Abstract
Rationale
Countries worldwide rely on the COVID-19 vaccine to contain the spread of the pandemic. However, because of the inequality in distribution, people in many demographic groups and regions still do not have access to a safe and effective COVID-19 vaccine.
Objective
To aid vaccine promotion campaigns that target populations with different access to the COVID-19 vaccine, this study examined how vaccine availability and vaccination intention influence people's consideration of the COVID-19 vaccine.
Method
We conducted a two-wave longitudinal survey and choice-based conjoint experiment to examine the influence of vaccine availability and vaccination intention on perceived barriers of vaccination (e.g., safety and cost concern) and preference in different vaccine features (e.g., FDA approval status and number of doses administered).
Result
We found that low availability and intention increased attention to global behavioral barriers such as safety concern and high-level vaccine attributes such as efficacy. In contrast, high availability articulates practical considerations such as cost and logistics associated with vaccination.
Conclusion
Based on such findings, we conclude that health communicators need to strategically customize their messages based on audience access to the COVID-19 vaccine and their intention to get vaccinated. Highlighting the safety and effectiveness of the vaccine may be more effective in low-accessibility and low-intention groups, while emphasis on practical considerations such as vaccine cost and logistics may be more effective in high-accessibility and high-intention groups.
Keywords: COVID-19, Vaccine, Conjoint analysis, Psychological distance, Construal level
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has taken a toll on societies worldwide, leaving hundreds of millions infected and millions deceased (World Health Organization (WHO, 2021). Since the early stage of the pandemic, people have been expecting a safe and effective vaccine that reduce transmission of, and the mortality risk, of the disease. The outcome of a yearlong wait is encouraging. With multiple tested vaccines available to a growing number of people worldwide, the infection and death rates of COVID-19 in many countries have been decreasing since February 2021 (WHO, 2021). The development and approval of COVID-19 vaccines has been drastically faster in comparison to other vaccines (Slaoui and Hepburn, 2020). However, it took almost a year for the vaccines to become widely available, and the wait time was even longer for people in certain demographic groups and locations.
Although studies have identified the different factors associated with people's intention to get vaccinated for COVID-19 (Chu and Liu, 2021; Motta, 2021), to date, none has studied the implication of vaccine availability for the public acceptance of the COVID-19 vaccine. Considering that behavioral adoption is not a static process but involves different considerations at different stages (Prochaska and Velicer, 1997), understanding the impacts of vaccine availability is critical to prepare those who have yet to be eligible for a COVID-19 vaccine and keep the momentum among those eligible to receive a vaccine. From a broader perspective, as solutions to many health and environmental risks (e.g., novel energy sources and vaccines for cancer) are still under development and may take years to become available, examining the influence of COVID-19 vaccine availability helps determine effective communication strategies that promote continued public support for the development and implementation of risk solutions.
The construal level theory of psychological distance offers a useful perspective to explain the influence of vaccine availability (Trope and Liberman, 2010). According to the theory, psychological distance denotes the perceived distance between an observer and the target object on four interrelated dimensions, including spatial, temporal, social, and hypothetical dimensions. Change in one distance dimension often leads to variation in others. In terms of the COVID-19 vaccine, lower availability not only means that one gets a vaccine in the future (i.e., far temporal distance) but also increases the perceived social (i.e., people like me cannot receive a vaccine now), spatial (i.e., people in my area are not getting vaccinated), and hypothetical (i.e., the chance for me to receive a vaccine is low) distances of the COVID-19 vaccine.
Another proposition of the construal level theory is that change in an object's distance leads to variation in people's mental representation of such object (i.e., construal level). Specifically, distant objects are often construed abstractly (i.e., high construal level), while nearby objects are construed more concretely (i.e., low construal level). For instance, people tend to use more abstract language to describe events that took place in a distant than in nearby setting (Fujita et al., 2006). Because of the association between psychological distance and construal level, the theory suggests that people may respond to psychologically far or close stimuli differently because of different availability and accessibility of abstract and concrete cues. As a consequence, abstract consideration tends to exert stronger influence when the distance perception is far, while concrete concerns may carry more weight in decision-making processes involving short distance. For example, Liberman and Trope (1998) found that students preferred a convenient task (a concrete feature) over a rewarding one (an abstract feature) when the task would take place in the near future. However, their preference reversed when the temporal distance increased. A similar shift in preference was also observed when distance changes in other dimensions (Liviatan et al., 2008).
Based on the construal level theory, it is reasonable to suggest that availability of COVID-19 vaccines and the corresponding distance perception may also influence what people consider when contemplating a vaccine. In particular, when the COVID-19 vaccine is available to a person, concrete considerations may be more accessible in a person's construal of the vaccine. Abstract considerations may exert stronger influence when the vaccine is hard to obtain. Such possibility points to another important question: what are the concrete and abstract considerations of the COVID-19 vaccine? We argue that people's consideration of the COVID-19 vaccine can be examined from two perspectives, which are perceived barriers to getting the COVID-19 vaccine and characteristics of the COVID-19 vaccine.
Perceived barriers have long been studied as an integral components of health behavior theories such as the health belief model (HBM) (Janz and Becker, 1984). Perceived barrier was found to exert strong influence on people's intention to get different types of vaccines such as HPV and influenza vaccines (Brewer and Fazekas, 2007; Schmid et al., 2017). Previous studies often take a unidimensional approach to operationalize such construct. A single composite variable averaged from ratings of multiple perceived barriers (e.g., too busy to receive a vaccine, vaccine safety concern) is often included in analytical models instead of multiple variables, capturing different aspects of barriers (Allen et al., 2009; Weinstein, 1993). However, more recent studies propose a multidimensional model of perceived barriers (Gerend et al., 2013). Specifically, Gerend et al. (2013) argue that some barriers are more abstract and global (e.g., safety concern), while others are more concrete and practical (e.g., time constraint). Therefore, psychological distance should be positively associated with global barriers but negatively linked to practical barriers. Indeed, they identified three practical barriers (i.e., logistics, cost, and fear of shots) and two global barriers (i.e., safety concern and relevance of the vaccine) that exerted different influences on people's intention to receive an HPV vaccine.
Perceived barriers to receive a COVID-19 vaccine characterize people's consideration of their ability to perform the vaccination behavior. On the other hand, vaccine characteristics delineate individual perception of the vaccine itself. Similar to perceived barriers, perception of risk prevention measures such as vaccination has been studied in health behavior theories. For instance, the extended parallel process model (EPPM) captures perception of preventive solutions with response efficacy, that is, a solution's ability to prevent negative consequences (Witte, 1992). However, people's evaluation of vaccine goes beyond its efficacy in preventing diseases. For instance, recent studies show that people's evaluations of vaccines are determined by multiple factors such as cost, effectiveness, country of origin, and side effects (Kreps et al., 2020; Motta, 2021; Sun et al., 2020). Moreover, WHO's Strategic Advisory Group of Experts on vaccine hesitancy suggests that people's confidence in vaccine and the convenience of vaccination work together to shape their intention to get vaccinated (Schuster et al., 2015). Therefore, it is reasonable to believe that people's evaluation of vaccine may also be multidimensional, and different dimensions may associate differently with high or low construal level.
