Abstract
Response to weekly evidence-based PTSD treatments varies. Little is known about response trajectories and predictors in intensive PTSD treatments. This study sought to identify different trajectories of symptom change among veterans who completed a 3-week CPT-based intensive PTSD treatment program and examined potential predictors of trajectory group membership. Four hundred fifty-two veterans completed the program. Demographics, PTSD and depression severity, negative posttrauma cognitions, and alcohol use were assessed at intake and evaluated as possible predictors of group membership. Group based trajectory modeling was used to determine distinct groups based on PTSD symptom trajectory over the course of treatment, as well as predictors of group membership. Four distinct treatment trajectories were identified: Fast responders (15.3%), steady responders (32.0%), partial responders (38.4%), and minimal responders (14.4%). Fast and steady responders reported substantial symptom reductions and dropped below the “probable PTSD” threshold, with fast responders achieving improvements after just one week of treatment. Partial responders experienced clinically significant reductions but remained above the “probable PTSD” threshold. Minimal responders reported the highest baseline PTSD symptoms and changed the least throughout treatment. Negative posttrauma cognitions as well as self-reported and clinician-rated PTSD symptom severity assessed at intake successfully predicted trajectory membership. The identified trajectories closely resemble findings in the limited existing literature on intensive PTSD treatment trajectories. Results suggest that some individuals may improve with even shorter interventions and others might benefit from additional treatment sessions. Overall, findings support the importance of evaluating individual- and group-level treatment responses.
Keywords: PTSD, Veterans, Intensive Treatment, Cognitive Processing Therapy, Trajectory, Treatment Response
Responses to first-line, evidence-based treatments for posttraumatic stress disorder (PTSD), such as Cognitive Processing Therapy (CPT; Resick et al., 2016) and Prolonged Exposure therapy (PE; Foa et al., 2019), differ for individuals, with some responding more favorably than others (Allan et al., 2017; Dewar et al., 2020; Galovski et al., 2016; Stein et al., 2012). Individuals who receive these treatments can generally be categorized into two to five response trajectory groups, with a classification of responder, non-responder, and sub-threshold groups being most common (Dewar et al., 2020). Depending on the sample, comorbid mental health conditions (e.g., depression and alcohol use) as well as demographic factors (e.g., age and combat exposure) can be used to predict treatment response.
Most research on PTSD treatment response trajectories has focused on weekly treatments. Although increased session frequency is associated with improved treatment response (Gutner et al., 2016), little is known about response trajectories for intensive PTSD treatments, which involve daily treatment sessions over 1-3 weeks (Held et al., 2019a). Intensive PTSD treatments have been shown to be feasible and effective, producing substantial PTSD symptom reductions while reducing dropout rates compared to weekly interventions (Bryan et al., 2018; Ehlers et al., 2014; Foa et al., 2018; Goetter et al., 2020; Harvey et al., 2018; Hendriks et al., 2018; Held et al., 2019b; Zalta et al., 2018). Only two published studies have examined treatment trajectories and their predictors in intensive PTSD treatments for civilians. Hendriks and colleagues (2018) examined response to intensive PE delivered 3x/day over four days followed by four weekly booster sessions and identified four treatment trajectories: fast responders (13%) who lost their PTSD diagnosis directly following the intensive treatment phase and experienced additional symptom reduction during the booster phase; slow responders (26%) who showed no significant treatment response directly after the intensive phase but experienced symptom reduction and lost their PTSD diagnosis during the booster phase; partial responders (32%) who also showed no significant treatment response directly after the intensive phase but experienced continued symptom reduction during the booster phase and the follow-up period to an ultimate loss of PTSD diagnosis by the end of the 6-month follow-up period; and non-responders (29%) who reported no significant symptom reduction over the course of the study. Unlike research from weekly PTSD treatment, baseline symptom severity did not predict treatment response. Instead, early treatment process variables, including between-session fear habituation from the first to the second imaginal exposure session, predicted treatment response (Hendriks et al., 2018). Brown and colleagues (2019) conducted a similar study examining treatment trajectories for individuals who received daily PE (M-PE) delivered over the course of 2 weeks, weekly PE delivered over the course of 8 weeks, or weekly Present Centered Therapy (PCT) delivered over the course of 8 weeks. For each of these treatments, five distinct trajectories were identified: rapid responder (7–17%; 16.8% M-PE); steep linear responder (14–22%; 18.8% M-PE); gradual responder (30–34%; 30.7% M-PE); non-responder (27–33%; 26.7% M-PE); and symptom exacerbation (7–13%; 6.9% M-PE) (Brown et al., 2019). Baseline clinical characteristics also did not predict group membership (Brown et al., 2019), suggesting that one-time assessments of individuals’ symptom severity prior to treatment may not be helpful in predicting response to intensive PTSD treatment.
