Abstract
In four high‐risk patients with chronically occluded femoro‐popliteal bypass suffering from Rutherford 4‐5 chronic limb threatening ischemia we performed, as an alternative for redo surgery, endovasculair relining with covered stent grafts. During follow‐up (3, 8, 14 and 20 months) one patient had redo percutaneous intervention and eventually below‐the‐knee amputation.
Keywords: critical limb ischemia, endovascular intervention, stent graft, vascular surgery
For frail patients suffering from chronic limb threatening ischemia due to a chronically occluded bypass, who are at high risk when complex open procedures are necessary due to comprehensive prior vascular interventions, endovascular relining of the bypass with covered stents seems to be a viable alternative with low‐perioperative morbidity.

1. INTRODUCTION
Chronic limb threatening ischemia (CLTI) represents the end stage of peripheral artery disease. The incidence is estimated to be between 500 and 1000 per million per year.1 Treatment consists of risk factor management, best medical treatment, and revascularization. Based on the patient‐average risk and individual clinical and anatomical status an endovascular approach or open surgery will be considered. Although there has been a shift from open to endovascular treatment, open surgery still plays an important role for patients with CLTI.2 The patency rate of bypass surgery in these patients is around 60% after 3 years of follow‐up.3 This might explain why, nowadays, one in six patients scheduled for bypass surgery had previous ipsilateral bypass surgery.4 Randomized‐controlled trials regarding treatment of CLTI based on occluded femoro‐popliteal bypass are lacking; however, studies on redo bypass surgery in CLTI patients show more postoperative complications,5, 6 as well as higher rates of re‐intervention and amputation when compared to, patients with no history of ipsilateral arterial procedures.7
In order to avoid redo surgery in these patients with chronically occluded bypasses, endovascular treatment can be considered a good alternative. While endovascular options might reduce perioperative morbidity and result in limb salvage, it should be noted that technical failure rates for endoluminal or subintimal recanalisation of the native vessels in long femoro‐popliteal occlusions are approximately 10%.8 Because of high‐morbidity rates of redo bypass surgery and/or inability to cross the occluded native vessels in redo CLTI endovascular procedures, we sought to find a different solution for these patients in need for revascularization. We describe four cases of chronically occluded above‐the‐knee or below‐the‐knee femoro‐popliteal bypasses, in which the occluded bypass was relined with covered stent grafts.
2. CASE REPORT
2.1. Case 1
A 69‐year‐old male patient presented with gangrene of his left forefoot. His general medical history revealed, among others, a recent cardiac arrest based on a myocardial infarction and a carotid endarterectomy (Table 1). In addition, he was known with comprehensive peripheral vascular diseases; an above‐the‐knee prosthetic bypass was constructed, followed by a below‐the‐knee venous bypass. Several percutaneous transluminal angioplasty (PTA) procedures were performed with stenting of the common and external iliac artery (EIA). The bypass has occluded several times resulting in numerous redo procedures including additional stent placement across the distal anastomosis of the above‐the‐knee prosthetic bypass (6 × 40 mm self‐expandable stent), as well as in the popliteal artery (PA) (5 × 40 mm self‐expandable stent) just a few months prior to the current procedure.
TABLE 1.
Clinical characteristics
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| Age (years) | 69 | 87 | 75 | 79 |
| Sex | male | male | male | male |
| Diabetes | No | Yes | No | No |
| Renal dysfunction | No | Yes | No | No |
| Congestive heart failure | Yes | Yes | No | No |
| Myocardial infarction | Yes | No | Yes | Yes |
| Stroke | Yes | Yes | Yes | No |
| Hypertension | Yes | Yes | Yes | Yes |
| Atrial fibrillation | Yes | Yes | No | No |
| COPD | Yes | No | No | No |
| ASA class | 3 | 4 | 3 | 3 |
| Rutherford class | 5 | 5 | 5 | 4 |
| Occluded bypass | ||||
| Distal landing | Above knee | Below knee | Below knee | Above knee |
| Material | Prosthetic | Vein | Vein | Prosthetic |
Abbreviations: ASA, American Society of Anesthesiologists Physical Status; COPD, Chronic Obstructive Pulmonary Disease.
