Abstract
A multimodality approach in addition to high level of clinical suspicion and thorough physical examination is important in the diagnosis and management of left ventricular aneurysm and rupture after a silent inferior infarction.
Keywords: ischemia, left ventricle aneurysm, mechanical complications, myocardial infarction, ventricular septal rupture
A multimodality approach in addition to high level of clinical suspicion and thorough physical examination is important in the diagnosis and management of left ventricular aneurysm and rupture after a silent inferior infarction.

1. QUESTION
A 68‐year‐old man, whose medical history is significant for hypertension and diabetes mellitus type II, was admitted for constant substernal chest pressure and exertional dyspnea associated with orthopnea and bilateral lower extremity edema for 1 week. His exam was remarkable for elevated jugular venous pressure, a holosystolic murmur at the left lower sternal border radiating toward the apex, and 2+ pitting edema in bilateral lower extremities. Electrocardiogram (EKG) showed right bundle branch block with T wave inversions in inferior and anterolateral leads without a prior EKG for comparison. Serial troponin levels were negative, and the brain‐natriuretic peptide level was elevated (535 pg/mL). Chest radiograph showed cardiomegaly and interstitial edema.
2. WHAT IS THE DIAGNOSIS?
2.1. Answer
New‐onset heart failure with rare concomitant occurrence of ventricular septal rupture (VSR) and left ventricular aneurysm (LVA) secondary to silent inferior infarction.
An echocardiogram (TTE) revealed a 4.5 cm LVA extending from the base to mid‐section of the inferoseptum (Figure 1A) and a VSR of 1.5 cm in mid‐ventricular septum (Figure 1B) with an estimated Qp:Qs of 1.6. Heparin drip was discontinued ~24 hours after acute coronary syndrome was ruled out, and heart failure therapy was started. Cardiac magnetic resonance imaging (CMR) was obtained which showed a 6 cm inferior wall LVA (Figure 2A) and a 0.8 cm inferobasal VSR (Figure 2B). Coronary angiography showed 90% stenosis of the proximal right coronary artery (RCA) with severe diffuse distal disease (Figure 3A) and a 50% focal napkin ring lesion of the proximal left main coronary artery (Figure 3B). Coronary artery bypass graft (CABG) and left ventriculoplasty were subsequently performed with left internal mammary artery to left anterior descending artery and saphenous vein graft to obtuse marginal artery. The LVA was resected and the VSR was repaired using a Dacron Patch. Post‐surgery TTE showed successful LVA repair (Figure 4A) and resolution of previous VSR without residual interventricular shunt (Figure 4B). Our case demonstrated a rare concomitant occurrence of VSR and LVA secondary to silent inferior infarction. Given the high mortality, clinicians should be vigilant in their evaluation for post‐MI mechanical complications.1 A multimodality approach can facilitate the diagnosis and management of these complications. Although surgical repair remains the definitive treatment for VSR and selectively indicated in certain LVA cases, the optimal timing should be considered in an individualized fashion.1
FIGURE 1.
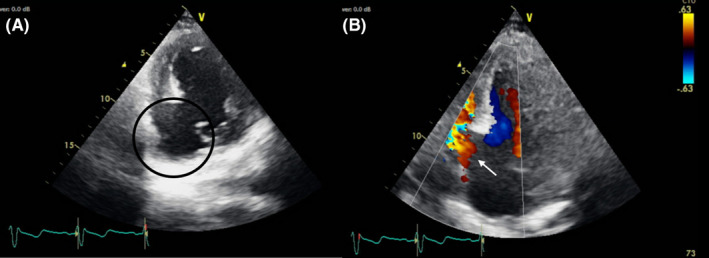
Transthoracic echocardiogram demonstrating ventricular septal aneurysm and defect. A, Left ventricle short axis view showing an inferobasal septal left ventricular aneurysm (circled in black). B, Modified apical view showing a ventricular septal defect from the base to mid inferoseptum with left to right shunt (black arrow)
FIGURE 2.