Treatment response trajectories and their predictors for CPT-based intensive PTSD treatment programs (ITPs) for veterans have yet to be examined. We have previously demonstrated that participation in a 3-week CPT-based ITP, which combined daily individual and group CPT with daily adjunctive services, was well-tolerated (Held et al., 2019b) and associated with large reductions in PTSD symptoms in the short- and long-term (Zalta et al., 2018; Held et al., 2020b). It is likely that findings from previous research on intensive PE may not be directly applicable to such CPT-based ITPs due to the difference in treatment modality (i.e., PE vs. CPT), the delivery format (standalone evidence-based treatment vs. combining evidence-based treatment with adjunctive services) of ITPs, treatment lengths (1 vs. 2 vs. 3 weeks). This study’s primary aim was to identify treatment trajectories of symptom change among veterans who completed the 3-week CPT-based ITP for PTSD. Based on limited research on intensive PE (Brown et al., 2019; Hendriks et al., 2018), we expected to identify four distinct treatment trajectories (fast, slow, partial, and non-response). A secondary aim was to examine demographic and pre-treatment clinical variables, such as PTSD, depression, alcohol use severity, and negative posttrauma cognitions, as predictors of treatment trajectory group membership, as has been shown in previous research (e.g., Dewar et al., 2020). Better understanding and being able to predict response trajectories could allow for individualized and personalized approaches to intensive treatment for PTSD. Such personalization might include adjusting treatment length or changing the treatment approach during treatment if an individual is predicted to be minimally or non-response to treatment in order to achieve improved outcomes.
Method
Participants
Data were collected from 452 service members (n = 15) and veterans (n = 437; hereafter collectively referred to as veterans) who completed a 3-week CPT-based ITP for PTSD between April 2016 and February 2020. Completion rates for the ITP are high (90.8%) and individuals who completed the ITP and were included in this study did not statistically differ on the baseline PTSD Checklist for DSM-5 rating from those who did not (d=0.18; p=.34). On average, veterans in the sample were 41.44 years old (SD=9.45, range: 24-74 years), 65.93% identified as male, and 68.36% identified as White. Demographic and military-related characteristics can be found in Table 1.
Table 1.
Demographic characteristics for the total sample and by identified trajectory group
| Total Sample | Fast Responders |
Steady Responders |
Partial Responders |
Minimal Responders |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | % | n | % | n | % | n | % | n | % |
| Sex | ||||||||||
| Male | 298 | 65.93 | 48 | 73.85 | 97 | 62.58 | 109 | 68.55 | 44 | 60.27 |
| Female | 154 | 34.07 | 17 | 26.15 | 58 | 37.42 | 50 | 31.45 | 29 | 39.63 |
| Ethnicity | ||||||||||
| Hispanic | 87 | 19.25 | 15 | 23.08 | 34 | 21.94 | 27 | 16.98 | 11 | 15.07 |
| Not Hispanic or Latinx | 365 | 80.75 | 50 | 76.92 | 121 | 78.06 | 132 | 83.02 | 62 | 84.93 |
| Race | ||||||||||
| American Indian/Alaskan Native | 9 | 2.99 | 2 | 2.94 | 2 | 1.14 | 3 | 2.01 | 2 | 3.08 |
| Asian | 6 | 1.33 | 1 | 1.47 | 3 | 1.70 | 1 | 0.70 | 1 | 1.54 |
| Black or African American | 89 | 19.69 | 11 | 16.18 | 31 | 17.61 | 27 | 18.88 | 20 | 30.77 |
| Native Hawaiian/Pacific Islander | 3 | 0.66 | 0 | 0 | 1 | 0.57 | 2 | 1.40 | 0 | 0 |
| Other | 36 | 7.96 | 4 | 5.88 | 15 | 8.52 | 13 | 9.09 | 4 | 6.15 |
| White | 309 | 68.36 | 50 | 73.53 | 124 | 70.45 | 97 | 67.83 | 38 | 58.46 |
| Marital Status | ||||||||||
| Divorced | 94 | 20.80 | 17 | 25.00 | 32 | 18.18 | 29 | 20.28 | 16 | 24.61 |
| Domestic Partner | 1 | 0.22 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1.54 |
| Legally separated | 20 | 4.42 | 2 | 2.94 | 6 | 3.41 | 8 | 5.59 | 4 | 6.15 |
| Married | 242 | 53.54 | 40 | 58.82 | 102 | 57.95 | 72 | 50.35 | 28 | 43.08 |
| Single | 93 | 20.58 | 8 | 11.76 | 36 | 20.45 | 33 | 23.08 | 16 | 24.62 |
| Widowed | 2 | 0.44 | 1 | 1.47 | 0 | 0 | 1 | 0.70 | 0 | 0 |
| Military Service Branch | ||||||||||
| Air Force | 36 | 8.04 | 7 | 10.45 | 9 | 5.17 | 11 | 7.75 | 9 | 13.85 |
| Army | 297 | 66.29 | 41 | 61.19 | 120 | 68.97 | 97 | 68.31 | 39 | 60.00 |
| Coast Guard | 4 | 0.89 | 1 | 1.49 | 2 | 1.15 | 1 | 0.70 | 0 | 0 |
| Marines | 67 | 14.96 | 12 | 17.91 | 29 | 16.67 | 17 | 11.97 | 9 | 13.85 |
| Navy | 44 | 9.82 | 6 | 8.96 | 14 | 8.05 | 16 | 11.27 | 8 | 12.31 |
| Last/Current Military Pay Grade | ||||||||||
| E1 – E3 | 49 | 10.94 | 9 | 13.43 | 12 | 6.90 | 17 | 11.97 | 11 | 16.92 |
| E4 – E9 | 364 | 81.25 | 54 | 80.60 | 150 | 86.21 | 110 | 77.46 | 50 | 76.92 |
| Officer | 35 | 7.81 | 4 | 5.97 | 12 | 6.90 | 15 | 10.56 | 4 | 6.15 |
| Deployed | ||||||||||
| Yes | 93 | 21.01 | 9 | 13.85 | 39 | 25.16 | 30 | 18.87 | 17 | 23.29 |
| Cohort Type | ||||||||||
| Military Sexual Trauma | 155 | 34.29 | 21 | 32.31 | 55 | 35.48 | 47 | 29.56 | 32 | 43.84 |
Program Description
To determine suitability for the ITP, providers administered the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2018) to confirm a PTSD diagnosis during the intake evaluation. Exclusion criteria included requiring a higher level of care (e.g., active suicidality; a recent suicide attempt within the past three months; active homicidality; active psychosis; unmanaged mania; severe self-harming behaviors; high levels of active substance use or active eating disorders that would require medical attention) or other problems that would prevent full engagement in the ITP (e.g., serious health issues or legal problems).