Because of both his extensive medical history and numerous vascular (redo) procedures in his left leg the patient was deemed unfit for another redo bypass operation. Percutaneous intervention of the native arterial system had been tried several times in the years before without success (resulting in bypass surgery). Therefore, we chose to engage the occluded bypass primarily and reline it with a covered stent graft thus creating an endoluminal bypass within an occluded bypass.
After ultrasound‐guided puncture of the right common femoral artery (CFA), a 7 Fr crossover sheath was placed. Angiography indeed showed patent iliac stents but complete occlusion of the above‐the‐knee prosthetic bypass and stent at the distal anastomosis. Initially, recanalization of the native superficial femoral artery (SFA) was tried but reentry at the distal level proved to be impossible. Also antegrade cannulation of the occluded bypass failed. Therefore, retrograde access via the popliteal stent was obtained and a 4 Fr sheath was placed in the PA. The occluded above‐the‐knee prosthetic bypass was cannulated retrogradely using a 0.018” wire. After pick up of this wire and reversal and exchange for a 0.035” wire, the procedure was continued in an antegrade fashion. Predilation of the occluded bypass and occluded part of PA was performed using a 5 mm PTA balloon starting dilatation at the distal end, then at the proximal end followed by dilatation of the middle part of the bypass. The occluded above‐the‐knee prosthetic bypass was relined with a 6 × 250 mm and a 5 × 250 mm covered stent graft (Viabahn, W.L. Gore) with postdilatation using the 4 mm balloon starting distally, then proximally and the middle part at the end. A completion angiography showed patent iliac stents, and both covered stents graft in the previous occluded above‐the‐knee prosthetic bypass, with outflow of three crural vessels (Figure 1). In addition, an amputation of the second toe of the left foot was performed. Patient was prescribed dual antiplatelet therapy (DAPT). Follow‐up visits with duplex ultrasound were scheduled for 6 weeks, 3, 6, 12, and 24 months after the procedure, as has also been advised in recent publications.9
FIGURE 1.
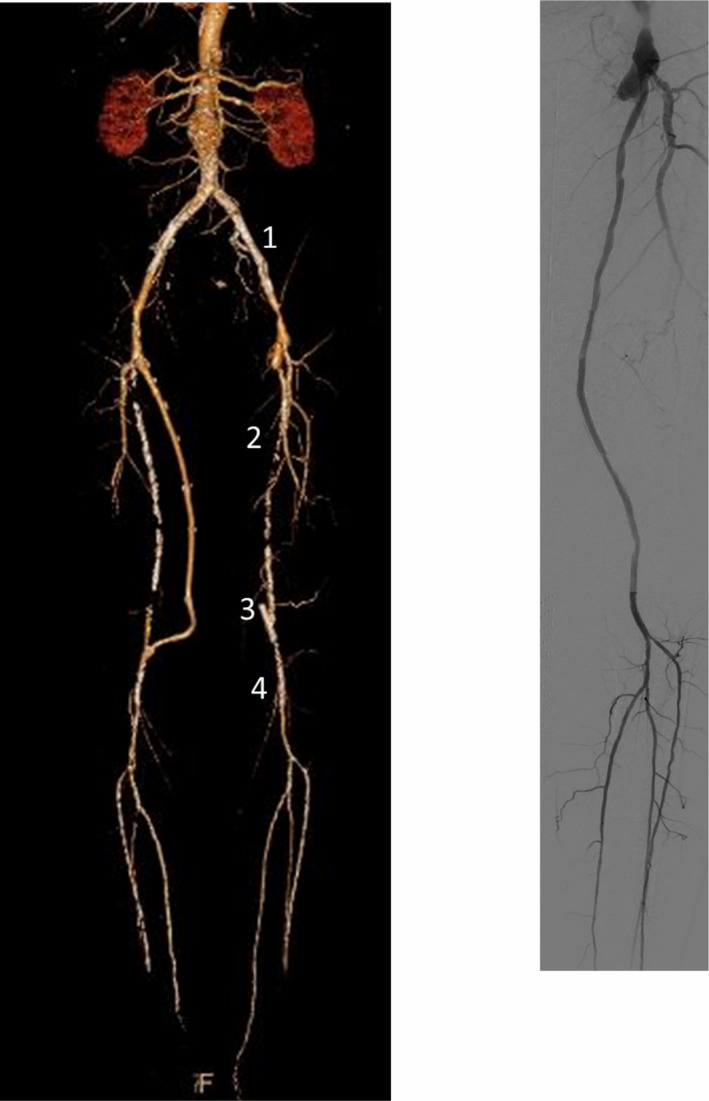
Case 1: Preoperative CT angiography showing the occluded left‐sided bypass with (A) patent stents in CIA and EIA, (B) occluded above‐the‐knee and occluded below‐the‐knee bypasses, (C) occluded stent at distal anastomosis of above‐the‐knee bypass, (D) patent self‐expandable stent in PA. Postoperative angiography showing the relined occluded above‐the‐knee prosthetic bypass
