Abstract
Purpose:
Youth suicide clusters may be exacerbated by suicide contagion–the spread of suicidal behaviors. Factors promoting suicide contagion are poorly understood, particularly in the advent of social media. Using cross-sectional data from an ongoing youth suicide cluster in Ohio, this study examines associations between suicide cluster-related social media and suicidal behaviors.
Methods:
We surveyed 7th- to 12th-grade students in northeastern Ohio during a 2017–2018 suicide cluster to assess the prevalence of suicidal ideation (SI), suicide attempts (SAs), and associations with potential contagion-promoting factors such as suicide cluster–related social media, vigils, memorials, news articles, and watching the Netflix series 13 Reasons Why before or during the cluster. Generalized estimating equations examined associations between potential contagion-promoting factors and SI/SA, adjusting for nonmodifiable risk factors. Subgroup analyses examined whether associations between cluster-related factors and SI/SA during the cluster varied by previous history of SI/SA.
Results:
Among participating students, 9.0% (876/9,733) reported SI and 4.9% attempted suicide (481/9,733) during the suicide cluster. Among students who posted suicide cluster–related content to social media, 22.9% (267/1,167) reported SI and 15.0% (175/1,167) attempted suicide during the suicide cluster. Posting suicide cluster–related content was associated with both SI (adjusted odds ratio 1.7, 95% confidence interval 1.4–2.0) and SA during the cluster (adjusted odds ratio 1.7, 95% confidence interval 1.2–2.5). In subgroup analyses, seeing suicide cluster–related posts was uniquely associated with increased odds of SI and SA during the cluster among students with no previous history of SI/SA.
Conclusions:
Exposure to suicide cluster–related social media is associated with both SI and SA during a suicide cluster. Suicide interventions could benefit from efforts to mitigate potential negative effects of social media and promote prevention messages.
Keywords: Suicide, Suicide cluster, Social media
Suicide clusters engender deep concern in the communities where they occur. Suicide clusters may be defined as nonrandom increases in suicide (or suicidal behaviors) occurring in close temporal or geographic proximity [1,2]. Clusters have received limited study, with available data suggesting they occur more frequently among youth aged 15–24 years [3] and account for 1%–5% of youth suicides [1,4]. Causes of clustered suicides are complex, multifactorial, and not fully understood [5].
One factor that may contribute to clustering is suicide contagion, the process by which suicidal behaviors of one or more persons promote the occurrence of subsequent suicidal behaviors in others [6,7]. Transmission of behaviors is theorized to take place both directly, through interaction or friendship with someone who dies by suicide, and indirectly, such as through exposure to media [5]. Growing research indicates that exposure to suicidal behaviors can increase the risk of already vulnerable people (e.g., individuals with a history of mental illness or feelings of hopelessness) [8]. Evidence suggests that knowledge of peers’ suicidal behaviors increases youths’ risk of subsequent suicidal behaviors: a nationally representative study of U.S. adolescents revealed that risk of suicide attempts (SAs) was consistently higher among youth exposed to friends with suicidal behaviors compared with unexposed adolescents of similar predicted risk [9,10]. Correspondingly, the occurrence of one adolescent suicide is known to be a population-based risk factor for additional suicides [3,11].
Centers for Disease Control and Prevention (CDC) recommendations exist to inform prevention and control of suicide clusters [2] but have not been updated since the advent of social media. Established in 1988 by expert consensus, these recommendations include developing a community response plan before a suicide occurs, coordinating efforts by stakeholders, minimizing media sensationalism, avoiding glorification of suicide victims, modifying environments as needed, and identifying and referring individuals at high risk of suicide [2]. Safe suicide reporting recommendations were developed for traditional media sources (e.g., television news and newspapers) to reduce contributions of media sensationalism to suicide contagion [12,13]. Proper adherence to safe suicide reporting recommendations by traditional media is associated with decreased suicide incidence [14].
The use of social media to communicate about suicide presents unique benefits and challenges in the context of suicide contagion. Potential benefits include accessibility, acceptability of social media platforms, and speed with which helpful messages can be transmitted [15]. Conversely, social media posts may contain distressing or sensationalized content, normalize suicide as a response to one’s problems, and spread information about suicide location and methods [16], all of which may increase suicidal behaviors [16,17] and contribute to suicide contagion. As yet, best practices for social media and suicide prevention are in their infancy [13,18]. Evidence-informed, publicly available #chatsafe guidelines to help young people communicate safely about suicide via social media were recently released for a U.S. audience but have yet to be widely adopted [19].
Research is emerging about the growing importance of social media on suicidal behaviors [16], but no quantitative studies have investigated social media’s impact on suicide clustering [20]. Further understanding of the mechanisms involved in clusters is needed–particularly how suicidal behaviors propagate. Most studies focus on cluster decedents; very little work has been done with attempted suicide survivors in the context of a cluster. Our study aims to describe the prevalence of suicidal behaviors and quantify the impact of suicide cluster–related exposures on adolescent suicidal behaviors in a community affected by an ongoing suicide cluster.
Methods
Design and population
Between August 2017 and March 2018, there were 12 suicide deaths among youth aged 13–18 years in a single Ohio county. During this time frame, the county’s suicide rate among youth aged 10–19 years rose to 20 deaths per 100,000 person-years–a 217% increase from previous years (2011–2016)–prompting postvention programs throughout the county and a public health investigation to prevent further deaths [21]. From April to May 2018, the local health department and Ohio Department of Health, assisted by CDC, conducted an online, anonymous, cross-sectional survey of 7th- to 12th-grade students attending public schools in the affected county to inform prevention efforts. Primary data were anonymously collected as an emergency public health response to the suicide cluster and did not qualify as human subjects’ research, as determined by a CDC Institutional Review Board/Office of Management and Budget official; secondary data analyses were also determined to be exempt from human subjects’ regulations by CDC Institutional Review Board/Office of Management and Budget. Parents/guardians were notified in advance and could refuse their child’s participation. Students could opt out of participation at any time and skip questions by selecting the response “Prefer not to say.” Students absent during the survey were unable to participate. A standardized script was read before administration, introducing the survey as a confidential, anonymous, voluntary public health activity to prevent youth suicide. Surveys were electronically administered on school-issued laptops using the Ohio Department of Health’s Research Electronic Data Capture tool [22]. School response rates were calculated as the number of completed/submitted surveys divided by the number of opened surveys. The analysis included participants with complete surveys and nonmissing data on variables of interest. Sensitivity analyses examining differences between included and excluded participants were conducted using chi-squared tests. In addition, a handful of students reporting SA without any SI were examined (n = 172). This group may represent participants with impulse control-related issues (wherein planning and premeditation do not precede attempt) or a group of “mischievous responders” who were potentially providing extreme, and potentially untruthful, responses.
