Abstract
Primary pleural angiosarcoma (PPA) is an extremely rare and clinically aggressive tumor. We report the case of a 66-year-old man having PPA with chest computed tomography (CT) scan showing a large oval-shaped, nonenhancing high attenuation cystic mass in the left hemithorax. Morphological and immunohistochemical findings supported the diagnosis of epithelioid angiosarcoma. Pleural angiosarcoma should be considered in the differential diagnosis of spontaneous hemothorax manifesting as high attenuation loculated pleural fluid on CT.
Keywords: Angiosarcoma, Pleura, Hemothorax, Pyothorax, CT
Introduction
Angiosarcoma is a rare malignant tumor that accounts for about 1–2% of all soft tissue sarcomas. This tumor originates from the endothelial cells of small blood vessels and can affect any organ, often occurring in the skin, soft tissues, liver, spleen, heart, and breast. Primary pleural angiosarcoma (PPA) is an extremely rare malignancy and only 50 cases have been reported in the English literature. The majority of reported cases describe the pathology and clinical findings of PPA [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], and only a few reports elaborated on the specific radiologic findings of PPA. Radiologic findings of the disease are nonspecific including pleural effusion, pleural mass or thickening, and PPA is pathologically difficult to diagnose unless sufficient samples are available [1], [2], [3].
Herein, we report a case of PPA manifesting as loculated hemothorax mimicking chronic empyema and review the computed tomography (CT) findings of PPA.
Case report
A 66-year-old man was admitted to the respiratory clinic with a one-week history of blood-tinged sputum and cough. The patient was a never smoker and had no history of fever, weight loss, chest pain, or dyspnea.
A huge left pleural effusion was seen on the initial chest radiograph. CT showed a localized round-shaped, nonenhancing high attenuation (HU 55) mass with diffuse minimal pleural thickening and a focal enhancing soft tissue lesion at the medial aspect of the pleural mass, which was thought to be collapsed lung tissue abutting pleural empyema or mixed lymph node enlargement. Based on the CT findings, we considered the most likely diagnosis to be a chronic pleural empyema complicated by a hemothorax, and less likely, a pyothorax-related malignancy (Figs. 1 A–C).
Fig. 1.
Enhanced chest computed tomography (CT) for initial workup of the left pleural effusion (A, B, C) shows heterogeneous attenuation (mean 55 HU) of left pleural fluid (A), diffusely and evenly thickened left pleura with a few nodular pleural calcification (B), and small soft tissue mass-like density (arrows) medial to pleural mass (C).
Analysis of the hemorrhagic fluid drained through the percutaneous drainage (PCD) catheter revealed a large number of red and white blood cells (WBCs). Bronchoscopy showed hemorrhage from the left lower lobar bronchus. No malignant cells were seen on the fluid obtained after bronchoalveolar lavage and PCD catheter insertion. Acid-fast bacilli staining and tuberculosis (TB) polymerase chain reaction were negative.
About 4 months later, the patient was re-admitted through our emergency room with dyspnea and hemoptysis. A repeat chest CT demonstrated that the heterogeneous fluid collection in the left pleural space was unchanged, but there was a newly developed left lateral enhancing pleural mass and an interval increase in the size of the previous soft tissue lesion at the medial aspect of the loculated hemothorax (Figs. 2 A-C). The patient underwent positron emission tomography-computed tomography (PET-CT) (Figs. 2 D) and biopsy with chest tube insertion via video-assisted thoracotomy to rule out an underlying malignancy. The chest tube discharged 100-300 cc of blood per day. The PET-CT scan showed hypermetabolism at the soft tissue mass site along the loculated hemothorax. Pathologic analysis of the biopsy specimen showed fibrosis and necrosis.
Fig. 2.
Enhanced chest computed tomography (CT) (A, B, C) for follow up after 4 months was done. No significant changes were observed of the amount of the left pleural fluid (A). However, the size of the soft tissue mass (arrows) at the left pleura and the retrocardiac space (B) was increased and new soft tissue lesion (arrows) was detected at the lowermost portion of left pleura (C). Positron emission tomography-computed tomography (PETCT) (D) revealed hypermetabolism at the pleural masses and subcarinal node .
For the purpose of both diagnosis and hemostasis, a left thoracotomy was performed. Surgical exploration revealed a large hematoma mixed with a soft tissue mass in the left pleural cavity and the mass adhered to the left lower lobe. The mass was inseparable from the surrounding soft tissue. The tumor was cut open and its contents were removed to the greatest extent possible.
Immunohistochemical examination of the resected specimen confirmed a pleural epithelioid angiosarcoma (CD31 +, CD34 +, CK -, CK7 -, CK5/6 -, Calretinin -, D2-40 -, Vimentin -) (Figs. 3 A,B). The patient lost consciousness due to persistent dyspnea and bleeding over the next few days and deteriorated quickly and died within a week.