Specifically, construal level theory argues that high- and low-level features can be determined based on two criteria: centrality and subordination (Trope and Liberman, 2010). Centrality refers to high-level features' more dominant influence on the meaning of an object. For instance, a vaccine that is not safe may not be considered as a viable prevention against COVID-19, but a vaccine that costs more than others may still be attractive to many. On the other hand, subordination refers to low-level features' dependence on high-level features to create meaning. For instance, vaccine cost may be an important consideration when a vaccine is safe and effective, but vaccine safety and effectiveness are important to people regardless of its costs. Therefore, we argue that high-level features of a COVID-19 vaccine, such as safety, may weigh more in people's decision-making on vaccine when the psychological distance of COVID-19 vaccine is far. On the contrary, low-level characteristics, such as cost and logistics, may exert stronger impacts on people's vaccine preference when the distance is close.
Importantly, another factor that may also shape perceived distance and construal of COVID-19 vaccines is vaccination intention. Goal pursuit theories suggest that concrete cognition of the means to achieve a goal tend to be more accessible when the goal is active, that is, when the person intends to achieve such goal (Gerend et al., 2013). Therefore, a person who intends to get vaccinated may construe COVID-19 vaccines more concretely and perceive it as closer. To support this claim, studies have determined that people who intended to receive an HPV vaccine were more likely to cite practical concerns such as vaccine cost as a behavioral barrier, while those with lower intention were more likely to cite high-level barriers such as safety concerns (Gerend et al., 2013). Reciprocally, global and practical barriers also exerted different levels of influence on vaccination intention. Thus, we argue that, along with the vaccine availability, vaccination intention may influence people's consideration of abstract and concrete barriers or vaccine characteristics.
It is worth noting that psychological distance and construal level are not novel concepts in health research. Studies have long examined how proximal and distant health risks influence people's willingness to adopt preventive behaviors (Kim and Nan, 2019; Liu and Yang, 2020). However, most studies focused on the distance of risks, with few investigated the distance of solutions such as vaccine. Thus, the current study seeks to address this gap. We specifically ask three research questions:
RQ1. Do availability of the COVID-19 vaccine and intention to receive a COVID-19 vaccine influence people's perceived distance of the vaccine?
RQ2. Do availability of the COVID-19 vaccine and intention to receive a COVID-19 vaccine influence people's consideration of global and practical barriers of getting a COVID-19 vaccine?
RQ3. Do availability of the COVID-19 vaccine and intention to receive a COVID-19 vaccine influence people's consideration of high- and low-level characteristics of the COVID-19 vaccine?
To address these questions, we conducted a longitudinal survey and choice-based conjoint experiment that targeted two national samples. The longitudinal survey was fielded before and after COVID-19 vaccines became widely available in the United States. The conjoint experiment was conducted few months before the COVID-19 vaccine entered the U.S. market. We manipulated perceived availability of the COVID-19 vaccine and examined people's preference in vaccine characteristics with conjoint analysis.
2. Study 1
2.1. Sample
Upon approval from the Institutional Review Board at the lead author's institution, a sample of 934 participants was recruited from an online panel managed by Prolific.co between September 5 and 8, 2020. A total of 1001 participants started the survey. Responses from those who passed the attention check questions and did not contract COVID-19 nine months prior to taking the survey were retained. The age and gender composition of the sample is representative of the U.S. population (Table 1 ; U.S. Census Bureau, 2019). Six months after the first survey (March 23–29, 2021), the participants who completed the wave 1 questionnaire were invited to participate in a follow-up survey. A total of 554 participants responded to the second survey. They were asked to provide their age and gender to ensure that the same person was taking time 2 questionnaire. Responses from those who provided different age or gender were dropped, resulting in a sample of 534 participants (response rate = 56.6%). Among those who completed the second survey, 199 have received at least one dose of a COVID-19 vaccine, with 37 scheduled to receive a vaccine soon. There were 291 participants who reported that they have not received any COVID-19 vaccine, and their responses were used in the repeated measure analyses. There was no significant difference in age, gender, race, and income between time 1 and final sample. However, participants retained in the final sample were slightly less educated than those in time 1 sample (χ2 [7] = 21.39, p < 0.01). The observed power of the statistical analyses ranges from 0.980 to 1.00 (α = 0.95). Informed consent was obtained from all participants included in the study. A link to the data collected in this study is in the supplementary file.
Table 1.
Sample demographics.
| Study 1 (Time 1 Survey) |
Study 1 (Time 2 Survey) |
Study 2 |
|
|---|---|---|---|
| Sample percentage or Mean (Standard Deviation) | |||
| Age | 46.01 (16.17) | 46.91 (14.26) | 46.45 (17.2) |
| Gender | |||
| Female | 50.1% | 51.5% | 50.8% |
| Male | 48.7% | 47.4% | 49.2% |
| Other | 1.2% | 1.0% | – |
| Race | |||
| Non-Hispanic White or Caucasian | 74.7% | 73.5% | 60.9% |
| Non-Hispanic Black or African American | 12.2% | 14.4% | 13.2% |
| Hispanic or Latino | 3.6% | 3.1% | 18.3% |
| Asian, Pacific Islander, Native American | 7.3% | 6.9% | 6.1% |
| Other | 2.1% | 2.1% | 1.5% |
| Education | |||
| Less than High School | 0.6% | 1.0% | 15.0% |
| High School/GED | 12.4% | 14.1% | 27.9% |
| Some College | 23.3% | 26.5% | 14.0% |
| 2-year College Degree | 9.7% | 13.7% | 8.4% |
| 4-year College Degree | 33.7% | 29.9% | 18.6% |
| Graduate Degree | 20.3% | 14.8% | 16.1% |
| Income | |||
| Below $35,000 | 31.3% | 35.7% | 28.3% |
| $35,000 - $49,999 | 13.8% | 14.4% | 12.4% |
| $50,000 - $74,999 | 21.0% | 21.3% | 18.2% |
| $75,000 - $99,999 | 14.0% | 10.0% | 12.2% |
| $100,000 and above | 19.9% | 18.5% | 28.9% |
2.2. Procedure
The means and standard deviations of the measurement items and scale reliability are reported in Table 2 . In summary, time 1 survey measured participants’ demographics, perceived availability and distance of the COVID-19 vaccine, perceived barriers to receiving a vaccine, and intention to receive a COVID-19 vaccine. Those who have not received or scheduled a COVID-19 vaccine were asked to indicate their perceived availability of COVID-19 vaccine and barriers that may prevent them from getting a COVID-19 vaccine at time 2. As expected, participants perceived a COVID-19 vaccine as more available at time 2 than at time 1 (F [1, 193] = 83.90, η 2 = 0.303; time 1: M = 3.24, SD = 0.87; time 2: M = 2.44, SD = 0.97).