Measures
Students self-reported past and current suicidal ideation (SI) or SA using a modified version of the Suicidal Behaviors Questionnaire-Revised [23], which separately assessed SI and SAs, reflecting on two different periods while completing the survey: during the suicide cluster (2017–2018 school year) and before the suicide cluster (before 2017–2018 school year). Students answering “yes” to “I had a plan at least once to kill myself but did not try to do it” or “I had a plan at least once to kill myself and really wanted to die” were classified as having SI; students who endorsed having “a brief passing thought” of killing themselves were not classified as having SI. Students answering “yes” to “Yes, I have attempted to kill myself at least once, but did not want to die” or “I have attempted to kill myself at least once, and really wanted to die” were classified as having SA.
We examined modifiable, potential suicide contagion-promoting factors related to the suicide cluster: passive exposure to vigils or moments of silence for teenagers who died by suicide during the cluster (“During this school year [2017–2018], have there been any vigils or moments of silence at your school for teenagers who died by suicide?”), seeing suicide cluster–related social media posts, posting on social media about the cluster, location of social media post (e.g., Snapchat and Facebook), seeing online news related to the cluster, and seeing memorials for cluster victims. Suicide cluster-related social media content included general posts about the suicide cluster and posts about individual adolescents who died by suicide in the affected community. Although not directly related to the suicide cluster, we considered exposure to the Netflix series 13 Reasons Why as a modifiable, potential suicide contagion-promoting factor and included variables related to viewing the show before and during the suicide cluster in our model.
Other variables examined included suicide of a friend, significant other, or family member during the 2017–2018 school year; race/ethnicity; grade; self-reported sex; gender/sexual minority (self-identification as transgender, gay, lesbian, bisexual, other, or unsure of one’s sexual orientation); and attending a school where a fellow student died by suicide during the cluster. Survey questions are provided in Supplementary Table 1.
Statistical analysis
Data analyses and visualizations were conducted using SAS version 9.4 (Cary, NC) and R version 3.4.0 (Vienna, Austria). Multivariable analyses with generalized estimating equations based on logistic distribution were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for associations between cluster-related factors and SI/SA during the cluster, accounting for clustering of students within schools using an exchangeable correlation structure. We adjusted for sociodemographics (sex, grade, race/ethnicity, gender/sexual minority); known, nonmodifiable risk factors for SI/SA during a cluster (losing a friend, significant other, or family member to suicide during the 2017–2018 school year; history of SI before cluster; and history of SA before cluster) [24]; and significant modifiable cluster-related risk factors (exposure to vigils, memorials or online news, seeing or posting suicide cluster–related content, and viewing 13 Reasons Why before or during the cluster). We computed counts and percentages of students seeing or posting on specific social media platforms for the entire analytic population and stratified by the presence/absence of suicidal outcome before the cluster. Sensitivity analyses examining differences between included and excluded participants, respondents reporting SI without SA, and respondents reporting SA without SI were conducted using chi-square tests.
Results
In total, 15,083 students from 34 schools and three counties participated (73% of all participating schools’ students; n = 20,655). We analyzed cross-sectional survey data from 27 schools that completed all survey modules and were located in the affected county (n = 12,448). Among students who completed the survey, 9,733 (78.2%) had nonmissing data on variables of interest and were included. The median school response rate was 92.0% (range: 76.8%–96.8%). The analytic sample was 50.3% female (n = 4,891), 83.8% non-Hispanic white (n = 8,154), and 10.9% identified as a gender/sexual minority (n = 1,059).
Overall, 876 students (9.0%) reported SI, and 481 students (4.9%) reported SA during the cluster (Table 1). Prevalence of both SI and SA during the cluster significantly differed for all cluster-related risk factors, excepting exposure to vigils or moments of silence and attending a school where a fellow student died by suicide during the cluster. Among youth posting about the cluster on social media (n = 1,167), one in five reported SI (22.9%, n = 267) and one in six reported SA during the cluster (15.0%, n = 175).
Table 1.
