Abstract
Introduction
Because of the inadequate level of public awareness of the disease, the incidence of stroke has been sharply rising. Eventually, due to the prehospital delay, many stroke cases could not be eligible for thrombolysis thereby poor rehabilitative outcome has been tremendously increased. Thus, this study aimed to review the level of knowledge, prevention practice, and associated factors of stroke among hypertensive and diabetic patients.
Methods
A systematic review of primarily published articles (2010–2020) related to knowledge and prevention practices of stroke was performed by searching online electronic databases like PubMed, Google Scholar, Refseek, Science direct, ResearchGate, and manual Google search by using the keywords and MeSH terms. Studies conducted on knowledge and prevention practices amongst hypertensive and/or diabetic patients were included.
Results
Out of 531 searched studies, 42 articles were identified to be reviewed. The reported overall knowledge of stroke was ranging from 4.4% to 79%. Knowledge to the signs/symptoms of stroke was 23.6% to 87%. However, 15% to 77% of subjects were also reported that they did not know any sign of stroke. The range of risk factor knowledge was 10.5% to 86.6%. The reported level of stroke prevention practice was 2.4% to 72% but physical activity and weight reduction practice were relatively low. Inadequate level of knowledge and prevention practice of stroke was related to elderly, female gender, uneducated, unmarried, rural residents, economically low, comorbidity and unemployed individuals.
Conclusion
The current finding revealed that the level of knowledge and prevention practice of stroke was inadequate. Hence, the finding highlights health educational programs should be planned as an important avenue to enhance stroke awareness among the high-risk populations.
Keywords: stroke, knowledge, warning sign, risk factor, prevention
Introduction
Despite global age-standardized mortality rates of stroke had shown a sharp decline from 1990 to 2016, its prevalence rate and burden have been still high.1 Reports showed that 80·1 million prevalent cases, 5.5 million deaths, and 116·4 million DALYs of stroke in the world were recorded at the end of 2016. Its burden in developing countries especially Sub-Saharan Africans (SSA) is still high.2,3
Although stroke is considered as multi-factorial, it is majorly attributed to the contributing risk factors like uncontrolled hypertension (HTN), diabetes mellitus (DM), dyslipidemia, heart disease, and other modifiable risk factors. The highest contributor is HTN which accounts for up to 75% of stroke cases.4–8 Moreover DM contributes up to 30% incidence to stroke events.1,9–13
Therefore, prior awareness in these high-risk populations can have a very important implication to decrease the incidence of stroke emergencies. Creating awareness about stroke helps to promote early hospital presentation thereby reduces long-term complications of the disease. Due to the inability to know the disease condition 50–87% of patients presented to the hospital out of the window period of recombinant Tissue Plasminogen Activator (tPA). As a result, they could not be eligible to the American Heart Association and American Stroke Association (AHA/ASA) recommended treatment protocol.14–16
Poor recognition of warning signs of stroke often results in a delay in hospital presentation so that increases stroke-related morbidity and mortality. Extensive studies devoted to assessing the knowledge status of patients admitted on stroke and were reported as they had not had information on stroke disease and the way how to prevent it.17–20 More than 70% of stroke patients did not know risk factors and 20–25% were smokers and alcoholics.21
Increasing awareness towards risk factors, warning signs, and prevention strategies of the stroke to the high-risk populations can imply a reduction of its incidence and pre-hospital care delay.22–25Therefore, this study aimed to review the level of knowledge, prevention practice, and associated factors towards stroke among hypertensive and diabetic populations.
Method
This systematic review was reported with the recommended protocols of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).26
Information Source and Search Strategy
A search strategy was developed to look at recent existing articles and adapted to search, PubMed, Google Scholar, ResearchGate, Refseek, Science direct, and Manual google search by using keywords, indexing terms (MeSH terms), and the combination of them. Keywords were, “Stroke”, “Knowledge”, “Awareness”, “Risk Factor”, “Warning Sign”, “Primary Prevention”, “Lifestyle”, “Self-Care”, “Hypertension”, “Diabetic Mellitus”. An advanced searching method by Boolean operators (AND & OR) was also used; “Stroke AND Awareness”, Stroke AND Knowledge”, “Stroke AND Awareness AND Hypertension OR Diabetic”, “Stroke AND Prevention”. Two reviewers independently reviewed the titles and abstracts of the articles identified by these searching databases. Finally, any article that appeared to meet the inclusion criteria was read in detail.
Inclusion and Exclusion Criteria
Primary studies published between 2010 and 2020 were included. The assessment questions used to test knowledge and practice could be open-ended, closed, or multiple choice. The way of delivering the questions could be through telephone, face-to-face, or postal surveys. We excluded articles that could not be accessed full text because of the limited data that could be extracted. Studies published other than English could be excluded due to the poor ability of reviewers in other languages. Non-empiric citations including editorials, letters, commentaries, and opinions were also excluded.
Study Selection and Quality Assessment
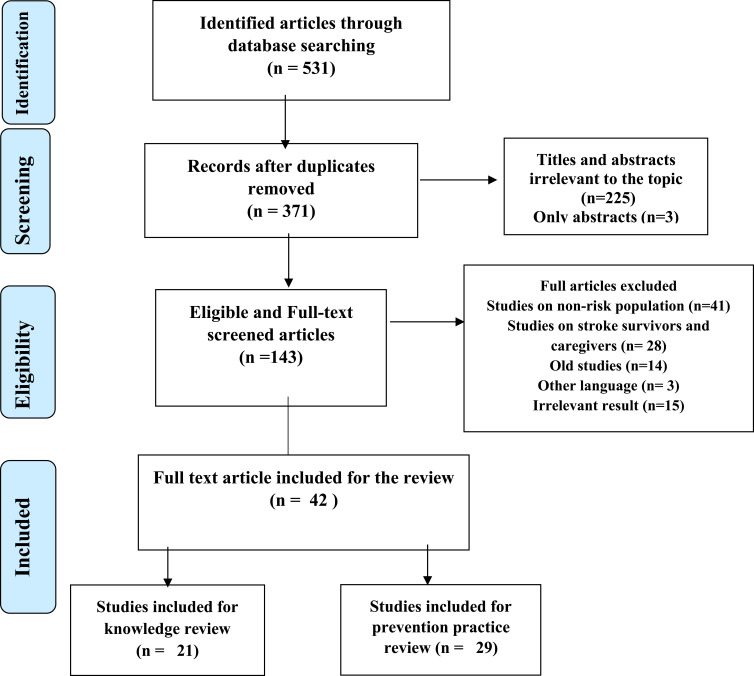
We used Endnote version 7 reference manager to remove duplicated articles as shown in Figure 1. The authors assessed the quality of each study independently. If any discrepancy happened, it was resolved through consensus discussions. The methodological quality of all the reviewed studies was checked by the National Institute of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies before inclusion in the review.27 The tool has 14 questions to be rated as Yes, No, Not applicable, and Not reported. Of course, it does not have a numerical scale, the general guidance provides to determine the overall quality of studies and to be grade as good, fair, and poor. Accordingly, studies answer more questions positively graded as Good (≥7) followed by Fair (5–6) and poor quality (≤4) as it was adapted from a previous study.28
Figure 1.
Flow chart of the article selection process.
Data Extraction and Synthesis
The authors looked at and screened the articles independently based on the inclusion/exclusion criteria. The following details were extracted from each study using an abstraction format prepared in Microsoft excel: author, year of publication, study area, study subjects, sample size, study design, sampling technique, general and/or overall knowledge of stroke, knowledge towards risk factors, knowledge towards the signs and symptoms of stroke, knowledge towards stroke prevention, lifestyle practices of stroke prevention and associated factors related to knowledge and prevention practices.
After the raw data collected from the included articles, the results were synthesized into tables as per the objectives of the review. Finally, the studies included in the review were categorized under one or more of the following topics to be narratively synthesized; knowledge of general concepts of stroke, knowledge of risk factors of stroke, knowledge of stroke sign/symptoms, knowledge of the pre-stroke prevention, and lifestyle modification practice (LMP) of stroke prevention. It was impossible to express the result quantitatively in the form of meta-analysis since the reported data was insufficient.
Result
A total of 531 titles were identified in the searching databases. After duplicates and irrelevant articles were screened, 42 eligible studies were left to be reviewed for knowledge and prevention practice as shown in Figure 1.