Table 2.
Measurement.
| Measurement | Study 1 (Time 1) |
Study 1 (Time 2) |
Study 2 |
|||
|---|---|---|---|---|---|---|
| M (SD) or percentage | α | M (SD) | α | M (SD) | α | |
| Perceived availability | ||||||
| On the scale of 1–5, how soon or far in the future do you think the COVID-19 vaccine will be available to you? (1 = very soon; 5 = very far) | 3.23 (0.84) | – | 2.44 (0.97) | – | 3.23 (1.13) | – |
| Perceived distance | ||||||
| Temporal distance | 3.16 (0.76) | 0.77 | – | – | 3.11 (0.84) | 0.70 |
| Please indicate how much you agree or disagree with the following statement: The COVID-19 vaccine will be available to me very soon. (reverse coded) (1 “strongly disagree” to 5 “strongly agree) | 3.47 (0.88) | – | – | – | 3.04 (1.06) | – |
| The COVID-19 vaccine will NOT be available to me until very far in the future. | 2.85 (0.96) | – | – | – | 3.01 (1.10) | – |
| I will have to wait for a long time before the COVID-19 vaccine become available to me. | 3.18 (0.91) | – | – | – | 3.29 (1.03) | – |
| Hypothetical distance | 2.92 (0.85) | 0.78 | – | – | 2.89 (0.79) | 0.65 |
| I am uncertain whether the COVID-19 vaccine will be available to me. | 2.96 (1.07) | – | – | – | 2.99 (1.11) | – |
| It is hard to predict whether the COVID-19 vaccine will be available to me. | 3.27 (1.08) | – | – | – | 3.34 (1.07) | – |
| I am certain that the COVID-19 vaccine will be available to me. (reverse coded) | 2.53 (0.92) | – | – | – | 2.34 (0.92) | – |
| Spatial distance | 2.25 (0.67) | 0.77 | – | – | 2.41 (0.70) | 0.58 |
| The COVID-19 vaccine will likely be available in my area. (reverse coded) | 2.14 (0.74) | – | – | – | 2.20 (0.85) | – |
| People in my neighborhood will likely be able to get the COVID-19 vaccine. (reverse coded) | 2.31 (0.76) | – | – | – | 2.34 (0.89) | – |
| The COVID-19 vaccine will likely be only available in places far away from my community. | 2.30 (0.93) | – | – | – | 2.70 (1.11) | – |
| Social distance | 2.34 (0.70) | 0.8 | – | – | 2.43 (0.73) | 0.63 |
| The COVID-19 vaccine will likely be available to people like me. (reverse coded) | 2.23 (0.80) | – | – | – | 2.23 (0.89) | – |
| It will be hard for people like me to get the COVID-19 vaccine. | 2.52 (0.93) | – | – | – | 2.77 (1.10 | – |
| The COVID-19 vaccine will likely be available to my family and friends. (reverse coded) | 2.26 (0.74) | – | – | – | 2.30 (0.87) | – |
| Perceived barriers | ||||||
| Global barrier | ||||||
| Safety concern | 3.31 (1.23) | 0.88 | 2.82 (1.51) | 0.94 | – | – |
| When the COVID-19 vaccine is available to you, how much would the following factors prevent you from getting the COVID-19 vaccine? - Concerns about whether the COVID-19 vaccine is safe. (1 “very little” to 5 “a great deal”) | 3.39 (1.38) | – | 2.82 (1.59) | – | – | – |
| Not enough research done on the COVID-19 vaccine | 3.36 (1.36) | – | 2.68 (1.60) | – | – | – |
| I have concerns about possible side effects of the COVID-19 vaccine | 3.18 (1.37) | – | 2.97 (1.58) | – | – | – |
| Relevance | ||||||
| I don't think I need a COVID-19 vaccine | 1.57 (1.13) | – | 1.90 (1.38) | – | – | – |
| Practical Barriers | ||||||
| Fear of shot | 1.37 (0.72) | 0.78 | 1.39 (0.71) | 0.77 | – | – |
| I'm worried it may hurt a lot to receive the COVID-19 vaccine | 1.48 (0.92) | – | 1.48 (0.90) | – | – | – |
| Fear of shots and needles | 1.38 (0.88) | – | 1.41 (0.89) | – | – | – |
| I have concerns about fainting if I get vaccine shots | 1.27 (0.77) | – | 1.29 (0.79) | – | – | – |
| Logistics | 1.51 (0.65) | 0.55 | 1.40 (0.61) | 0.57 | – | – |
| I am not sure where to get a COVID-19 vaccine | 1.91 (1.12) | – | 1.62 (1.07) | – | – | – |
| Getting a COVID-19 vaccine may take too much time | 1.38 (0.81) | – | 1.33 (0.72) | – | – | – |
| I am too busy to get vaccinated | 1.24 (0.69) | – | 1.25 (0.66) | – | – | – |
| Cost | 2.01 (1.07) | 0.8 | 1.36 (0.73) | 0.77 | – | – |
| Vaccine cost (it's too expensive) | 2.32 (1.38) | – | 1.40 (0.90) | – | – | – |
| I'm not sure how to file the insurance claim to get reimbursed | 1.72 (1.11) | – | 1.33 (0.83) | – | – | – |
| My insurance may not cover the COVID-19 vaccine | 1.98 (1.28) | – | 1.36 (0.91) | – | – | – |
| Intention (study 1) | – | – | – | – | – | – |
| Do you plan to get a COVID-19 vaccine when it is available to you? - Yes | 52.70% | – | – | – | – | – |
| No | 13.70% | – | – | – | – | – |
| Not sure | 33.60% | – | – | – | – | – |
| Intention (study 2) | – | – | – | – | 3.68 (1.33) | 0.95 |
| One the scale of 1 (very unlikely) to 5 (very likely), please indicate the likelihood that you will: Consider getting the COVID-19 vaccine. | – | – | – | – | 3.80 (1.36) | – |
| … try to get the COVID-19 vaccine. | – | – | – | – | 3.64 (1.40) | – |
| … actually get vaccinated for COVID-19. | – | – | – | – | 3.60 (1.41) | – |
2.3. Analysis
Statistical analyses in study 1 were performed using SPSS 26.0. To identify the influence of vaccine availability on perceived barriers before and after the COVID-19 vaccine became widely available in the United States, repeated measure analysis of variance (ANOVA) was used. Further, a mixed-model ANOVA was employed to test the interactive effects of vaccine availability and vaccination intention on different barrier perceptions. These models allow concurrent comparison of within- and between-subject difference in perceived barriers, providing more accurate examination of the influences of vaccine availability and vaccination intention than between-subject models. No missing data imputation was used, as participants were requested to answer all questions in the questionnaire. A link to study 1 data set can be found in the supplementary file.