Veterans were prospectively assigned to either a treatment cohort for PTSD secondary to combat or military sexual trauma (MST) based on the details of their index traumas. Veterans in either cohort type were provided with 14 daily 50-minute sessions of individual CPT, 13 daily 120-minute sessions of group CPT, 13 daily 75-minute group sessions of mindfulness, and 12 daily 50-minute group sessions of yoga along with other 50-minute educational classes on relevant topics, such as sleep hygiene and distress management.
Assessment Procedures
Data collection was approved by the Rush University Medical Center Institutional Review Board. A waiver of consent was obtained since all data collection occurred as part of routine clinical care. Self-report assessments were conducted electronically at intake (within two weeks before ITP start), during treatment, and at treatment endpoint.
Measures
Demographic and Military Characteristics.
At intake, veterans reported sex, age, race, ethnicity, cohort type (MST vs. combat trauma), education, service branch, and marital status.
The PTSD Checklist for DSM-5 (PCL-5).
The PCL-5 (Blevins et al., 2015) is a 20-item self-report measure of PTSD symptom severity based on DSM-5 diagnostic criteria, assessing intrusions, avoidance, negative cognition and mood, and hyperarousal symptoms (Blevins et al., 2015; Bovin et al., 2016; Wortmann et al., 2016). A recommended PCL-5 cutoff score of ≥ 33 indicates “probable PTSD” (Bovin et al., 2016), with higher scores indicating greater PTSD symptom severity. A 10-point change has been suggested as an indication of clinically meaningful change for a previous version of the instrument and was recommended on the website of the National Center for PTSD (https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp) when this manuscript was composed. The PCL-5 was administered at intake, on ITP days 2, 3, 5, 6, 8, 11, 13, and at post-treatment. Symptom severity was measured for the past month during the intake assessment and for the past week at each additional timepoint. Individuals were asked to rate their PTSD symptoms in relation to their index trauma they targeted during CPT. Internal reliability for the PCL-5 in the present sample ranged from .893-.962.
Clinician Administered PTSD Scale for DSM-5 (CAPS-5).
The CAPS-5 (Weathers et al., 2018) is a clinician-rated assessment to determine PTSD severity based on DSM-5 diagnostic criteria, assessing intrusions, avoidance, negative cognition and mood, and hyperarousal symptoms. Intake data were used for analyses. Higher CAPS-5 scores reflect greater PTSD symptom severity. Internal reliability for the CAPS-5 in the present sample was .785.
Patient Health Questionnaire (PHQ-9).
The PHQ-9 (Kroenke et al., 2001) is a 9-item self-report measure of depression symptoms occurring during the past two weeks. Intake data were used for analyses. Higher PHQ-9 scores reflect greater depression symptom severity. Internal reliability for the PHQ-9 in the present sample was .813.
Alcohol Use Disorder Identification Test (AUDIT-C).
The AUDIT-C (Bush et al., 1998) is a self-report measure of alcohol consumption during the past year that consists of the first three items of the standard 10-item AUDIT. Intake data were used for analyses. Higher AUDIT-C scores reflect greater alcohol consumption. Internal reliability for the AUDIT in the present sample was .871.
Posttraumatic Cognitions Inventory (PTCI).
The PTCI (Foa et al., 1999) is a 33-item self-report measure that assesses trauma-related cognitions including self-blame, negative cognitions about the self, and negative cognitions about others and the world. Intake data were used for analyses. Higher PTCI scores reflect greater negative posttrauma cognitions. Internal reliability for the PTCI in the present sample was .951.