Risk of Bias
High risk of bias can be expected in studies where the quality assessment element was not reported as per the standards. In the contrary studies that were rated as yes (reported) in the quality assessment questions considered as low risk of bias. As a result, more than 80% of the studies had clearly settled objectives,17,29–69 specified study populations,17,29–35,37,39–53,55,56,58,60–64,66–69 inclusion/exclusion criteria,17,29–35,37,40,42–51,53–57,59,61–69 adjusted confounders,17,29–69 defined dependent variables,17,29,30,32–44,46–51,53,55–58,63–69 and independent variables.17,29–31,33,34,36,37,39–44,46–49,51–60,63–65,69 Whereas ≥50% participation rate,29–31,33–35,37,39–42,44,46,48,50–53,55,56,61–63,65,68,69 justified sample size determination,29–32,34,37–40,42–44,46–52,55–57,60,61,63,65,66,68,69 and less 20% lost follow up/response rate,17,29–31,34–36,39,47,49–51,56,66,68 were clearly stated in 61.9%, 69% and 35.7% of studies, respectively. Other questions were not applicable for our reviewed studies. Finally, after critically appraised near to 62%, 31% and 7% of studies were found in good, fair, and poor quality, respectively.
Characteristics of Studies
The reviewed 42 articles comprised a total of 10,063 sampled participants obtained from 20 different world countries; 20 Asian, 16 African, 3 European, 2 North American, and 1 South American study. Twenty-two studies (52.4%) were done among hypertensive patients, ten studies (23.8%) among diabetic patients, and ten (23.8%) of the studies were done among hypertensive and diabetic patients. The mean age of participants was 55.1±5.7 years per study. The sex proportion of the subjects was 53±14.5% of males and 49.1±12% of females. The search results revealed that most of these articles were institutionally based and were designed as a cross-sectional study. However, their randomization technique was a probabilistic and non-probabilistic method as mentioned in Table 1.
Table 1.
Characteristics of Reviewed Studies
| Study, Year of Publication | Country | Disease Condition | Sample Size | Mean Age (Years) | Male (%) | Female (%) | Data Collection | Method & Sampling |
|---|---|---|---|---|---|---|---|---|
| Abate et al, 201929 | Ethiopia | HTN | 278 | 54.40 | 47.80 | 52.20 | Y | Cross sectional, SRS |
| Aboutorabi Zarchi et al, 201930 | Iran | DM | 281 | 54.04 | 29.60 | 70.40 | O, MCQ | Cross-sectional |
| Al-Beladi et al, 201631 | Saudi Arabia | DM & HTN | 166 | - | 42.20 | 57.80 | O&C | Cross-sectional, Consecutive Sampling |
| Amen, 201632 | Iraq | HTN | 114 | 58.40 | 58.8 | 45.70 | C | Cross-sectional Purposive sampling |
| Ampiah et al, 201833 | Ghana | DM & HTN | 208 | 57.30 | 41.30 | 58.70 | C | Cross-sectional, Convenient S |
| Arisegi et al, 201834 | Nigeria | DM & HTN | 239 | 48.21 | 34.3 | 65.7 | Cross-sectional, SRS | |
| Chukwuocha, 201838 | Nigeria | DM | 91 | 59 | 33 | 67 | O | Cross-sectional |
| Dar et al, 201939 | Pakistan | HTN | 384 | 51.4 | 52.90 | 47.10 | Y | Cross-sectional, consecutive S |
| Ehidiamen et al, 201843 | Nigeria | HTN | 144 | 58.50 | 53.50 | 46.50 | O | Cross-sectional, consecutive S |
| Mersal et al, 202050 | Saudi Arabia | HTN | 203 | 41.83 | 51.20 | 48.80 | C | Cross-sectional, |
| Oparah, 201753 | Nigeria | DM & HTN | 148 | 54.30 | 45.90 | 54.10 | O | Cross-sectional, |
| Poongothai et al, 201754 | India | HTN | 50 | 48.7 | 72.00 | 28 | Observational | |
| Venkatesh et al, 201661 | India | HTN | 105 | 47.50 | 66.70 | 33.5 | C | Cross-sectional, consecutive S |
| Vincent et al, 201562 | Nigeria | DM & HTN | 200 | 47.50 | 66.70 | 33.30 | O | Cross-sectional, consecutive S |
| Wahab et al, 201563 | Nigeria | DM & HTN | 314 | 56.40 | 47.10 | 52.90 | Cross-sectional, consecutive S | |
| Weltermann et al, 201365 | Germany | DM | 218 | - | 50.40 | 49.50 | O | Cross-sectional |
| Konduru et al, 201747 | India | DM | 100 | - | 64.00 | 36.00 | Prospective and observational | |
| Chimberengwa et al, 201969 | Zimbabwe | HTN | 304 | 59.00 | 34.60 | 65.40 | Cross-sectional | |
| Okonta et al, 201452 | South Africa | DM | 217 | - | - | - | Cross-sectional | |
| Tesema et al, 2016 60 | Ethiopia | HTN | 130 | - | 57.70 | 42.30 | O&C | Cross-sectional |
| Buda et al, 201737 | Ethiopia | HTN | 205 | 53.90 | 48.8 | 51.2 | Cross-sectional | |
| Durai et al, 201542 | India | HTN | 100 | 51 | 100 | NP | Cross-sectional | |
| Mutyambizi et al, 202068 | South Africa | DM | 396 | - | 39.24 | 60.76 | MCQ | Cross-sectional |
| Rashidi et al, 201857 | Iran | HTN | 110 | 57.97 | 47.3 | 52.7 | MCQ | Cross-sectional |
| Faiz et al. 201844 | Norway | DM & HTN | 173 | 68 | 63.6 | 36.4 | O | Prospective cross sectional |
| Sheeba et al, 201759 | India | DM | 100 | - | 75 | 25 | Cross-sectional, Convenient S | |
| Dinesh et al, 201640 | India | DM | 400 | - | 62.25 | 38.75 | C | Cross-sectional, Random |
| Bollampally et al, 201666 | India | HTN | 160 | - | 47.5 | 52.5 | O | Prospective, observational |
| Warren-Findlow et al, 201164 | Carolina | HTN | 188 | 53 | 28.70 | 71.3 | Cross-sectional | |
| Rajan et al, 201955 | India | HTN | 200 | 56.6 | 40.5 | 59.5 | MCQ | Cross-sectional, Convenient S |
| Kisokanth et al 201846 | Sri Lanka | HTN | 424 | 60.4 | 41 | 59 | MCQ | Cross-sectional, SRS |
| Obirikorang et al, 201851 | Ghana | HTN | 300 | 63.6 | 62 | 38 | Y | Cross-sectional, Simple Random |
| Bakhsh et al, 201736 | Saudi Arabia | HTN | 211 | 51.8 | 60.2 | 39.8 | Y | Cross-sectional, |
| Rajasekharan et al, 201556 | India | DM | 290 | 47.9 | 60 | 40 | MCQ | Cross-sectional, Convenient S |
| Metias et al, 201767 | Canada | DM & HTN | 791 | - | - | - | Prospective Survey | |
| Bacha et al 201935 | Ethiopia | HTN | 385 | 57.6 | 54.5 | 48.3 | Cross-sectional, SRS | |
| Duque et al, 201841 | Portugal | HTN | 163 | - | - | - | O&C | Cross-sectional, Simple Random |
| N IK and B VR, 201548 | India | DM & HTN | 100 | 59 | 73 | 27 | O | Retrospective cross sectional |
| Parappilly et al, 201917 | Colombia | DM & HTN | 100 | 66.6 | 60 | 4 | MCQ | Cross-sectional, Convenient S |
| Kaddumukasa et al, 201745 | Uganda | HTN | 440 | 54 | - | - | Cross-sectional, | |
| Lai et al, 201549 | Taiwan | DM | 597 | 51.28 | - | - | Retrospective, SRS | |
| Selcuk Ozkan et al, 201958 | Turk | HTN | 336 | 53.2 | 39 | 61 | Cross-sectional, consecutive S |
Abbreviations: C, closed ended; O, open ended; MCQ, multiple choice questions; Y, yes/no questions; SRS, systematic random sampling; S, sampling; DM, diabetes mellitus; HTN, hypertension; Np, not participated.
Overall Knowledge Towards Stroke
Overall knowledge can be operationalized as knowing pick general concepts obtained from inquiries regarding the definition, cause, organs affected, and preventions of stroke. Of the reviewed studies, seven studies reported the calculated overall good knowledge of respondents towards stroke. As good awareness was shown in Ghana (79.18%),33 low awareness in Iraq (4.4%),32 Nigeria (16.9%),53 and Ethiopia (18.3%)29 were reported. The participants’ scope of knowledge that stroke affects the brain was also reported in six studies ranged from 21.6%,29 to 87.4%.34 With a comparative cross-sectional study aimed to assess the knowledge difference of native and migrant diabetic patients towards stroke in Germany and Turkey, only 50% of the native and 25% migrant diabetic cases responded exactly that the brain is the affected organ with stroke.65 The participants’ overall knowledge can be seen in Table 2.