At the routine surveillance ultrasound 6 months after the procedure a stenosis of the distal edge of the stent graft was detected and treated successfully with PTA. Ten months after the procedure the patient presented with acute limb ischemia of his left leg due to an occlusion of the stent grafts and thrombolysis was started. As thrombolysis did not result in resolvement of the thrombus, thrombectomy and patch angioplasty of the distal PA was performed using a medial approach of the distal PA. Six months after this procedure the relined above‐the‐knee prosthetic bypass was patent on duplex ultrasound without signs of restenosis. Twenty months after the initial procedure the patient again presented with acute limb ischemia due to a re‐occlusion of the stent grafts. This eventually led to a transtibial amputation.
2.2. Case 2
A 87‐year‐old male patient presented with gangrene of his right foot one year after he underwent a below‐the‐knee venous bypass for acute limb ischemia. The bypass already needed a PTA procedure for a proximal stenosis within the previous year and was now occluded for several weeks based on clinical history. His further medical history revealed diabetes, hypertension, chronic renal dysfunction, carotid endarterectomy, atrial fibrillation and chronic limb ischemia of his left foot for which he was treated several times with PTA procedures in the previous year (Table 1). Due to his extensive medical co‐morbidities and patient preference an open approach or redo bypass was not an option. Previous endovascular interventions of the ipsilateral SFA and PA failed. Therefore, a relining of the occluded below‐the‐knee bypass was considered.
After ultrasound‐guided puncture of the left CFA a 7 Fr crossover sheath was placed. Angiography indeed showed an occluded below‐the‐knee venous bypass. The occluded bypass was engaged and cannulated. Subsequently, an angiography was performed. After predilatation with a 4 mm balloon of the proximal bypass (the distal part of the bypass was open), the occluded bypass was relined using 2 5 × 250 mm and a 5 × 50 mm covered stent graft (Viabahn, W.L. Gore) with postdilatation using the 4 mm balloon starting distally, then proximally and the middle part at the end (Figure S1).
The vitamin K‐antagonist was resumed after the procedure. Three and six months after the procedure the ultrasound duplex showed a patent relined below‐the‐knee venous bypass. Eight months after the procedure the patient died due to his extensive co‐morbidities with a patent bypass and without the need for major amputation.
2.3. Case 3
A 75‐year‐old male patient presented with critical ischemia of his right foot due to an occluded below‐the‐knee venous bypass. On CTA, a stenosis of the distal EIA and the proximal CFA were found, an occlusion of the SFA and, an occlusion of the below‐the‐knee venous bypass. The distal PA as well as the trifurcation was patent. Due to his co‐morbidity (Table 1) and previous ipsilateral vascular procedures an endovascular procedure was preferred.