Prevalence of suicidal ideation and suicide attempt during suicide cluster by cohort characteristics, Northeast Ohio Youth Health Survey, 2018a
| Characteristic | Suicidal ideation during suicide cluster | Suicide attempt during suicide cluster | ||||||
|---|---|---|---|---|---|---|---|---|
| Cases (n = 876) | Total (N = 9,733) | %b | p c | Cases (n = 481) | Total (N = 9,733) | %b | p c | |
| Exposed to any vigils or moments of silence for teenagers who died by suicide during the suicide cluster | ||||||||
| Yes | 363 | 3,785 | 9.6 | .10 | 201 | 3,785 | 5.3 | .18 |
| No | 513 | 5,948 | 8.6 | 280 | 5,948 | 4.7 | ||
| Seen any suicide cluster–related social media posts | ||||||||
| Yes | 719 | 6,609 | 10.9 | <.001 | 401 | 6,609 | 6.1 | <.001 |
| No | 157 | 3,124 | 5.0 | 80 | 3,124 | 2.6 | ||
| Posted on social media about the suicide cluster | ||||||||
| Yes | 267 | 1,167 | 22.9 | <.001 | 175 | 1,167 | 15.0 | <.001 |
| No | 609 | 8,566 | 7.1 | 306 | 8,566 | 3.6 | ||
| Seen any news related to the suicide cluster online on a news site | ||||||||
| Yes | 505 | 5,128 | 9.8 | .002 | 273 | 5,128 | 5.3 | .07 |
| No | 371 | 4,605 | 8.1 | 208 | 4,605 | 4.5 | ||
| Seen any memorials for teenagers who died by suicide during suicide cluster | ||||||||
| Yes | 426 | 3,663 | 11.6 | <.001 | 248 | 3,663 | 6.8 | <.001 |
| No | 450 | 6,070 | 7.4 | 233 | 6,070 | 3.8 | ||
| Student at a school where a fellow student died by suicide during the suicide cluster | ||||||||
| Yes | 128 | 1,601 | 8.0 | .12 | 74 | 1,601 | 4.6 | .52 |
| No | 748 | 8,132 | 9.2 | 407 | 8,132 | 5.0 | ||
| Saw 13 Reasons Why before suicide cluster | ||||||||
| Yes | 428 | 3,633 | 11.8 | <.001 | 249 | 3,633 | 6.9 | <.001 |
| No | 448 | 6,100 | 7.3 | 232 | 6,100 | 3.8 | ||
| Saw 13 Reasons Why during suicide cluster | ||||||||
| Yes | 183 | 1,269 | 14.4 | <.001 | 114 | 1,269 | 9.0 | <.001 |
| No | 693 | 8,464 | 8.2 | 367 | 8,464 | 4.3 | ||
| History of suicidal ideation before suicide cluster | ||||||||
| Yes | 655 | 1,072 | 61.1 | <.001 | 351 | 1,072 | 32.7 | <.001 |
| No | 221 | 8,661 | 2.6 | 130 | 8,661 | 1.5 | ||
| Suicidal ideation during suicide cluster | ||||||||
| Yes | 407 | 876 | 46.5 | <.001 | ||||
| No | 74 | 8,857 | .8 | |||||
| History of suicide attempt before suicide cluster | ||||||||
| Yes | 430 | 712 | 60.4 | <.001 | 370 | 712 | 52.0 | <.001 |
| No | 446 | 9,021 | 4.9 | 111 | 9,021 | 1.2 | ||
| Suicide attempt during suicide cluster | ||||||||
| Yes | 407 | 481 | 84.6 | <.001 | ||||
| No | 469 | 9,252 | 5.1 | |||||
Suicide cluster time frame defined as August 2017 to April 2018. Northeast Ohio Youth Health Survey data collected from 7th- to 12th-grade students from 27 schools in one Ohio county.
Row percent.
p calculated from chi-square test.
Overall, 67.9% of students saw (n = 6,609) and 12.0% of students posted (n = 1,167) suicide cluster–related content on social media (Table 1). Social media engagement differed by SI during the cluster. Among students with SI during the cluster (n = 876), 82.0% saw and 30.5% posted suicide cluster–related content. Among students without SI during the cluster (n = 8,857), 66.5% saw and 10.2% posted cluster-related content. Figure 1 displays social media engagement on specific platforms by the history of SI during the suicide cluster.
Figure 1.
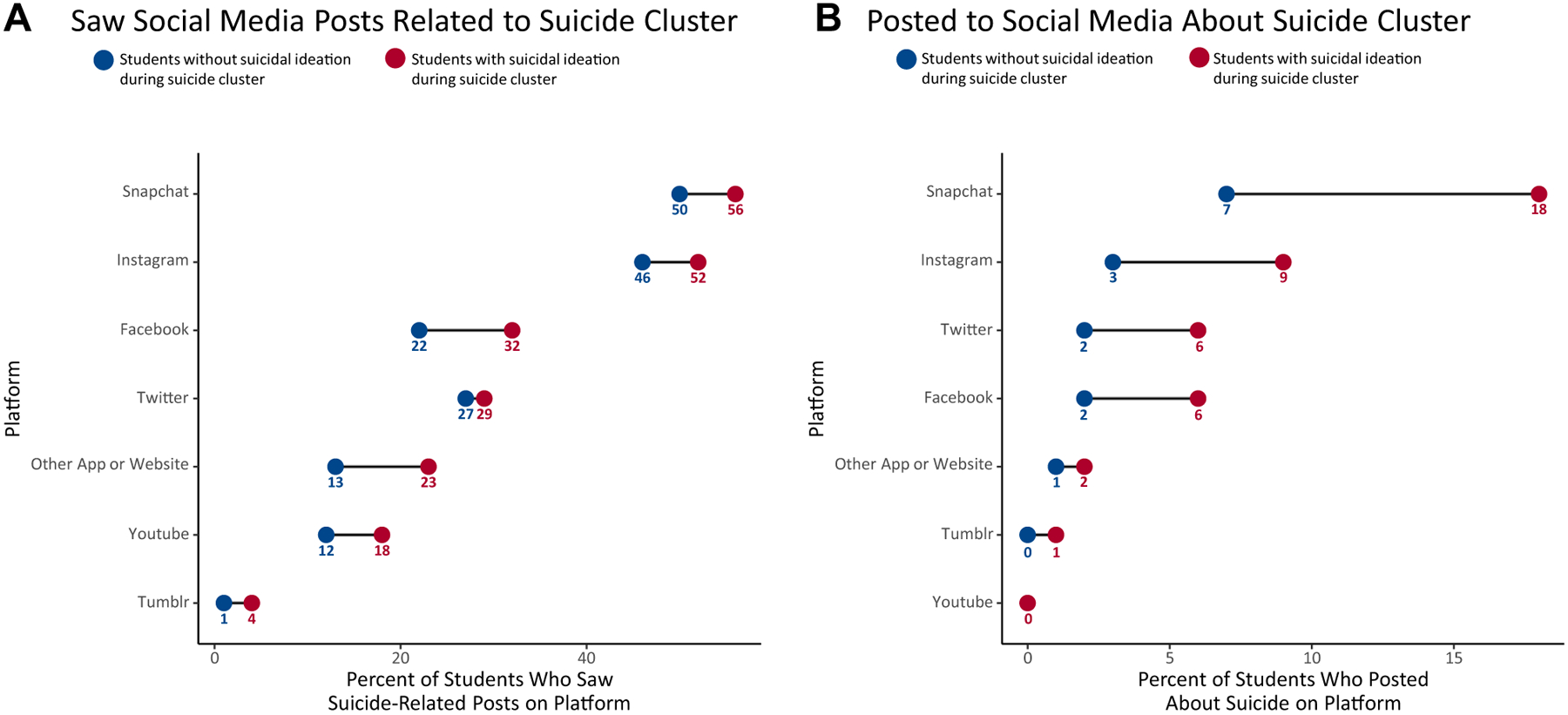
Percent of students interacting with suicide cluster–related social media by the type of social media platform and type of interaction, based on history of suicidal ideation during the suicide cluster.a Panel A shows the prevalence of seeing a post about local youth suicide cluster deaths on various social media platforms for students with and without suicidal ideation during the suicide cluster (coincident with the 2017‒2018 school year). Panel B shows the prevalence of posting to social media about the local youth suicide cluster deaths for students with and without suicidal ideation during the suicide cluster. Other app or website was defined as any other chat app, anonymous posting app, or website that a student used to interact with suicide cluster–related social media. aData reported by 9,733 7th- to 12th-grade students from 27 schools in one Ohio county following a suicide cluster (August 2017–April 2018).