Table 2.
Overall Knowledge of HTN and DM Patients Towards Stroke
| Study | Country | Disease Condition | Overall Good Knowledge of Stroke (%) | Know Stroke Affects Brain (%) |
|---|---|---|---|---|
| Abate A29 | Ethiopia | HTN | 18.30 a | 21.6 |
| Ehidiamen43 | Nigeria | HTN | NR | 56.3 |
| Dar39 | Pakistan | HTN | NR | 76 |
| Weltermann65 | Germany | DM | 39.4 a | 50- Native 25 -Migrant |
| Oparah53 | Nigeria | DM & HTN | 16.9 | NR |
| Arisegi34 | Nigeria | DM & HTN | 70.3 | 87.4 |
| Amen32 | Iraq | HTN | 4.4 | NR |
| Ampiah33 | Ghana | DM & HTN | 79.16b | 68.30 |
| Venkatesh61 | India | HTN | 66.7 | NR |
Notes: Associated factors: aage <61 years, educated, urban residents, high income, bmarried, employed, educated, NR-not reported.
Abbreviations: DM, diabetes mellitus; HTN, hypertension.
Knowledge Towards Warning Signs of Stroke
Seventeen studies have been employed to knowledge towards warning signs of a stroke. Out of these, eight articles revealed the computed prevalence of overall good level of knowledge of warning signs of stroke ranged from 23.6%53 to 87%;34 half of them were below 50%. The ability to name the signs/symptoms of stroke markedly varied between the studies. The signs of stroke sudden half body paralysis/weakness, sudden trouble speaking, sudden severe headache, and sudden double vision were reported by more than 65% of the studies. From these, 70–85% of studies reported low knowledge (<50%) of sudden double vision and severe headache as the signs of a stroke. Besides these, though few studies were reporting, there was low awareness detected to numbness, imbalance movement, memory loss, and dizziness. Unfortunately, eight studies depicted that 15–77% of the respondents did not know any sign of stroke as shown in Table 3.
Table 3.
Knowledge Towards Warning Signs of Stroke
| Study | Good Knowledge (%) | Did not Know any Sign (%) | Trouble Speaking (%) | One body Paralysis (%) | Double Vision (%) | Numbness (%) | Headache (%) | Dizziness (%) | Memory Loss (%) | Loss of Balance (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Abate A29 | – | 77.3 | – | 35.9 | – | – | – | – | – | – |
| Aboutorabi30 | – | – | 77.9 | 87.2 | 54.4 | – | 56.8 | – | 85.1 | 88.6 |
| Al-Beladi31 | 48.2 c | - | 36.1 | 43.4 | 22.9 | 35.5 | 22.9 | - | - | 33.1 |
| Amen32 | 24.6 a c | 34.2 | 28.9 | 29.8 | 23 | - | 23.7 | - | - | 20.20 |
| Ampiah33 | 75 d e | - | 75.5 | 70.2 | 48.5 | 69 | 66 | 59.6 | - | - |
| Arisegi34 | 87 a c d | - | 83.3 | 85.5 | 41 | - | 86.2 | 59.6 | 81.2 | |
| Dar, N39 | - | 26.2 | 67 | - | 28.6 | 66.9 | 32.8 | 34.6 | 22.4 | - |
| Ehidiamen43 | 54.9 abc | 45.1 | 28.5 | 36.1 | 0 | - | 0 | - | 0 | - |
| Mersal50 | - | - | 41.40 | 51.2 | 42.4 | 34 | 46 | 45.8 | - | 42.8 |
| Oparah53 | 23.6 | - | - | - | - | - | - | - | - | - |
| Venkatesh61 | - | - | - | 72.4 | - | - | 45.7 | - | - | - |
| Vincent62 | - | 15 | - | - | - | - | - | - | - | - |
| Weltermann65 | 53 | 24.3 | 25.2 | - | 9.2 | - | - | - | - | |
| Duque41 | - | 23.3 | 96.3 | 93.6 | - | 87.7 | 91.4 | - | - | |
| Faiz, K44 | 43.5 | 33.8 | 50.3 | 60.7 | 6.4 | - | 3.5 | 4.6 | 4.6 | 3.5 |
| Selcuk58 | 69 | 30 | 32 | 22 | 3.5 | 48 | 37 | - | ||
| Lai, Y49 | - | - | 63.5 | 67.1 | 31.5 | - | 10.4 | 26.1 | - | - |
Notes: Associated factors: aage <50, bmale, b*female, chigher education, demployed, emarital status/married.
Knowledge Towards Risk Factors of Stroke
Based on studies that stated on risk factor awareness, 10.5%32 to 86.6%34 overall good levels of risk factor knowledge were reported. But only two studies were reporting more than 50%.34,43 Despite it was not adequate, just more than half of the studies reported whether their respective subjects had better knowledge of HTN as the risk of stroke. The majority of studies reported a low level of knowledge to hypercholesterolemia, DM, past stroke history, cigarette smoking, obesity, physical inactivity, bad diet, alcohol intake, family history, elderly, and heart disease. Studies inquired on stress as a risk of stroke and revealed up to 96% of knowledge. However, the review found 2.3–77% of the HTN and DM patients that did not know any risk factors of stroke as shown in Table 4.
Table 4.
Knowledge Towards Risk Factors of Stroke
| Study | Good Knowledge to RF (%) | Did not Know any RF (%) | HTN (%) | DM (%) | Dyslipidemia (%) | Alcohol Use (%) | Physical Incivility (%) | Bad Diet (%) | Past Hx of Stroke (%) | Obesity (%) | CAD (%) | Family Hx (%) | Stress (%) | Smoking (%) | Elderly Age (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abate 29 | 14 | 77 | 3.6 | – | – | 18.7 | 21.6 | – | – | 20.1 | – | – | – | – | – |
| Al-Beladi31 | 38 c | - | 57.8 | 59.6 | - | - | - | - | - | - | - | 15.1 | 36.1 | 52.4 | 37.3 |
| Wahab63 | acdfg | 52 | 34.7 | 7.3 | - | 4.5 | - | 0.6 | - | 1.9 | 0.6 | - | 12.7 | 3.8 | - |
| Chukwuocha38 | - | 36.3 | 55 | 80 | - | - | - | - | - | - | - | - | - | 1 | - |
| Aboutorabi30 | - | - | 93 | 71.5 | 85.1 | 64.1 | 22.1 | 88.6 | 87.9 | 79.4 | 69.8 | 39.6 | 82.2 | 78.6 | 62.3 |
| Venkatesh61 | - | - | 80 | - | - | - | - | - | - | - | - | 18.6 | |||
| Weltermann65 | - | - | 27.5 | 21.6 | 4.5 | 14.7 | - | 4.1 | 29.8 | ||||||
| Poongothai54 | - | - | 76 | 64 | 24 | 32 | - | 24 | 16 | 16 | 12 | 32. | |||
| Dar39 | 19.5 | 2.3 | 93.4 | 45.3 | 37.7 | - | - | - | - | - | - | - | 30.4 | ||
| Arisegi34 | 86.6 c | - | 92 | 76.2 | 85.7 | 72.8 | 80.8 | 85.7 | 85 | 63.2 | 54.8 | 71 | 42.3 | ||
| Oparah53 | 49.3 c | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Mersal A50 | - | - | 56.7 | 43 | 48.8 | 34 | 47.3 | 37.9 | 39.9 | 48.3 | |||||
| Vincent62 | 15 | 80 | 61.5 | 3 | - | 5 | 0.5 | 22 | 1 | 0.5 | 11 | 24 | |||
| Amen32 | 10.5abce | 25 | - | - | 42.1 | 17.5 | 43 | 39.5 | 39.5 | 39.5 | |||||
| Ampiah33 | - | - | 87 | 77 | 76 | 79 | 74 | 71 | 42.3 | 76 | 69.7 | 35 | |||
| Ehidiamen43 | 56.9abc | - | 35.4 | 22.2 | - | 9.7 | - | - | - | - | - | - | 41 | 15.9 | - |
| Duque41 | 14 | 98.7 | 85.1 | 99.3 | 95.7 | 95.7 | 98.2 | 96.9 | 74.9 | 95.7 | 96.9 | ||||
| Faiz, K44 | 14.4 | 68.1 | 21.4 | 8.7 | 10 | 11.6 | 7.5 | 8.4 | 12.1 | 7.5 | 6.9 | 26.6 | |||
| Parappilly17 | 31 | 10 | |||||||||||||
| Metias67 | 49 | 12.4 | 27.4 | 4.7 | 16.5 | 20.7 | 10.1 | 13.7 | 43.7 | 3.7 | |||||
| Selcuk58 | 89 | 7 | 19 | 3 | 26 | 23 | 45 | 12 |
Notes: Associated factors: aage <55, b-male, b*female, ceducation, durban, elonger duration of disease, ftook health education previously, gfamily history of stroke.