After ultrasound‐guided retrograde puncture of the left CFA a 7 Fr crossover sheath was placed. Angiography indeed showed an occluded below‐the‐knee venous bypass. The occluded bypass was engaged and cannulated. After predilatation using a 4 mm balloon according to the standardized manner, the occluded below‐the‐knee venous bypass was relined with a 5 × 250 mm, a 6 × 250 mm and a 6 × 50 mm covered stent graft (Viabahn, W.L. Gore) with postdilatation using the 4 mm balloon starting distally, then proximally and the middle part at the end. Due to a stenosis of the distal anastomosis of the bypass an additional nitinol self‐expandable stent (5 × 40 mm, Innova, Boston Scientific) was placed (Figure 2A).
FIGURE 2.
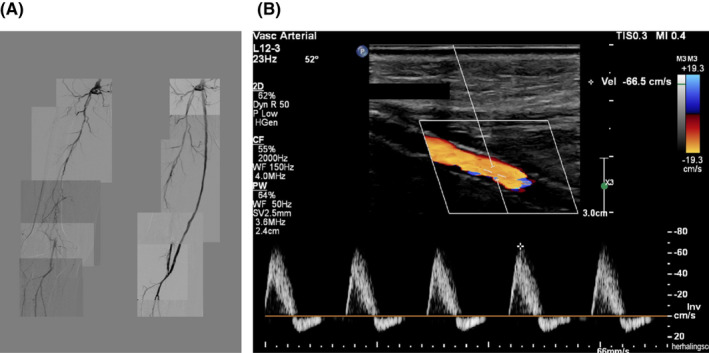
(A) Case 3: Pre‐ and postprocedure angiography of relined occluded below‐the‐knee venous bypass. (B) Case 3: Duplex ultrasound surveilance of the relined occluded below‐the‐knee venous bypass 12 months after the procedure
The completion angiography showed patent three covered stents grafts in the previous occluded below‐the‐knee venous bypass, and outflow of three crural vessels (Figure 2A). After the procedure rivaroxaban and aspirin was resumed. At 3, 6 and 12 months follow‐up the ultrasound duplex (Figure 2B) showed a patent relined below‐the‐knee venous bypass without signs of restenosis.
2.4. Case 4
A 79‐year‐old male patient presented with CLTI (Rutherford class 4) of his right foot. His medical history included prostate cancer with lymph node metastases for which he was treated with radiation therapy and hormone therapy. In addition, the patient had comprehensive peripheral vascular diseases; in 1995 on both legs above‐the‐knee prosthetic bypasses were constructed and multiple endovascular interventions for iliac disease. In 2009, after occlusion of the left above‐the‐knee prosthetic bypass a below‐the‐knee venous bypass was constructed, which was complicated by wound infection and prolonged hospitalization. Given the limited life expectancy of the patient combined with his strong disfavor for open reconstruction and possible quality of life impairment in case of complications after redo bypass surgery, we chose for an endovascular solution for his CLTI on the right side. On CTA, stenosis of the right common and EIA was found with a total occlusion of the right SFA, occlusion of the right above‐the‐knee prosthetic bypass with an occluded and extremely calcified PA distal to the distal anastomosis.
After ultrasound‐guided retrograde puncture of the left CFA a 7 Fr crossover sheath was placed. Angiography confirmed the CTA findings. A PTA procedure of the common and EIA was performed and a balloon expandable 9 × 29 mm stent (Isthmus Logic, AlviMedical) was placed to treat the common iliac artery stenosis. Using a 0.035” glidewire and PIER catheter the occluded above‐the‐knee prosthetic bypass was engaged and cannulated. After predilation (5 mm, distally 6 mm balloon) an interwoven nitinol stent (5 × 80 mm, Supera, Abbott) was placed across the distal anastomosis to tackle the extensive calcifications in the native PA. Subsequently, the occluded above‐the‐knee prosthetic bypass was relined with a 6 × 250 mm and 6 × 150 mm covered stent graft (Viabahn, W.L. Gore). Proximal of the covered stent grafts an additional 6 × 40 mm self‐expandable nitinol stent was placed (Innova, Boston Scientific). Postdilatation was performed with a 5 mm balloon, starting proximally at the last placed self‐expandable stent, then distally and then the middle part at the end (Figure S2). After the procedure DAPT‐ was restarted. At six weeks and 3 months follow‐up the ultrasound duplex showed a patent relined below‐the‐knee prosthetic bypass and the patient was free of symptoms.