2.4. Results
In response to RQ1, we analyzed whether availability and intention were correlated with the perceived distance of the vaccine. As expected, participants who believed that a COVID-19 vaccine will be available to them soon perceived it as closer to them on all four distance dimensions (temporal: r = 0.60, p < 0.001; hypothetical: r = 0.29, p < 0.001; social: r = 0.32, p < 0.001; spatial: r = 0.25, p < 0.001).
In addition, vaccination intention led to different distance perceptions (temporal: F [2, 931] = 15.94, p < 0.001, η 2 = 0.033; hypothetical: F [2, 931] = 37.09, p < 0.001, η 2 = 0.055; social: F [2, 931] = 37.09, p < 0.001, η 2 = 0.074; and spatial: F [2, 931] = 28.62, p < 0.001, η 2 = 0.058). Post-hoc tests show that those who intended to receive a COVID-19 vaccine in general perceived it as closer on four dimensions than those who were not sure whether they will get vaccinated (temporal: mean difference = −0.292, se = 0.054, p < 0.001; hypothetical: mean difference = −0.439, se = 0.060, p < 0.001; spatial: mean difference = −0.311, se = 0.047, p < 0.001; social: mean difference = −0.373, se = 0.049, p < 0.001). However, intenders and non-intenders only differed in spatial and social distance perceptions but not temporal and hypothetical distance perceptions (temporal: mean difference = 0.002, se = 0.074, p = 1.000; hypothetical: mean difference = −0.136, se = 0.082, p = 0.296; spatial: mean difference = −0.354, se = 0.065, p < 0.001; social: mean difference = −0.398, se = 0.067, p < 0.001).
RQ2 asks whether vaccine availability and vaccination intention influence perceived barriers to receive a COVID-19 vaccine. We conducted a full-factorial mixed model ANOVA with types of perceived barriers and time as within-subject factors and vaccination intention at time 1 as the between-subject factor. Mauchly's Test of Sphericity indicates that the assumption of sphericity had been violated for barrier type (χ2 [9] = 202.24, p < 0.001) and the interaction between barrier type and time (χ2 [9] = 160.20, p < 0.001). Therefore, Greenhouse–Geisser correction was applied to the degrees of freedom. As the objective of this study, that is, to identify the influence of availability and intention on people's consideration of different barriers, our analysis centers on the interaction between barrier type, time, and intention. The results of within-subject effect tests indicate that the interaction between barrier type and time (F [3.30, 951.37] = 37.01, p < 0.001, partial η 2 = 0.114) is a significant predictor of perceived barriers to receive a COVID-19 vaccine. Moreover, significant interactions were identified between vaccination intention and barrier type (F ([6.24, 899.15] = 52.04, p < 0.001, partial η 2 = 0.265) and in all three variables (F [6.61, 951.37] = 3.91, p < 0.001, partial η 2 = 0.026).
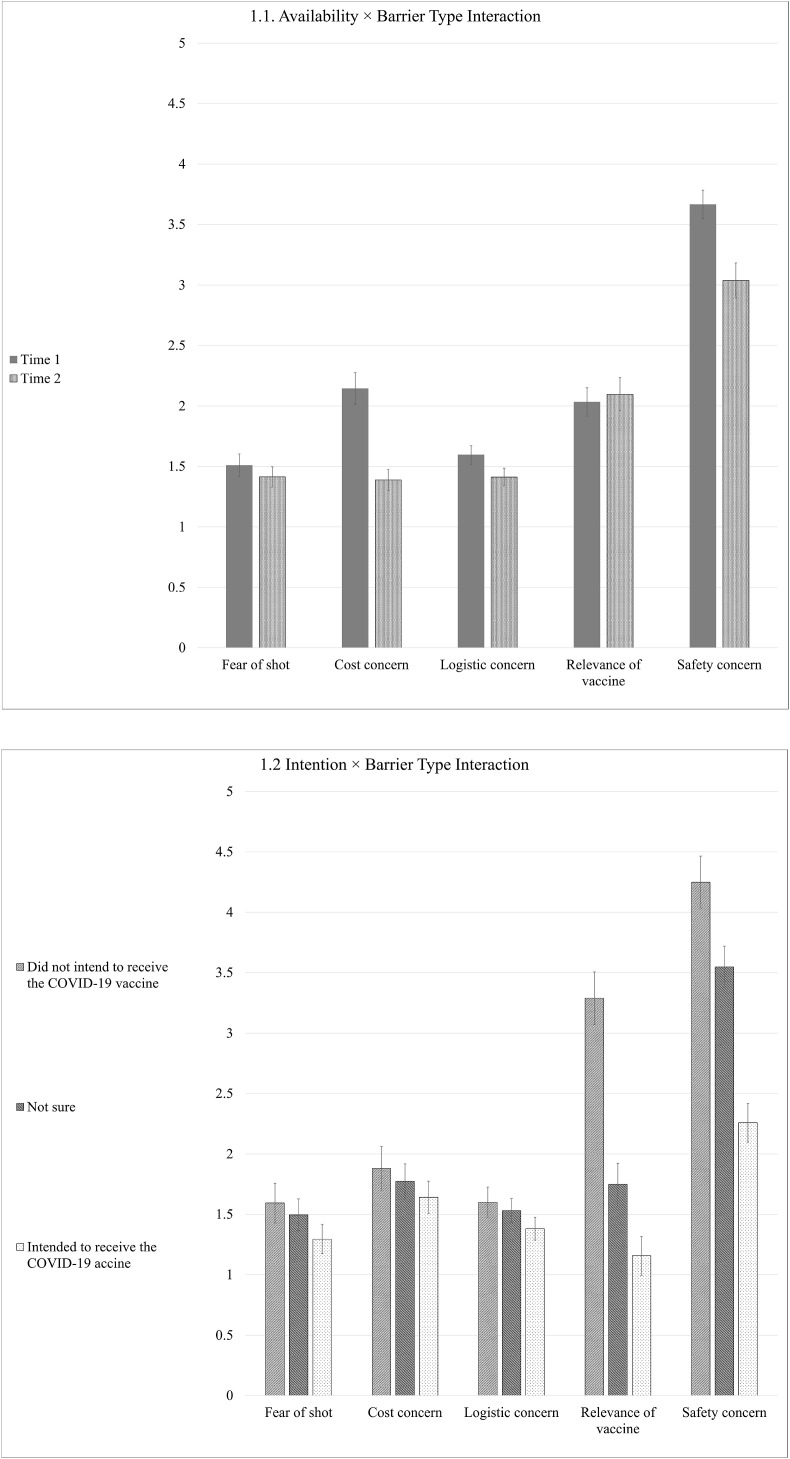
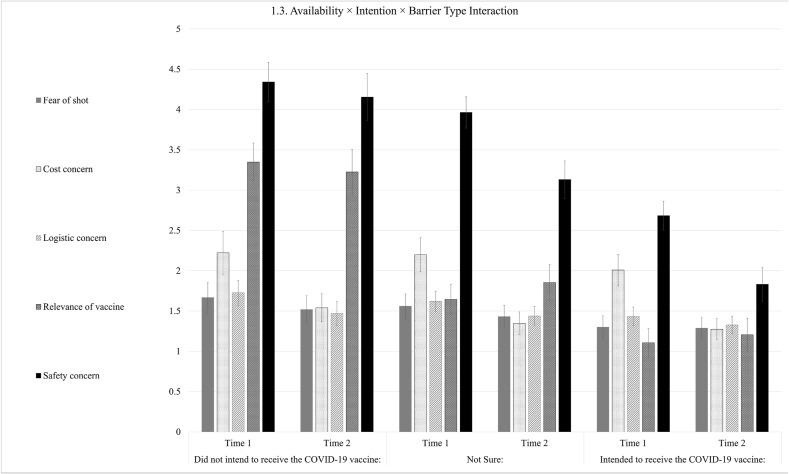
To identify the influence of availability on perceived barriers, Fig. 1.1 plots their marginal means in two time points. Evidently, safety concern, a global barrier, decreased at time 2, indicating that a higher availability of the vaccine may have reduced people's consideration of such high-level obstacle. In contrast, practical barriers, such as fear of shot and logistic concern, did not change much between time points. Notably, cost concern also dropped at time 2, which may be due to the free distribution of the COVID-19 vaccine in the United States.
Fig. 1.
Marginal means of perceived barriers across time points and intention groups.
Similarly, Fig. 1.2 plots marginal means of perceived barriers depending on participants’ intention to vaccinate themselves. Similar pattern emerged as individuals who did not intend to receive a COVID-19 vaccine were far more likely to cite global barriers (i.e., relevance and safety concern) as a barrier than those in the high-intention group. However, consideration of practical barriers did not differ among groups.
Last, we plotted marginal means of perceived barriers across different combinations of vaccination intention and time points in Fig. 1.3. Similar drop in safety and relevance concerns were observed when vaccination intention and vaccine availability were higher. However, practical concerns did not vary (except for between-time change in cost concern) across time points and intention groups.
2.5. Discussion