Abbreviations: CAD, coronary artery disease; DM, diabetes mellitus; HTN, hypertension; Hx, history; RF, risk factor.
Knowledge Towards the Prevention of Stroke
Even though few studies were enrolled in the knowledge of stroke prevention, a single study reported the overall calculated level of stroke prevention knowledge (90.8%).34 Two authors reported 82–85% of subjects were knowing whether a stroke is preventable.33,39 Furthermore, four studies investigated and reported regular physical exercise (49–88%), avoiding fat intake (40–89%), and frequent use of vegetables (37–87%).17,34,39,61 Likewise, three studies reported whether subjects had knowhow of smoking cessation (6–85%) as prevention of stroke.34,39,61 Avoiding alcohol use and weight reduction were also revealed by studies as shown in Table 5.
Table 5.
Knowledge Towards the Prevention of Stroke
| Study | Good Knowledge of Prevention (%) | Know Stroke is Preventable (%) | Avoid Alcohol (%) | Avoid Fat Intake (%) | Smoking Cessation (%) | Physical Activity (%) | Weight Reduction (%) | Vegetable Use (%) |
|---|---|---|---|---|---|---|---|---|
| Venkatesh61 | – | – | 9.5 | 45.7 | 5.7 | 42.8 | 5.7 | 37.1 |
| Dar39 | – | 85.4 | – | 40.4 | 85.2 | 49 | – | 76 |
| Arisegi34 | 90.8 a | – | 77.8 | 88.7 | 78.6 | 88.3 | 87.9 | 87 |
| Parappilly17 | – | – | – | 57 | – | 51 | – | 52 |
| Ampiah33 | – | 82 | – | – | – | – | – | – |
Notes: Associated factors: aeducational and employment status.
Prevention Practices Towards Stroke
One of the prevention strategies of stroke emergency is pre-stroke LMP which is supported by many pieces of evidence.70 In this review, we extracted data from primary studies that were done related to LMP. In doing so, 29 studies were reviewed to generalize the trends of stroke prevention practices.
As a result, seven studies reported 2.4% (South Africa)52 to 72% (Ghana)51 prevalence of good LMP among the respondents. But only three studies were reporting more than 50% good practice.51,59,61 When asked what actions have you ever practice to maintain their body and to prevent the incidence of stroke, the majority of the studies reported sub-optimal practice; nineteen studies reported for smoking cessation (>50%), fourteen studies for avoiding alcohol (60–90%), nine studies for avoiding added salt (57–95%), five studies for vegetable use (60–100%), four studies for regular home/facility BP or blood glucose (BG) checking (57–77%), three studies for reducing fat intake (59–95%). However, the practice of regular physical exercise was too low. Similarly, weight reduction practice was low as shown in Table 6.
Table 6.
Prevention Practice Towards Stroke
| Study | Good Practice % | Medication Adherence % | Check BP/ BG Regularly% | Avoid Alcohol% | Avoid Fat Intake % | Not Add Salt % | Smoking Cessation % | Physical Activity % | Weight Reduction % | Vegetable Use (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Venkatesh61 | 62.9 | 79 | – | 10.5 | 75.2 | 71.4 | 52.4 | – | 62.9 | |
| Dar, N.Z39 | – | 45.1 | 38 | – | 40.4 | – | 85.2 | 49 | – | 76 |
| Mersal A50 | – | – | – | – | – | – | 43.3 | 55.2 | – | – |
| Arisegi34 | − bd | 66.5 | 9.2 | 75.7 | 39.7 | 58.6 | 85.4 | - | 36.8 | 41.8 |
| Amen32 | - | - | - | 91.2 | - | - | 49.1 | - | - | - |
| Konduru47 | - | - | 27 | - | - | - | - | 28 | - | - |
| Chimberengwa69 | a b | - | - | 75 | - | 41.1 | 88.2 | - | - | 73.7 |
| Metias67 | - | - | - | - | - | 56.4 | - | - | - | |
| Okonta52 | 2.4 | - | - | - | - | - | - | 8.3 | 2.3 | |
| Tesema60 | - | - | - | - | - | 94.6 | 98.5 | 14 | - | - |
| Buda37 | 27.3 b e | - | - | 87.9 | - | 57.5 | 91.2 | 16.1 | 41.9 | - |
| Durai42 | - | - | - | 72 | - | 75 | 89 | 89 | - | 3 |
| Mutyambizi68 | a b c | 67 | - | - | - | - | 85 | 9 | - | - |
| Rashidi57 | - | - | 57.3 | - | 59 | 76.35 | - | 37.25 | - | - |
| Sheeba59 | 63 | 88 | 63 | - | - | - | - | 46 | 57 | - |
| Dinesh40 | - | 48 | 65.25 | - | - | - | 46.75 | 20.5 | - | - |
| Bollampally66 | 41.25 | 64.35 | - | 81 | - | 61.25 | 95.7 | 16.25 | - | - |
| Warren-Findlow64 | 58 | 65.4 | 22.3 | 75 | 52.1 | 30.3 | - | |||
| Rajan55 | - | 84 | 77 | - | - | 72 | - | 9 | - | - |
| Kisokanth46 | - | - | 47.2 | - | - | - | - | - | - | 95 |
| Obirikorang51 | 72 b f | - | - | 84.3 | - | 92.7 | 98 | - | 99.4 | |
| Bakhsh36 | - | 46.7 | 19.8 | - | - | 79.3 | 31.2 | 57.3 | 60 | - |
| Rajasekharan56 | - | 60.50 | - | 63.1 | 93.8 | - | 70.3 | 43.4 | - | 26.20 |
| Bacha35 | 39.5 | - | - | 83 | - | - | 96.4 | - | - | - |
| Duque41 | - | - | 91.4 | - | - | 77.3 | - | - | - | |
| N IK. and B V48 | - | - | - | - | - | 74.6 | - | - | - | |
| Faiz44 | - | - | 73 | - | - | 76 | - | - | - | |
| Kaddumukasa45 | - | - | 93.5 | - | - | 95.7 | - | - | - | |
| Lai49 | - | 68 | - | - | 68.68 | - | - | - |
Notes: Associated factors: amale gender, beducation, curbane residency, demployed, eincome.
Discussion
To the reviewer’s knowledge, this systematic review has been the first paper synthesized regarding knowledge and prevention practices of stroke amongst hypertensive and diabetic patients. To undergo the review, the results of 42 existing articles were collected. The reported results were variable in between the studies. This might be due to the difference in the time course of the conducted studies and/or the variability in the socioeconomic status of the study population/study setting/. Irrespective of this, the overall results of the review show that the prevalent level of knowledge and LMP towards stroke was limited. Almost 40–80% of subjects were not aware of what a stroke is and the organ to be affected.29,43,65 Obviously, individuals with HTN and/or DM are at greater risk of suffering stroke.8,71 Hence, it is expected to be familiar with stroke and its warning signs.
The present review depicted that there was low awareness of the clinical signs and symptoms of a stroke.32,53 In contrast, two studies showed better knowledge of the signs/symptoms of a stroke.33,34 Even if suboptimal knowledge was found in other signs/symptoms, more than 50% of respondents did not know the exact double vision and severe headache as symptoms of a stroke in the majority of the reviewed studies. Severe headache,72 and double vision/diplopia are major clinical presentations that should be identified as warning symptoms of a stroke.5,73,74 So far, the reviewed studies reported 15–77% of patients with no knowledge of any of the mentioned warning signs of stroke as shown in Table 3.
It is important to note that left to unaware these vulnerable groups to the warning signs will come up with complicated medical situations up on attacked with stroke events. This is because not identifying the early warning signs leads to a prehospital delayed. The main reason for stroke victims too late hospital presentation was considered as their inability to recognize the symptoms of stroke, waiting for the sign to abate by itself, and eventually lack of awareness of the advantages that could be obtained from early treatment of thrombolysis.14–16 On the contrary, having previous information to this able to increased patient’s early hospital arrival by 10-fold thereby enhanced thrombolysis eligibility.75 Therefore, creating awareness of the sign and treatment of stroke has a paramount advantage to enhance the need for a rapid medical call.74–76
Years ago, many countries were launching an effective Face Arm Speech Time (FAST) campaign that can have a positive implication to increase public awareness to the warning signs of stroke and thereby to promote immediate response; it aimed to raise the need for rapid medical call whenever anyone manifest early warning signs and symptoms of stroke, ie, facial deviation, arm weakness, and speech disturbance. Their intention was not only to these signs of stroke but as far as possible to familiarize people even to other signs and symptoms of a stroke. Because the clinical manifestations may not be always similar in all individuals.74,77–81 Therefore, this review also suggests such educational strategies should be reconsidered and planned in the future.