3. DISCUSSION
In our four frail patients suffering from CLTI due to a chronically occluded bypass, endovascular relining of the bypass with covered stents seems to be a viable alternative for open revision with low perioperative morbidity. This technique could be a relatively simple alternative in the armament of treating high‐risk patients with technically challenging lesions. Our findings are in line with the initial experiences by Fujimura et al.10 in a heterogeneous group of patients (64% CLTI) with an occluded above‐the‐knee prosthetic bypass that also suggested good results in prosthetic bypasses.
Although relatively easy cannulation of the occluded bypasses was achieved even in autologous vein bypasses that were occluded for months, there are several potential pitfalls and risks in the described procedures. In particular pre‐ and postdilatation are procedures with risk of embolization of thrombotic material from within the occluded bypass to either the distal arteries or proximal into the common femoral or deep femoral artery potentially resulting in devastating consequences when not treated appropriately. In contrast to Fujimura et al.10 where 79% of patients underwent concomitant thrombectomy or thrombus aspiration in order to reduce the risk of thromboembolisms we had a different protection algorithm. In order to minimize this risk we carefully predilated the occluded bypasses in a standardized manner, starting with a long balloon at the distal end overlapping a few centimeters into the native PA, then at the proximal end overlapping just into the CFA and after that the remainder of the bypass. In our patients none had thrombectomy or thrombus aspiration prior to stent placement and with appropriate care in sizing and order of pre‐ and postdilatation we experienced no negative effects.
Because of the risk of perioperative thromboembolism we chose a stent graft over an open self‐expandable stent design. Furthermore, stent grafts have shown good result in native femoro‐popliteal lesions in previous trials.11, 12 In long and complex TASC C and D native femoro‐popliteal lesion 1‐year primary and secondary patency rates were approximately 65% and 90% respectively. Compared to open bypass surgery in these trials stent grafts resulted in less morbidity, faster recovery, and improvement in quality of life while patency rates were similar. It might be argued that domains as morbidity, recovery and quality of life are even more affected in patients undergoing redo bypass surgery.
Longterm antiplatelet therapy reduces artherotrombotic events and improves patency and limb salvage. In line with current guidelines, for the two patients who previously had monotherapy (clopidogrel) DAPT (aspirin plus clopidogrel) was prescribed after the procedure. Two patients used anticoagulation medication, which were discontinued during the procedure and resumed after the procedure while aspirin was added. Considering the recently published trial it might be considered to have these patients on rivaroxaban and aspirin as efficacy and safety of this combination seems to be proven.13
4. CONCLUSION
This case report of four patients, suffering from CLTI due to a chronically occluded bypass, offers a new technique for patients who are very frail and/or when complex open procedures are necessary due to comprehensive prior vascular interventions. In these patients relining of the occluded bypass with covered stent grafts might be considered.
CONFLICTS OF INTEREST
The authors disclose no conflicts of interest.
AUTHOR CONTRIBUTIONS
AN: Acquired the data and wrote the manuscripts. OS: performed the surgery, acquired the data, wrote the manuscript and supervised. HS: performed the surgery and contributed to the manuscript editing. All authors: contributed sufficiently and met the criteria for authorship.
ETHICAL APPROVAL
All procedures were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration and its later amendments or comparable ethical standards.
