Abstract
The novel pandemic of coronavirus infection (COVID-19) has been linked with coagulopathy and thromboembolic events, causing limb loss and finally death. The present report describes a case of upper limb ischemia in a patient with COVID-19 infection, who lacked conventional risk factors for acute limb ischemia (ALI).mAn 83 year-old man with intraluminal thrombus and the occlusion of the axillary and brachial arteries, ceasing blood supply to the distal part of the body, was tested positive for the COVID-19 infection. The patient received therapeutic anticoagulation and underwent open thromboembolectomy, which failed to save the patient's life. The link between COVID-19 and thromboembolism remains unknown and needs further studies to be disclosed.
The novel coronavirus infection (COVID-19) can be associated with coagulopathy, which may cause thromboembolic events.1 The COVID-19 disease is an emerging threat due to the risk of thrombosis in microvascular, venous, and arterial beds. Moreover, thrombosis in patients with the COVID-19 infection may also be more extensive, leading to limb loss and death.2 Acute limb ischemia (ALI) is characterized with an abrupt decrease in the arterial perfusion of a limb, threatening its viability and integrity.3 The present report describes a patient developing upper-ALI, without any conventional risk factor for ALI, in a patient with confirmed COVID-19 infection.
CASE REPORT
An 83 year-old Iranian man came to our hospital with the symptoms of sudden pallor, pain, and paresthesia in his left upper limb in the past 10 hrs. He also reported a history of illness, fever, and dyspnea in the past week. He had no previous medical history and was not taking any drug. Examining his vital signs showed low blood pressure (BP = 90/60 mmHg), fever (40°C), tachycardia (heart rate = 110), tachypnea (respiratory rate = 30 cycles per minute), and the peripheral oxygen saturation of 75% while breathing in the ambient air.
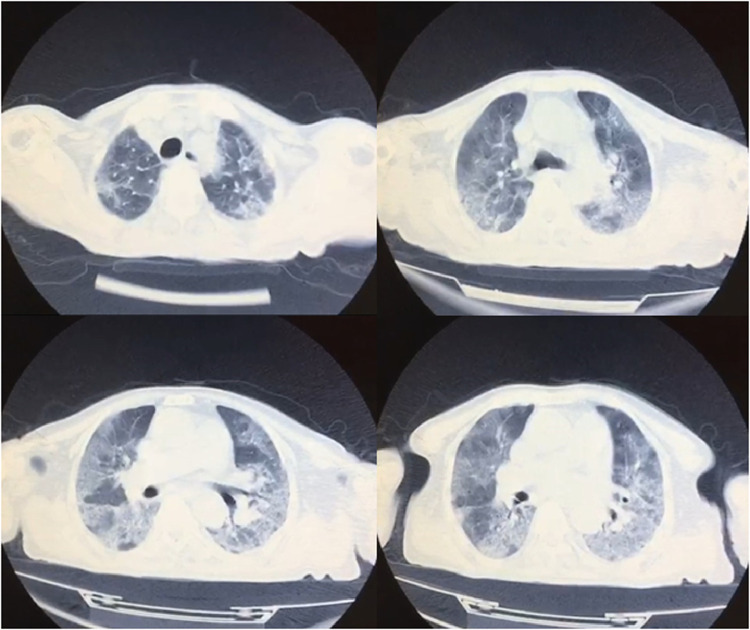
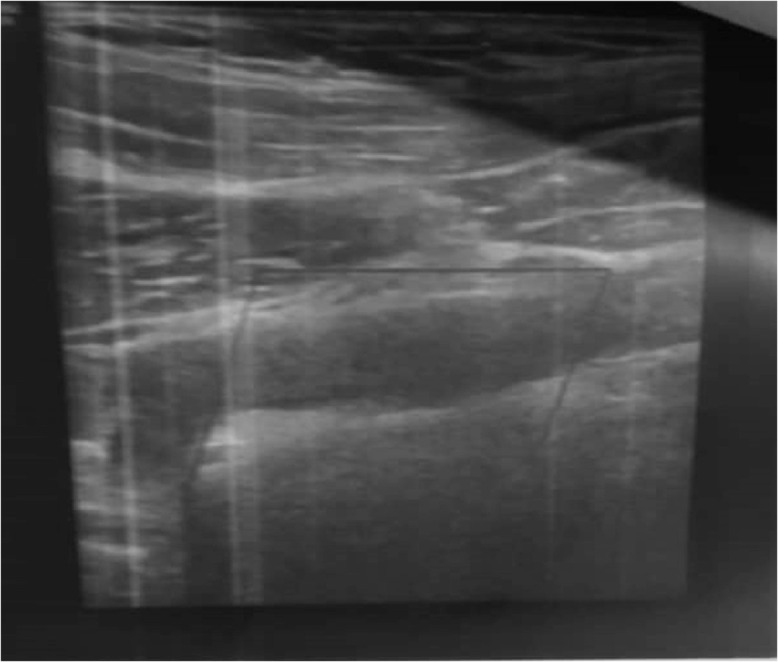