Statistical Analyses
Group Based Trajectory Modeling (GBTM)1 was utilized to identify and define distinct groups based on trajectory of total PTSD symptoms measured repeatedly over the course of treatment, as well as predictors of trajectory group membership. This approach is based on finite mixture modeling, and probabilistically identifies latent clusters of individuals with similar trajectories over the course of the program. Estimation uses maximum likelihood based on a general quasi-Newton procedure (Jones & Nagin, 2012). As no generally conclusive method of determining true number of trajectories exists, and prior work has suggested a tendency for fit indices to over or under-estimate classes (e.g., Henson et al., 2007), a priori theory and clinical judgment were strongly considered in evaluating trajectory makeup, as generally suggested (e.g., Bauer & Curran, 2003; Muthén, 2003; Nagin, 2005; van der Nest et al., 2020). Demonstration of adequate trajectory membership as well as Akaike’s Information Criterion (AIC), and Bayesian Information Criterion (BIC) were explored as well in assessing trajectory number and shape. Trajectory adequacy was assessed based on Nagin’s (2005) guidelines that average posterior probabilities of group membership should exceed .70 and odds of correct classification should exceed 5. GBTM assumes data are missing at random (MAR), which has been supported in prior analyses of ITP outcomes (Held et al., 2020b). Baseline measurements were assessed as time-invariant predictors as well as demographic variables: age, race, ethnicity, sex, military service branch, cohort type (MST or combat trauma), education level, and marital status. Due to the exploratory nature of this research as well as existence of predictors that are often closely correlated, each covariate was initially examined individually as a predictor of trajectory membership prior to creation of adjusted models including relevant predictors. Following examination of each predictor in unadjusted models, we included all significant predictors in an adjusted model. Baseline predictors of trajectory membership in GBTM are examined with a generalized logit function and change in BIC was also assessed to compare improvement in model fit when including predictors in the presence of others. All analyses were conducted in Stata version 15.
Results
In total, 72.92% of individuals reported clinically meaningful PTSD symptom reductions (i.e., 10-point PCL-5 change), and 50.62% of veterans fell below the “probable PTSD” cutoff by the completion of treatment.
Trajectory Groups
A 4-trajectory model was selected based on prior theory and similarity to expected group composition, and AIC & BIC analyses clearly supported quadratic curvature for all trajectories. Average posterior probabilities of group membership exceeded .90 and odds of correct classification exceeded 10, supporting model adequacy based on Nagin's (2005) guidelines. Table 1 illustrates demographic makeup of each trajectory group. Figure 1 illustrates trajectories and confidence intervals. Trajectories represented fast responders, steady responders, partial responders, and minimal responders. Each group was labeled based on the speed and overall amount of the reported PCL-5 symptom reduction during the ITP. Groups differed significantly on baseline total PTSD symptom severity, with those that experienced more rapid and substantial amounts of PTSD symptom reductions reporting significantly lower baseline PTSD symptoms compared to groups that experienced less change. Similarly, aside from the fast and steady responder groups, the different trajectory groups also reported significantly different PTSD symptom severity at post-treatment (see Table 2).
Figure 1. Intensive PTSD treatment response trajectories.
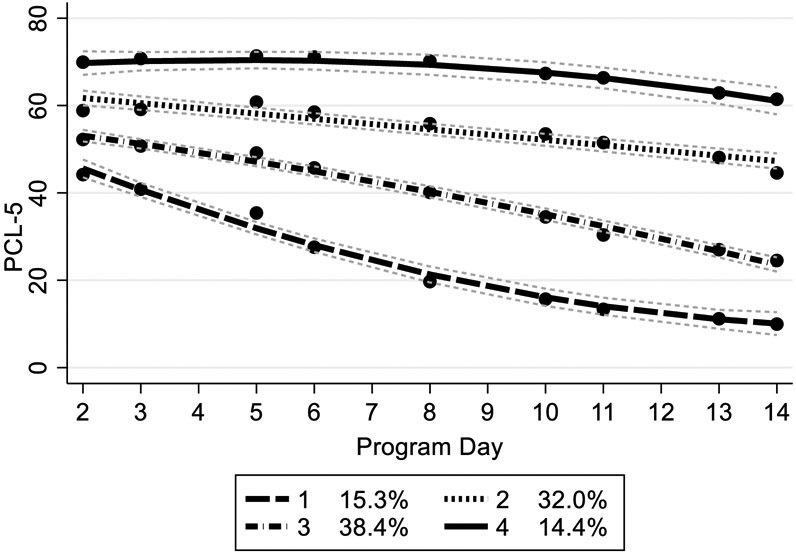
Note: Trajectory 1: Fast Responders. Trajectory 2: Partial Responders. Trajectory 3: Steady Responders. Trajectory 4: Minimal Responders. Predicted and observed trajectory values, with 95% confidence intervals. PCL-5 refers to PTSD Checklist for DSM-5 total score.
Table 2.