Evidently, people were more likely to cite global barriers, such as safety and relevance concerns, when the availability of vaccine and their intention to get one were low. Interestingly, the effects of barrier type, vaccine availability, and vaccination intention were also relatively high. However, we did not observe the increase in practical concerns among low-intention individuals reported in Gerend et al. (2013). This may be due to the national push to provide the COVID-19 vaccine to everyone in the country. It may have reduced people's consideration of practicalities such as vaccine cost and wait time. It is worth mentioning that the increase in availability may also be related to increased knowledge of the vaccine, which may render information of the vaccine more readily accessible and thus influence people's consideration of global and practical barriers. However, knowledge alone may not explain the different changes in barrier perceptions between two time points, as knowing more about the vaccine (e.g., vaccine safety, where to get the vaccine) may likely lead to consistent decrease in all perceived behavioral barriers.
In summary, the results of study 1 partially supported our reasoning. Low availability and intention led to farther distance perception of the COVID-19 vaccine, which may further influence people's mental construal. Low vaccine availability and vaccination intention increased the weight of global barriers, such as vaccine safety in people's consideration of behavioral barriers to receiving a COVID-19 vaccine.
3. Study 2
3.1. Sample
A sample of 727 participants were recruited from an opt-in panel maintained by Qualtrics between October 8 and 20, 2020. The sample demographic is representative of the U.S. population (Table 1; U.S. Census Bureau, 2019). A total of 1856 participants started the survey. The responses from those who passed the attention check questions and have not contracted COVID-19 nine months prior to taking the survey were retained (N = 727). Power analysis indicates that the sample is sufficient to achieve a power of 0.92 in detecting small difference between participant preferences in different vaccine characteristics (AMCE = 0.05, level = 3, tasks = 5). Informed consent was obtained from all participants included in the study.
3.2. Procedure
A choice-based conjoint experiment embedded in an experimental survey was delivered on Qualtrics.com. Perceived availability of the COVID-19 vaccine was manipulated with a mock vaccine availability estimate system. First, the participants were asked to report their demographics and were then informed that their information is being analyzed to estimate how soon a COVID-19 vaccine would be available to them. In the high-availability condition, the participants were told that a COVID-19 vaccine will be available to them in one to three months. In the low-availability condition, the estimated wait time was 10–12 months. As a manipulation check, the participants responded to the same perceived availability question in study 1. Those in the low-availability condition reported a significant longer wait time (M = 3.48, SD = 1.10) than those in the high-availability condition (M = 2.99, SD = 1.11; F [1725] = 36.82, p < 0.001, η 2 = 0.048). The experimental manipulation was successful. The participants were fully debriefed at the end of the survey and were directed to the Centers for Disease Control and Prevention's (CDC) website for information related to COVID-19 vaccine distribution.
Utilizing the similar distance perception measurement in study 1, we assessed participants’ perceived distance of the COVID-19 vaccine. Those in the low-availability condition perceived the COVID-19 vaccine as temporally (F [1725] = 23.73, p < 0.001, η 2 = 0.032) distant than those in the high-availability condition. However, there was no significant between-condition difference in hypothetical (F [1725] = 1.62, p = 0.20, η 2 = 0.002), social (F [1725] = 0.76, p = 0.382, η 2 = 0.001), and spatial (F (1,725) = 1.75, p = 0.186, η 2 = 0.002) distance perceptions.
Furthermore, we measured participants’ intention to receive a COVID-19 vaccine with three items (see means, standard deviations, and scale reliability in Table 2). The scale was reliable, and an average composite score was created (median = 4.00). The intention variable was dichotomized with a median split to create a categorical variable for subgroup conjoint analysis (n low-intention = 405, n high-intention = 322).