On examination, there were bilateral coarse crackles in lungs. His hand and forearm were mottled and cold with motor and sensory loss on physical examination. His radial, ulnar, brachial, and axillary pulses were absent. The Doppler ultrasound of the left arm showed intraluminal thrombus with an occlusion of the axillary and brachial arteries without any blood supply to the distal (Fig. 1 ). Transthoracic echocardiogram (TTE) showed a left ventricular ejection fraction (LVEF) of 55% and no intracardiac thrombus. He was evaluated for the COVID-19 infection by pulmonary computed tomography (PCT) and reverse-transcriptase polymerase chain reaction (RT-PCR). Other routine blood tests were also performed. In chest CT-scan, round-glass opacities were seen in both lungs, suggesting COVID-19 (Fig. 2 ). Laboratory findings presented elevated WBC, LDH, and CPK, and negative troponin I (Table I ).
Fig. 1.
Doppler ultrasound showing intraluminal thrombus.
Fig. 2.
The chest CT-scan of a COVID-19 patient, showing round-glass opacities in both lungs.
Table I.
The laboratory findings of the patient
| Parameters | Result | Normal range | Unit |
|---|---|---|---|
| Red blood cell count | 5.75 | 4.70-6.10 | 10*6/μL |
| Hemoglobin | 17.5 | 12-16 | g/dL |
| Hematocrit | 50.4 | 41-52 | % |
| White blood cell count | 30 | 4.50-11 | 10*3/μL |
| Lymphocyte | 89.7 | 20-50 | % |
| Neutrophil | 4.6 | 35-70 | % |
| Platelet count | 237 | 150-450 | 10*3/μL |
| Glucose | 103 | 70-100 | mg/dL |
| Sodium | 140 | 135-145 | mmol/L |
| Potassium | 3.9 | 3.5-5.1 | mmol/L |
| Troponin | 0.01 | 0-0.8 | ng/mL |
| D-dimer | >20 | 0-0.45 | ug/mL |
| C-reactive protein | 26 | Less than1.0 | mg/dL |
| Blood urea nitrogen | 230 | 12-45 | mg/dL |
| Creatinine | 3.1 | 05-1.20 | mg/dL |
| Aspartate transaminase | 125 | 17-60 | U/L |
| Alanine aminotransferase | 150 | 0-49 | U/L |
| Alkaline Phosphatase | 244 | 80-200 | U/L |
| CPK | 3300 | 20-200 | U/L |
| Lactate dehydrogenase | 700 | 120-246 | U/L |
The patient was treated with anticoagulation therapies and underwent open thromboembolectomy, but unfortunately, he died before undergoing the surgical operation.