Among all students, after adjusting for sociodemographics and known, nonmodifiable risk factors for suicide during a cluster (e.g., losing a loved one to suicide and previous history of suicidal behaviors), seeing (adjusted OR [AOR] 1.3, CI 1.1–1.7) and posting (AOR 1.7, CI 1.4–2.0) suicide cluster–related social media content were significantly associated with SI during the cluster (Table 2). When adjusted for sociodemographic and other cluster-related risk factors, exposures to memorials, vigils, moments of silence, and online cluster-related news articles were not significantly associated with SI during the cluster. Watching 13 Reasons Why during the suicide cluster was associated with increased odds of SI after adjustment for other factors (AOR 1.4, CI 1.04–1.8); precluster exposure to 13 Reasons Why did not demonstrate significant associations with SI during the cluster. After adjustment, only posting suicide cluster–related social media content (AOR 1.7, CI 1.2–2.5) was associated with increased odds of SA during the cluster (Table 3). Seeing news related to the suicide cluster online on a news site was associated with decreased odds of SA during the cluster (AOR .8, CI .6–.99). When adjusted for sociodemographic and other risk factors, exposures to memorials, vigils, moments of silence, watching 13 Reasons Why, or seeing suicide cluster–related social media posts were not associated with SA during the cluster. When adjusted for sociodemographic variables only, exposure to memorials remained significantly associated with SA during the cluster; addition of ≥2 suicide cluster–related exposures (exposure to vigils or online news, seeing or posting suicide cluster–related content, and viewing 13 Reasons Why before or during the cluster) eliminated effects observed in the bivariate model.
Table 2.
Associations between suicide cluster–related risk factors and suicidal ideation during suicide cluster, Northeast Ohio Youth Health Survey, 2018a
| Modifiable risk factor | Suicidal ideation among all students | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedb | |||||||||||
| OR | 95% CI | p | OR | 95% CI | p | |||||||
| Exposed to any vigils or moments of silence for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.1 | .96–1.3 | .15 | 1.1 | .8–1.4 | .56 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any suicide cluster–related social media posts | ||||||||||||
| Yes | 2.3 | 2.0–2.7 | <.001 | 1.3 | 1.1–1.7 | .01 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Posted on social media about the suicide cluster | ||||||||||||
| Yes | 3.8 | 3.2–4.4 | <.001 | 1.7 | 1.4–2.0 | <.001 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any news related to the suicide cluster online on a news site | ||||||||||||
| Yes | 1.3 | 1.1–1.5 | .001 | .9 | .8–1.1 | .24 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any memorials for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.6 | 1.4–1.8 | <.001 | 1.0 | .9–1.2 | .97 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why before suicide cluster | ||||||||||||
| Yes | 1.7 | 1.4–1.9 | <.001 | 1.1 | .9–1.3 | .48 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why during suicide cluster | ||||||||||||
| Yes | 1.8 | 1.6–2.1 | <.001 | 1.4 | 1.04–1.8 | .03 | ||||||
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
CI = confidence interval; OR = odds ratio.
Suicide cluster timeframe defined as August 2017–April 2018. Northeast Ohio Youth Health Survey data collected from 7th- to 12th-grade students from 27 schools in one Ohio county.
Adjusted for race; grade; sex; gender/sexual minority; losing a friend, significant other, or family member to suicide during the 2017–2018 school year (coincident with the suicide cluster); previous history of suicidal ideation before cluster; previous history of attempt before cluster; and all variables in table.
Table 3.
Associations between suicide cluster–related risk factors and suicide attempt during suicide cluster, Northeast Ohio Youth Health Survey, 2018a
| Modifiable risk factor | Suicide attempts among all students | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjustedb | |||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Exposed to any vigils or moments of silence for teenagers who died by suicide during this school year | ||||||
| Yes | 1.1 | .9–1.3 | .27 | 1.3 | .99–1.7 | .06 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Seen any social media posts related to suicide | ||||||
| Yes | 2.5 | 2.0–3.1 | <.001 | 1.2 | .9–1.5 | .25 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Posted on social media related to suicide | ||||||
| Yes | 4.5 | 3.6–5.7 | <.001 | 1.7 | 1.2–2.5 | .003 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Seen any news online on a news site | ||||||
| Yes | 1.3 | 1.03–1.6 | .03 | .8 | .6–.99 | .04 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Seen any memorials | ||||||
| Yes | 1.8 | 1.5–2.1 | <.001 | .9 | .7–1.1 | .28 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Saw 13 Reasons Why before suicide cluster | ||||||
| Yes | 1.8 | 1.6–2.2 | <.001 | 1.1 | .9–1.4 | .49 |
| No | 1.0 | Reference | 1.0 | Reference | ||
| Saw 13 Reasons Why during suicide cluster | ||||||
| Yes | 2.1 | 1.6–2.6 | <.001 | 1.4 | .9–2.2 | .16 |
| No | 1.0 | Reference | 1.0 | Reference | ||
CI = confidence interval; OR = odds ratio.
Suicide cluster timeframe defined as August 2017–April 2018. Northeast Ohio Youth Health Survey data collected from 7th- to 12th-grade students from 27 schools in one Ohio county.
Adjusted for race; grade; sex; gender/sexual minority; losing a friend, significant other, or family member to suicide during the 2017–2018 school year (coincident with the suicide cluster); previous history of suicidal ideation before cluster; previous history of attempt before cluster; and all variables in table.