Supporting information
Figure S1
Figure S2
van Nistelrooij AMJ, van ’t Sant HP, Schouten O. Covered stent grafts for relining of chronically occluded femoro‐popliteal bypasses in frail patients. Clin Case Rep. 2021;9:e04647. 10.1002/ccr3.4647
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Menard MT, Farber A, Assmann SF, et al. Design and rationale of the best endovascular versus best surgical therapy for patients with critical limb ischemia (BEST‐CLI) Trial. J Am Heart Assoc. 2016;5(7):e003219. 10.1161/JAHA.116.003219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodney PP, Tarulli M, Faerber AE, Schanzer A, Zwolak RM. Fifteen‐year trends in lower limb amputation, revascularization, and preventive measures among medicare patients. JAMA Surg. 2015;150(1):84‐86. 10.1001/jamasurg.2014.1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schouten O, Hoedt MT, Wittens CH, et al. End‐to‐end versus end‐to‐side distal anastomosis in femoropopliteal bypasses; results of a randomized multicenter trial. Eur J Vasc Endovasc Surg. 2005;29:457‐462. [DOI] [PubMed] [Google Scholar]
- 4.Reifsnyder T, Arhuidese IJ, Hicks CW, et al. Contemporary outcomes for open infrainguinal bypass in the endovascular era. Ann Vasc Surg. 2016;30:52‐58. 10.1016/j.avsg.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 5.Nolan BW, De Martino RR, Stone DH, et al. Prior failed ipsilateral percutaneous endovascular intervention in patients with critical limb ischemia predicts poor outcome after lower extremity bypass. J Vasc Surg. 2011;54(3):730‐736. 10.1016/j.jvs.2011.03.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodewes TCF, Ultee KHJ, Soden PA, et al. Perioperative outcomes of infrainguinal bypass surgery in patients with and without prior revascularization. J Vasc Surg. 2017;65(5):1354‐1365.e2. 10.1016/j.jvs.2016.10.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones DW, Schanzer A, Zhao Y, et al. Growing Impact of restenosis on the surgical treatment of peripheral arterial disease. J Am Heart Assoc. 2013;2(6):e000345. 10.1161/JAHA.113.000345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soga Y, Iida O, Suzuki K, et al. Initial and 3‐year results after subintimal versus intraluminal approach for long femoropopliteal occlusion treated with a self‐expandable nitinol stent. J Vasc Surg. 2013;58(6):1547‐1555. 10.1016/j.jvs.2013.05.107 [DOI] [PubMed] [Google Scholar]
- 9.Venermo M, Sprynger M, Desormais I, et al. Editor's choice–follow‐up of patients after revascularisation for peripheral arterial diseases: a consensus document from the European society of cardiology working group on aorta and peripheral vascular diseases and the European society for vascular surgery. Eur J Vasc Endovasc Surg. 2019;58(5):641‐653. 10.1016/j.ejvs.2019.06.017 [DOI] [PubMed] [Google Scholar]
- 10.Fujimura N, Obara H, Iwasa K, et al. Preliminary experience of viabahn stent graft inside the occluded prosthetic bypass graft for the treatment of above knee femoropopliteal bypass occlusion. Cardiovasc Intervent Radiol. 2019;43(2):223‐230. 10.1007/s00270-019-02376-6 [DOI] [PubMed] [Google Scholar]
- 11.Reijnen MMPJ, van Walraven LA, Fritschy WM, et al. 1‐Year results of a multicenter randomized controlled trial comparing heparin‐bonded endoluminal to femoropopliteal bypass. JACC Cardiovasc Interv. 2017;10(22):2320‐2331. 10.1016/j.jcin.2017.09.013 [DOI] [PubMed] [Google Scholar]
- 12.Zeller T, Peeters P, Bosiers M, et al. Heparin‐bonded stent‐graft for the treatment of TASC II C and D femoropopliteal lesions: the viabahn‐25 cm trial. J Endovasc Ther. 2014;21(6):765‐774. 10.1583/14-4790R.1 [DOI] [PubMed] [Google Scholar]
- 13.Bonaca MP, Bauersachs RM, Anand SS, et al. Rivaroxaban in peripheral artery disease after revascularization. N Engl J Med. 2020;382(21):1994‐2004. 10.1056/NEJMoa2000052 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Figure S2
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