Stroke awareness is necessary not only to the clinical signs and symptoms but also to the risk factors and prevention as well. The ultimate objective of conducting population awareness is to increase the trend of abstaining from those contributing lifestyle risk factors. However, almost all the reviewed studies stated that the HTN and/or DM patients’ level of recognition to the potential relation of stroke and risk factors has been low so that they were recommending educational programs/campaigns to be held as an important concern of the national health policies.29–31,38,39,43,50,53,54,65
Since stroke is multi-factorial, people especially risky individuals should be conscious enough to measure their level of exposure and to be away from those risk factors. Risk factor knowledge begins with the identification of the current own medical conditions. Surprisingly, 64.6% to 94.6% of the hypertensive29,43 and more than 78% of the diabetic patients65 were found that they did not know whether their own medical condition is the cause of a stroke as shown in Table 4.
By far the most cited risk factor of stroke in the majority of the reviewed studies was HTN.30,31,34,38,39,41,50,54,58,61,62 Though HTN is the major, it is not the only risk of stroke; other risk factors should be identified well. Some studies reported that more than 50% of the respective respondents with no knowledge to at least one risk factor of stroke.29,44,63 Of course, being hypertensive and/or hyperglycemic contributes to stroke events by itself; their effect is much accelerated whenever other modifiable lifestyle factors (ie, smoking, excessive alcohol use, physical inactivity/sedentary life, obesity, high cholesterol, and habit of diet) are poorly managed.70,82–85 However, the result of this review revealed that more than 85% of the sampled participants did not consider the above-listed behavioral factors as the risk of stroke.38,44,62,63,65,86
Interestingly, stress that was highlighted in many of the reviewed studies; 12.7%63 to 96%41 of the subjects consider it exactly as the risk of stroke. Noticeably, stressful life events increase 2–3 times to the emergence of stroke by increasing excessive sympathomimetic activity and other different postulated mechanisms.87–90 So, people at risk of stroke should identify and be away from any psychologically stressful situations. The review also found a low level of knowledge of the non-modifiable risk factors as if a stroke is highly associated with older age, family, and previous history of stroke.31–34,44,50,54,58,62 Therefore, it should be of great concern to healthcare providers that so many patients do not understand the cause of stroke and have a limited understanding of basic stroke prevention methods.
Another important finding worth of highlighted in this review was LMP as the primary prevention (PP) of stroke. Though stroke is preventable primarily by avoiding or reducing the contributing risk factors,70 the result of this review shows that more than 60% of the vulnerable individuals did not strive to prevent stroke and other cardiovascular complications.35,37,52,61,66 Take for example smoking; the pattern of smoking habit contributes 2–4 times the likelihood of developing stroke as compared to non-smokers.91,92 Nonetheless, with this review, 50–70% of subjects were found to be smokers with a double burden to their medical condition in some studies.32,36,40,50 This could amplify the rate of stroke in risky individuals unless immediate action is taken.84,85
Although its detailed biological mechanism is not clearly stated, evidence suggests physical activity (3–5 days/week) to reduce the likelihood of a stroke event.93–95 Unfortunately, subjects of the review level of engagement to practice regular physical exercise were found to be low. More than 70% of papers stated <50% of the respondents were striving to do regular physical exercise as shown in Table 6. Sedentary life has been the leading cause of mortality in the world; it increases 20–30% risk of all causes of death. Hence, WHO proposed in raising awareness of physical activity and to be a key component in the prevention of non-communicable diseases including stroke.96
Moreover, weight reduction was reported as a poor practice by many reviewed studies.34,37,52,64 Overweight and obesity are important public health problems associated with many serious medical conditions including stroke. Recent American College of Cardiology and American Heart Association (ACC/AHA) guidelines recommend weight reduction as PP of stroke and other cardiovascular complications.97 Alternatively, a cohort study also suggests that not only weight gain but also weight loss more than 5% should be emphasized to the increased incidence rate of Transient ischemic attack (TIA).98 Therefore, weight management to be optimal to prevent a stroke rate.
The trend of alcohol reduction practice was good in most studies but a single study in India showed too low (10.5%).61 This worldwide prevalent practice has been established as a risk factor for stroke disease principally hemorrhagic stroke since alcohol affects the coagulation pathway and cerebral vessel integrity.99 In fact, excessive alcohol use is a risk factor of stroke events, low to moderate alcohol intake has advantages to reduce the incidence of ischemic stroke.99–101 Regardless of this controversy alcohol is not that much recommended to be used especially in risky individuals.
Another point of discussion was medication adherence, which was reported 45–90% adherence to the prescribed antidiabetic and hypertensive medications as shown in Table 6. Even if they did not feel any problem, 55–77% of them were regularly checking their BP and/or BG either in-home or health facilities as was reported by the reviewed studies.40,55,57,59 This is good practice that should be advocated more for early prevention of HTN and DM-associated emergence of stroke. Because the most plausible reasons for stroke events have been uncontrolled BP and BG.1,4,9
So far, dietary conditions, ie, fat, salt, and vegetable use should have to be emphasized for PP of stroke as if there has been a suboptimal practice in few reviewed studies.102 Evidence showed that bad nutritional formula is considered as the risk of stroke, especially in high-risk populations. Early prevention of stroke and other cardiovascular complications starts from adjusting the day-to-day dietary conditions. For example, habiting the Mediterranean diet, high in olive oil, whole grains, fruits, vegetables, and legumes, and low in cholesterol/saturated fat is advised as prevention of stroke.103–105 Habiting these diets can reduce the stroke rate by up to 40% or more in high-risk patients.104 Hence, awareness to apply diet-based stroke prevention is necessary to these populations.
Finally, significantly associated sociodemographic factors of stroke knowledge and practice were systematically reviewed. As a result, educational level,29,31,32,34,43,53,63 urban residency,29,33,63 employment,33,34 age <60 years,29,32,34,63,65 monthly income29 and marital status30 were statistically associated with good level of stroke knowledge. Moreover, male gender in Nigeria43 and female in Iraqi32 was found to be strongly associated sole predictor variable of stroke knowledge. Similarly, LMP was affected with these independent sociodemographic factors; male gender,10,35 higher educational level,34,35,37,51,69 urban residency,35 income,37 employment34 and marital status.51 Meanwhile, the elderly and comorbidity were the preventive factors of good stroke prevention practice.37 The main highlighted reason for the high level of knowledge and practice to these subgroups was due to the sufficient and easy accessibility of the different information sources to them.
Limitation
Despite this review has strong parts like critically apprizing and compiling the results of the published articles systematically, some other limitations that we could not avoid may be here. The limitations might be obtained from the reviewed studies; some data were not complete; their data collection questioneers were not similar in studies that could reduce the generalizability of this review. Additionally, all the reviewed articles were published in journal cites; unpublished studies could not be accessed. So far, to show the result quantitatively, the pooled estimated value was not attempted to be calculated because of diverse outcomes and the insufficient data reported in the studies.
Conclusion
It is clear from the above discussion that knowledge and prevention practice of stroke amongst hypertensive and diabetic patients has been low. The reported level of knowledge in high-risk populations towards the general concepts, warning signs, risk factors, and prevention methods of stroke was very low. There is also suboptimal lifestyle modification practice to prevent stroke. Especially the trend of regular physical activity and weight reduction practice was relatively low. This inadequate knowledge and prevention practice were associated with elderly, educationally low, economically poor, rural residents, unmarried, unemployed, and comorbid populations. Finally, the review highlights the importance of increasing public awareness about stroke symptoms, risk factors, and prevention strategies as well.
Acknowledgment
The authors would like to thank their colleagues who gave constructive feedback on the completion of this paper.
Funding Statement
We did not receive specific funding for this work.
Abbreviations
ACC/AHA, American College of Cardiology and American Heart Association; AHA/ASA, American Heart Association and American Stroke Association; BG, Blood Glucose; DALYS, Disability-Adjusted Life Years; DM, Diabetes Mellitus; HTN, Hypertension; LMP, Lifestyle Modification Practice; NIH, National Institute of Health; PP, Primary Prevention; SSA, Sub-Saharan African; TIA, Transient Ischemic Attack; tPA, Tissue Plasminogen Activator; WHO, World Health Organization.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Feigin VL, Nichols E, Alam T, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurology. 2019;18(5):459–480. doi: 10.1016/S1474-4422(18)30499-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. [DOI] [PubMed] [Google Scholar]
- 3.WHO. The top 10 causes of death; 2016. Available from:https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed August4, 2021.