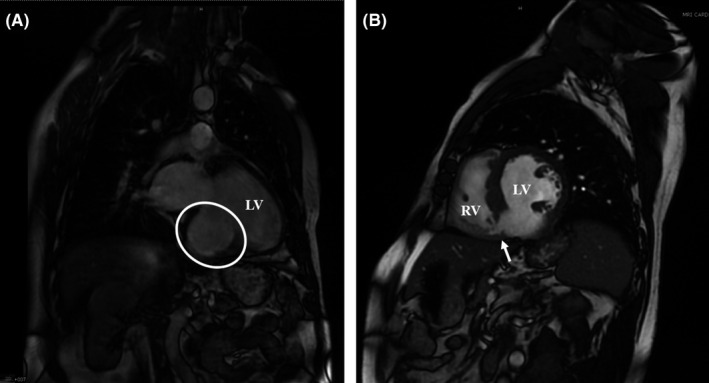
Cardiac magnetic resonance imaging showing left ventricular septal defect and aneurysm. A, Cardiac magnetic resonance imaging (MRI) coronal view showing the left ventricular (LV) inferobasal septal aneurysm (outlined by the white circle). B, Cardiac MRI sagittal view showing the inferobasal septal defect (black arrow) with the interventricular connection between the left ventricle (LV) and the right ventricle (RV)
FIGURE 3.
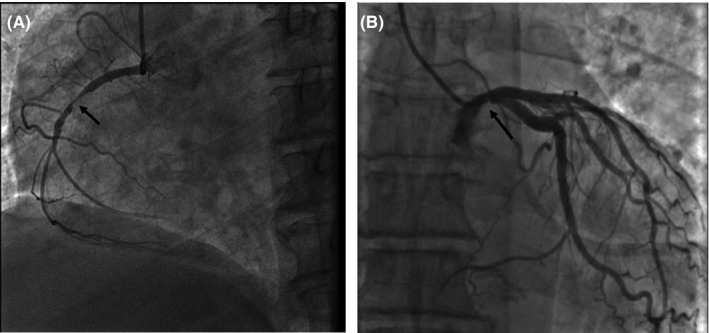
Coronary angiogram. A, The proximal right coronary artery is 90% occluded (arrow). B, Proximal left main coronary artery has a 50% focal napkin ring lesion (arrow)
FIGURE 4.
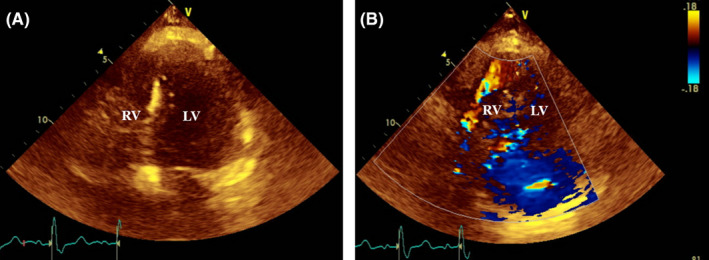
Post‐VSR and LVA repair TTE. A, Previously found inferobasal LVA is no longer visualized. B, No interventricular connection or residual shunt between LV and RV is visualized with color Doppler
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
HLN: substantially contributed to conception and design, or acquisition of data, or analysis and interpretation of data, involved in drafting the manuscript or revising it critically for important intellectual content, involved in final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. HLN, NP, NL and RT: involved in drafting the manuscript or revising it critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
ETHICAL APPROVAL
The paper is in compliance with Wiley's Publication Ethical Guidelines.
CONSENT STATEMENT
Published with written consent of the patient.
ACKNOWLEDGMENTS
We would like to thank reviewers for their time in reviewing and providing valuable feedback to improve the current manuscript
Nguyen HL, Palaskas N, Lakkis N, Tabbaa R. Rare silent ischemic ventricular septal aneurysm and rupture: A multimodality diagnostic approach. Clin Case Rep. 2021;9:e04284. 10.1002/ccr3.4284
DATA AVAILABILITY STATEMENT
All relevant data have been included in the current manuscript.
REFERENCES
- 1.Arnaoutakis GJ, Zhao Y, George TJ, Sciortino CM, McCarthy PM, Conte JV. Surgical repair of ventricular septal defect after myocardial infarction: outcomes from the society of thoracic surgeons national database. Ann Thorac Surg. 2012;94(2):436‐444. 10.1016/j.athoracsur.2012.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data have been included in the current manuscript.