PTSD symptom severity by trajectory group
| Measure | Fast Responders |
Steady Responders |
Partial Responders |
Minimal Responders |
|---|---|---|---|---|
| (n = 65) | (n = 155) | (n = 159) | (n = 73 | |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Baseline PCL-5 | 46.37 (14.08) | 52.87 (10.43) | 56.55 (9.82) | 68.47 (6.96) |
| Endpoint PCL-5 | 9.46 (6.40) | 23.62 (9.81) | 42.17 (12.12) | 60.89 (11.16) |
| Overall PCL-5 Change | 37.30 (16.44) | 29.29 (16.05) | 14.14 (15.77) | 7.41 (13.27) |
Note. PCL-5 refers to PTSD Checklist for DSM-5 total score.
Fast and steady responders reported nearly identical overall symptom reductions (see Table 2). Fast responders reported a rapid symptom reduction of 19.83 points on average on the PCL-5 in a single week, whereas steady responders needed an additional two weeks to reach a similar symptom reduction. Both fast and steady responders experienced a substantial symptom reduction (average PCL-5 symptom reduction; fast responders:37.30 (SD=16.44); steady responders:29.29 (SD=16.05) that resulted in them falling below the “probable PTSD” threshold. Partial responders experienced a large and clinically meaningful reduction in their PTSD symptoms. However, unlike the fast and steady responders, they continued to screen positive for “probable PTSD” post-treatment. Partial responders tended to first report symptom reductions starting in the second ITP week, following which their rate of symptom change at this time was comparable to steady responders. Notably, individuals in the partial responder trajectory reported significantly greater baseline PTSD severity compared to fast and steady responders, suggesting that these individuals require much larger symptom reductions in order to reach the “probable PTSD” threshold. The minimal responders reported the most severe baseline PTSD symptoms and reported the least amount of overall change. Despite minimal symptom reductions, individuals in this trajectory group continued to report high PTSD symptoms at post-treatment.
Predictors of Trajectory Group Membership
Baseline scores for the CAPS-5 and PCL-5 subscales, PHQ-9, and PTCI, as well as numerous demographic variables were significant predictors of trajectory membership in unadjusted models (ps<.001). Lower scores in all clinical predictors significantly predicted membership in trajectories with greater improvement over time, with differences between all trajectory groups reaching significance at the p<.05 level for all predictors when examined individually. Initial analyses indicated that sex (p=.146), age (p=.224), race (p=.187), ethnicity (p=.190), cohort type (p=.130), education (p=.577), service branch (p=.919), alcohol use/abuse (p=.133) and marital status (p=.095) were not significant predictors of trajectory membership.
In adjusted models, total baseline PTCI severity significantly predicted trajectory membership (p<.001). Higher baseline PTCI predicted being in a worse trajectory (i.e., a group with less rapid and smaller overall symptom reductions) across all comparisons except partial and minimal response trajectories (see Supplementary Table 1). PCL-5 Intrusions, PCL-5 Negative Cognitions and Mood, and PCL-5 Hyperarousal were significant predictors of trajectory membership in all adjusted models. Higher scores on the PCL-5 Intrusions, Negative Cognitions and Mood, and Hyperarousal subscales differentiated membership in the minimal responder group relative to other trajectory groups (ps<.05), though they did not predict differences between the other three trajectory groups. PCL-5 Avoidance was not significant when adjusting for other baseline PCL-5 subscales (p=.647) in the adjusted model. CAPS-5 Intrusions (p=.023) and CAPS-5 Avoidance (p=.029) subscales were significant predictors of trajectory, though they only differentiated the fast responders from steady responders. Total baseline PHQ-9 severity (p=.054), CAPS-5 Negative Cognitions and Mood (p=.206) and Hyperarousal (p=.655) subscales, and AUDIT-C (p=.288) did not improve model fit in adjusted models including other clinical covariates.
Discussion
Although prior research demonstrated that participation in a 3-week CPT-based ITP was associated with large symptom reductions, not all veterans responded to treatment equally. In line with research on intensive treatments, the present study identified four distinct treatment response trajectories: Fast responders (15.3%), steady responders (32.0%), partial responders (38.4%), and minimal responders (14.4%). Overall, the present findings are consistent with prior research noting that many individuals who completed PTSD treatments delivered weekly experienced significant improvement (Elliott et al., 2005; Galovski et al., 2016; Schumm et al., 2013; Stein et al., 2012). Study results are also consistent with previous research suggesting that participants with the most severe PTSD symptoms exhibited the least amount of change during CPT and those entering treatment with less severe PTSD symptom severity exhibited increasingly greater change during CPT (Schumm et al., 2013). Despite vastly different treatment structures and treatment content between Hendriks and colleagues’ (2018) intensive PE treatment and the present study (i.e., 1-week of standalone PE plus booster vs. 3-week CPT plus adjunctive services in an ITP), the identified trajectory group distributions into fast (13% vs. 14.38%), slow/steady (26% vs. 31.42%), partial (32% vs. 38.50%), and non-/minimal responder groups (29% vs. 14.38%) were similar. Importantly, the present study examined trajectories over the course of CPT, whereas Hendricks and colleagues (2018) examined trajectories during active treatment, four weekly 90-minute booster sessions, and follow-up assessments. Compared to those found by Hendriks and colleagues’ (2018) and Brown and colleagues’ (2019) we identified a lower number of minimal responders, which may be related to differences in treatment modality (CPT vs. PE), the spacing of sessions (1 daily 50-minute individual CPT session plus 1 daily 120-minute group CPT session as well as adjunctive services vs. 3 daily individual 90-minute PE sessions vs. 1 daily individual 90-minute PE session), and the general treatment length (3 weeks vs. 1 weeks vs. 2 weeks). The identified 4-trajectory model is slightly more nuanced and differs from the 3-trajectory model observed in weekly treatment (responder, non-responder, and sub-threshold groups) (e.g., Allan et al., 2017; Clapp et al., 2016; Dewar et al., 2020; Galovski et al., 2016). Difference may be explained by different samples (e.g., civilians; Galovski et al., 2016), varying timeframes (e.g., 2-years after treatment completion; Elliot et al., 2005), and different treatment formats (e.g., weekly treatment; Elliot et al., 2005; Galovski et al., 2016; Schumm et al., 2013).