- 4.Namale G, Kamacooko O, Kinengyere A, et al. Risk factors for hemorrhagic and ischemic stroke in sub-Saharan Africa. J Trop Med. 2018;2018:1–11. doi: 10.1155/2018/4650851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fekadu G, Chelkeba L, Kebede A. Risk factors, clinical presentations and predictors of stroke among adult patients admitted to stroke unit of Jimma university medical center, south west Ethiopia: prospective observational study. BMC Neurol. 2019;19(1):183. doi: 10.1186/s12883-019-1412-5 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Owolabi MO, Sarfo F, Akinyemi R, et al. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Global Health. 2018;6(4):e436–e446. doi: 10.1016/S2214-109X(18)30002-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang F-L, Guo Z-N, Wu Y-H, et al. Prevalence of stroke and associated risk factors: a population based cross sectional study from northeast China. BMJ Open. 2017;7(9):e015758. doi: 10.1136/bmjopen-2016-015758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Habibi-koolaee M, Shahmoradi L, Niakan Kalhori SR, Ghannadan H, Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in gorgan: a retrospective hospital-based study–2015–2016. Neurol Res Int. 2018;2018:548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Onwuegbuzie GA, Reng RS. Diabetes as a risk factor for ischemic stroke in a tertiary health care center, Abuja. New Nigerian J Clin Res. 2018;7(11):16. [Google Scholar]
- 10.Owolabi L, Nagode M, Ibrahim A, Uloko A, Gezawa I, Datti M. Stroke in patients with diabetes mellitus: a study from North Western Nigeria. Afr Health Sci. 2016;16(3):781–789. doi: 10.4314/ahs.v16i3.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharif F, Ghulam S, Sharif A. Prevalence of risk factors associated with stroke. Pakistan Heart J. 2019;52(1):2–85. [Google Scholar]
- 12.Ghimire MR, Soti B, Prajapati S, Thapa L, Ghimire S, Shrestha S. Risk factors associated with stroke among the clients attending Neuro and Allied Clinic, Bhairahawa. Stroke J. 2019;3(1):1–8. [Google Scholar]
- 13.Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843 [DOI] [PubMed] [Google Scholar]
- 14.Arulprakash N, Umaiorubahan M. Causes of delayed arrival with acute ischemic stroke beyond the window period of thrombolysis. J Family Med Primary Care. 2018;7(6):1248. doi: 10.4103/jfmpc.jfmpc_122_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fladt J, Meier N, Thilemann S, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc. 2019;8(20):e013101. doi: 10.1161/JAHA.119.013101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahmoud Hewedi K. Pre-hospital and in hospital delays after the onset of acute ischemic stroke in a sample of Egyptian patients. Al-Azhar Med J. 2019;48(4):311–322. doi: 10.21608/amj.2019.64940 [DOI] [Google Scholar]
- 17.Parappilly BP, Field TS, Mortenson WB, Sakakibara BM, Eng JJ. Determinants influencing the prestroke health behaviors and cardiovascular disease risk of stroke patients: a Cross-Sectional Study. J Stroke Cerebrovascular Dis. 2019;28(6):1509–1518. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.015 [DOI] [PubMed] [Google Scholar]
- 18.Karkout RA, Shamaa O, Al Ammour ST, Abd Elmaged RS, Al Kassar LA, Al Ali MN. Knowledge about stroke among adults in Sharjah, United Arab Emirates. Int J Res Med Sci. 2019;7(10):3632. doi: 10.18203/2320-6012.ijrms20194194 [DOI] [Google Scholar]
- 19.Wan L-H, Zhao J, Zhang X-P, et al. Stroke prevention knowledge and prestroke health behaviors among hypertensive stroke patients in mainland China. J Cardiovascular Nursing. 2014;29(2):E1–E9. doi: 10.1097/JCN.0b013e31827f0ab5 [DOI] [PubMed] [Google Scholar]
- 20.Sowtali SN, Harith S, Mohamed M, Yusoff DM. Stroke knowledge level among stroke patients admitted to hospital Raja Perempuan Zainab II, Kelantan, Malaysia. J Exp Stroke Transl Med. 2016;9(1):1–11. [Google Scholar]
- 21.Indira Kumari N, Veera Raghavulu B. Risk factor assessment of stroke and its awareness among stroke survivors: a retrospective study. Int J Res Health Sci. 2015;3(1):140–145. [Google Scholar]
- 22.Alzahrani FA, Alenzy AE, Alghamdi AM. Stroke in Tabuk, KSA: awareness and prevalence of risk factors. Life Sci J. 2019;16(6):256. [Google Scholar]
- 23.Ojike N, Ravenell J, Seixas A, et al. Racial disparity in stroke awareness in the US: an analysis of the 2014 National Health Interview Survey. J Neurol Neurophysiol. 2016;7(2). doi: 10.4172/2155-9562.1000365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sadeghi-Hokmabadi E, Vahdati SS, Rikhtegar R, Ghasempour K, Rezabakhsh A. Public knowledge of people visiting Imam Reza hospital regarding stroke symptoms and risk factors. BMC Emerg Med. 2019;19(1):36. doi: 10.1186/s12873-019-0250-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karnad A, Pannelay A, Boshnakova A, Lovell AD, Cook RG. Stroke prevention in Europe: how are 11 European countries progressing toward the European Society of Cardiology (ESC) recommendations? Risk Manag Healthc Policy. 2018;11:117. doi: 10.2147/RMHP.S163439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Network E. PRISMA (2009) checklist for reporting systematic reviews and meta-analyses.. J ASEAN Federation Endocrine Societies. 2015;30(2):196. [Google Scholar]
- 27.Health NIo. National Institutes of Health Quality Assessment tool for Observational Cohort and Cross-Sectional Studies: National Institutes of Health. 2016. [Google Scholar]
- 28.Boateng D, Wekesah F, Browne JL, et al. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: a systematic review. PLoS One. 2017;12:12. doi: 10.1371/journal.pone.0189264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abate AT, Bayu N, Mariam TG. Hypertensive patients’ knowledge of risk factors and warning signs of stroke at Felege Hiwot Referral Hospital, Northwest Ethiopia: a cross-sectional study. Neurol Res Int. 2019;2019:1–7. doi: 10.1155/2019/8570428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aboutorabi-Zarchi M, Jam Ashkezari S, Gholami S, Razavi-Ratki SK, Namiranian N. Is Knowledge of type 2 diabetic patients about stroke acceptable - a cross sectional study. Iranian J Diabetes Obesity. 2019;11(1):22–27. [Google Scholar]
- 31.Al-Beladi B, Khulood M, Al O, Mesed A, Nafea R, Mosleh H. Awareness of stroke among diabetic and hypertensive patients at King Fahad hospital in al-madinah. KSA. 2018;2016:5. [Google Scholar]
- 32.Amen MR. Assessment of hypertensive patients’ knowledge about lifestyle risk factors and warning signs of stroke. J Contemporary Med Sci. 2016;2(5):28–32. [Google Scholar]
- 33.Ampiah PK. 2018 knowledge of stroke among hypertensive-diabetic patients at the national diabetes management and research centre of Korle-bu teaching hospital in Ghana. J Prevent Rehabilitative Med. 2018;1(1):46–62. [Google Scholar]
- 34.Arisegi SA, Awosan KJ, Oche MO, Sabir AA, Ibrahim MT. Knowledge and practices related to stroke prevention among hypertensive and diabetic patients attending Specialist Hospital, Sokoto, Nigeria. Pan African Med J. 2018;29(1):1–17. doi: 10.11604/pamj.2018.29.63.13252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bacha D, Abera H. Knowledge, Attitude and self-care practice towards control of hypertension among hypertensive patients on follow-up at St. Paul’s Hospital, Addis Ababa. Ethiop J Health Sci. 2019;29:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bakhsh LA, Adas AA, Murad MA, et al. Awareness and knowledge on hypertension and its self-care practices among hypertensive patients in Saudi Arabia. Ann Int Med Dent Res. 2017;2(5). doi: 10.21276/aimdr.2017.3.5.ME13. [DOI] [Google Scholar]
- 37.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertension. 2017;23(1):26. doi: 10.1186/s40885-017-0081-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chukwuocha I, Anyanwu A, Nwazor E. Awareness of stroke among subjects with diabetes mellitus attending a tertiary diabetes outpatient clinic in South-East Nigeria. Int J Endocrinol Metab Disord. 2018;4(1):364. [Google Scholar]