In the choice-based conjoint experiment, the participants were given six pairs of hypothetical COVID-19 vaccines that may differ in seven attributes and were asked to choose one vaccine they prefer out of each pair. Table 3 illustrates the attributes and their corresponding levels. Conjoint experiment has long been used in marketing research and gained attention from political science and public health scholars in the recent years (Hainmueller et al., 2014; Kreps et al., 2020; Motta, 2021; Sun et al., 2020). Unlike vignette-based experiment, in which respondents are exposed to one or few of the treatment conditions, conjoint analysis concurrently assesses people's preference in multiple attributes. In addition, the unique format of conjoint experiment better mimics real-life decision-making scenarios, where people do not evaluate choices based on just one characteristic (as in vignette experiments) but with consideration of different aspects of available options (Hainmueller et al., 2014). Conjoint experiment is particularly applicable to construal level studies, as it provides an effective solution to assess the influence of high- and low-level features simultaneously.
Table 3.
Conjoint experiment choices.
| Attribute | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| Out-of-pocket cost | $0 | $20 | $100 |
| Vaccination site | Offsite drive/walk-through | Clinic | Pharmacy |
| Wait time | <1 h | 1–2 h | 2 h |
| Number of doses | 1 | 2 | – |
| Effective rate | 50% | 65% | 80% |
| Approval status | Approved by FDA | Emergency Use Authorization (EUA) | – |
| Side effect | None reported | Mild | Moderate |
| Recommended by | Your doctor | CDC | The White House |
Note. Vaccine profiles include random combination of different attribute levels.
The seven attributes assessed in this experiment include both high- and low-level features (Table 3). High-level features are central to people's perception of the COVID-19 vaccine and include its effective rate and FDA approval status, which is related to the safety of a vaccine. Low-level features include cost and logistics associated with getting a COVID-19 vaccine. Based on the centrality and subordination principles, we argue that vaccine side effects and endorsement may also be considered as low-level features. Specifically, change in the effectiveness and safety of a vaccine are more likely to alter people's overall evaluation of the vaccine (i.e., centrality), and variation in side effects and endorsement may not alter evaluation of an effective and safe vaccine as much as the other way around (i.e., subordination).
3.3. Analysis
A total of 727 participants viewed 8725 vaccine profiles and completed 4362 choice tasks. However, upon close inspection, we found that the order of tasks (e.g., the fifth and sixth choice tasks) interacted with vaccine features to influence people's choices (F [15, 8694] = 1.70, p = 0.044, η 2 = 0.003). This may be caused by fatigue of completing six rounds of conjoint tasks. Thus, we retain results from the first four rounds of conjoint tasks that involved 5816 profiles and 2908 choice tasks. No significant interaction between task order and vaccine attributes were identified (F [15, 5786] = 1.66, p = 0.052, η 2 = 0.004) in the final sample.
We computed the average marginal component effects (AMCEs) of each attribute level for the overall sample. The AMCEs are ordinary least squares (OLS) regression coefficients of attribute levels that predict participants' preference for one vaccine profile over another, with standard errors clustered at individual level. It represents the probability of a participant choosing one attribute level (e.g., a vaccine with two doses) over another (e.g., a vaccine with one dose) averaged in all possible combination of other features (Hainmueller et al., 2014). Marginal means were used to compare subgroup preference in different vaccine attributes to avoid bias in reference group selection (Leeper et al., 2020). Marginal means measures participants’ favorability toward each attribute level averaged in all other features. Higher marginal means indicate a stronger preference for an attribute level. The AMCEs and marginal means were computed in R with the “cregg” package (Leeper, 2018). No missing data imputation was used, as participants were requested to answer all questions in the questionnaire. A link to study 2 data set can be found in the online supplementary file.
3.4. Results
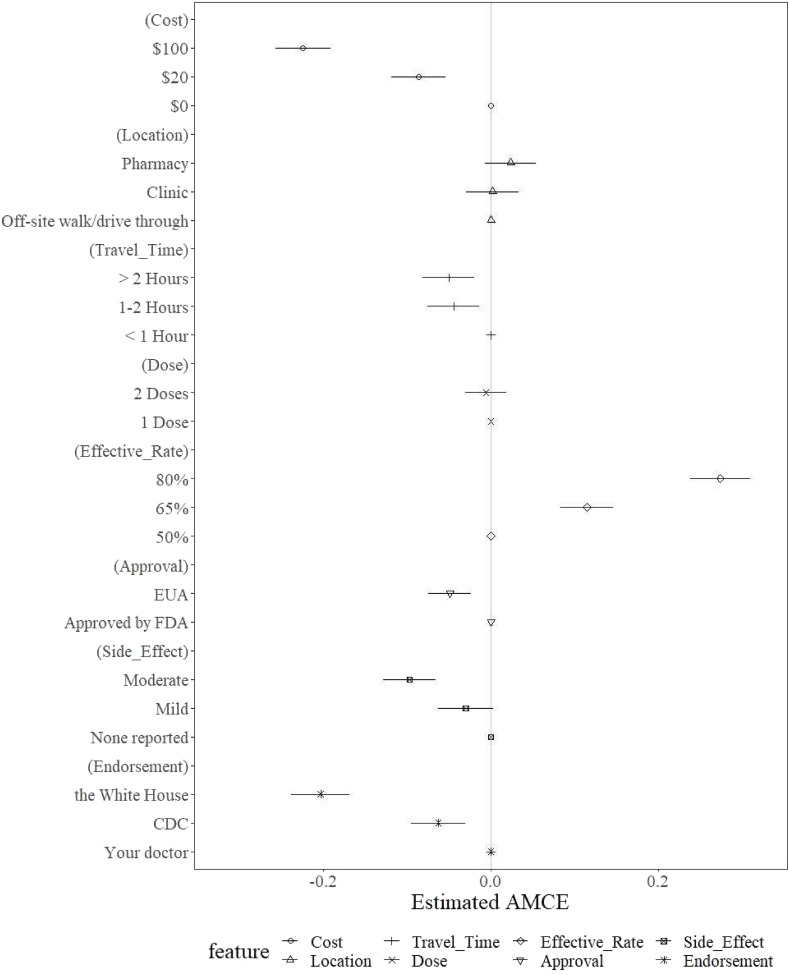
Fig. 2 illustrates the AMCEs and their standard errors for each attribute level. Higher AMCEs indicate that a level is preferred over the reference level (which are represented as dots at 0). Reference levels were determined based on existing studies (Kreps et al., 2020). Evidently, the participants tend to prefer a vaccine that costs less and requires less than 1 h wait time. Moreover, vaccines with no side effects reported and higher effectiveness rates were preferred over other levels. A vaccine recommended by one's doctor is also preferred over those recommended by the CDC or the White House. However, vaccination sites and number of doses did not significantly influence participants' favorability toward a vaccine.