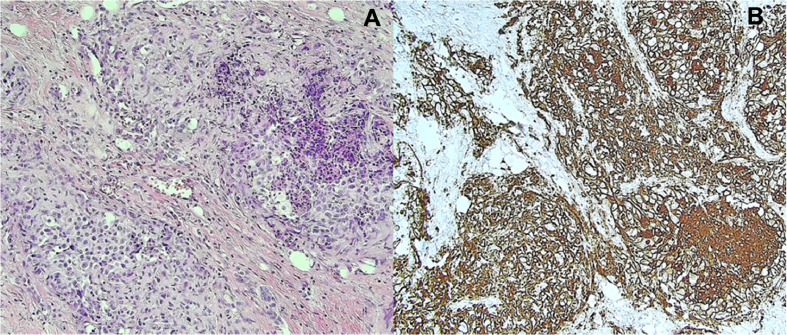
Fig. 3.
The angiosarcoma tissues were stained with hematoxylin (A) and eosin and analyzed by immunohistochemistry. The tumor cells were strongly positive for CD34 (B).
Discussion
The clinical manifestation of PPA is usually nonspecific. The most common symptoms are thoracic chest pain, pleural pain, hemoptysis, anemia, and recurring hemothorax. The pathogenesis and etiology of PPA are still unclear. Japanese researchers reviewed nine cases of PPA and found an association with a history of chronic tuberculous pyothorax [17], while western research reported pleural angiosarcoma is related with a history of radiation and asbestos exposure [2]. However, most reported PPA cases are unrelated to these factors, which means that most PPA are de novo tumor.
We conducted a literature review and identified 15 cases of PPA with corresponding CT image findings [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17]. Free pleural effusion was found in 6 cases, loculated pleural effusion in 7 cases, pleural soft tissue mass in 5 cases, and diffuse pleural thickening in 5 cases. In 11 cases, hemothorax was diagnosed through CT, pleural fluid analysis, or surgery.
Among the 7 cases of loculated pleural effusion, 6 cases with hemothorax were confirmed by CT or fluid analysis. Loculated hemothorax can be easily confused with pyothorax. There were 2 cases of pyothorax-associated pleural angiosarcoma with CT imaging [9,17]. In one case [9], there was a pleural mass within a shrunken hemithorax due to old pleurisy that was revealed to be a hematoma related to pleural angiosarcoma during surgery. This case was actually not a pyothorax-associated pleural angiosarcoma but localuated hematoma on shrunken hemithorax due to old pleural empyema . In the other case [17], CT showed a localized pleural empyema with rim calcification and small pleural bulging, and distant vertebral body metastasis.
The radiologic features of PPA are nonspecific, and it is difficult to distinguish pleural angiosarcoma clearly from other pleural tumors through imaging alone. On CT, the lesion appears to be a heterogeneous enhancement with pleural nodules or masses and may be accompanied by pleural effusion and thickening. PET-CT may be used to determine the extent of the lesion [6].
According to Liu et al [18], discrimination between hemothorax and empyema was obtained with a cutoff value of 15.9 HU of the pleural fluid attenuation. However, it is not easy to distinguish chronic pleural empyema from spontaneous loculated hemothorax, because the incidence of the latter is much lower than that of pleural empyema and pyothorax-related hemothorax. Decreased volume of the involved hemithorax and pleural calcification are common findings of pyothorax, but not loculated hemothorax, in PPA cases.
The most important differential diagnoses of PPA manifesting as loculated pleural fluid include benign complications of chronic empyema; pyothorax associated lymphoma; other rare malignant tumors such as mesothelioma, malignant fibrous histiocytoma; and squamous cell carcinoma. Reactivated tuberculosis can also result in aggressive features that can mimic PPA. In our case, we initially misdiagnosed the patient with TB empyema, because we considered that the combined soft tissue density around the pleural fluid collection was too small to be a tumor.
Ueda et al [19] described the radiologic features of pyothorax-associated lymphoma and concluded that lymphoma usually arises at the margin of the pleural empyema cavity secondary to chronic stimulation by the long-standing presence of empyema which favors the development of neoplasia in the pleura. On the contrary, spontaneous hemothorax is the main associated finding with PPA and occurs due to the highly hemorrhagic feature of angiosarcoma, and the pleural mass of PPA can occur anywhere in the hemothorax pleural cavity. Spontaneous loculated hemothorax is a more common manifestation of PPA than of other pleural tumors such as mesothelioma and adenocarcinoma.
Careful pathologic examination and immunohistochemical examination with sufficient samples play an important role in the diagnosis of pleural angiosarcoma, as most cases are the epithelioid type and can be confused with other primary pleural tumors or metastatic pleural tumors. To confirm angiosarcoma, at least one endothelial cell marker (including CD31, CD34, factor VIII) must be positively expressed. CD31 is the most specific and sensitive marker, and FLI-1 is known to be helpful for diagnosis [2].
Surgery is the best option for localized disease, and chemotherapy and radiation therapy can be used as adjuvant or palliative treatment. However, most patients with PPA have a poor prognosis and die within a few months of diagnosis [1], [2].
In our patient, de novo type PPA occurred without any specific risk factors and presented as a loculated hemothorax on CT. Initial pathologic evaluation of the pleural fluid did not provide an accurate diagnosis, and PPA could only be diagnosed by immunohistochemistry of a sufficient sample obtained after surgery.