A secondary goal of the present study was to evaluate various demographic and baseline clinical predictors of the response trajectories. Baseline negative posttrauma cognitions as well as self-reported and clinician-rated PTSD severity were identified as predictors of ITP trajectory group membership. Only negative posttrauma cognitions successfully distinguished membership across all the different trajectory groups. This finding aligns with research identifying change in negative posttrauma cognitions as a key factor associated with PTSD symptom change in weekly treatment (Zalta et al., 2015). Similar to what can be observed in weekly treatment, individuals who hold negative beliefs less tightly or have fewer negative posttrauma cognitions overall may also find it easier to challenge these beliefs, which would result in more rapid response in a primarily cognitive treatment such as the ITP.
Only higher self-reported intrusions, cognitions and mood, and hyperarousal symptoms increased the likelihood that individuals were minimal responders. Self-reported avoidance symptoms did not significantly predict membership in any of the trajectory groups, possibly due to avoidance being a hallmark PTSD symptom that is present in all participants, thus lacking sufficient variability to function as a successful predictor. Finally, clinician-rated intrusion and avoidance symptom severity helped to distinguish fast from steady responders. Thus, objectively rated avoidance may be used to preemptively identify individuals who are likely to exhibit a faster ITP response. Individuals with higher clinician-rated avoidance at the onset of treatment may benefit from discussing the role of avoidance in symptom maintenance and identifying and developing a plan to change frequently employed avoidance strategies.
Unlike in studies examining treatment trajectories for weekly PTSD treatments (Dewar et al., 2020; Schumm et al., 2015), clinical variables, such as depression severity and alcohol use, demographic variables, or cohort type (military sexual trauma vs. combat trauma) did not emerge as significant predictors of trajectory groups. These findings resemble those from prior research (Hendriks et al., 2018; Brown et al., 2019) which indicated that most of the demographic or clinical variables were not statistically significant predictors of trajectory group membership and suggested that individuals with a range of comorbid concerns can benefit from intensively delivered PTSD treatments.
Several limitations must be considered. First, the sample was limited to veterans with PTSD who sought treatment via a 3-week ITP that involved a multitude of treatment components, limiting the study’s generalizability to other populations and programs that use different timeframes, structures, and content. Second, the present study evaluated treatment trajectories as part of a clinical program lacking many of the controls found in clinical trials. Although this may increase the generalizability of findings to other practice settings, differences across several providers and the lack of close treatment monitoring may account for some of the variance in individuals’ treatment responses. Third, aside from the CAPS-5 at intake, all assessments administered during the program were limited to self-report measures, which may have introduced additional bias. For example, it is possible that as some individuals may have felt better quickly, they may have overreported how much better they felt, and vice versa. Additionally, the PCL-5 assessed symptoms experienced over the past week, which may have been confusing given the daily sessions. This may have led individuals to report symptoms since the last session and affected trajectory analyses. Fourth, most variables that were examined as potential predictors of trajectory group membership were also self-reports and thus may introduce error due to shared method variance. Alcohol use was captured over the past year and alcohol or substance use at the time of the start of the program was not assessed. Finally, trajectory modelling generally involves some degree of uncertainty regarding number of trajectories, due to lack of generally agreed-upon metrics for selection. Correspondingly, findings across studies are often divergent due to differences in apriori theory and analytic approach, as has been noted elsewhere (e.g., Frankfurt et al., 2016). Here, information criteria-based metrics generally favored models with the lowest number of trajectories, despite clinical criteria and model adequacy indices supporting more.