In subgroup analyses of students without prior history of SI or SA, both SI and SA during the cluster were significantly associated with seeing (SI: AOR 2.0, CI 1.3–3.0; and SA: AOR 1.6, CI 1.1–2.3) and posting (SI: AOR 1.7, CI 1.2–2.4; and SA: AOR 2.0, CI 1.3–3.0) cluster-related social media content (Tables 4 and 5). Watching 13 Reasons Why during the suicide cluster was only associated with increased odds of SI for students without previous history of SI (AOR 1.5, CI 1.03–2.1), and students with previous history of SI/SA or students who saw 13 Reasons Why before the suicide cluster did not demonstrate increased odds of SI or SA. Among students with previous history of SI or SA, only posting suicide cluster–related content was associated with SI (AOR 1.5, CI 1.2–1.8) during the cluster. Exposure to vigils or moments of silence for teenagers who died by suicide during the suicide cluster was associated with increased odds of SA among students with previous history of SA (AOR 1.3, CI 1.01–1.6). Seeing suicide cluster–related news online on a news site was associated with decreased odds of SA among students with prior history of SA (AOR .6, CI .4–.9).
Table 4.
Associations between suicide cluster–related risk factors and suicidal ideation during suicide cluster, based on history of suicidal ideation before suicide cluster, Northeast Ohio Youth Health Survey, 2018a
| Modifiable risk factor | Among students without history of suicidal ideation before suicide cluster | Among students with history of suicidal ideation before suicide cluster | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedb | Unadjusted | Adjustedb | |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Exposed to any vigils or moments of silence for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.2 | .9–1.5 | .14 | 1.0 | .7–1.3 | .78 | 1.1 | .9–1.5 | .35 | 1.2 | .9–1.5 | .22 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any suicide cluster–related social media posts | ||||||||||||
| Yes | 2.7 | 1.8–3.9 | <.001 | 2.0 | 1.3–3.0 | .001 | 1.1 | .9–1.5 | .38 | .9 | .7–1.3 | .75 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Posted on social media about the suicide cluster | ||||||||||||
| Yes | 3.5 | 2.5–4.8 | <.001 | 1.7 | 1.2–2.4 | .002 | 1.6 | 1.3–2.0 | <.001 | 1.5 | 1.2–1.8 | .001 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any news related to the suicide cluster online on a news site | ||||||||||||
| Yes | 1.2 | .9–1.7 | .17 | .9 | .6–1.2 | .35 | 1.0 | .8–1.3 | .92 | .9 | .7–1.2 | .68 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any memorials for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.7 | 1.3–2.1 | <.001 | 1.1 | .9–1.4 | .41 | 1.0 | .9–1.3 | .64 | .9 | .7–1.1 | .30 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why before suicide cluster | ||||||||||||
| Yes | 1.7 | 1.2–2.2 | .001 | 1.2 | .9–1.7 | .31 | .9 | .7–1.2 | .63 | .9 | .6–1.2 | .46 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why during suicide cluster | ||||||||||||
| Yes | 2.0 | 1.5–2.7 | <.001 | 1.5 | 1.03–2.1 | .04 | 1.3 | .9–1.7 | .15 | 1.2 | .8–1.7 | .43 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
CI = confidence interval; OR = odds ratio.
Suicide cluster timeframe defined as August 2017–April 2018. Northeast Ohio Youth Health Survey data collected from 7th- to 12th-grade students from 27 schools in one Ohio county.
Adjusted for race; grade; sex; gender/sexual minority; losing a friend, significant other, or family member to suicide during the 2017–2018 school year (coincident with the suicide cluster); history of suicide attempt before suicide cluster; and all variables in table.
Table 5.
Associations between suicide cluster–related risk factors and suicide attempt during suicide cluster, based on history of suicide attempt before suicide cluster, Northeast Ohio Youth Health Survey, 2018a
| Characteristic | Among students without history of suicide attempt before suicide cluster | Among students with history of suicide attempt before suicide cluster | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedb | Unadjusted | Adjustedb | |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Exposed to any vigils or moments of silence for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.3 | .8–2.1 | .28 | 1.2 | .7–2.1 | .46 | 1.1 | .8–1.4 | .58 | 1.3 | 1.01–1.6 | .04 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any suicide cluster–related social media posts | ||||||||||||
| Yes | 2.3 | 1.6–3.3 | <.001 | 1.6 | 1.1–2.3 | .03 | 1.1 | .7–1.6 | .72 | 1.0 | .6–1.6 | .85 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Posted on social media about the suicide cluster | ||||||||||||
| Yes | 4.2 | 2.9–6.2 | <.001 | 2.0 | 1.3–3.0 | .002 | 1.6 | 1.2–2.2 | .005 | 1.5 | .9–2.4 | .09 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any news related to the suicide cluster online on a news site | ||||||||||||
| Yes | 1.2 | .9–1.7 | .15 | 1.0 | .7–1.4 | .98 | .7 | .5–.9 | .02 | .6 | .4–.9 | .003 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Seen any memorials for teenagers who died by suicide during the suicide cluster | ||||||||||||
| Yes | 1.4 | 1.1–1.9 | .02 | .9 | .7–1.3 | .55 | 1.0 | .7–1.3 | .90 | .8 | .6–1.1 | .17 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why before suicide cluster | ||||||||||||
| Yes | 1.5 | 1.1–2.0 | .007 | 1.1 | .8–1.7 | .54 | 1.1 | .9–1.4 | .52 | 1.0 | .7–1.3 | .83 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
| Saw 13 Reasons Why during suicide cluster | ||||||||||||
| Yes | 2.0 | 1.2–3.2 | .004 | 1.4 | .8–2.4 | .23 | 1.3 | .9–1.9 | .19 | 1.2 | .7–2.1 | .54 |
| No | 1.0 | Reference | 1.0 | Reference | ||||||||
CI = confidence interval; OR = odds ratio.
Suicide cluster timeframe defined as August 2017–April 2018. Northeast Ohio Youth Health Survey data collected from 7th- to 12th-grade students from 27 schools in one Ohio county.
Adjusted for race; grade; sex; gender/sexual minority; losing a friend, significant other, or family member to suicide during the 2017–2018 school year (coincident with the suicide cluster); history of suicidal ideation before suicide cluster; and all variables in table.
In sensitivity analyses, participants with missing data differed from included participants for 14/18 variables. Participants with missing data were more likely to have SI/SA before and during the cluster; be a racial, ethnic, gender, or sexual minority; have seen 13 Reasons Why during the suicide cluster; have lost a friend, significant other, or family member to suicide during the suicide cluster; and report exposure to 4/5 cluster-related variables (Supplementary Table 2). Adjusted results did not significantly differ when missing participants were included.