Fig. 2.
Estimated average marginal component means (AMCEs) of vaccine attribute levels.
To address RQ3, we tested whether vaccine availability and vaccination intention influenced people's consideration of different vaccine characteristics. Fig. 3.1 compares the marginal means of each attribute level between high- and low-availability conditions and high- and low-intention groups. As previously suggested, marginal means comparison could effectively avoid biased results because of reference group selection (Leeper et al., 2020). To aid interpretation of the results, conditional AMCEs are also reported as regression coefficients (Hainmueller et al., 2014). Those in the high-availability group preferred less than 1 h wait time than more than 2 h wait time (B = −0.072, se = 0.023, p < 0.01). However, the difference was not significant in the low-availability group (B = −0.028, se = 0.022, p = 0.186). Nonetheless, the omnibus F-test indicates that there is no significant interaction between conditions and attribute levels (F [15, 5801] = 0.63, p = 0.85, η 2 = 0.002). In contrast, vaccination intention interacted with attribute levels to influence people's preference in vaccines (F [15, 5786] = 2.84, p < 0.001, η 2 = 0.007; Fig. 3.2). Specifically, participants with higher intention to receive a COVID-19 vaccine preferred a vaccine that requires less than an hour than over 2 h wait time (B = −0.069, se = 0.024, p < 0.01), while those with lower intention were less sensitive to such difference (B = −0.039, se = 0.021, p = 0.061). Although not revealed in the marginal means comparison, conditional AMCEs also indicate that participants with lower vaccination intention preferred a COVID-19 vaccine with no side effects reported than the one with mild side effects (B = −0.049, se = 0.022, p < 0.05). However, the difference was not significant among those with higher vaccination intention (B = 0.005, se = 0.025, p = 0.835).
Fig. 3.
Marginal means of vaccine attribute levels across vaccine availability conditions and vaccination intention groups.
Fig. 4 compares whether the high- or low-availability cue led to different vaccine preference among participants with high or low vaccination intention (F [15, 5756] = 1.70, p < 0.01, η 2 = 0.013). Among low-intention individuals, low availability of a COVID-19 vaccine made them more sensitive to the difference between vaccines with a full FDA approval or emergency use authorization (EUA) (low availability: B = −0.058, se = 0.027, p < 0.05; high availability: B = −0.047, se = 0.026, p = 0.071), and the difference between vaccines with mild or moderate side effects (low availability: B = −0.065, se = 0.030, p < 0.05; high availability: B = −0.049, se = 0.029, p = 0.089). On the other hand, participants in the high-availability group were more sensitive to the difference between $20 and free vaccines (low availability: B = −0.054, se = 0.031, p = 0.081; high availability: B = −0.130, se = 0.030, p < 0.001) and vaccines recommended by their doctor or the CDC (low availability: B = −0.033, se = 0.032, p = 0.296; high availability: B = −0.112, se = 0.030, p < 0.001). Among high-intention individuals, low availability information led to heightened sensitivity to the difference between vaccine effective rates (65% vs. 50% effective; low availability: B = 0.151, se = 0.0.030, p < 0.001; high availability: B = 0.064, se = 0.035, p = 0.073) and side effects (moderate vs. mild side effects: low availability; B = −0.098, se = 0.032, p < 0.01; high availability: B = −0.062, se = 0.034, p = 0.069). In contrast, high availability information increased their sensitivity to vaccine approval status (approved by FDA vs. EUA; low availability: B = 0.001, se = 0.027, p = 0.979; high availability: B = −0.090, se = 0.026, p < 0.001) and wait time at the vaccination site (more than 2 h vs. less than 1 h; low availability: B = −0.015, se = 0.034, p = 0.657; high availability: B = −0.134, se = 0.034, p < 0.001).
Fig. 4.
Marginal means of vaccine attribute levels across different combinations of vaccine availability conditions and vaccination intention groups.
3.5. Discussion
Although vaccine availability did not lead to significant change in people's consideration of vaccine characteristics, different valuation of high- and low-level attributes depending on vaccine availability emerged when participants with different levels of vaccination intention were analyzed separately. Specifically, lower availability, which corresponds to a closer perceived distance of the vaccine, increased the weight of low-level practical features (e.g., cost, wait time, and endorsement) in participants' evaluation of a COVID-19 vaccine. In contrast, high availability motivated consideration of high-level global features (e.g., effective rate and FDA approval status). Although the effects identified are relatively small, such findings may indicate that the influence of vaccine availability may function differently on people with high or low intention to receive a COVID-19 vaccine.
Unlike perceived barriers, participants with higher intention were more sensitive to difference in vaccine effective rates, a high-level characteristic. On the other hand, participants with lower intention were more sensitive to the difference in vaccine endorsement, a low-level characteristic. This may indicate that vaccination intention may function differently to influence people's consideration of vaccination barriers and vaccine characteristics. In particular, as perceived barriers are more relevant to one's consideration of their own behavior, increase in intention may lead to attention to the practicality of performing such behavior. In contrast, as vaccine characteristics are more relevant to the object of such behavior, higher intention may render the central feature of such objective (e.g., effective rate) more salient, and lower-intention individual may be more likely distracted by less central features such as endorsement. It is also worth noting that vaccination intention was dichotomized in study 2 to allow between-group comparison of marginal means of the attribute levels. Future studies may utilize different research design and modeling strategy to examine the relationships reported here.
4. General discussion
The results from the two studies show that vaccine availability and vaccination intention influenced people's consideration of the COVID-19 vaccine. Low availability led to more distant perception of the vaccine, which enhanced the salience of high-level behavioral barriers and vaccine characteristics. On the other hand, lower intention signaled the importance of global concerns surrounding vaccine safety and one's need to get a vaccine. Findings from this study attest the explanatory power of construal level theory of psychological distance in examining individual's perception of different vaccines (Gerend et al., 2013; Trope and Liberman, 2010). As perceived distance of the vaccines increases, either owing to low availability or low vaccination intention, high construal level information tends to be more available and accessible. In contrast, shorter psychological distance promotes attention to low-level features of vaccines.