Overall, the identification of four different response trajectories supports the importance of evaluating individual- and group-level treatment responses. Having information to predict the trajectory an individual will likely fall into during treatment can be important for clinicians and may help them plan or even adjust treatment, as necessary. Additional research is needed to accurately classify individuals into treatment response trajectories prior to the initiation of treatment. Future research should evaluate process-based variables, such as the ability to identify treatment targets (e.g., maladaptive beliefs) prior to or during early phases of treatment that may slow down the therapeutic process or the ability to establish a strong working alliance with the treating clinician. Future studies should also evaluate whether flexing the structure of intensive PTSD treatment (Galovski et al., 2012) can improve outcomes for the different groups. For example, extending ITPs may help partial responders experience additional symptom reductions and possibly experience a full remission of PTSD symptoms; offering shorter programming may be sufficient for fast responders. Finally, it will be important to examine whether individuals who are classified as minimal responders could benefit from other intensive treatments (e.g., intensive PE) or from programs that involve different treatment components, or whether these are individuals who generally do not respond to intensive PTSD treatment. Given the vastly different approaches to intensive PTSD treatment and the multitude of treatment components that are offered during ITPs, it will initially be critical to identify predictors of different treatment trajectories for specific programs. With an increasing number of ITPs being developed and systematically evaluated, it will eventually be possible and important to identify characteristics that make individuals good fits for intensive PTSD treatment in general as well as identify optimal candidates for the specific programs.
Supplementary Material
Acknowledgments
We thank the Wounded Warrior Project for their support of the Warrior Care Network and the resulting research. We would also like to thank the participating veterans and their families, as well as acknowledge the administrators, research assistants, and clinicians at the Road Home Program.
Philip Held is supported by a career development award from the National Institute of Health’s National Center for Advancing Translational Sciences (5KL2TR002387-04) and receives grant support from Wounded Warrior Project and RTI International. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Wounded Warrior Project, or any other funding agency.
Footnotes
Declaration of Interest
All other authors declare that they have no competing interests.
Due to the assumption of GBTM that equal error variances are constant over time we also explored trajectory models using Growth Mixture Modeling, which relaxes this assumption and allows for random effects. Results were similar and confirmed the superior fit of the 4-trajectory model via BIC values as well as supporting the utility of PTCI and baseline PCL-5 subscales to predict trajectory membership. As such, only GBTM models are reported here.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allan NP, Gros DF, Myers US, Korte KJ, & Acierno R (2017). Predictors and outcomes of growth mixture modeled trajectories across an exposure-based PTSD intervention with veterans. Journal of Clinical Psychology, 73(9), 1048–63. doi: 10.1002/jclp.22408 [DOI] [PubMed] [Google Scholar]
- Bauer D, & Curran P (2003b). Overextraction of latent trajectory classes: Much ado about nothing? Reply to Rindskopf (2003), Muthén (2003), and Cudeck and Henly (2003). Psychological Methods, 8, 384–393. doi: 10.1037/1082-989X.8.3.384 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Brown LA, Clapp JD, Kemp JJ, Yarvis JS, Dondanville KA, Litz BT, … & Foa EB (2019). The pattern of symptom change during prolonged exposure therapy and present-centered therapy for PTSD in active duty military personnel. Psychological Medicine, 49(12), 1980–1989. doi: 10.1017/S0033291718002714 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Leifker FR, Rozek DC, Bryan AO, Reynolds ML, Oakey DN, & Roberge E (2018). Examining the effectiveness of an intensive, 2-week treatment program for military personnel and veterans with PTSD: Results of a pilot, open-label, prospective cohort trial. Journal of Clinical Psychology, 74(12), 2070–2081. doi: 10.1002/jclp.22651 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. JAMA Internal Medicine, 158(16), 1789–95. doi: 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- Clapp JD, Kemp JJ, Cox KS, & Tuerk PW (2016). Patterns of change in response to prolonged exposure: Implications for treatment outcome. Depression and Anxiety, 33(9), 807–15. doi: 10.1002/da.22534 [DOI] [PubMed] [Google Scholar]
- Dewar M, Paradis A, & Fortin CA (2020). Identifying trajectories and predictors of response to psychotherapy for post-traumatic stress disorder in adults: A systematic review of literature. The Canadian Journal of Psychiatry, 65(2), 71–86. doi: 10.1177/0706743719875602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, Albert I, … Clark DM (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry, 171(3), 294–304. doi: 10.1176/appi.ajp.2013.13040552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott P, Biddle D, Hawthorne G, Forbes D, & Creamer M (2005). Patterns of treatment response in chronic posttraumatic stress disorder: An application of latent growth mixture modeling. Journal of Traumatic Stress, 18(4), 303–311. doi: 10.1002/jts.20041 [DOI] [PubMed] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO, & Rauch SAM (2019). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences, second edition. New York, NY: Oxford University Press. [Google Scholar]