DISCUSSION
Despite being initially a respiratory infection, several studies have reported other complications for COVID-19, including cardiovascular problems, renal insufficiency, liver failure, and thromboembolic events, whose occurrence has been associated with a poor prognosis.4 , 5 The prevalence of thromboembolic events among patients with COVID-19 has not been determined, yet a number of studies have shown a strong association between COVID-19 and thromboembolic events. Most studies focus on hospitalized COVID-19 patients who are likely to have comorbidities, and a few reports have noted that acute thrombotic events can be among initial manifestations.2 , 6
Thromboembolic events mainly manifest as venous thromboembolism (VTE), and peripheral arterial involvement is actually rare.7 , 8 Acute limb ischemia is characterized with a sudden decrease in the arterial perfusion of an extremity, which compromises its viability and integrity. According to the definition, in patients with ALI, the duration of symptoms is less than two weeks.3 The etiologies of ALI include embolization from proximal sources, in situ thrombosis due to atherosclerotic plaques, traumatic arterial injuries, and iatrogenic thromboembolism.3 Recently, COVID-19 has also been reported to be a possible cause of this phenomenon.8., 9., 10., 11. The deregulated hyper-inflammatory response may be responsible for the occurrence of arterial thromboembolism in patients with COVID-19;10., 11., 12. however, a combination of mechanisms may be involved in the incidence of arterial thromboembolism in these patients. Our patient demonstrated acute unilateral upper extremity ischemia, which was an unusual event.
The COVID-19 causative agent can predispose individuals to thromboembolic events by deranging the factors involved in blood coagulation regulation.7 Evidence suggests that in COVID-19 patients, the pathogenesis of arterial thrombosis is different from that of the classical arterial thrombosis,12 and COVID-19 patients may present with acute non-atherosclerotic thrombosis.8 Further studies are required to divulge the mechanisms involved in the development of thromboembolism in COVID-19 patients.
Footnotes
The Authors have no conflict of interest to disclose.
References
- 1.Mural B. Extensive arterial thrombus following discharge after a covid-19 infection. Ann of Vasc Surg. 2021;72:205–208. doi: 10.1016/j.avsg.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muhammet Ozer, Fatemah Abbasi, Mohammed Mahdi et al. Massive biventricular thrombi complicating new-onset heart failure in a patient with suspected COVID-19. J of cardiol cases doi: 10.1016/j.jccase.2021.02.016. [DOI] [PMC free article] [PubMed]
- 3.Björck Martin, Earnshaw Jonothan J, Acosta Stefan, et al. Editor's Choice- European society for vascular surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia. Eur J Vasc Endovasc Surg. 2020;2:173–218. doi: 10.1016/j.ejvs.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Madjid Mohammad, Safavi-Naeini Payam, Solomon Scott D., et al. Potential effects of coronavirus on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 5.Tang Ning, Li Dengju, Wang Xiong, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shao Tony, Lee Christina In Bok, Jabori Sinan, et al. Acute upper limb ischemia as the first manifestation in a patient with COVID-19. J Vasc Surg. 2020;6:674–677. doi: 10.1016/j.jvscit.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bilaloglu Seda, Aphinyanaphongs Yin, Jones Simon, et al. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Topcu Ahmet Can, Ozturk Altunyurt Gozde, Akman Dilara, et al. Acute limb ischemia in hospitalized COVID-19 Patients. Ann Vasc Surg. 2021 doi: 10.1016/j.avsg.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gomez Arbelaez Diego, Ibarra Sanchez Gabriela, Garcia Gutierrez Ania, et al. COVID-19 related aortic thrombosis: a report of four cases. Ann Vasc Surg. 2020;67:10–13. doi: 10.1016/j.avsg.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perini Paolo, Nabulsi Bilal, Massoni Claudio Bianchini, et al. Acute limb ischaemia in two young, non-atherosclerotic patients with COVID-19. Lancet. 2020;395:1546. doi: 10.1016/S0140-6736(20)31051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Indes Jeffrey E, Koleilat Issam, Hatch Ayesha Nzeribe, et al. Ealy experience with arterial thromboembolic complications in patients with COVID-19. J Vasc Surg. 2021;73:381–389. doi: 10.1016/j.jvs.2020.07.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piazza Gregory, Morrow David A. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA. 2020;324:2548–2549. doi: 10.1001/jama.2020.23422. [DOI] [PubMed] [Google Scholar]