The findings of this study may contribute to the communication of health and other risks from three perspectives. First, because of the geographical and social inequity of COVID-19 vaccine distribution, many people are still waiting to receive a vaccine (Gupta and Morain, 2021). To sustain public interest in getting vaccinated among these groups, public health authorities may highlight the high-level feature of the vaccine, such as its effectiveness and safety. On the contrary, in areas where COVID-19 vaccine supplies are sufficient, enhancing its accessibility and promoting it through trustworthy communicators, such as primary care physicians, may be more efficient in enhancing vaccination rate. Second, public health campaigns promoting other vaccines and health behaviors may also benefit from this study. Specifically, when communicating a novel health risk solution such as the COVID-19 vaccine, emphasizing on its safety and effectiveness may be more effective in increasing public acceptance. On the contrary, existing vaccines and medications such as flu shot may be better campaigned with its ease of access highlighted. Similarly, health communicators should also tailor their messages according to individual characteristics (Schuster et al., 2015). People with easy access and higher adoption intention may be better persuaded with messages that emphasize on practical features such as costs and logistics, while those with lower accessibility and intention may respond more positively to messages that highlight the safety and effectiveness of the solutions. Finally, and from a broader perspective, as solutions to health and environmental risks often take years to become widely available and continue to serve the world, strategic design and implementation of campaigns fit to the life cycle of such solutions are needed. Specifically, early campaigns should articulate its central features, while stronger emphasis should be given to practical features when availability and public acceptance increase.
This study also has several limitations. First, both samples were recruited from opt-in panels. Although they share similar demographic characteristics with the general population in the United States, a random sample may enhance the external validity of findings reported here. In a similar vein, the U.S. samples may have limited the applicability of our conclusions to other cultures. Thus, we recommend future studies to test the framework introduced here on more diverse samples. Second, the reliability of some scales (e.g., hypothetical distance perception and logistics concern in study 1) was not optimal (Cronbach's α < 0.70). Future studies may revise the scales to improve their reliability. Finally, the current study focused on the COVID-19 vaccine, which is novel to most people. It would be meaningful to examine whether these findings replicate in other contexts, such as the influenza and HPV vaccines.
5. Conclusion
This study demonstrates that vaccine availability and vaccination intention influenced people's consideration of the COVID-19 vaccine. Low availability and intention led to heightened attention to high-level considerations such as safety concern and vaccine approval status. On the other hand, high availability increased practical concerns, such as cost, logistics, and endorsement associated with the vaccine. Because of the inequality in COVID-19 vaccine distribution, we recommend public health authorities and other health communicators to tailor their messages when communicating to populations with different vaccination intention and access to the COVID-19 vaccine.
Declaration of competing interest
none.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114315.
Author statement
Haoran Chu: Conceptualization, Methodology, Formal analysis, Resources, Data curation, Writing – original draft preparation, Writing – Reviewing and Editing, Visualization, Sixiao Liu: Conceptualization, Methodology, Validation, Writing – original draft, Writing – review & editing
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Allen J.D., Mohllajee A.P., Shelton R.C., Othus M.K., Fontenot H.B., Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Prev. Med. 2009;48:420–425. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Brewer N.T., Fazekas K.I. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev. Med. 2007;45:107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Chu H., Liu S. Integrating health behavior theories to predict American's intention to receive a COVID-19 vaccine. Patient Educ. Counsel. 2021 doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita K., Henderson M.D., Eng J., Trope Y., Liberman N. Spatial distance and mental construal of social events. Psychol. Sci. 2006;17:278–282. doi: 10.1111/j.1467-9280.2006.01698.x. [DOI] [PubMed] [Google Scholar]
- Gerend M.A., Shepherd M.A., Shepherd J.E. The multidimensional nature of perceived barriers: global versus practical barriers to HPV vaccination. Health Psychol. 2013;32:361. doi: 10.1037/a0026248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R., Morain S.R. Ethical allocation of future COVID-19 vaccines. J. Med. Ethics. 2021;47:137–141. doi: 10.1136/medethics-2020-106850. [DOI] [PubMed] [Google Scholar]
- Hainmueller J., Hopkins D.J., Yamamoto T. Causal inference in conjoint analysis: understanding multidimensional choices via stated preference experiments. Polit. Anal. 2014;22:1–30. [Google Scholar]
- Janz N.K., Becker M.H. The health belief model: a decade later. Health Educ. Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kim J., Nan X. Temporal framing effects differ for narrative versus non-narrative messages: the case of promoting HPV vaccination. Commun. Res. 2019;46:401–417. [Google Scholar]
- Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., et al. Factors associated with US adults' likelihood of accepting COVID-19 vaccination. JAMA network open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25594. e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeper T.J. Cregg: simple conjoint analyses and visualization. R package version 0. 2018;2:1. [Google Scholar]
- Leeper T.J., Hobolt S.B., Tilley J. Measuring subgroup preferences in conjoint experiments. Polit. Anal. 2020;28:207–221. [Google Scholar]
- Liberman N., Trope Y. The role of feasibility and desirability considerations in near and distant future decisions: a test of temporal construal theory. J. Pers. Soc. Psychol. 1998;75:5. [Google Scholar]
- Liu S., Yang J.Z. The role of temporal distance perception in narrative vs. non-narrative persuasion related to e-cigarettes. J. Health Commun. 2020;25:543–553. doi: 10.1080/10810730.2020.1788678. [DOI] [PubMed] [Google Scholar]
- Liviatan I., Trope Y., Liberman N. The effect of similarity on mental construal. J. Exp. Soc. Psychol. 2008;44:1256–1269. doi: 10.1016/j.jesp.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta M. Can a COVID-19 vaccine live up to Americans' expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc. Sci. Med. 2021;272:113642. doi: 10.1016/j.socscimed.2020.113642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J.O., Velicer W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.-L. Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy. PLoS One. 2017;12 doi: 10.1371/journal.pone.0170550. 2005–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster M., Eskola J., Duclos P., SAGE Working Group on Vaccine Hesitancy Review of vaccine hesitancy: rationale, remit and methods. Vaccine. 2015;33:4157–4160. doi: 10.1016/j.vaccine.2015.04.035. [DOI] [PubMed] [Google Scholar]
- Slaoui M., Hepburn M. Developing safe and effective Covid vaccines—operation Warp Speed's strategy and approach. N. Engl. J. Med. 2020;383:1701–1703. doi: 10.1056/NEJMp2027405. [DOI] [PubMed] [Google Scholar]
- Sun X., Wagner A.L., Ji J., Huang Z., Zikmund-Fisher B.J., Boulton M.L., et al. A conjoint analysis of stated vaccine preferences in Shanghai, China. Vaccine. 2020;38:1520–1525. doi: 10.1016/j.vaccine.2019.11.062. [DOI] [PubMed] [Google Scholar]
- Trope Y., Liberman N. Construal-level theory of psychological distance. Psychol. Rev. 2010;117:440. doi: 10.1037/a0018963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau American community survey 1-year estimates. 2019. https://data.census.gov/cedsci/table?q=ACS%202019&tid=ACSST1Y2019.S0101 Retreived from.
- Weinstein N.D. Testing four competing theories of health-protective behavior. Health Psychol. 1993;12:324. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]
- Witte Kim. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992;59(4):329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]
- World Health Organization . World Health Organization; 2021. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.