- Foa EB, McLean CP, Zang Y, Rosenfeld D, Yadin E, Yarvis JS, … Peterson AL (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. JAMA, 319(4), 354–364. doi: 10.1001/jama.2017.21242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankfurt S, Frazier P, Syed M, & Jung KR (2016). Using group-based trajectory and growth mixture modeling to identify classes of change trajectories. The Counseling Psychologist, 44(5), 622–660. doi: 10.1177/0011000016658097 [DOI] [Google Scholar]
- Galovski TE, Blain LM, Mott JM, Elwood L, & Houle T (2012). Manualized therapy for PTSD: flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology, 80(6), 968–81. doi: 10.1037/a0030600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Harik JM, Blain LM, Farmer C, Turner D, & Houle T (2016). Identifying patterns and predictors of PTSD and depressive symptom change during cognitive processing therapy. Cognitive Therapy and Research, 40(5) 617–26. doi 10.1007/s10608-016-9770-4 [DOI] [Google Scholar]
- Goetter EM, Blackburn AM, Stasko C, Han Y, Brenner LH, Lejeune S, Tanev KS, Spencer TJ, & Wright EC (2020). Comparative effectiveness of prolonged exposure and cognitive processing therapy for military service members in an intensive treatment program. Psychological Trauma: Theory, Research, Practice, and Policy. Advance online publication. doi: 10.1037/tra0000956 [DOI] [PubMed] [Google Scholar]
- Harvey MM, Petersen TJ, Sager JC, Makhija-Graham NJ, Wright EC, Clark EL, … Simon NM (2018). An intensive outpatient program for veterans with posttraumatic stress disorder and traumatic brain injury. Cognitive and Behavioral Practice, 26(2), 323–34. doi: 10.1016/j.cbpra.2018.07.003 [DOI] [Google Scholar]
- Held P Bagley JM, Klassen BJ, & Pollack MH (2019a). Intensively delivered cognitive-behavioral therapies: An overview of a promising treatment delivery format for PTSD and other mental health disorders. Psychiatric Annals, 49(8), 339–42. doi: 10.3928/00485713-20190711-01 [DOI] [Google Scholar]
- Held P, Klassen BJ, Boley RA, Wiltsey Stirman S, Smith DL, Brennan MB, … Zalta AK (2019b). Feasibility of a 3-week intensive treatment program for service members and veterans with PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 422–30. doi: 10.1037/tra0000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Held P, Klassen BJ, Small CF, Brennan MB, Van Horn R, Karnik NS, … & Zalta AK (2020a). A case report of cognitive processing therapy delivered over a single week. Cognitive and Behavioral Practice, 27(2), 126–135. doi: 10.1016/j.cbpra.2019.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Held P, Zalta AK, Smith DL, Bagley JM, Steigerwald VL, Boley RA, … Pollack MH (2020b). Maintenance of treatment gains up to 12-months following a three-week cognitive processing therapy-based intensive PTSD treatment program for veterans. European Journal of Psychotraumatology. doi: 10.1080/20008198.2020.1789324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks L, Kleine R. A. d., Broekman TG, Hendriks G, & van Minnen A (2018). Intensive prolonged exposure therapy for chronic PTSD patients following multiple trauma and multiple treatment attempts. European Journal of Psychotraumatology, 9(1), 1425574. doi: 10.1080/20008198.2018.1425574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson JM, Reise SP, & Kim KH (2007). Detecting mixtures from structural model differences using latent variable mixture modeling: A comparison of relative model fit statistics. Structural Equation Modeling, 14(2), 202–226. doi: 10.1080/10705510709336744 [DOI] [Google Scholar]
- Jones BL, & Nagin DS (2012). A stata plugin for estimating group-based trajectory models. https://www.andrew.cmu.edu/user/bjones/ [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B (2003). Statistical and substantive checking in growth mixture modeling: Comment on Bauer & Curran (2003). Psychological Methods, 8, 369–377. doi: 10.1037/1082-989X.8.3.369 [DOI] [PubMed] [Google Scholar]
- Nagin DS (2005). Group-based modeling of development. Cambridge, MA: Harvard University Press. [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2016). Cognitive processing therapy for PTSD: A comprehensive manual. New York, NY: Guilford Press. [Google Scholar]
- Schumm JA, Walter KH, & Chard KM (2013). Latent class differences explain variability in PTSD symptom changes during cognitive processing therapy for veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 5(6), 536–544. doi: 10.1037/a0030359 [DOI] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, & Marmar CR (2015). Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA, 314(5), 489–500. doi: 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- Stein NR, Dickstein BD, Schuster J, Litz BT, & Resick PA (2012). Trajectories of response to treatment for posttraumatic stress disorder. Behavior Therapy, 43(4), 790–800. doi: 10.1016/j.beth.2012.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Nest G, Passos VL, Candel MJ, & van Breukelen GJ (2020). An overview of mixture modelling for latent evolutions in longitudinal data: Modelling approaches, fit statistics and software. Advances in Life Course Research, 43, 100323. doi: 10.1016/j.alcr.2019.100323 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, … Marx BP (2018). The clinician-administered PTSD scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. doi: 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, … Hembree EA (2016). Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. doi: 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Zalta AK (2015). Psychological mechanisms of effective cognitive–behavioral treatments for PTSD. Current Psychiatry Reports, 17(4), 23. doi: 10.1007/s11920-015-0560-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta AK, Held P, Smith DL, Klassen BJ, Lofgreen AM, Normand PS, … Karnik NS (2018). Evaluating patterns and predictors of symptom change during a three-week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18(1), 242. doi: 10.1186/s12888-018-1816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


