatal care clinic in southwest ethiopia: institutional-based cross-sectional study. Int J Gen Med. 2021;14:2385–2395. doi: 10.2147/IJGM.S314346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wake DA. The willingness to receive COVID-19 vaccine and its associated factors: “vaccination refusal could prolong the war of this pandemic” – a systematic review. Risk Manag Healthc Policy. 2021;14:2609–2623. doi: 10.2147/RMHP.S311074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015–2025. doi: 10.2147/IDR.S312116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cerda AA, García LY. Hesitation and refusal factors in individuals’ decision-making processes regarding a coronavirus disease 2019 vaccination. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.626852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paterson P, Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700–6706. doi: 10.1016/j.vaccine.2016.10.0425 [DOI] [PubMed] [Google Scholar]
- 28.Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9:119. doi: 10.3390/vaccines9020119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pataka A, Kotoulas S, Stefanidou E, et al. Acceptability of healthcare professionals to get vaccinated against COVID-19 twoweeks before initiation of national vaccination. Medicina. 2021;57:611. doi: 10.3390/medicina57060611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Unroe KT, Evans R, Weaver L, Rusynaik D, Blackburn J. Willingness of long-term care staff to receive a COVID-19 vaccine: a single state survey. Am Geriatrics Soc. 2021;69:593–599. [DOI] [PubMed] [Google Scholar]
- 31.Akibu M, Nurgi S, Mesgfin T, Tsega WD. Attitude and vaccination status of healthcare workers against hepatitis b infection in a teaching hospital, Ethiopia. Scientifica (Cairo). 2018:2018:6705305. doi: 10.1155/2018/6705305 [DOI] [PMC free article] [PubMed] [Google Scholar]