The results from analyses including and excluding students who reported SA without any SI (n = 172) varied little.
Discussion
This is the first quantitative study to examine associations between social media and suicidal behaviors in a suicide cluster. Among those who posted suicide cluster–related content to social media, 24.9% reported SI or SA during the cluster (22.9% SI and 15.0% SA). Exposure to suicide cluster–related social media content was associated with significantly increased odds of SI/SA during the cluster when compared with students without any suicide cluster–related social media exposure. Most studies of suicide-related social media exposure occur outside of suicide clusters: one such study reported 25% of adolescents were exposed to suicide stories on social networking sites and 15% on online discussion forums [17]. In our study, over two thirds of students saw posts related to the suicide cluster on social media, suggesting that clusters may increase attention and engagement with suicide-related content on social media. Our findings suggest that vulnerable youths’ risk of suicidal behaviors may be compounded by interactions with suicide cluster–related social media.
One interesting aspect of our results is the differing associations for seeing versus posting suicide cluster–related content. In general, passive exposure to content (seeing suicide cluster–related posts) was associated with SI but not SAs. In contrast, actively producing content (posting about the suicide cluster) was associated with both SI and SA during the cluster. In general, producing suicide cluster–related content may occur among individuals at higher risk on the spectrum of suicidal behaviors. Creating suicide cluster–related social media content may be motivated by different thought processes for different individuals: a “rehearsal” of SI or plan, a cry for help, a way to connect with others with similar problems. Further research is needed to understand how the frequency and quality of social media posts correlate with the risk of suicide. Moreover, qualitative studies analyzing the content of suicide cluster–related posts would be helpful to determine and categorize posters’ psychology.
Previous research demonstrates the negative impacts of exposure to traditional media on suicide and suicide clusters [6,25]. However, our study found that when adjusted for sociodemographics, history of suicidality, and social media exposure, seeing suicide-related online news articles was not associated with SI and was, in fact, associated with decreased odds of SA during the cluster. This may be explained in part by the displacement of conventional news sources in favor of social media or viewing news-related content on social media rather than traditional sources or adherence by journalists to safe suicide reporting guidelines [26]. Although journalists may receive training on safe suicide reporting, safe social media guidelines have yet to be widely adopted by the public [19]. Without increased public awareness, the inclusion of potentially harmful content in user-created posts is likely, including sensationalized language or information about suicide location and methods. Furthermore, one of the mechanisms by which news media is theorized to confer risk–differential identification–may be amplified by exposure to peers’ social media posts [27]. Differential identification speculates that social similarity between an individual and a “model” (e.g., same age and sex) is an important factor in identification and imitative behavior [28]. Social media may heighten differential identification, conveying subsequent increased risk of identification and suicidal behaviors in vulnerable individuals.
We found associations between viewing the Netflix series 13 Reasons Why during the suicide cluster and SI among students without a previous history of SI. This is consistent with previous studies demonstrating correlations between the release of 13 Reasons Why and suicide-related behaviors, such as increased internet queries related to suicide and excess pediatric hospital admissions for SAs [29,30]. One study of youths’ exposure to 13 Reasons Why found that the majority of youth at high risk of suicide viewed the show alone and did not discuss their reaction with a parent or other adult [31]. More than half of this previous study’s viewers believed the series increased their suicide risk to a nonzero degree, particularly those individuals who strongly identified with the lead female character. The fact that we did not detect a statistically significant effect of watching the show during the suicide cluster among those youth with a prior history of SI or SA may be attributable to low numbers and smaller power among this subpopulation, as the AOR trended in the expected direction.
A major strength of our study was the use of data from an ongoing suicide cluster. Most studies take place after a cluster concludes; to the authors’ knowledge, this is one of the first studies to collect data from an ongoing suicide cluster [11,32,33]. Our study revealed that many risk factors traditionally associated with suicide contagion–seeing memorials, online news articles, attending the same school as a decedent–were not associated with suicidal behaviors in this active suicide cluster. Further research on active suicide clusters is needed to better understand modifiable risk factors. In addition, most studies focus on cluster decedents [4,8,20,34]. By investigating youth at risk for suicide during an active cluster, stakeholders immediately used findings to inform prevention. Within weeks of the investigation, local stakeholders used survey results to increase mental health counselors and educators at schools, increase the availability of behavioral health mobile response teams, strengthen cross-system collaboration and improvements to address suicide risk and prevention factors, and expand gatekeeper training in the community. The timeliness and relevance of information gathered about suicide risk was directly applied to stop transmission of risk in the context of the suicide cluster.
Our study has important limitations. First, given the cross-sectional design, we cannot establish causality. To strengthen conclusions, questions referenced explicit time points where possible, but we cannot establish whether social media exposure preceded SI/SA. Future studies could be improved by clarifying the timing and context of social media exposure (e.g., intended vs. unintended, purposeful search for material, passive exposure, and time spent on platform). This may help clarify whether associations between SI/SA and exposure to suicide cluster–related social media are explained by assortative relating–the tendency for similar individuals to preferentially associate with one another (e.g., teens with history of SI/SA may be more likely to form online relationships with others reporting history of SI/SA and thereby experience increased exposure to online suicide-related content)–or if exposure to suicide cluster–related content is generating new SI/SA in vulnerable individuals. Research is needed to understand how the quantity and quality of exposure to suicide-related social media influences identified associations (e.g., dose–response pattern for the number of posts seen/created). Second, results may not be generalizable to other clusters. Our analyses represent students with nonmissing data from participating public schools in the affected county. We analyzed the risk factors for nonfatal suicidal behaviors in a cluster; risk factors associated with dying by suicide may differ. Additional studies of ongoing clusters are merited. Third, exclusion of participants with missing data and potential hesitance to participate by youth with higher prevalence of SI/SA may lead to underrepresentation of the true prevalence and associations. For example, 22% of the excluded participants self-identified as a sexual or gender identity minority–a group that traditionally has higher rates of SI/SA than their cisgender, heterosexual peers. Finally, the Northeast Ohio Youth Health Survey assessed passive exposure to vigils or moments of silence using a single question: “During this school year (2017–2018), have there been any vigils or moments of silence at your school for teenagers who died by suicide?” Future surveys would benefit from assessing active exposure (attendance at a vigil) and separately measuring vigils and moments of silence.