In conclusion, radiologists should consider the possibility of pleural angiosarcoma in patients with spontaneous hemothorax manifesting as high attenuation loculated pleural fluid on CT, and should examine in detail the presence of a pleural mass on CT. In addition, because of the difficulty in identifying malignant cells by pleural fluid analysis alone, clinicians should obtain sufficient tissue for an accurate diagnosis.
Funding
None.
Patient consent
Informed consent for publication of this case was obtained from the patient.
References
- 1.Durani U, Gallo de Moraes A, Beachey J. Epithelioid angiosarcoma: A rare cause of pericarditis and pleural effusion. Respir Med Case Rep. 2018;24:77–80. doi: 10.1016/j.rmcr.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang PJ, Livolsi VA, Brooks JJ. Malignant epithelioid vascular tumors of the pleura: report of a series and literature review. Hum Pathol. 2000;31:29–34. doi: 10.1016/s0046-8177(00)80194-x. [DOI] [PubMed] [Google Scholar]
- 3.Panjwani A, Singh I, Parvataneni N. Spontaneous hemothorax: primary pleural epithelioid angiosarcoma. Egypt J Intern Med. 2016;28:170–173. [Google Scholar]
- 4.Zhang S, Zheng Y, Liu W. Primary epithelioid angiosarcoma of the pleura: a case report and review of literature. Int J Clin Exp Pathol. 2015;8:2153–2158. [PMC free article] [PubMed] [Google Scholar]
- 5.Roh MS, Seo JY, Hong SH. Epithelioid angiosarcoma of the pleura: a case report. J Korean Med Sci. 2001;16:792–795. doi: 10.3346/jkms.2001.16.6.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azzakhmam M, Elktaibi A, El Ochi MR. Primary epitheloid angiosarcoma of the pleura: an exceptional tumor location. Pan Afr Med J. 2019;33:327. doi: 10.11604/pamj.2019.33.327.18145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lorentziadis M, Sourlas A. Primary de novo angiosarcoma of the pleura. Ann Thorac Surg. 2012;93:996–998. doi: 10.1016/j.athoracsur.2011.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Alexiou C, Clelland CA, Robinson D. Primary angiosarcomas of the chest wall and pleura. Eur J Cardiothorac Surg. 1998;14:523–526. doi: 10.1016/s1010-7940(98)00211-5. [DOI] [PubMed] [Google Scholar]
- 9.Kimura M, Ito H, Furuta T. Pyothorax-associated angiosarcoma of the pleura with metastasis to the brain. Pathol Int. 2003;53:547–551. doi: 10.1046/j.1440-1827.2003.01510.x. [DOI] [PubMed] [Google Scholar]
- 10.Pramesh CS, Madur BP, Raina S. Angiosarcoma of the pleura. Ann Thorac Cardiovasc Surg. 2004;10:187–190. [PubMed] [Google Scholar]
- 11.Chen L, Shih HJ, Seguerra E Jr. Pathologic quiz case: a 39-year-old man with diffuse pleural thickening and massive hemothorax. Epithelioid angiosarcoma of pleura. Arch Pathol Lab Med. 2004;128:1299–1300. doi: 10.5858/2004-128-1299-PQCAYM. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz JE, Serra S, Duclos B. Diffuse primary angiosarcoma of the pleura: a case report and review of the literature. Sarcoma. 2004;8:103–106. doi: 10.1155/2004/794907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dainese E, Pozzi B, Milani M. Primary pleural epithelioid angiosarcoma. A case report and review of the literature. Pathol Res Pract. 2010;206:415–419. doi: 10.1016/j.prp.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Miyazaki H, Goto A, Hino R. Pleural cavity angiosarcoma arising in chronic expanding hematoma after pneumonectomy. Hum Pathol. 2011;42:1576–1579. doi: 10.1016/j.humpath.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 15.Abu-Zaid A, Mohammed S. Primary pleural angiosarcoma in a 63-year-old gentleman. Case Rep Pulmonol. 2013;2013 doi: 10.1155/2013/974567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quesada A, Quesada J, Khalil K. Morphoproteomic study of primary pleural angiosarcoma of lymphangioendothelial lineage: a case report. Ann Clin Lab Sci. 2013;43:317–322. [PubMed] [Google Scholar]
- 17.Kubo S, Kobayashi N, Kaneko A. Computed tomography imaging-based observation of the aggressive growth of angiosarcoma: a case study. Respirol Case Rep. 2019;7:e00479. doi: 10.1002/rcr2.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu F, Huang YC, Ng Y-B. Differentiate pleural effusion from hemothorax after blunt chest trauma; comparison of computed tomography attenuation values. J Acute Med. 2016;6:1–6. [Google Scholar]
- 19.Ueda T, Andreas C, Itami J. Pyothorax-associated lymphoma: imaging findings. AJR Am J Roentgenol. 2010;194:76–84. doi: 10.2214/AJR.09.2603. [DOI] [PubMed] [Google Scholar]