- 39.Dar NZ, Khan SA, Ahmad A, Maqsood S. Awareness of stroke and health-seeking practices among hypertensive patients in a tertiary care hospital: a cross-sectional survey. Cureus. 2019;11:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dinesh PV, Kulkarni AG, Gangadhar NK. Knowledge and self-care practices regarding diabetes among patients with Type 2 diabetes in Rural Sullia, Karnataka: a community-based, cross-sectional study. J Family Med Primary Care. 2016;5(4):847. doi: 10.4103/2249-4863.201176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duque AS, Fernandes L, Correia AF, et al. Awareness of stroke risk factors and warning signs and attitude to acute stroke. Int Arch Med. 2015;8:8. [Google Scholar]
- 42.Durai V, Muthuthandavan AR. Knowledge and practice on lifestyle modifications among males with hypertension. Indian J Community Health. 2015;27(1):143–149. [Google Scholar]
- 43.Ehidiamen OF, Ehinwenma OJ. Awareness of stroke risk factors and warning symptoms amongst hypertensive patients in Benin city. Ann Med Health Sci Res. 2018;1:78. [Google Scholar]
- 44.Faiz KW, Sundseth A, Thommessen B, Rønning OM. Patient knowledge on stroke risk factors, symptoms and treatment options. Vasc Health Risk Manag. 2018;14:37. doi: 10.2147/VHRM.S152173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaddumukasa M, Kayima J, Nakibuuka J, et al. Modifiable lifestyle risk factors for stroke among a high risk hypertensive population in Greater Kampala, Uganda; a cross-sectional study. BMC Res Notes. 2017;10(1):675. doi: 10.1186/s13104-017-3009-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kisokanth G. Perceptions, attitudes and self-care practices on management of hypertension among hypertensive patients at teaching hospital, Batticaloa district, Sri lanka. Open Hypertens J. 2018;10(1):1–7. doi: 10.2174/1876526201810010001 [DOI] [Google Scholar]
- 47.Konduru S, Ranjan A, Karthik SM, Shaik S, Vakkapatla LS. Assessment of diabetes related knowledge, attitude and practice among diabetics and non-diabetics using self prepared questionnaire for awareness of health promotion. Indian J of Pharm Pract. 2017;10:32–38. doi: 10.5530/ijopp.10.1.8 [DOI] [Google Scholar]
- 48.Ik N, Vr B. Risk factor assessment of stroke & its awareness among stroke survivors: a retrospective study. Int J Res Health Sci. 2015;3(1):140–145. [Google Scholar]
- 49.Lai Y-J, Hu H-Y, Lee Y-L, Ku P-W. A retrospective cohort study on the risk of stroke in relation to a priori health knowledge level among people with type 2 diabetes mellitus in Taiwan. BMC Cardiovasc Disord. 2017;17(1):130. doi: 10.1186/s12872-017-0568-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mersal FA, Tork HM. Stroke risk perception and its awareness among hypertensive patients in Qassim region Saudi Arabia. Majmaah J Health Sci. 2020;8(1):9–22. doi: 10.5455/mjhs.2020.01.003 [DOI] [Google Scholar]
- 51.Obirikorang Y, Obirikorang C, Acheampong E, et al. Adherence to lifestyle modification among hypertensive clients: a descriptive cross-sectional study. Open Access Library J. 2018;5(2):1–13. [Google Scholar]
- 52.Okonta HI, Ikombele JB, Ogunbanjo GA. Knowledge, attitude and practice regarding lifestyle modification in type 2 diabetic patients. African j Primary Health Care Family Med. 2014;6(1):1–6. doi: 10.4102/phcfm.v6i1.655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oparah SK, Uhegbu VM, Etokidem AJ. Knowledge of stroke among at risk persons: a survey of patients at a tertiary hospital in Calabar, Southern Nigeria. [Google Scholar]
- 54.Poongothai. R. Risk awareness and knowledge of stroke among hypertensive patients. Int J Sci Res. 2017;6(7):2. [Google Scholar]
- 55.Rajan J. Knowledge, attitude and practice of hypertension among hypertensive patients in a tertiary care teaching hospital. Int J Basic Clin Pharmacol. 2019;8(5):5. [Google Scholar]
- 56.Rajasekharan D, Kulkarni V, Unnikrishnan B, Kumar N, Holla R, Thapar R. Self care activities among patients with diabetes attending a tertiary care hospital in Mangalore Karnataka, India. Ann Med Health Sci Res. 2015;5(1):59–64. doi: 10.4103/2141-9248.149791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rashidi Y, Manaflouyan H, Azar FP, Nikniaz Z, Nikniaz L, Ghaffari S. Knowledge, attitude and practice of Iranian hypertensive patients regarding hypertension. J Cardiovascular Thoracic Res. 2018;10(1):14. doi: 10.15171/jcvtr.2018.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Selcuk Ozkan NA. Stroke awareness in people with hypertension. Medicine. 2019;8(3):651–654. [Google Scholar]
- 59.Sheeba S, Sneha A, Veena B. Knowledge and self‑care practices among diabetics. Asian J Pharm Clin Res. 2017;10(12):234–237. doi: 10.22159/ajpcr.2017.v10i12.21072 [DOI] [Google Scholar]
- 60.Tesema S, Disasa B, Kebamo S, Kadi E. Knowledge, attitude and practice regarding lifestyle modification of hypertensive patients at Jimma University specialized hospital, Ethiopia. Prim Health Care. 2016;6(1):218–221. [Google Scholar]
- 61.Venkatesh U, Srivastava D. Knowledge, attitude and practice in relation to stroke: comparative study between hypertensive and non-hypertensive patients attending a tertiary care centre in Gorakhpur, Uttar Pradesh. India J Med Sci Clin Res. 2016;4:15014–15021. doi: 10.18535/jmscr/v4i12.116 [DOI] [Google Scholar]
- 62.Vincent-Onabajo G, Mshelia JY, Abubakar U, et al. Knowledge of stroke risk factors among individuals diagnosed with hypertension and diabetes: a hospital-based survey. J Adv Med Med Res. 2015;3:1–8. [Google Scholar]
- 63.Wahab KW, Kayode OO, Musa OI. Knowledge of stroke risk factors among Nigerians at high risk. J Stroke Cerebrovascular Dis. 2015;24(1):125–129. doi: 10.1016/j.jstrokecerebrovasdis.2014.07.053 [DOI] [PubMed] [Google Scholar]
- 64.Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103(6):503–512. doi: 10.1016/S0027-9684(15)30365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weltermann BM, Driouach-Bleckmann Y, Reinders S, Berndt P, Gesenhues S. Stroke knowledge among diabetics: a cross-sectional study on the influence of age, gender, education, and migration status. BMC Neurol. 2013;13(1):202. doi: 10.1186/1471-2377-13-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bollampally M, Chandershekhar P, Kumar K, Surakasula A, Srikanth S, Reddy T. Assessment of patient’s knowledge, attitude and practice regarding hypertension. Int J Res Med Sci. 2016;4(6):3299–3304. doi: 10.18203/2320-6012.ijrms20162283 [DOI] [Google Scholar]
- 67.Metias MM, Eisenberg N, Clemente MD, et al. Public health campaigns and their effect on stroke knowledge in a high-risk urban population: a five-year study. Vascular. 2017;25(5):497–503. doi: 10.1177/1708538117691879 [DOI] [PubMed] [Google Scholar]
- 68.Mutyambizi C, Pavlova M, Hongoro C, Groot W. Inequalities and factors associated with adherence to diabetes self-care practices amongst patients at two public hospitals in Gauteng, South Africa. BMC Endocr Disord. 2020;20(1):15. doi: 10.1186/s12902-020-0492-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chimberengwa PT, Naidoo M. Knowledge, attitudes and practices related to hypertension among residents of a disadvantaged rural community in southern Zimbabwe. PLoS One. 2019;14(6):e0215500. doi: 10.1371/journal.pone.0215500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kalkonde YV, Alladi S, Kaul S, Hachinski V. Stroke prevention strategies in the developing world. Stroke. 2018;49(12):3092–3097. doi: 10.1161/STROKEAHA.118.017384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang J, Wen X, Li W, Li X, Wang Y, Lu W. Risk factors for stroke in the Chinese population: a systematic review and meta-analysis. J Stroke Cerebrovascular Dis. 2017;26(3):509–517. doi: 10.1016/j.jstrokecerebrovasdis.2016.12.002 [DOI] [PubMed] [Google Scholar]
- 72.Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: a systematic review and meta-analysis. Neurology. 2020;94(1):e75–e86. doi: 10.1212/WNL.0000000000008591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rathore SS, Hinn AR, Cooper LS, Tyroler HA, Rosamond WD. Characterization of incident stroke signs and symptoms: findings from the atherosclerosis risk in communities study. Stroke. 2002;33(11):2718–2721. doi: 10.1161/01.STR.0000035286.87503.31 [DOI] [PubMed] [Google Scholar]
- 74.American stroke association. Stroke Symptoms; 2020. Available from:https://www.stroke.org/en/about-stroke/stroke-symptoms. Accessed June7, 2020.