Social media represent an important prevention opportunity, whether suicide-related content contributes to the development of suicidality or suicidal youth are more likely to engage with suicide-related posts. A 21st-century update to CDC’s suicide cluster response recommendations with explicit guidelines around safe social media practices would be valuable [2]. Just as improved understanding of traditional media’s effects on suicide contagion led to safer suicide reporting, better comprehension of social media’s influence on suicidal behaviors may prevent suicide. One potential way to mitigate suicide contagion is adaptation of safe suicide reporting recommendations for social media. Several suicide prevention organizations have already created recommendations for social media [18,19,35]; widely sharing and incorporating these recommendations into social media platforms may save lives. Some strategies–policies on how to respond to potentially suicidal users, timeliness of response to suicidal content, and information on where to refer potentially suicidal individuals–may be easily integrated into digital platforms [16]. The National Suicide Prevention Lifeline developed a toolkit to help digital community managers identify and respond to concerning suicidal content online [36]; the warning signs and response plans outlined in this toolkit may be adopted by online communities and adapted for use by parents and peers. Similarly, resources developed for parents, providers, and journalists by the American Association of Suicidology promote social media strategies rooted in journalism ethics and suicide prevention [37,38].
How communities effectively offer online support to individuals is a research question in its own right. Some interventions (e.g., efforts to facilitate ongoing support, connection, and guidance on how to access supportive services) could lead to positive outcomes or counterproductive outcomes (e.g., decreased participation in a given online community or migration to alternative platforms where finding/extending help to vulnerable individuals may be harder). Research is needed to clarify how social media can best help those at risk of suicidal behaviors during a cluster (e.g., screening and providing resources).
Social media are a powerful tool with the capacity to provide protective effects and meaningful interventions for those at risk of suicide. Although excessive social media use has been linked to adverse outcomes like depression and anxiety [39], social media has also been associated with positive outcomes such as reinforcement of healthy behaviors and help-seeking [40]. For some vulnerable youth, online social platforms can be protective, linking otherwise isolated individuals with supportive communities [41]. Social media provide a valuable resource for suicidal people in need of support, particularly on platforms that offer constructive help and actively avoid normalizing or condoning suicidal behavior [13]. Available research suggests that both protective and harmful effects are possible; further research is needed to clarify how social media can be used to better protect and promote youth mental health.
Importantly, even with the development and adoption of safe social media recommendations, the ways youth discuss suicide on social media may not change [42]. A comprehensive prevention approach is needed. Teaching young people safe ways to communicate about suicide and develop content is one promising method [42]. Gatekeeper training on identification and support of people at risk for suicide empowers peers, parents, educators, and community members to monitor and provide assistance [43]. Given the large percentage of youth who saw posts on difficult-to-monitor platforms, educating youth about safe online communication, risk identification, and response is an important component of a larger, comprehensive approach to suicide prevention [44].
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
This quantitative study examines the associations between social media and suicidal behaviors in a suicide cluster. These findings suggest that vulnerable youth’s risk of suicidal behaviors may be compounded by interactions with suicide cluster–related social media content.
Acknowledgments
The authors would like to thank the members of the Stark County Coordinating Committee for facilitating the Northeast Ohio Youth Health Survey and advancing youth suicide prevention efforts in Stark County. The authors are grateful to John Aller, Michele Boone, Allison Esber, Joe Chaddock, Marty Bowe, Dack Warner, Sherry Smith, and Avi Joseph for their contributions to the 2018 youth suicide cluster response. The authors would like to thank the teachers and school administrators who facilitated the survey and the students for their candid participation.
Everyone who contributed significantly to the work has been listed in Acknowledgments.
Funding Sources
This work was supported by the Centers for Disease Control and Prevention and Ohio Department of Health.
Footnotes
Supplementary Data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2020.05.049.
Conflicts of interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- [1].Gould MS, Wallenstein S, Davidson L. Suicide clusters: A critical review. Suicide Life-Threat Behav 1989;19:17–29. [DOI] [PubMed] [Google Scholar]
- [2].O’Carroll PW, Mercy JA, Steward JA. CDC recommendations for a community plan for the prevention and containment of suicide clusters. MMWR Suppl 1988;37:1–12. [PubMed] [Google Scholar]
- [3].Gould M, Wallenstein S, Kleinman M, et al. Suicide clusters: An examination of age-specific effects. Am J Public Health 1990;80:211–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gould MS, Wallenstein S, Kleinman M. Time-space clustering of teenage suicide. Am J Epidemiol 1990;131:71–8. [DOI] [PubMed] [Google Scholar]
- [5].Haw C, Hawton K, Niedzwiedz C, et al. Suicide clusters: A review of risk factors and mechanisms. Suicide Life-Threat Behav 2013;43:97–108. [DOI] [PubMed] [Google Scholar]
- [6].Gould M, Jamieson P, Romer D. Media contagion and suicide among the young. Am Behav Scientist 2003;46:1269–84. [Google Scholar]
- [7].Poijula S, Wahlberg K-E, Dyregrov A. Adolescent suicide and suicide contagion in three secondary schools. Int J Emerg Ment Health 2001;3: 163–70. [PubMed] [Google Scholar]
- [8].Davidson LE, Rosenberg ML, Mercy JA, et al. An epidemiologic study of risk factors in two teenage suicide clusters. J Am Med Assoc 1989;262:2687–92. [PubMed] [Google Scholar]
- [9].Randall JR, Nickel NC, Colman I. Contagion from peer suicidal behavior in a representative sample of American adolescents. J affective Disord 2015; 186:219–25. [DOI] [PubMed] [Google Scholar]
- [10].Mueller AS, Abrutyn S, CJSp Stockton. Can social ties be harmful? Examining the spread of suicide in early adulthood. Sociol Perspect 2015;58: 204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Askland KD, Sonnenfeld N, Crosby A. A public health response to a cluster of suicidal behaviors: Clinical psychiatry, prevention, and community health. J Psychiatr Pract 2003;9:219–27. [DOI] [PubMed] [Google Scholar]
- [12].Recommendations for reporting on suicide. Available at: http://reportingonsuicide.org/wp-content/themes/ros2015/assets/images/Recommendations-eng.pdf.AccessedApril 8, 2020.
- [13].World Health Organization. Preventing suicide: A resource for media professionals, update 2017. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- [14].Sonneck G, Etzersdorfer E, Nagel-Kuess S. Imitative suicide on the Viennese subway. Social Sci Med 1994;38:453–7. [DOI] [PubMed] [Google Scholar]
- [15].Hui A, Wong PW-C, Fu K-W. Evaluation of an online campaign for promoting help-seeking attitudes for depression using a Facebook advertisement: An online randomized controlled experiment. JMIR Ment Health 2015;2:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Luxton DD, June JD, Fairall JM. Social media and suicide: A public health perspective. Am J Public Health 2012;102:S195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dunlop SM, More E, Romer D. Where do youth learn about suicides on the Internet, and what influence does this have on suicidal ideation? J Child Psychol Psychiatry 2011;52:1073–80. [DOI] [PubMed] [Google Scholar]
- [18].TEAM Up. Social media guidelines for mental health promotion and suicide prevention. Sterling, VA: Entertainment Industry Council; 2015. [Google Scholar]
- [19].Robinson J, Hill NTM, Thorn P, et al. The #chatsafe project. Developing guidelines to help young people communicate safely about suicide on social media: A Delphi study. PLoS One 2018;13:e0206584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Robertson L, Skegg K, Poore M, et al. An adolescent suicide cluster and the possible role of electronic communication technology. Crisis 2012;33:239–45. [DOI] [PubMed] [Google Scholar]
- [21].Swedo EA, Beauregard JR, Montgomery M, et al. Epi-aid 2018–025: Increase in youth suicides – Stark County, Ohio, 2018. Atlanta, GA: Centers for Disease Control and Prevention; 2019:134. [Google Scholar]
- [22].Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Osman A, Bagge C, Guitierrez P, et al. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment 2001;5:443–54. [DOI] [PubMed] [Google Scholar]
- [24].Centers for Disease Control and Prevention. Suicide: Risk and protective factors. Available at: https://www.cdc.gov/violenceprevention/suicide/riskprotectivefactors.html.AccessedApril 8, 2020.
- [25].Mueller AS. Does the media matter to suicide?: Examining the social dynamics surrounding media reporting on suicide in a suicide-prone community. Social Sci Med 2017;180:152–9. [DOI] [PubMed] [Google Scholar]
- [26].Twenge JM, Martin GN, Spitzberg BH. Trends in US Adolescents’ media use, 1976–2016: The rise of digital media, the decline of TV, and the (near) demise of print. Psychol Popular Media Cult 2018;8:329–45. [Google Scholar]
- [27].Stack S Celebrities and suicide: A taxonomy and analysis, 1948–1983. Am Soc Rev 1987;52:401–12. [PubMed] [Google Scholar]
- [28].Glaser D Criminality theories and behavioral images. Am J Sociol 1956;61: 433–44. [Google Scholar]
- [29].Cooper MT, Bard D, Wallace R, et al. Suicide attempt admissions from a single children’s hospital before and after the introduction of Netflix series 13 Reasons Why. J Adolesc Health 2018;63:688–93. [DOI] [PubMed] [Google Scholar]
- [30].Ayers JW, Althouse BM, Leas EC, et al. Internet searches for suicide following the release of 13 Reasons Why. JAMA Intern Med 2017;177:1527–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hong V, Ewell Foster CJ, Magness CS, et al. 13 Reasons Why: Viewing patterns and perceived impact among youths at risk of suicide. Psychiatr Serv 2018;70:107–14. [DOI] [PubMed] [Google Scholar]
- [32].Brent DA, Kerr MM, Goldstein C, et al. An outbreak of suicide and suicidal behavior in a high school. J Am Acad Child Adolesc Psychiatry 1989;28: 918–24. [DOI] [PubMed] [Google Scholar]
- [33].Fowler K, Crosby A, Parks S, et al. Epidemiological investigation of a youth suicide cluster: Delaware 2012. Del Med J 2013;85:15–9. [PMC free article] [PubMed] [Google Scholar]
- [34].Phillips DP, Carstensen LL. Clustering of teenage suicides after television news stories about suicide. New Engl J Med 1986;315:685–9. [DOI] [PubMed] [Google Scholar]
- [35].Acosta J, Ramchand R, Becker A. Best practices for suicide prevention messaging and evaluating California’s “Know the signs” Media Campaign. Crisis 2017;38:287–99. [DOI] [PubMed] [Google Scholar]
- [36].National Suicide Prevention Lifeline, Vibrant Emotional Health. Support for suicidal individuals on social and digital media. Available at: http://www.sprc.org/sites/default/files/resource-program/lifeline_socialmedia_toolkit.pdf.AccessedApril 8, 2020.
- [37].American Association of Suicidology. Suicide reporting recommendations: Media as partners in suicide prevention. Washington, DC: American Association of Suicidology; 2018. [Google Scholar]
- [38].American Association of Suicidology. Suicide and social media: A tipsheet for parents and providers. Available at: https://suicidology.org/wp-content/uploads/2019/07/SUICIDE-SOCIAL-MEDIA.pdf.AccessedApril 8, 2020.
- [39].Woods HC, Scott H. #Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J Adolesc 2016;51:41–9. [DOI] [PubMed] [Google Scholar]
- [40].Powell J, McCarthy N, Eysenbach G. Cross-sectional survey of users of Internet depression communities. BMC Psychiatry 2003;3:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Naslund JA, Grande SW, Aschbrenner KA, et al. Naturally occurring peer support through social media: The experiences of individuals with severe mental illness using YouTube. PLoS One 2014;9:e110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Robinson J, Bailey E, Hetrick S, et al. Developing social media-based suicide prevention messages in partnership with young people: Exploratory study. JMIR Ment Health 2017;4:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Isaac M, Elias B, Katz LY, et al. Gatekeeper training as a preventative intervention for suicide: A systematic review. Can J Psychiatry Revue canadienne de psychiatrie 2009;54:260–8. [DOI] [PubMed] [Google Scholar]
- [44].Stone DM, Holland KM, Bartholow BN, et al. Preventing suicide: A technical package of policies, programs, and practice. Atlanta, GA: Centers for Disease Control and Prevention; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