- 75.Nepal G, Yadav JK, Basnet B, Shrestha TM, Kharel G, Ojha R. Status of prehospital delay and intravenous thrombolysis in the management of acute ischemic stroke in Nepal. BMC Neurol. 2019;19(1):155. doi: 10.1186/s12883-019-1378-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim YS, Park -S-S, Bae H-J, et al. Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol. 2011;11(1):2. doi: 10.1186/1471-2377-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bray J, Finn J, Cameron P, et al. Stroke public awareness campaign are associated with improved ambulance use for stroke and tia in Victoria, Australia. Circulation. 2017;136(suppl_1):A16355–A16355. [Google Scholar]
- 78.Vo LP, Souksavong JH, Tran A, Chang J, Lor KB. Impact of the Act FAST stroke campaign delivered by student pharmacists on the primary prevention of stroke. J Am Pharmacists Assoc. 2017;57(3):326–332. doi: 10.1016/j.japh.2017.02.026 [DOI] [PubMed] [Google Scholar]
- 79.Nordanstig A, Asplund K, Norrving B, Wahlgren N, Wester P, Rosengren L. Impact of the Swedish National Stroke Campaign on stroke awareness. Acta Neurol Scand. 2017;136(4):345–351. doi: 10.1111/ane.12777 [DOI] [PubMed] [Google Scholar]
- 80.Hartigan I, O’Connell E, O’Brien S, et al. The Irish national stroke awareness campaign: a stroke of success? Applied Nursing Res. 2014;27(4):e13–e19. doi: 10.1016/j.apnr.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 81.Advani R, Naess H, Kurz M. Mass media intervention in western Norway aimed at improving public recognition of stroke, emergency response, and acute treatment. J Stroke Cerebrovasc Dis. 2016;25(6):1467–1472. doi: 10.1016/j.jstrokecerebrovasdis.2016.02.026 [DOI] [PubMed] [Google Scholar]
- 82.Sarfo FS, Mobula LM, Plange-Rhule J, Ansong D, Ofori-Adjei D. Incident stroke among Ghanaians with hypertension and diabetes: a multicenter, prospective cohort study. J Neurol Sci. 2018;395:17–24. doi: 10.1016/j.jns.2018.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kumar D. Association of modifiable risk factors with ischemic stroke among hypertensive patients (case control study at tertiary care hospital, Karachi). Int J Nur & Hos Car. 2018;1:3–07. [Google Scholar]
- 84.Huangfu X, Zhu Z, Zhong C, et al. Smoking, hypertension, and their combined effect on ischemic stroke incidence: a prospective study among inner Mongolians in China. J Stroke Cerebrovascular Dis. 2017;26(12):2749–2754. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.048 [DOI] [PubMed] [Google Scholar]
- 85.Nakamura K, Nakagawa H, Sakurai M, et al. Influence of smoking combined with another risk factor on the risk of mortality from coronary heart disease and stroke: pooled analysis of 10 Japanese cohort studies. Cerebrovascular Dis. 2012;33(5):480–491. doi: 10.1159/000336764 [DOI] [PubMed] [Google Scholar]
- 86.Sundseth A, Faiz KW, Rønning OM, Thommessen B. Factors related to knowledge of stroke symptoms and risk factors in a Norwegian stroke population. J Stroke Cerebrovascular Dis. 2014;23(7):1849–1855. doi: 10.1016/j.jstrokecerebrovasdis.2014.02.026 [DOI] [PubMed] [Google Scholar]
- 87.Ramírez-Moreno J, Vega PM, Espada S, Alberca SB, Aguirre J, Peral D. Association between self-perceived psychological stress and transitory ischaemic attack and minor stroke: a case–control study. Neurología. 2019;2:798. [DOI] [PubMed] [Google Scholar]
- 88.Gradus JL, Farkas DK, Svensson E, et al. Associations between stress disorders and cardiovascular disease events in the Danish population. BMJ Open. 2015;5(12):e009334. doi: 10.1136/bmjopen-2015-009334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kotlęga D, Gołąb-Janowska M, Masztalewicz M, Ciećwież S, Nowacki P. The emotional stress and risk of ischemic stroke. Neurol Neurochir Pol. 2016;50(4):265–270. doi: 10.1016/j.pjnns.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 90.Jood K, Redfors P, Rosengren A, Blomstrand C, Jern C. Self-perceived psychological stress and ischemic stroke: a case-control study. BMC Med. 2009;7(1):53. doi: 10.1186/1741-7015-7-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pan B, Jin X, Jun L, Qiu S, Zheng Q, Pan M. The relationship between smoking and stroke: a meta-analysis. Medicine. 2019;98:12. doi: 10.1097/MD.0000000000014872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Monica W, Widyaningsih V, Sulaeman ES. Meta-analysis on the effects of hypertension, type ii diabetes mellitus, and smoking on the risk of stroke among asian young adult Population. J Epidemiol Public Health. 2019;4(4):296–306. doi: 10.26911/jepublichealth.2019.04.04.04 [DOI] [Google Scholar]
- 93.Prior PL, Suskin N. Exercise for stroke prevention. Stroke Vascular Neurol. 2018;3(2):59–68. doi: 10.1136/svn-2018-000155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Middleton LE, Corbett D, Brooks D, et al. Physical activity in the prevention of ischemic stroke and improvement of outcomes: a narrative review. Neurosci Biobehav Rev. 2013;37(2):133–137. doi: 10.1016/j.neubiorev.2012.11.011 [DOI] [PubMed] [Google Scholar]
- 95.Autenrieth CS, Evenson KR, Yatsuya H, Shahar E, Baggett C, Rosamond WD. Association between physical activity and risk of stroke subtypes: the atherosclerosis risk in communities study. Neuroepidemiology. 2013;40(2):109–116. doi: 10.1159/000342151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.García Ruiz R, Silva Fernández J, García Ruiz RM, et al. Response to symptoms and prehospital delay in stroke patients. Is it time to reconsider stroke awareness campaigns? J Stroke Cerebrovasc Dis. 2018;27(3):625–632. doi: 10.1016/j.jstrokecerebrovasdis.2017.09.036 [DOI] [PubMed] [Google Scholar]
- 97.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74(10):e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cho J-H, Rhee E-J, Park SE, et al. Maintenance of body weight is an important determinant for the risk of ischemic stroke: a nationwide population-based cohort study. PLoS One. 2019;14(1):e0210153. doi: 10.1371/journal.pone.0210153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Larsson SC, Wallin A, Wolk A, Markus HS. Differing association of alcohol consumption with different stroke types: a systematic review and meta-analysis. BMC Med. 2016;14(1):178. doi: 10.1186/s12916-016-0721-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Christensen AI, Nordestgaard BG, Tolstrup JS. Alcohol intake and risk of ischemic and haemorrhagic stroke: results from a Mendelian randomisation study. J Stroke. 2018;20(2):218. doi: 10.5853/jos.2017.01466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cunningham SA, Mosher A, Judd SE, et al. Alcohol consumption and incident stroke among older adults. J Gerontol. 2018;73(4):636–648. doi: 10.1093/geronb/gbw153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pandian JD, Gall SL, Kate MP, et al. Prevention of stroke: a global perspective. Lancet. 2018;392(10154):1269–1278. doi: 10.1016/S0140-6736(18)31269-8 [DOI] [PubMed] [Google Scholar]
- 103.Niewada M, Michel P. Lifestyle modification for stroke prevention: facts and fiction. Curr Opin Neurol. 2016;29(1):9–13. doi: 10.1097/WCO.0000000000000285 [DOI] [PubMed] [Google Scholar]
- 104.Spence JD. Nutrition in stroke prevention. Paper presented at: seminars in neurology; 2017 [DOI] [PubMed] [Google Scholar]
- 105.Tsivgoulis G, Psaltopoulou T, Wadley VG, et al. Adherence to a Mediterranean diet and prediction of incident stroke. Stroke. 2015;46(3):780–785. doi: 10.1161/STROKEAHA.114.007894 [DOI] [PMC free article] [PubMed] [Google Scholar]